Professional Documents
Culture Documents
Rehabilitation Protocol For Knee Replacement
Uploaded by
Shaun TylerOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rehabilitation Protocol For Knee Replacement
Uploaded by
Shaun TylerCopyright:
Available Formats
Mr.
Matthew Evans
9529 3820
www.matthewevans.com.au
Mr. Ashley Carr
9573 9684
www.ashleycarr.com.au
Melbourne Orthopaedic Group
A.C.N. 005 057 269
33 The Avenue, Windsor 3181.
P.O. Box 447, Prahran 3181.
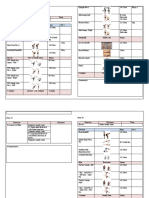
REHABILITATION PROTOCOL FOR
KNEE REPLACEMENT SURGERY
Physiotherapy Guidelines
This is a guideline for you physiotherapist to help you progress through rehabilitation over the
course of 12 weeks following your knee operation. A physiotherapist who is experienced in knee
rehabilitation should be consulted throughout the programme to supervise and where necessary
individually modify your programme.
Aims of Rehabilitation
To restore Range of Motion and Strength to the knee.
The final goal is to minimize knee pain and improve your knee function to improve your quality of
life.
Type of Replacement Performed
Total Knee Replacement
Unicompartmental Knee Replacement
Medial
Lateral
Patello-femoral
Post Operative Programme
1-14 Days
Manual Physiotherapy
Intermittent cryotherapy to minimize joint swelling over first 4-5 days.
Cryotherapy after exercises. Heat packs may be used on the knee and thigh prior to
exercises.
Circumferential compression dressing (Tubigrip) from ankle to thigh.
Elevate the affected limb to minimize swelling.
Ankle exercises for DVT prophylaxis.
Deep breathing exercises for basal atelectasis.
This letter is written both as a courtesy and in confidence to assist in the assessment and management of a referred patient. This letter must
not be copied to any third party, including the patient or anyone nominated by the patient, without the express permission of The Author.
Unauthorised publication of this letter would be a breach of The Authors copyright.
Range of Motion / Strengthening Exercises
Quadriceps sets, Gluteal sets.
Straight leg raises, supine.
Knee extensions supine over a roll.
Knee extensions from seated
Passive knee straightening with a heel roll supine.
Heel slides, seated and supine.
Functional Exercises
Transfer lying to standing, and seated to standing.
Gait training with crutches, including stairs.
Into and out of a car.
Weight bear as tolerated.
7-12 weeks
Manual Physiotherapy
Patellar mobilization exercises.
Quads and hamstrings deep tissue massage.
Wound massage with Bio-oil or Vitamin E cream.
Range of Motion / Strengthening Exercises
Core stabilization exercises.
Squats and single leg stance mini-squats.
Resistance exercises for quadriceps, hamstrings, gluteals and adductors.
Active and assisted ROM exercises.
Functional Exercises
Start driving using the affected leg.
Gait supervision without walking aids.
Lateral stepping.
Heel-toe walking.
Exercise bike (can start earlier if good balance).
3-6 weeks
Manual Physiotherapy
Cryotherapy after exercises, heat packs may be used on the knee and thigh prior to
exercises.
Circumferential compression dressing (Tubigrip) from ankle to thigh.
Ankle exercises for DVT prophylaxis.
Patellar mobilization exercises.
Quads and hamstrings deep tissue massage.
Range of Motion / Strengthening Exercises
Isometric quads, hamstrings, gluteals, adductors.
Core stabilizing exercises.
Active and assisted range of motion exercises.
Supported standing heel raises, calf stretches, mini squats, hamstring curls.
Hydrotherapy after week 3.
Functional Activities
Gait normalize gait between crutches, progressing to a single point stick.
Weight bearing as tolerated.
Increase endurance with longer walks and stairs.
Patients should be walking without aids and achieving flexion >90 by 6 weeks post-operation
13+ weeks
Training for Life
Once the patient has achieved full extension and flexion >110, normalized and unaided gait,
and good muscle balance institute an ongoing programme of regular exercise tailored to the
patient.
This may include:
Regular walking
Exercise bike
Hydrotherapy
Gentle gym workouts
Return to sport (golf, doubles tennis, lawn bowls, etc)
Encourage the patient to continue their exercise program indefinitely, to optimize the outcome
from their surgery.
You might also like
- Distal Biceps Repair Rehabilitation Protocol by Tendayi MutsopotsiDocument5 pagesDistal Biceps Repair Rehabilitation Protocol by Tendayi MutsopotsiPhysiotherapy Care SpecialistsNo ratings yet
- Achilles Tendon Rupture 0Document15 pagesAchilles Tendon Rupture 0Usman JabbarNo ratings yet
- Shoulder Post-Operative Rehabilitation ProtocolsDocument6 pagesShoulder Post-Operative Rehabilitation ProtocolsShrutiNo ratings yet
- ACL Reconstruction: Patellar Tendon Graft/Hamstring Tendon GraftDocument6 pagesACL Reconstruction: Patellar Tendon Graft/Hamstring Tendon GraftArun TamilvananNo ratings yet
- ACL Reconstruction Rehabilitation ProtocolDocument11 pagesACL Reconstruction Rehabilitation ProtocolNijin XmxNo ratings yet
- Pages - ACL W Meniscus Repair ProtocolDocument3 pagesPages - ACL W Meniscus Repair ProtocolSunit AroraNo ratings yet
- The Whartons' Strength Book: Lower Body: Total Stability for Upper Legs, Hips, Trunk, Lower Legs, Ankles, and FeetFrom EverandThe Whartons' Strength Book: Lower Body: Total Stability for Upper Legs, Hips, Trunk, Lower Legs, Ankles, and FeetRating: 3 out of 5 stars3/5 (3)
- Tennis Elbow ExerciseDocument2 pagesTennis Elbow Exercisedhirajkumar_1No ratings yet
- Ankle Fracture Rehab ProtocolDocument6 pagesAnkle Fracture Rehab Protocolbmj123No ratings yet
- Rehabilitation: Walking After Total Knee ReplacementDocument10 pagesRehabilitation: Walking After Total Knee ReplacementSandeep DhimanNo ratings yet
- Total Knee Arthroplasty PDFDocument10 pagesTotal Knee Arthroplasty PDFBhargav DaveNo ratings yet
- HO13 Oct 2007 Exercise SheetDocument2 pagesHO13 Oct 2007 Exercise SheetbendeniNo ratings yet
- Rotator CuffDocument4 pagesRotator Cuffcaldaseletronica280No ratings yet
- Medial Collateral Ligament Injury MCL Rehabilitation Yale 240271 28716Document8 pagesMedial Collateral Ligament Injury MCL Rehabilitation Yale 240271 28716Raluca Alexandra PlescaNo ratings yet
- Rehabilitation Protocol For Meniscus RepairDocument16 pagesRehabilitation Protocol For Meniscus RepairAnonymous ecI8GUbaNo ratings yet
- Exercise your way to health: Arthritis: Exercise plans to improve your lifeFrom EverandExercise your way to health: Arthritis: Exercise plans to improve your lifeNo ratings yet
- USM Student Research on Conservative Meniscus RehabilitationDocument2 pagesUSM Student Research on Conservative Meniscus RehabilitationShahroz Khan100% (1)
- ChondromalaciaDocument1 pageChondromalaciaricardox28No ratings yet
- PHTH 302 Exercises For Lumbar Instability PresentationDocument21 pagesPHTH 302 Exercises For Lumbar Instability Presentationmanx100% (1)
- GWS Total Hip ReplacementDocument17 pagesGWS Total Hip ReplacementRadu MoglanNo ratings yet
- Frozen Shoulder - Adhesive Capsulitis - OrthoInfo - AAOSDocument6 pagesFrozen Shoulder - Adhesive Capsulitis - OrthoInfo - AAOSpempekplgNo ratings yet
- Osgood Schlatter Disease With Exercises ChocDocument4 pagesOsgood Schlatter Disease With Exercises ChocJoni MokodoNo ratings yet
- ACL Rehab Guidelines for Early Range of Motion and StrengtheningDocument4 pagesACL Rehab Guidelines for Early Range of Motion and Strengtheningfia0711No ratings yet
- Grade 4 Chondromalacia Patella TreatmentDocument3 pagesGrade 4 Chondromalacia Patella TreatmentTroy0% (1)
- Passive MovementsDocument1 pagePassive MovementsomhreemaimhreemNo ratings yet
- ESWT - For Myositis Ossificans CaseDocument13 pagesESWT - For Myositis Ossificans CaseSienriesta NovianaNo ratings yet
- PCL Reconstruction Rehab ProtocolDocument19 pagesPCL Reconstruction Rehab ProtocolosamadrNo ratings yet
- Cervical Spine EvaluationDocument9 pagesCervical Spine EvaluationS.Muhaymen HussainNo ratings yet
- Ankle Sprains: If Your Symptoms Do Not Resolve Within 2-4 Weeks Please Contact Your ClinicianDocument2 pagesAnkle Sprains: If Your Symptoms Do Not Resolve Within 2-4 Weeks Please Contact Your ClinicianAndrei R LupuNo ratings yet
- Grade One Ankle Sprain Recovery TimeDocument4 pagesGrade One Ankle Sprain Recovery TimeMattNo ratings yet
- Self Management - Hip Muscle TrainingDocument2 pagesSelf Management - Hip Muscle Trainingfarrelly14100% (2)
- Biomechanics of The Knee During Closed Kinetic Chain ExercisesDocument31 pagesBiomechanics of The Knee During Closed Kinetic Chain ExercisesJean SantosNo ratings yet
- Introduction PhysiotherapistDocument12 pagesIntroduction Physiotherapistapi-371068989No ratings yet
- ACL Repair-HAMSTRING Graft ProtocolDocument4 pagesACL Repair-HAMSTRING Graft ProtocolmishbehavedNo ratings yet
- Prosthetic Case PresentationsDocument19 pagesProsthetic Case PresentationsptannenbaumNo ratings yet
- Ijspt-Biomechanics and Pathomechanics of The Patellofemoral JointDocument11 pagesIjspt-Biomechanics and Pathomechanics of The Patellofemoral JointDevi MigiekaNo ratings yet
- Liebenson - Functional Training Handbook ReviewDocument3 pagesLiebenson - Functional Training Handbook ReviewJoaoPncs SilvaNo ratings yet
- ACL Reconstruction PhysiotherapyDocument20 pagesACL Reconstruction Physiotherapyking4lifeNo ratings yet
- Shoulder ArthroplastyDocument53 pagesShoulder ArthroplastyWijaya X PutriNo ratings yet
- Oswestry Disability IndexDocument4 pagesOswestry Disability Indexpaulina_810No ratings yet
- Acl Rehab ProgrammeDocument8 pagesAcl Rehab ProgrammePengintaiNo ratings yet
- 9 Pregnancy Stretches For The Whole Body 4 Pager Apr17 v3Document4 pages9 Pregnancy Stretches For The Whole Body 4 Pager Apr17 v3LeiltonNo ratings yet
- SCIATICA EXERCISES Functional BestDocument3 pagesSCIATICA EXERCISES Functional BestMellow Moon RecordsNo ratings yet
- Suspension Therapy: DPT, Semester 2Document16 pagesSuspension Therapy: DPT, Semester 2Fatima SeharNo ratings yet
- Taping For Knee OsteoarthritisDocument9 pagesTaping For Knee OsteoarthritisLinda SugiartoNo ratings yet
- Physiotherapy Exercises Following Transfemoral (Above Knee) AmputationDocument5 pagesPhysiotherapy Exercises Following Transfemoral (Above Knee) AmputationLuqmanul HakimNo ratings yet
- 891 Paediatric Idiopathic FlatfootDocument12 pages891 Paediatric Idiopathic FlatfootRobertus Dwi AtmokoNo ratings yet
- Free Exercise Guide For Physiotherapy StudentsDocument14 pagesFree Exercise Guide For Physiotherapy StudentssenthilkumarNo ratings yet
- Chondromalacia Patella RehabDocument1 pageChondromalacia Patella Rehabjntownsend3404No ratings yet
- Hemiarthroplasty Hip - Apr20Document10 pagesHemiarthroplasty Hip - Apr20Shalu OjhaNo ratings yet
- Shoulder Special TestsDocument36 pagesShoulder Special TestsNidal HusseinNo ratings yet
- Rehabilitation protocol for mallet finger and zone injuriesDocument18 pagesRehabilitation protocol for mallet finger and zone injuriesaparnaNo ratings yet
- Physiotherapy in Disaster MenegementDocument82 pagesPhysiotherapy in Disaster MenegementAtiKa YuLiantiNo ratings yet
- Biomechanics of Elbow JointDocument10 pagesBiomechanics of Elbow JointGeddam SnehalathaNo ratings yet
- Shoulder Dislocation Factsheet: Exercises and Recovery TipsDocument2 pagesShoulder Dislocation Factsheet: Exercises and Recovery TipscilengsaiNo ratings yet
- Physical Therapy in Sport: Ryan Lobb, Steve Tumilty, Leica S. ClaydonDocument9 pagesPhysical Therapy in Sport: Ryan Lobb, Steve Tumilty, Leica S. Claydonilona ilincaNo ratings yet
- Neck PainDocument1 pageNeck PainHasan RahmanNo ratings yet
- SCALE-Selective Control Assesment PDFDocument3 pagesSCALE-Selective Control Assesment PDFjinil raj j.r.No ratings yet
- McKenzie Classification of Mechanical Spinal PainDocument7 pagesMcKenzie Classification of Mechanical Spinal PainVictor Andrés Olivares Ibarra100% (2)
- Miller 2015Document8 pagesMiller 2015Shaun TylerNo ratings yet
- General Fitness 5Document13 pagesGeneral Fitness 5Shaun TylerNo ratings yet
- 2021 Article 364Document28 pages2021 Article 364Shaun TylerNo ratings yet
- Muscular Strategy Shift in Human Running: Dependence of Running Speed On Hip and Ankle Muscle PerformanceDocument14 pagesMuscular Strategy Shift in Human Running: Dependence of Running Speed On Hip and Ankle Muscle PerformanceShaun TylerNo ratings yet
- Breakingmuscle-Bodyweight Workout Cycle 2Document9 pagesBreakingmuscle-Bodyweight Workout Cycle 2Shaun TylerNo ratings yet
- Modeling Overuse Injuries in Sport As A Mechanical Fatigue PhenomenonDocument8 pagesModeling Overuse Injuries in Sport As A Mechanical Fatigue PhenomenonShaun TylerNo ratings yet
- Training PlanDocument5 pagesTraining PlanShaun TylerNo ratings yet
- Breakingmuscle-Bodyweight Workout Cycle 1Document14 pagesBreakingmuscle-Bodyweight Workout Cycle 1sumopandianNo ratings yet
- VVKJVJVJVJVDocument27 pagesVVKJVJVJVJVAbhishekDashNo ratings yet
- Ganderton 2015Document2 pagesGanderton 2015Shaun TylerNo ratings yet
- Cervical Zygapophysial Joint Pain MapsDocument10 pagesCervical Zygapophysial Joint Pain MapsthiagoNo ratings yet
- Garca-Pinillos2020 IJSPPDocument8 pagesGarca-Pinillos2020 IJSPPShaun TylerNo ratings yet
- Rathmell2008 2Document12 pagesRathmell2008 2Shaun TylerNo ratings yet
- Diagnosis and Treatment of Sciatica2Document6 pagesDiagnosis and Treatment of Sciatica2Hayyu F RachmadhanNo ratings yet
- Physiotherapy Management of SciaticaDocument6 pagesPhysiotherapy Management of SciaticaMuly Arafah ZakariaNo ratings yet
- 311-Article Text-307-1-10-20140612Document6 pages311-Article Text-307-1-10-20140612Shaun TylerNo ratings yet
- Osteochondroma 02Document5 pagesOsteochondroma 02Shaun TylerNo ratings yet
- 2015 - 03 - 26 NEJM SciaticaDocument9 pages2015 - 03 - 26 NEJM SciaticaShaun TylerNo ratings yet
- Hunter2019 PDFDocument15 pagesHunter2019 PDFCarlos Andrés BernalNo ratings yet
- The Five Diaphragms in Osteopathic Manipulative MeDocument14 pagesThe Five Diaphragms in Osteopathic Manipulative MeShaun Tyler100% (1)
- Foot and Ankle Biomechanics in Walking And.3Document7 pagesFoot and Ankle Biomechanics in Walking And.3Shaun TylerNo ratings yet
- PT Alzheimer39s20DiseaseExercises AD10Document10 pagesPT Alzheimer39s20DiseaseExercises AD10Shaun TylerNo ratings yet
- What Treatment of Tendinopathy: Inflammation or Degeneration?Document4 pagesWhat Treatment of Tendinopathy: Inflammation or Degeneration?Shaun TylerNo ratings yet
- Early Versus Delayed Rehabilitation After Acute Mu PDFDocument3 pagesEarly Versus Delayed Rehabilitation After Acute Mu PDFShaun TylerNo ratings yet
- Musculoskeletal Science and PracticeDocument7 pagesMusculoskeletal Science and PracticeShaun TylerNo ratings yet
- Sports and Exercise MedicineDocument10 pagesSports and Exercise MedicineShaun TylerNo ratings yet
- Ryan - minimalistfootwearBJSM 2013Document8 pagesRyan - minimalistfootwearBJSM 2013Shaun TylerNo ratings yet
- Case History Form SummaryDocument4 pagesCase History Form SummaryShaun TylerNo ratings yet
- Snowboarding Injuries: LeadersDocument11 pagesSnowboarding Injuries: LeadersShaun TylerNo ratings yet
- Fitness to Practise Annual Report SummaryDocument18 pagesFitness to Practise Annual Report SummaryShaun TylerNo ratings yet
- Panduan IspaDocument170 pagesPanduan Ispameriza dahliaNo ratings yet
- SMCHS Boys Soccer Practice SessionsDocument57 pagesSMCHS Boys Soccer Practice SessionsSS Lazio100% (5)
- Business Communication - Iii: End Term Examination Trim - IiiDocument25 pagesBusiness Communication - Iii: End Term Examination Trim - IiiNSNo ratings yet
- BODYPUMP 100 Education Only - Print ReadyDocument5 pagesBODYPUMP 100 Education Only - Print ReadyNikolas MandilarasNo ratings yet
- Beat It Michael Jackson Base CompletaDocument3 pagesBeat It Michael Jackson Base CompletaBudachNo ratings yet
- Bai Tap Bo Tro Va Nang Cao Smart Start 3 Tap 2Document49 pagesBai Tap Bo Tro Va Nang Cao Smart Start 3 Tap 2hanh nguyenNo ratings yet
- SA ChannelsDocument5 pagesSA Channelsapi-3747040100% (2)
- Philosophy of Wing ChunDocument3 pagesPhilosophy of Wing Chungjh135No ratings yet
- Follow The Instructions For R.I.C.EDocument2 pagesFollow The Instructions For R.I.C.Eayatolla ayatollaTMNo ratings yet
- Newton's Law-WorksheetDocument1 pageNewton's Law-WorksheetJenniferNo ratings yet
- OKI Microline3320 Parts Katalog + Seznam SoučástekDocument11 pagesOKI Microline3320 Parts Katalog + Seznam SoučástekKlema HanisNo ratings yet
- Micro Merlin With HandbrakeDocument1 pageMicro Merlin With HandbrakeCarlos GutiérrezNo ratings yet
- Five Immortality Exercises From TibetDocument20 pagesFive Immortality Exercises From TibetJared Carpenter100% (1)
- Apca Tournament CalenderDocument9 pagesApca Tournament CalenderGopi KrishnaNo ratings yet
- Sparco Catalogue 2020 ENG PRICES LWDocument151 pagesSparco Catalogue 2020 ENG PRICES LWmarianNo ratings yet
- A World of Opportunities 18 03 22 (18187) X Ryan SummersDocument17 pagesA World of Opportunities 18 03 22 (18187) X Ryan SummersKumar Rao100% (1)
- Unit Plan - Pe Throwing and CatchingDocument11 pagesUnit Plan - Pe Throwing and Catchingapi-296784293100% (2)
- OPLS-DA Model DiagnosticsDocument44 pagesOPLS-DA Model DiagnosticshomeNo ratings yet
- Brunei Driving LicenceDocument18 pagesBrunei Driving Licenceapi-3051162580% (10)
- Materi Rom Untuk Ujian 1Document11 pagesMateri Rom Untuk Ujian 1Andy NuriyantoNo ratings yet
- Bharat RatnaDocument19 pagesBharat RatnaVenkatesh atmakuru100% (1)
- Soal Pas Bing 8 20212Document4 pagesSoal Pas Bing 8 20212Fitri Y UtiNo ratings yet
- Fitnessgram Student Report Accessible Version Name: Jane JoggerDocument3 pagesFitnessgram Student Report Accessible Version Name: Jane JoggermanasNo ratings yet
- PanzerBlitz Article IndexDocument65 pagesPanzerBlitz Article IndexBeagle75100% (2)
- Build a Dominant O-Line with Simple Schemes, Pride and TechniqueDocument25 pagesBuild a Dominant O-Line with Simple Schemes, Pride and TechniqueJJ Lawson83% (6)
- Describing Cristiano Ronaldo Kelas 7Document28 pagesDescribing Cristiano Ronaldo Kelas 7apud mahpudin0% (1)
- SBA Observation Checklist SAMPLESDocument4 pagesSBA Observation Checklist SAMPLESPincianna WilliamsNo ratings yet
- "Hot-Dogging Into History": How Modern Surfing Was Introduced To Australia.Document20 pages"Hot-Dogging Into History": How Modern Surfing Was Introduced To Australia.Martin DolheguyNo ratings yet
- Altec A Class Specifications: Standard Features OptionsDocument1 pageAltec A Class Specifications: Standard Features OptionsJorge RVNo ratings yet
- Leveling Guide from 1-85 in Lineage 2 ClassicDocument50 pagesLeveling Guide from 1-85 in Lineage 2 Classicanon_986224999No ratings yet