Professional Documents
Culture Documents
PPH
Uploaded by
GwEn LimCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PPH
Uploaded by
GwEn LimCopyright:
Available Formats
Color profile: Generic CMYK printer profile
Composite Default screen
44
SEPSIS AND POSTPARTUM HEMORRHAGE
B. Das and S. Clark
INTRODUCTION
Sepsis and postpartum hemorrhage are linked
by common predisposing factors, especially
considering that secondary postpartum hemorrhage can follow infection of retained placenta
or endometrium. Depending on the extent and
severity of the condition, postpartum uterine
infection is designated as postpartum endometritis, endomyometritis or parametritis.
Postpartum endometritis may be divided into
early-onset disease, occurring within the first
48 h, and late-onset disease, presenting up to
6 weeks postpartum. This chapter reviews the
causes, pathogenesis and management of
uterine sepsis.
CLINICAL RISK FACTORS
The most critical factor is the route of delivery.
After vaginal delivery, the incidence of postpartum endometritis varies between 0.9 and
3.9%, but can increase to 1251% after Cesarean section. Factors such as duration of labor,
bacterial vaginosis and vaginal interventions
are secondary predictors of post-Cesarean
endometritis. Early rupture of the membranes,
mid-forceps delivery, poor maternal health and
soft tissue trauma act as relative risk factors for
uterine sepsis, although they are not present
in most patients with such infections1. Indigent parturients are at higher risk of developing
postpartum endometritis.
ETIOLOGICAL AGENTS
Postpartum uterine sepsis is thought to arise
from an ascending infection caused by colonizing vaginal flora. Etiological agents include both
aerobic and anaerobic micro-organisms and
may consist of peptostreptococci, bacteroides,
streptococci, enterococci and E. coli. Group A
streptococcal endometritis, a rare cause in
developed countries, usually occurs in earlyonset disease (within the first 48 h of delivery),
often with high temperature > 39C (102.2F).
In contrast, Chlamydia trachomatis is involved
with late-onset disease (from 2 days up to
6 weeks postpartum) in patients who deliver
vaginally.
CLINICAL FEATURES AND
INVESTIGATIONS
Postpartum endometritis is diagnosed by significant pyrexia associated with uterine tenderness
or abnormal lochia in absence of other obvious
sources of infection. Significant pyrexia is
defined as oral temperature of 38.5C
(101.3F) or higher in the first 24 h after delivery or 38C (100.4F) or higher, for at least 4
consecutive hours, in the first 24 or more hours
after delivery. The first manifestation of fever
may occur at night2,3. Uterine sepsis associated
with late-onset disease and secondary postpartum hemorrhage usually presents as fever
on days 1012 after delivery.
Patients with suspected postpartum endometritis should have early clinical evaluation
including bimanual pelvic examination to determine size, consistency and tenderness of the
uterus and to detect any adnexal mass (ultrasound study may help, if available). Cesarean
section/episiotomy wounds should be assessed
for evidence of surgical site infection. Unremitting pain at the operative site may indicate
necrotizing fasciitis, wherein urgent debridement is life-saving3. A distant site of infection,
e.g. urinary or respiratory tract, should be ruled
out.
404
426
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:25:09
Color profile: Generic CMYK printer profile
Composite Default screen
Sepsis and postpartum hemorrhage
Laboratory investigations (where facilities are
available) include full blood count, transcervical
cultures (aerobic and anaerobic) and one set of
blood cultures, remembering that only 1020%
of patients with postpartum endometritis have
bacteremia. The presence of bacteremia does
not predict severity of infection or prolonged
recovery. Transcervical cultures, although difficult to interpret because of contamination with
vaginal flora, are helpful in those patients in
whom initial therapy fails. Whenever possible,
culture/antigen tests for chlamydia should be
performed in patients with late-onset disease or
those who are at high risk for acquisition of such
infections.
ANTIBIOTIC THERAPY AND
FURTHER MANAGEMENT
The aim of the antibiotics should be to provide
bactericidal cover for aerobic Gram-positive
cocci, Gram-negative bacilli and -lactamaseproducing anaerobes. Those antibiotics which
have been used for prophylaxis should be
avoided. Empirical treatment should be commenced as soon as possible. Parental treatment
with once-daily intravenous gentamicin and
intravenous clindamycin is an effective combination, especially in post-Cesarean section
patients and those awaiting surgical interventions, including removal of retained
placenta. Gentamicin levels need to be monitored. However, other alternatives, including
extended-spectrum penicillins or secondgeneration cephalosporins (cefoxitin), have
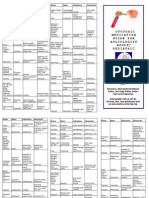
Table 1
been used, albeit with greater failure rates than
the combination of gentamicin and clindamycin4. Alternative antibiotic regimens are shown
in Table 1. Intravenous clindamycin and intravenous once-daily gentamicin are the cheapest
of the antibiotic regimen options, an important
issue in countries with restricted resources.
Parental therapy is continued until the
patient is pain-free, afebrile for 2448 h, the
leukocyte count returns to normal, and oral
liquids and solids are tolerated. There is no
need to continue with oral antibiotics after stopping parental treatment. Patients with positive
cultures for chlamydia should receive a 7-day
course of azithromycin or doxycycline, even if
there is good response to the initial empirical
antibiotic regimen. Azithromycin and doxycycline, although good antichlamydial agents,
are bacteriostatic drugs and should not be
used as first-line antimicrobial agents to treat
endometritis.
Failure to respond to the initial antibiotic
regimen in 48 h or clinical deterioration
requires further clinical evaluation and investigations to rule out another site of infection and
complications (see Figure 1). The antibiotic
regimen needs to be altered, preferably after
reviewing transcervical culture and sensitivity
results (see Table 2).
PREVENTION OF UTERINE SEPSIS
Strategies to prevent uterine sepsis include
improved obstetric care and the use of prophylactic antibiotics in high-risk patients, as well as
Initial antibiotic therapy1,2,4
Day 1
1. Clindamycin 900 mg 8-hourly + intravenous gentamicin 5 mg/kg body weight* once daily
or
2. Intravenous piperacillintazobactam 4.75 g 6-hourly
or
3. Intravenous metronidazole 500 mg 8-hourly + intravenous gentamicin 5 mg/kg body weight* once daily
or
4. Ampicillinsulbactam 3.1 g 6-hourly + intravenous gentamicin 5 mg/kg body weight* once daily
*Monitor gentamicin level
405
427
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:25:09
Color profile: Generic CMYK printer profile
Composite Default screen
POSTPARTUM HEMORRHAGE
Day 1
Specimen collected:
transcervical swab for
aerobic organism and
chlamydia* blood
culture
Empirical antibiotics, e.g.
i.v. gentamicin + i.v.
clindamycin
Surgical intervention if
clinically relevent
*Specimen for Chlamydia trachomatis to be obtained on patients with:
(a) late onset of disease or
(b) high risk for acquisition of this infection
Day 3
Patient on empirical antibiotic
Febrile
Afebrile
Clinical evaluation
Continue i.v. antibiotics
until:
Rule out other source of infection
Patient afebrile 2448 h
Urine, wound swab for culture
Pain-free
and sensitivity (if facility available)
Normal cell count
Imaging surgical intervention
Altered antibiotic regimen (see
Table 2) or specific antimicrobial
therapy as per culture results, e.g.
i.v. benzyl penicillin and i.v.
clindamycin for Group A
streptococci
Figure 1 Flow chart of treatment regimens for patient with suspected uterine sepsis and postpartum
hemorrhage1,2,4
coverage of planned or emergency surgical
interventions. In areas with limited resources,
education with the emphasis on a clean environment and simple infection control measures like
hand-washing, cleaning the genital area, preferably with mild detergents/disinfectant, and
minimizing the number of vaginal examinations
all play an important role in reducing uterine
infection.
The risk of infection increases with postpartum hemorrhage especially if the blood loss
is greater than 1 liter. If uterine sepsis occurs,
406
428
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:25:10
Color profile: Generic CMYK printer profile
Composite Default screen
Sepsis and postpartum hemorrhage
Table 2
Altered antibiotic regimen1,4. In all cases, the therapy should ideally be guided by culture results
If the patient deteriorates or Day 3 onwards if patient continues to be febrile on initial regimen:
Initial antibiotic regimen + another antimicrobial agent = altered regimen
1. Intravenous clindamycin + intravenous gentamicin* + intravenous ampicillin 12 g 6-hourly
or
2. Intravenous piperacillintazobactam + intravenous gentamicin 5 mg/kg* once daily)
or
3. Intravenous metronidazole + intravenous gentamicin* + intravenous ampicillin 12 g 6-hourly
or
4. Intravenous ampicillinsulbactam + intravenous gentamicin intravenous metronidazole 500 mg/8 hourly
The choice of antibiotics in the altered regimen may be determined by transcervical isolates (where culture
facilities are available), cost and availability of antimicrobial agents.
*Monitor gentamicin levels
such hemorrhagic consequences can be devastating: collapse can lead to death, as discussed
elsewhere in this book. In many developing
countries, the majority of deliveries do not
occur in a facility with a skilled attendant.
Traditional birth attendants (TBAs) need to
recognize the consequences of delayed referral.
Local and international organizations that aim
to provide resources to educate TBAs, increase
access to skilled attendants and to facilities for
prompt care of postpartum hemorrhage and
sepsis all help to decrease maternal mortality in
these countries.
blood and a B-Lynch compression suture was
inserted to stay the continual bleeding. The
patient received a total of 7 units of blood and 4
units of fresh frozen plasma. The patient continued to be pyrexial, her white blood cell rose
from 10 000 to 25 000; lochia was offensive and
a transcervical swab grew E. coli and anaerobes.
She was therefore administered an intravenous
clindamycin and once-daily intravenous gentamicin regimen for uterine sepsis. Gentamicin
levels were regularly monitored and the patient
was discharged after 8 days intravenous therapy,
having being ambulant, afebrile and pain-free
for 48 h. The baby remained well.
CASE STUDY
A 28-year-old primigravida presented at 41/40
weeks with a history of prolonged latent phase
of labor. She underwent a Cesarean section as
she failed to respond to 8-h oxytocin infusion,
commenced after artificial rupture of the
membranes. Prior to the procedure, the patient
received intravenous cefuroxime and intravenous metronidazole as she was found to be
pyrexial (38.7C). At Cesarean section, she had
offensive grade 1 meconium liquor; the placental membranes were found to be adherent but
were successfully removed. A live baby with
good Apgar score was delivered; however, the
patient had primary postpartum hemorrhage
due to uterine atony. The patient lost 6 liters of
References
1. Mead PB. Infections of the female pelvis. In
Mandel GL, Bennet JE, Dolin R, eds. Principles
and Practice of Infectious Disease, 5th edn. Philadelphia: Churchill Livingstone 2000:123543
2. Ledger WJ. Post partum endometritis diagnosis
and treatment: a review. J Obstet Gynaecol Res
2003;29:36473
3. Goepfert AR, Guinn AA, Andrews WW, et al.
Necrotising fasciitis after caesarean delivery.
Obstet Gynecol 1997;89:40912
4. French LM, Smaill FM. Antibiotic regimens for
endometritis after delivery. Cochrane review,
2004. Cochrane Library. Chichester: John Wiley
& Sons
407
429
Z:\Sapiens Publishing\A5211 - Postpartum Hemorrhage\Make-up\Postpartum Hemorrhage - Voucher Proofs #T.vp
30 August 2006 14:25:10
You might also like
- Hypertension TyDocument57 pagesHypertension TyGwEn LimNo ratings yet
- Diabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyDocument24 pagesDiabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyGwEn LimNo ratings yet
- 10 Vissers High Risk Airway SlidesDocument50 pages10 Vissers High Risk Airway SlidesGwEn LimNo ratings yet
- Clinical Key-Nutrition Food Security and Health (NElson)Document14 pagesClinical Key-Nutrition Food Security and Health (NElson)GwEn LimNo ratings yet
- Clinical Hey-Academy of Nutrition and PaedriticDocument29 pagesClinical Hey-Academy of Nutrition and PaedriticGwEn LimNo ratings yet
- Clinical Hey - Nutrition, Immunity and InfectionDocument39 pagesClinical Hey - Nutrition, Immunity and InfectionGwEn LimNo ratings yet
- ClinicalKey-Acid Base DisorderDocument7 pagesClinicalKey-Acid Base DisorderGwEn LimNo ratings yet
- Clinical Manifestations and Diagnosis of Congenital Anomalies of The UterusDocument37 pagesClinical Manifestations and Diagnosis of Congenital Anomalies of The UterusGwEn LimNo ratings yet
- Banana Pancakes - JamieOliverDocument1 pageBanana Pancakes - JamieOliverGwEn LimNo ratings yet
- Ultrasound Examination in Obstetrics and GynecologyDocument15 pagesUltrasound Examination in Obstetrics and GynecologyGwEn LimNo ratings yet
- Gui 214 CPG0809Document11 pagesGui 214 CPG0809Dennis GuzmanNo ratings yet
- Management of Spontaneous Abortion - American Family PhysicianDocument8 pagesManagement of Spontaneous Abortion - American Family PhysicianGwEn LimNo ratings yet
- Meconium Aspiration SyndromeDocument4 pagesMeconium Aspiration SyndromeGwEn LimNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Antibiotics PDFDocument8 pagesAntibiotics PDFSarah JaneNo ratings yet
- SCNICU Starter PackDocument7 pagesSCNICU Starter PackALIF HAIQAL MOHD HUSSEINNo ratings yet
- Antibiotic (Bacteriostatic) DrugsDocument15 pagesAntibiotic (Bacteriostatic) DrugsVictor LeeNo ratings yet
- Antibiotics - Classification & Mode of Action PDFDocument8 pagesAntibiotics - Classification & Mode of Action PDFtarun paulNo ratings yet
- Clinical Guideline: Aminoglycoside: Recommendations For Use, Dosing and Monitoring Clinical GuidelineDocument16 pagesClinical Guideline: Aminoglycoside: Recommendations For Use, Dosing and Monitoring Clinical GuidelineVita LesielaNo ratings yet
- UKMi-Gentamicin InfoDocument4 pagesUKMi-Gentamicin InfoAmisha VastaniNo ratings yet
- Aminoglycoside Dosing GuidelinesDocument3 pagesAminoglycoside Dosing GuidelinesaeromintNo ratings yet
- Gentamicin Sulphate According To EP & USP Method: Aminoglycosides AntibioticsDocument6 pagesGentamicin Sulphate According To EP & USP Method: Aminoglycosides Antibioticsmilatul amaliaNo ratings yet
- IMCI Technical Update - Including ZNDocument45 pagesIMCI Technical Update - Including ZNTinnie :)No ratings yet
- Medicinal Chemistry - PenicillinDocument39 pagesMedicinal Chemistry - PenicillinV G Viju KumarNo ratings yet
- AminoglycosidesDocument41 pagesAminoglycosidesAshish NeupaneNo ratings yet
- Case Study About Cystic Fibrosis GeneDocument40 pagesCase Study About Cystic Fibrosis GeneEvora, Sichem D.No ratings yet
- Ototoxic GuideDocument2 pagesOtotoxic GuideCempaka Kusuma DewiNo ratings yet
- Peritonitis GuiaDocument28 pagesPeritonitis GuiaAndrea ClaudieNo ratings yet
- List of AntibioticsDocument10 pagesList of AntibioticsAia JavierNo ratings yet
- Vig A Mox EyedropsDocument10 pagesVig A Mox EyedropsPinguin SatuNo ratings yet
- Antibiotic Prophylaxis in Gustilo Grade I To III Open Fractures of The Lower LimbV5 - April18th2012Document1 pageAntibiotic Prophylaxis in Gustilo Grade I To III Open Fractures of The Lower LimbV5 - April18th2012Yopi ArdhiaswariNo ratings yet
- Antibiotics Chart 2Document10 pagesAntibiotics Chart 2Vee MendNo ratings yet
- Cloxacillin and inDocument6 pagesCloxacillin and inGabb CabigtingNo ratings yet
- Protein Synthesis InhibitorsDocument12 pagesProtein Synthesis InhibitorsNirav SharmaNo ratings yet
- Aminoglycoside Guidance Document 20200424Document6 pagesAminoglycoside Guidance Document 20200424Marcelo UGNo ratings yet
- DRUGS Initial StockDocument163 pagesDRUGS Initial StockdeasyNo ratings yet
- File1 146 1714383Document366 pagesFile1 146 1714383Mutiara SazkiaNo ratings yet
- Protein Synthesis Inhibitors 2Document25 pagesProtein Synthesis Inhibitors 2AliImadAlKhasakiNo ratings yet
- Grand Case PresentationDocument22 pagesGrand Case PresentationTekels Curtis100% (1)
- GentamicinDocument1 pageGentamicinreinaNo ratings yet
- GENTAMICIN SULFATE-gentamicin S Ulfate Ointment Perrigo New York IncDocument4 pagesGENTAMICIN SULFATE-gentamicin S Ulfate Ointment Perrigo New York IncRezki NafiNo ratings yet
- Drug Induced Acute Kidney Injury.19 PDFDocument14 pagesDrug Induced Acute Kidney Injury.19 PDFJose santos MembreñoNo ratings yet
- Medication ListDocument14 pagesMedication ListMarie LeyvaNo ratings yet
- 2.11 SEPTIC ABORTION AND SEPTIC SHOCK. M. Botes PDFDocument4 pages2.11 SEPTIC ABORTION AND SEPTIC SHOCK. M. Botes PDFteteh_thikeuNo ratings yet