Professional Documents
Culture Documents
Intermittent Bolus Via Infracl
Uploaded by
andrew herringOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Intermittent Bolus Via Infracl
Uploaded by
andrew herringCopyright:
Available Formats
Can J Anesth/J Can Anesth (2014) 61:684685
DOI 10.1007/s12630-014-0172-3
CORRESPONDENCE
Intermittent bolus via infraclavicular nerve catheter using a
catheter-over-needle technique in a pediatric patient
Adam O. Spencer, MD Ban C. H. Tsui, MD
Received: 14 February 2014 / Accepted: 17 April 2014 / Published online: 6 May 2014
Canadian Anesthesiologists Society 2014
To the Editor,
Continuous peripheral nerve blocks (PNB) are
challenging to administer successfully in the pediatric
population due to the general uncooperative nature of
pediatric patients. Typically, catheters are placed
preoperatively under general anesthesia, putting the
anesthesiologist under time pressure to place the catheter
successfully and providing only one chance to place the
catheter since re-installation of a dislodged catheter
following surgery would require additional anesthesia.1
Postoperatively, there is an increased risk of PNB pumpcatheter systems being inadvertently detached upon
increased patient activity. A catheter-over-needle
technique has been used to place per neural catheters
successfully in adult patients.2,3 We describe a novel use of
the catheter-over-needle technique to administer a PNB
successfully in an anesthetized pediatric patient as well as
to manage postoperative pain effectively with intermittent
boluses of local anesthetic. Consent to describe this case
was provided by the patients parents.
A five-year-old 20-kg female presented for open-wedge
osteotomy and excision of approximately one-third of her
distal radius. Using an aseptic technique, an ultrasoundguided infraclavicular PNB was administered using an 18G
75-mm catheter-over-needle set (MultiSet UPK NanoLine
21156-40E, Pajunk, Germany) via an in-plane approach
(Figure A). Using a dosage regime similar to that
A. O. Spencer, MD
Department of Pediatric Anesthesiology, Alberta Childrens
Hospital, University of Calgary, Calgary, AB, Canada
B. C. H. Tsui, MD (&)
Department of Anesthesiology and Pain Medicine, University of
Alberta, Edmonton, AB, Canada
e-mail: btsui@ualberta.ca
123
previously reported for single-injection brachial plexus
block,4 a solution of 0.375% ropivacaine 6 mL was
injected between the axillary artery and the lateral cord.
After positioning the catheter tip posterior to the axillary
artery and the nerve (Figure B), an additional 6 mL of
solution were injected. The catheter was then fixed to the
patients anterior chest (Figure C).
Postoperatively, the patient was comfortable and had
complete sensory and motor block in all terminal nerve
distributions. About seven hours following the initial
injection of local anesthetic in the operating room, the
patient was comfortable with a visual analogue pain scale
score of 2/10 and showed complete sensory block for all
peripheral nerves and partial motor blockade of the
musculocutaneous nerve. Full motor function of the rest
of the peripheral nerves was observed. At this time, a bolus
of 0.2% ropivacaine 7.5 mL was given pre-emptively for
pain. The patient also received scheduled doses of oral
acetaminophen and intravenous ketorolac. Twenty-four
hours after the first postoperative bolus, the patient was
comfortable with full motor function. A second bolus of
0.2% ropivacaine 3.5 mL was administered, and the
catheter was removed. The patient was discharged four
hours later without complications.
As shown previously in adults,2,3 the catheter-overneedle method offers improved ease of use and increased
stability and flexibility compared with traditional designs.
Importantly, the catheter-over-needle technique closely
resembles the straightforward act of placing an intravenous
catheter and features no additional steps compared with the
single-injection technique. This is particularly relevant
since PNB in anesthetized children usually involves time
pressure when performing blocks in the operating room. In
this case, the operator (A.S.) had limited experience with
the catheter-over-needle assembly yet was able to perform
Intermittent bolus via infraclavicular nerve catheter
685
In children, single-injection infraclavicular blocks
provide four to six hours of analgesia,4 suggesting that an
intermittent bolus technique is a viable and feasible option.
We have administered successful supraclavicular blocks in
adults using this technique,2 and intermittent bolusing for
axillary block was shown to provide effective analgesia
and motor block with lower plasma levels of local
anesthetic when compared with continuous infusion.5 The
intermittent bolus method eliminates the need for
physically connecting the catheter to a pump, making this
option attractive in pediatric practice since the patients
increased activity heightens the risk of the catheter being
pulled out inadvertently.
This case serves to remind clinicians that intermittent
bolusing via a perineural catheter can be a plausible and
effective alternative to continuous infusion. It also alerts
pediatric anesthesiologists to the recent success of the
catheter-over-needle method in the adult population and its
easy adaptation for pediatric use.
Acknowledgement The authors thank Dr. Gareth Corry for
assistance with the article.
Funding Ban Tsui is supported by a Clinical Scholar Award from
the Alberta Heritage Foundation for Medical Research (AHFMR) and
a CAS/Abbott Laboratories Career Scientist Award from the
Canadian Anesthesiologists Society.
Conflict of interest The Pajunk MultiSet 211156-40E is modified
and re-designed by Ban Tsui. Dr. Tsui also has a patent-licensing
agreement with Pajunk.
References
Figure Ultrasound-guided infraclavicular block. A) In-plane
insertion of catheter-over-needle unit. B) Catheter position after
securing to patient. C) Ultrasound image showing needle position
relative to brachial plexus (L = lateral cord; P = posterior cord;
M = medial cord) and axillary artery (AA) prior to injection of
second 7-mL bolus of local anesthetic (see text). The catheter-overneedle unit is indicated by arrowheads
the PNB quickly (less than ten minutes) and efficiently,
avoiding delay of surgery. Due to the fixed length of the
outer catheter, it is important to pre-determine the depth of
the target structure and to select an appropriate catheterover-needle set based on the ultrasound finding.
1. Dadure C, Bringuier S, Raux O, et al. Continuous peripheral nerve
blocks for postoperative analgesia in children: feasibility and side
effects in a cohort study of 339 catheters. Can J Anesth 2009; 56:
843-50.
2. Ip VH, Tsui BC. The catheter-over-needle assembly facilitates
delivery of a second local anesthetic bolus to prolong
supraclavicular brachial plexus block without time-consuming
catheterization steps: a randomized controlled study. Can J Anesth
2013; 60: 692-9.
3. Shakespeare TJ, Tsui BC. Catheter-over-needle method facilitates
effective continuous infraclavicular block. Can J Anesth 2013; 60:
948-9.
4. Fleischmann E, Marhofer P, Greher M, Waltl B, Sitzwohl C,
Kapral S. Brachial plexus anaesthesia in children: lateral
infraclavicular vs axillary approach. Paediatr Anaesth 2003; 13:
103-8.
5. Mezzatesta JP, Scott DA, Schweitzer SA, Selander DE. Continuous
axillary brachial plexus block for postoperative pain relief.
Intermittent bolus versus continuous infusion. Reg Anesth 1997;
22: 357-62.
123
You might also like
- Current Techniques in Canine and Feline NeurosurgeryFrom EverandCurrent Techniques in Canine and Feline NeurosurgeryAndy ShoresNo ratings yet
- Continuous Pericapsular Nerve Group Block For Hip Surgery: A Case SeriesDocument17 pagesContinuous Pericapsular Nerve Group Block For Hip Surgery: A Case SeriesVivek Vishal SahNo ratings yet
- Percutaneous NephrolithotomyFrom EverandPercutaneous NephrolithotomyGuohua ZengNo ratings yet
- My Published Paper 6, AnesthesiaDocument5 pagesMy Published Paper 6, Anesthesiamir sahirNo ratings yet
- (10920684 - Neurosurgical Focus) Percutaneous Pedicle Screw Fixation of The Lumbar SpineDocument9 pages(10920684 - Neurosurgical Focus) Percutaneous Pedicle Screw Fixation of The Lumbar Spineefancoolhand09No ratings yet
- J Wneu 2019 05 148Document11 pagesJ Wneu 2019 05 148Cristian OñateNo ratings yet
- TUBİTAKDocument8 pagesTUBİTAKAYŞE GÜLŞAH ATASEVERNo ratings yet
- Comparison of Ultrasound-Guided Thoracic Paravertebral and Pectoralis Interfascial Plane Block For Modified Radical MastectomyDocument7 pagesComparison of Ultrasound-Guided Thoracic Paravertebral and Pectoralis Interfascial Plane Block For Modified Radical MastectomyIJAR JOURNALNo ratings yet
- 4 IndianJAnaesth617581-2226112 - 061101Document6 pages4 IndianJAnaesth617581-2226112 - 061101Mythology KingdomNo ratings yet
- Yoshida Proximal Obturator Nerve BlockDocument7 pagesYoshida Proximal Obturator Nerve BlockFACULTY FOLDERSNo ratings yet
- Rib Fracture SerratusDocument3 pagesRib Fracture Serratusandrew herring100% (1)
- Research ProposalDocument12 pagesResearch ProposalLeanne Prosser Pizarro100% (2)
- CombinedDocument3 pagesCombinedSolape Akin-WilliamsNo ratings yet
- The Erector Spinae Plane Block For Effective.9Document4 pagesThe Erector Spinae Plane Block For Effective.9Rully ZenNo ratings yet
- 14Document10 pages14Juliana ObandoNo ratings yet
- 4 Arthroscopic Bankart Repair With Inferior To Superior Capsular Shift in Lateral Decubitus Position 1723226228Document6 pages4 Arthroscopic Bankart Repair With Inferior To Superior Capsular Shift in Lateral Decubitus Position 1723226228César ArveláezNo ratings yet
- Comparison of Two Approaches ofDocument96 pagesComparison of Two Approaches ofJacob OrtizNo ratings yet
- Touhy y CateterDocument8 pagesTouhy y CateterhumildementeanestesiosNo ratings yet
- Ultrasound-Guided Truncal Blocks For PerioperativeDocument15 pagesUltrasound-Guided Truncal Blocks For PerioperativeRuxandra GrigorescuNo ratings yet
- Tsui CSF Lavage CJA 14Document4 pagesTsui CSF Lavage CJA 14Aida TantriNo ratings yet
- ACB Vs FIN NoninDocument12 pagesACB Vs FIN NoninLêQuangPhongNo ratings yet
- Spinal Anesthesia: Monica M. Mordecai and Sorin J. BrullDocument7 pagesSpinal Anesthesia: Monica M. Mordecai and Sorin J. Brulljaka purna yudhaNo ratings yet
- Thesis Protocol Submitted For Diplomate of National Board (DNB) in AnaesthesiologyDocument24 pagesThesis Protocol Submitted For Diplomate of National Board (DNB) in AnaesthesiologyPraveen KumarNo ratings yet
- Real-Time Ultrasound-Guided Paramedian Epidural Access: Evaluation of A Novel In-Plane TechniqueDocument10 pagesReal-Time Ultrasound-Guided Paramedian Epidural Access: Evaluation of A Novel In-Plane TechniqueANGELICANo ratings yet
- Research ArticleDocument7 pagesResearch Articlefm_askaNo ratings yet
- Modified Arthroscopic Latarjet Procedure: Suture-Button Fixation Achieves Excellent Remodeling at 3-Year Follow-UpDocument9 pagesModified Arthroscopic Latarjet Procedure: Suture-Button Fixation Achieves Excellent Remodeling at 3-Year Follow-UpFarida KhodjaNo ratings yet
- Local and Regional Anaesthesia in Children: T. C. K. Brown, R. L. Eyres and R. J. McdougallDocument0 pagesLocal and Regional Anaesthesia in Children: T. C. K. Brown, R. L. Eyres and R. J. McdougallmiqbaljuherNo ratings yet
- Regional AnalgesiaDocument5 pagesRegional AnalgesiajdjhdNo ratings yet
- ASA Regional AnesthesiaDocument10 pagesASA Regional Anesthesiayessy32lNo ratings yet
- Trans Versus Abdominis Plane BlockDocument7 pagesTrans Versus Abdominis Plane BlockIvette M. Carroll D.No ratings yet
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552No ratings yet
- Supraclavicular Brachial Plexus BlockDocument7 pagesSupraclavicular Brachial Plexus BlockFACULTY FOLDERSNo ratings yet
- Transcaruncular Double Injection Technique For Peribulbar Anesthesia in Vitreoretinal SurgeryDocument5 pagesTranscaruncular Double Injection Technique For Peribulbar Anesthesia in Vitreoretinal SurgeryanxNo ratings yet
- Rectus Sheath Vs TAP BlocksDocument6 pagesRectus Sheath Vs TAP BlocksMikeMacKinnon100% (1)
- Chapter-41 Nasojejunal Tube Placement: January 2016Document12 pagesChapter-41 Nasojejunal Tube Placement: January 2016Issa AbuzeidNo ratings yet
- [19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedDocument7 pages[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matchedBruno MañonNo ratings yet
- Revista Brasileira DE AnestesiologiaDocument9 pagesRevista Brasileira DE AnestesiologiayulianiNo ratings yet
- Ultrasound-Guided Interventions of The Cervical Spine and NervesDocument12 pagesUltrasound-Guided Interventions of The Cervical Spine and NervestriNo ratings yet
- Surgically Placed Rectus Sheath Catheters For Post-Laparotomy AnalgesiaDocument6 pagesSurgically Placed Rectus Sheath Catheters For Post-Laparotomy AnalgesiaKarthikNo ratings yet
- Journal of Clinical Anesthesia: Original ContributionDocument6 pagesJournal of Clinical Anesthesia: Original ContributionzaimmuhtarNo ratings yet
- TAP Vs QL CesareanDocument7 pagesTAP Vs QL CesareanEmmanuel FortalezaNo ratings yet
- Aaos 2010Document220 pagesAaos 2010Yusufa ArdyNo ratings yet
- 2013-Jessica Burgner-Debulking From Within A Robotic Steerable Cannula For Intracerebral Hemorrhage EvacuationDocument9 pages2013-Jessica Burgner-Debulking From Within A Robotic Steerable Cannula For Intracerebral Hemorrhage Evacuationitm.ggwpNo ratings yet
- Anaesthesia For Awake Craniotomy With Non-Invasive Positive Pressure VentilationDocument4 pagesAnaesthesia For Awake Craniotomy With Non-Invasive Positive Pressure VentilationsaframikdarhafisNo ratings yet
- Effective Volume of Ropivacaine 0.75% Through A Catheter Required For Interscalene Brachial Plexus BlockadeDocument5 pagesEffective Volume of Ropivacaine 0.75% Through A Catheter Required For Interscalene Brachial Plexus BlockadeKarina Mega WNo ratings yet
- Original ArticleDocument8 pagesOriginal ArticleCelina Castañeda MartinezNo ratings yet
- Journal Review: Failed Spinal AnaesthesiaDocument61 pagesJournal Review: Failed Spinal Anaesthesiaferoza97100% (1)
- To Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesDocument4 pagesTo Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- ESPB As A Plan A Block - Endorsement by British AnaesDocument6 pagesESPB As A Plan A Block - Endorsement by British Anaesrandomaeiou7273No ratings yet
- The Use of Sphinkeeper® in Faecal IncontinenceDocument5 pagesThe Use of Sphinkeeper® in Faecal IncontinenceAthenaeum Scientific PublishersNo ratings yet
- Journal Reading 1Document6 pagesJournal Reading 1Mutivanya Inez MaharaniNo ratings yet
- IndianJPain 2021 35 3 254 334102Document3 pagesIndianJPain 2021 35 3 254 334102manoj majiNo ratings yet
- Difficult Intubation and Anesthetic Management in An Adult Patient With Undiagnosed Congenital Tracheal Stenosis: A Case ReportDocument6 pagesDifficult Intubation and Anesthetic Management in An Adult Patient With Undiagnosed Congenital Tracheal Stenosis: A Case ReportBianca CaterinalisendraNo ratings yet
- Role of Ultrsonography in Detecting The Location of Tip of Percutaneous Central Venous Catheters in Neonates at Hi-Tech Medical College and Hospital, BhubaneswarDocument5 pagesRole of Ultrsonography in Detecting The Location of Tip of Percutaneous Central Venous Catheters in Neonates at Hi-Tech Medical College and Hospital, BhubaneswarInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Caudal Anesthesia in PediatricDocument7 pagesCaudal Anesthesia in PediatricDavid PesireronNo ratings yet
- EJMCM - Volume 9 - Issue 2 - Pages 133-138Document6 pagesEJMCM - Volume 9 - Issue 2 - Pages 133-138Julio AltamiranoNo ratings yet
- Spinal Needle Stabilization Using A Hand Locking Maneuver With The Conventional Back-Eye Combined Spinal-Epidural SetDocument2 pagesSpinal Needle Stabilization Using A Hand Locking Maneuver With The Conventional Back-Eye Combined Spinal-Epidural SetMohammad HamidNo ratings yet
- IndianJAnaesth6311924-2183535 060355Document8 pagesIndianJAnaesth6311924-2183535 060355Abhijeet ThakurNo ratings yet
- Focus: Real-Time Ultrasound-Guided External Ventricular Drain Placement: Technical NoteDocument5 pagesFocus: Real-Time Ultrasound-Guided External Ventricular Drain Placement: Technical NoteOdiet RevenderNo ratings yet
- ImplantDocument11 pagesImplantElyes ElyesNo ratings yet
- K Opiods For Pain BupDocument2 pagesK Opiods For Pain Bupandrew herringNo ratings yet
- Original Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve BlockDocument7 pagesOriginal Article: Serratus Plane Block: A Novel Ultrasound-Guided Thoracic Wall Nerve Blockandrew herringNo ratings yet
- Roux 2013Document7 pagesRoux 2013andrew herringNo ratings yet
- Highland Guidelines - LDK 2013-2-15Document3 pagesHighland Guidelines - LDK 2013-2-15andrew herringNo ratings yet
- Buprenorphine 2016-7-18Document1 pageBuprenorphine 2016-7-18andrew herringNo ratings yet
- Rib Fracture SerratusDocument3 pagesRib Fracture Serratusandrew herring100% (1)
- Intravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-OperatóriaDocument6 pagesIntravenous Lidocaine To Treat Postoperative Pain : Lidocaína Intravenosa No Tratamento Da Dor Pós-Operatóriaandrew herringNo ratings yet
- Rib Fracture W: PecsDocument8 pagesRib Fracture W: Pecsandrew herring100% (1)
- 3.2.16.highland Emergency Medicine Journal Club Methods.2Document2 pages3.2.16.highland Emergency Medicine Journal Club Methods.2andrew herringNo ratings yet
- Herring ED Intractable Abdominal pain-N+VDocument1 pageHerring ED Intractable Abdominal pain-N+Vandrew herringNo ratings yet
- Dex For Dental Pain & SwellingDocument7 pagesDex For Dental Pain & Swellingandrew herring100% (1)
- CVS Action Plan v2Document1 pageCVS Action Plan v2andrew herringNo ratings yet
- Nej MR A 1511480Document9 pagesNej MR A 1511480Tohari Masidi AminNo ratings yet
- Ultrasound-Guided Block of TheDocument6 pagesUltrasound-Guided Block of Theandrew herringNo ratings yet
- Ketamine As Rescue Treatment FDocument8 pagesKetamine As Rescue Treatment Fandrew herringNo ratings yet
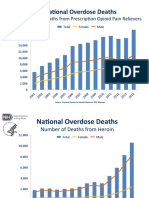
- OPR - Heroin DeathsDocument2 pagesOPR - Heroin Deathsandrew herringNo ratings yet
- Ultrasound Guided Interventional Procedures In.13Document14 pagesUltrasound Guided Interventional Procedures In.13andrew herring100% (1)
- Ultrasound Guided Interventional Procedures In.4Document13 pagesUltrasound Guided Interventional Procedures In.4andrew herringNo ratings yet
- NewspaperDocument2 pagesNewspaperbro nabsNo ratings yet
- ABS CBN CorporationDocument16 pagesABS CBN CorporationAlyssa BeatriceNo ratings yet
- Elaborare Modele de Rating in Conformitate Cu IFRS 9Document8 pagesElaborare Modele de Rating in Conformitate Cu IFRS 9MstefNo ratings yet
- Al Rafay ProfileDocument8 pagesAl Rafay ProfileRana UsmanNo ratings yet
- University of Dar Es Salaam: Faculty of Commerce and ManagementDocument37 pagesUniversity of Dar Es Salaam: Faculty of Commerce and ManagementEric MitegoNo ratings yet
- Dry Docking QuotationDocument4 pagesDry Docking Quotationboen jayme100% (1)
- 1422-Article Text-3684-1-10-20211104Document57 pages1422-Article Text-3684-1-10-20211104f.kpobi1473No ratings yet
- Russian Sec 2023-24Document2 pagesRussian Sec 2023-24Shivank PandeyNo ratings yet
- Post Market Surveillance SOPDocument8 pagesPost Market Surveillance SOPgopinathNo ratings yet
- Structure of An Atom Revision PaperDocument5 pagesStructure of An Atom Revision PaperZoe Kim ChinguwaNo ratings yet
- Platos Apology SummaryDocument3 pagesPlatos Apology SummaryFMSANo ratings yet
- Student Exploration: Magnetism (Find Gizmo Icon On Eclass)Document4 pagesStudent Exploration: Magnetism (Find Gizmo Icon On Eclass)Abdel Majeed Tuffaha0% (1)
- Assessment 3 Comparative Analysis Primary Vs Secondary SourcesDocument5 pagesAssessment 3 Comparative Analysis Primary Vs Secondary SourcesMATOZA, YLJOE V.No ratings yet
- Text Ranslation and TradicitonDocument283 pagesText Ranslation and TradicitonSCAF55100% (4)
- Neonatal Resuscitation ProgramDocument6 pagesNeonatal Resuscitation ProgramRick Frea100% (5)
- Olp Lesson PlanDocument2 pagesOlp Lesson Planapi-654865620No ratings yet
- Epri Guide For Transmission Line Groundingpdf PDF FreeDocument188 pagesEpri Guide For Transmission Line Groundingpdf PDF FreeHolman Wbeimar Suarez Niño100% (1)
- Altium Designer Training For Schematic Capture and PCB EditingDocument248 pagesAltium Designer Training For Schematic Capture and PCB EditingAntonio Dx80% (5)
- Ringleman Chart FlareDocument12 pagesRingleman Chart FlareguhadebasisNo ratings yet
- Data Processing and Management Information System (AvtoBərpaEdilmiş)Document6 pagesData Processing and Management Information System (AvtoBərpaEdilmiş)2304 Abhishek vermaNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaUlul Azmi Rumalutur NeinaNo ratings yet
- ScriptDocument12 pagesScriptWaleed Nadeem50% (2)
- Installation Manual of FirmwareDocument6 pagesInstallation Manual of FirmwareOmar Stalin Lucio RonNo ratings yet
- Optimizing Patient Flow: Innovation Series 2003Document16 pagesOptimizing Patient Flow: Innovation Series 2003Jeff SavageNo ratings yet
- Gunnar Fischer's Work On Ingmar Bergman's The Seventh Seal and Wild StrawberriesDocument6 pagesGunnar Fischer's Work On Ingmar Bergman's The Seventh Seal and Wild StrawberriesSaso Dimoski100% (1)
- Sekonic L 758Document68 pagesSekonic L 758mariosapereiraNo ratings yet
- Organization of Production: Test IiDocument7 pagesOrganization of Production: Test IiKamarul NizamNo ratings yet
- Final Project Part-3 Marketing PlanDocument8 pagesFinal Project Part-3 Marketing PlanIam TwinStormsNo ratings yet
- Unpriced Proposed Renovation of Bugolobi Flat, Block C For Uganda Coffee Development AuthorityDocument39 pagesUnpriced Proposed Renovation of Bugolobi Flat, Block C For Uganda Coffee Development AuthoritynicolasNo ratings yet
- Unit 2: TransducerDocument24 pagesUnit 2: TransducerROYAL GAMER YTNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Breaking the Habit of Being YourselfFrom EverandBreaking the Habit of Being YourselfRating: 4.5 out of 5 stars4.5/5 (1459)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissFrom EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissRating: 4.5 out of 5 stars4.5/5 (82)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipFrom EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipRating: 4.5 out of 5 stars4.5/5 (1135)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Peaceful Sleep Hypnosis: Meditate & RelaxFrom EverandPeaceful Sleep Hypnosis: Meditate & RelaxRating: 4.5 out of 5 stars4.5/5 (143)
- 369: Manifesting Through 369 and the Law of Attraction - METHODS, TECHNIQUES AND EXERCISESFrom Everand369: Manifesting Through 369 and the Law of Attraction - METHODS, TECHNIQUES AND EXERCISESRating: 5 out of 5 stars5/5 (50)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)



































![[19330715 - Journal of Neurosurgery_ Pediatrics] Comparative effectiveness of flexible versus rigid neuroendoscopy for endoscopic third ventriculostomy and choroid plexus cauterization_ a propensity score–matched](https://imgv2-1-f.scribdassets.com/img/document/722525723/149x198/0c84be9862/1712965550?v=1)