Professional Documents
Culture Documents
Caesarean Section
Uploaded by
William SonyoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Caesarean Section
Uploaded by
William SonyoCopyright:
Available Formats
If printed, this document is only valid for the day of printing.
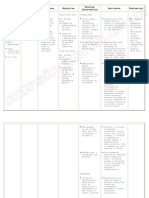
Caesarean Section (CS) Pre, Peri & Post-Op Care
Document Type
Function(s)
Health Service Group (HSG)
Department(s) affected
Patients affected (if applicable)
Staff members affected
Key words
Author role only
Owner (see ownership structure)
Edited by
Date first published
Date this version published
Date of next scheduled review
Unique Identifier
Guideline
Clinical Service Delivery
Womens Health
Maternity
Maternity patients requiring elective or acute
caesarean section
All ADHB clinicians in Womens Health and all LMC
access holders
Midwifery Educator
Clinical Director of Obstetrics
Clinical Policy Advisor
January 2001
May 2012
May 2018
NMP200/SSM/016
Contents
1. Purpose of guideline
2. Guideline management principles and goals
3. Abbreviations
4. Prioritisation of access to operating room
5. Medical preparation for acute procedure
6. Clerical preparation for acute procedure
7. Midwifery preparation for caesarean section
8. Midwife responsibility in operating room
9. Caesarean section category 1: extreme emergency flowchart
10. Caesarean section category 2 flowchart
11. Post natal care of the women following caesarean section
12. Supporting evidence
13. Associated ADHB documents
14. Disclaimer
15. Corrections and amendments
Caesarean Section May12.doc
Page 1 of 13
If printed, this document is only valid for the day of printing.
1. Purpose of guideline
This guideline establishes the assistance of obstetric, anaesthetic, midwifery and
support staff members in achieving best use of a limited operating room resource for
acute and elective caesarean sections within Auckland District Health Board (ADHB).
Back to Contents
2. Guideline management principles and goals
In this context, best includes appropriate prioritisation, efficiency, patient (mother and
baby) safety and best interests of those patients balanced against the needs of other
patients.
Nothing in this guideline is of itself intended to be a professional standard against
which individual performance can be assessed although external standards may be
referred to. It may however provide a framework for service audit.
At womens health, the Royal Australian and New Zealand College of Obstetricians
and Gynaecologists (RANZCOG) categories for urgency of access to OR for
caesarean sections should be utilised in determining the degree of expediency
required for a given birth and the relative need (one patient versus another) for
prioritising access to the OR.
Back to Contents
3. Abbreviations
CS
CTG
DDI
L&B
OR
PACU
SMO
caesarean section
cardiotocography
decision to delivery time
Labour and Birthing Suite
operating room
Post Anaesthetic Care Unit
senior medical officer
Back to Contents
Caesarean Section May12.doc
Page 2 of 13
If printed, this document is only valid for the day of printing.
4. Prioritisation of access to operating room
Categorisation of caesarean sections
The RANZCOG states that decision to delivery intervals (DDI) of 30 minutes, although
decreed as necessary in many legal judgements, seem based more on custom and
practice than on objective evidence in relation to condition of the newborn. The
categories developed by RANZCOG are:
Category 1: Immediate threat to the life of a woman or fetus;
Category 2: Maternal or fetal compromise but not immediately life threatening;
Category 3: Needing early delivery but no maternal or fetal compromise;
Category 4: At a time to suit the woman and the caesarean section team.
In line with RANZCOG recommendations, no specific time should be attached to the
various types of caesarean section. Each case should be managed according to the
clinical evidence of urgency, with every single case being considered on its merits. For
example, a category 2 caesarean section can become urgent if recurrent delays for
other emergencies in a labour ward repeatedly postpone surgery.
However, these recommendations should not be used to justify inadequate staffing or
resourcing of obstetric operating rooms.
For audit or other purposes, judgement on the appropriateness of DDIs should be
made on the basis of information available before birth, including available resources
at that time and not judged on the condition of the baby at birth.
See Associated ADHB documents section for the level 8 acute version.
Back to Contents
Caesarean Section May12.doc
Page 3 of 13
If printed, this document is only valid for the day of printing.
5. Medical preparation for acute procedure
Follow the steps below to prepare a woman for an acute procedure and to provide safe
care in the operating room. Tasks may be performed by any member of the team but
specific responsibilities are assigned.
Surgeon
i.
Ensure that appropriate intrauterine resuscitation measures are in place for both
the mother and the foetus as required while OR is being organised.
Clinical decision made for caesarean section by obstetric team in collaboration
with the woman, support person and LMC
The woman and partner receive adequate explanation about the operation and
procedure from the surgeon and the woman gives verbal informed consent
An interpreter may be required for consent, if time allows.
Agreement to Treatment form is completed by woman and surgeon unless
extreme emergency
Surgeon liaises with clinical charge midwife of L&B, and/or Oncall SMO of L&B
to allow safe coordination of care in the facility
ii. Document decision time in clinical record.
Notify anaesthetist and inform them of urgency, indication and co-existing
medical problems
You may require an Obstetric emergency Code in extreme emergencies
Complete Acute Surgical Booking form (CR2789) including obstetric urgency
category. Leave the acuity section of the form blank (see appendix re College
Statement)
Send form to OR co-coordinator via a medical member of the team
Complete indication as per audit sticker
Notify neonatal team
iii. Check Concerto for haematology and blood bank results:
If there are no current results, blood must be taken from the patient and sent to:
Blood bank for group and screen phone Blood bank if urgent
LabPLUS for FBC; use urgent form or phone blood bank and notify of
urgency.
If blood is required urgently:
Contact blood bank on ext. 24015 or ext. 24017
Notify blood bank staff members of the urgency of the request and required
products
If blood is required immediately and cross-matched or group specific blood is
not available request emergency O Rh(D) negative units be sent to the
ward/OR
*This responsibility may be delegated to another team member
Caesarean Section May12.doc
Page 4 of 13
If printed, this document is only valid for the day of printing.
Anaesthetist and surgeon
Ensure appropriate intrauterine resuscitation measures in place for both the mother
and the foetus if required while the section is being organised.
Anaesthetist
Discuss appropriate anaesthetic with surgeon, woman and support person
Complete Agreement to Treatment form, anaesthesia section with woman
Ensure that appropriate resource for OR is available including blood products
Back to Contents
6. Clerical preparation for acute procedure
Ward clerk
Print new labels for operating room
Notify the duty manager
Obtain a post natal bed
Back to Contents
7. Midwifery preparation for caesarean section
Midwife
i.
Ensure clinical record is complete with:
Front sheet
Patient labels
Registration form (CR0100)
Anaesthesia Record (CC4019)
Pre-Operative Assessment Record (CR4048)
Agreement to Treatment (CR111)
Epidural/Spinal Insertion Record (CR4039)
Labour and Birth Summary (CR3732)
Fluid Balance Record (CC4052)
Medication Chart (CR0452)
Newborn Record (CR3731)
Placenta Release form (CR2025)
ii. Prepare woman for the operating room:
ID bracelet correct
Nil by mouth
IV infusion commenced or continued and fluids administered as prescribed
Pre-operative medications are administered as prescribed
Caesarean Section May12.doc
Page 5 of 13
If printed, this document is only valid for the day of printing.
Insert in-dwelling urinary catheter (IDC) as time allows. For elective CS catheter
insertion in OR
Dress in operating room gown
Finger nail polish and hair clips removed
Rings and jewellery removed or taped, tongue studs removed
Check birth-care plan to ascertain whether woman wants placenta returned
Complete Placental Release form
Luggage to be locked in appropriate cupboard in L&B
For elective CS store safely in ward room, valuables in drug room
iii. In Emergency cases woman remains in labour room until operating room is
available:
Continue to monitor maternal vital signs
Continue to monitor fetal heart rate with continuous CTG
Cease Syntocinon infusion (unless for trial of instrumental birth)
Position the woman in left-lateral
Administer O2 via mask if clinically appropriate
iv. For elective CS:
Monitor maternal vital signs as necessary
Monitor fetal heart with CTG if required
v. On transfer to operating room via handover room, if appropriate midwife may:
Discontinue abdominal CTG monitoring (minimise unmonitored time)
Leave fetal scalp electrode in situ until in OR,
Bring CTG machine into OR
Pre-operative checklist completed and signed midwife and OR staff
Hand over to operating room nurse is completed
Surgical Safety Checklist sign in completed
vi. The OR Health Care assistant will assist the support person and show them where
to change into OR scrubs or if the woman is having a general Anaesthetic where to
sit and wait.
vii. Change into operating room attire;
Back to Contents
Caesarean Section May12.doc
Page 6 of 13
If printed, this document is only valid for the day of printing.
8. Midwifery responsibility in operating room
Support and assist in positioning the patient during insertion of spinal/epidural
anaesthetic.
For elective sections where appropriate fetal heart checked prior to and following
insertion of epidural/spinal anaesthesia. Document in clinical record
For emergency sections monitoring of the fetal heart is directed by the most senior
obstetric doctor present
If fetal scalp electrode is in situ continue CTG monitoring, otherwise monitor with
ultrasound or sonicaid as appropriate especially during insertion of epidural/spinal
anaesthesia. Document as appropriate in clinical records.
Remove fetal scalp electrode immediately prior to catheterising or prepping of the
skin
Assist with positioning of patient for catheterisation and surgery
Check resuscitaire
Support woman until time of birth
Assist neonatal staff members with the resuscitation and examination of the baby
as required
Ensure name bracelets (2) are checked with mother and are attached one on each
ankle
Initiate interaction and skin to skin contact between the parents and the baby as
soon as practicable and after agreement with the anaesthetist, surgeon, neonatal
staff members and the mother
Weigh baby at an appropriate time
The baby remains with the mother in the operating room under the care of a
midwife who is responsible for the babys safety
Discuss with operating room staff members appropriateness of the baby remaining
with the mother, if this is not possible the midwife should transfer the baby to the
postnatal ward
Complete documentation of the clinical record
Documentation
Ensure completion of forms:
Newborn Record (page one Prior to Birth)
Labour and Birthing Summary
Clinical records
Ensure Placenta disposal form is correct and completed
Completed Registration form handed to OR receptionist Monday Friday 0700
1500 hours. After hours labour and birthing unit ward clerk
Healthware data entry:
Electives entered by OR receptionist 0700hrs - 1500hrs Mon Friday. After hours
to be completed by L&B ward clerk or appropriate ward clerk
Caesarean Section May12.doc
Page 7 of 13
If printed, this document is only valid for the day of printing.
Acute caesarean sections entered by L&B ward clerk for LMCs otherwise
completed by core midwifery staff members
PACU
Midwifery handover of baby to PACU staff members
As appropriate midwife or PACU staff members to initiate breastfeeding with
mothers consent
If not on level 9, the midwife must remain with the woman for breastfeeding and for
postnatal observations and care (Fundus& blood loss)
Link to Caesarean section post anaesthesia care unit
Link to Newborn care in post anaesthesia care unit
Back to Contents
Caesarean Section May12.doc
Page 8 of 13
If printed, this document is only valid for the day of printing.
9. Caesarean section category 1: extreme emergency flowchart
Call an obstetric emergency (777)
Midwife/obstetric doctor
Remain in room
Commence intrauterine resuscitation
Discontinue syntocinon
Patient in full left lateral
IV fluids commence or increase
volume
Fetal monitoring continuously
Oxygen by face mask if required
Complete forms
CCM
Phone operating room coordinator
021471618
Reason for caesarean section
Room number and surgeon
At handover
Metalware yes no
Allergies (including Latex)
Blood group/antibody screen
Status of blood availability
Call neonatal team level 2 93 5536
Obstetrician and anaesthetist to discuss reason for caesarean and co-existing morbidity
Operating room co-coordinator will notify room when theatre ready and dispatch HCA
OR HCA will assist with transfer to operating room directly
Fetal heart record
For regional anaesthesia
Monitor with fetal scalp electrode
if attached
Listen continuously with sonicad
throughout procedure and
document
If appropriate use abdominal
trace
Fetal heart record
For general anaesthesia
Listen with sonicad prior to
prepping and document
There should no significant time
without fetal heart monitoring
Fetal condition to be continually communicated to anaesthetist
Back to Contents
Caesarean Section May12.doc
Page 9 of 13
If printed, this document is only valid for the day of printing.
10. Caesarean section category 2 flowchart
Decision for caesarean section made
Doctor notify:
Anaesthetist ph. 021924017
reason and comorbidity
Operating room coordinator ph.
021471618 with completed
booking form
Neonatal team appropriate level
Midwife notify:
CCM
Ward clerk
Complete forms
If fetal distress continue to EFM until transfer to operating room
Regional anaesthetic insitu
Regional yet to be placed
Top-up epidural in room
Continue EFM
When operating room ready then
discontinue monitoring for transfer
Listen to fetal heart with sonicaid prior
to prepping
If a delay use continuous monitoring
If
Continue to monitor with FSE or
sonicaid as appropriate
Listen prior to prepping
There should be no significant time
without fetal heart monitoring
deterioration in condition of the mother or the baby, obstetric doctor to discuss timing of delivery with anaesthetist
Back to Contents
Caesarean Section May12.doc
Page 10 of 13
If printed, this document is only valid for the day of printing.
11. Post natal care of the women following caesarean section
Midwife
The womens condition is assessed in the immediate post-operative period.
On collecting and returning to the post-natal area with the woman from the recovery
room:
Assess level of consciousness
Record BP, temperature and pulse
Check:
Redivac/s and record the amount and type of drainage
Intravenous infusion and site and checks the IV fluid prescription
PCA/PCEA prescription on pump
Dose of previous analgesia administered, level of pain and prescription for further
analgesia
Epidural site
Appropriate Venous Thromboprophylaxis prevention in place e.g. Flowtron, TEDs
Clexane
Oxygen administration and prescription if necessary
Patency of urinary catheter, colour and amount of urine
Wounds for ooze
Amount of lochia
Ecbolic prescription
If breastfeeding has been initiated
This initial assessment is documented in the clinical record, and the Postnatal
Observation Chart (CR420).
Optimum ventilation and haemodynamic status is maintained
Position the woman in the semi-recumbent position in the initial post-operative
period
Administer oxygen as per guideline
Record blood pressure, temperature and pulse half hourly for 4 hours or until
stable
Encourage deep breathing, coughing and leg exercises
Begin ambulation within 6 12 hours
Bonding between mother and baby
Assist with breastfeeding
Give mother-craft education as appropriate
If baby is in NICU or PIN:
Caesarean Section May12.doc
Page 11 of 13
If printed, this document is only valid for the day of printing.
Assist with establishing lactation
Ensure that the mother has a photograph of her baby
Reassure the mother and assist and encourage her to visit her baby regularly
Arrange adequate progress reports on the baby
Fluid and electrolyte balance is maintained
Administer the IV regime as prescribed and document on the Fluid Balance
Record (CC2384)
Ensure regular anti-emetics and sips of iced water are given for nausea
Record initial micturition following removal of indwelling catheter (normally 12
hours post delivery)
Catheterise the woman if she is unable to pass urine after 6 hours or bladder
palpable following removal of catheter
While indwelling catheter in situ measures urinary output on Fluid Balance
Record. The midwife notifies the obstetrician of any concerns re fluid balance
Comfort is maintained
Introduce ice and sips of water as tolerated by the woman
Introduce diet as desired
Evaluate location/type pain and administer analgesia as charted and assess
effectiveness
Assist with baby cares and feeding
Assist the woman to position herself whilst breastfeeding to maximise comfort
Patient anxiety is minimised
Obstetric team member to debrief with the women and talk about possibilities for
birth options with next pregnancy prior to discharge
Provide full explanations of all cares and procedures
Allow time for the woman and family to express fears/problems and to answer
any questions
Back to Contents
Caesarean Section May12.doc
Page 12 of 13
If printed, this document is only valid for the day of printing.
12. Supporting evidence
Royal Australian and New Zealand College of Obstetricians and Gynaecologists
(RANZCOG) - categories for urgency of access to OR for caesarean sections
Back to Contents
13. Associated ADHB documents
Bladder Care Postpartum & Urinary Retention Management
Caesarean Section (CS) - Acute - Management in Level 8 Operating Rooms
Caesarean Section (CS) - Post Anaesthesia Care Unit (PACU)
Count Policy for Surgical Procedures Perioperative
Identification of Patients (includes newborns)
Group & Screen Requirements in Maternity
Infant Feeding - Breastfeeding
Newborn Care in Post Anaesthesia Care Unit (PACU)
Oxygen Prescribing, Administration & Equipment - Adult
Postpartum Haemorrhage
Support Person in Operating Rooms & Procedure Rooms - Perioperative
Surgical Safety Checklist Perioperative
Clinical forms
Acute Surgical Booking Form CR2789
Anaesthesia Record CC0100
Pre-operative Assessment Record CR4049
Back to Contents
14. Disclaimer
No guideline can cover all variations required for specific circumstances. It is the
responsibility of the health care practitioners using this ADHB guideline to adapt it for
safe use within their own institution, recognise the need for specialist help, and call
for it without delay, when an individual patient falls outside of the boundaries of this
guideline.
Back to Contents
15. Corrections and amendments
The next scheduled review of this document is as per the document classification
table (page 1). However, if the reader notices any errors or believes that the
document should be reviewed before the scheduled date, they should contact the
owner or the Clinical Policy Advisor without delay.
Back to Contents
Caesarean Section May12.doc
Page 13 of 13
You might also like
- Robotic Assisted Single Site For Bilateral InguinalDocument3 pagesRobotic Assisted Single Site For Bilateral InguinalWilliam SonyoNo ratings yet
- Incidence of Inguinal Hernia Repairs in Olmsted County, MNDocument7 pagesIncidence of Inguinal Hernia Repairs in Olmsted County, MNWilliam SonyoNo ratings yet
- COMI Score Assesses Chronic Pain and Quality of Life After Hernia RepairDocument13 pagesCOMI Score Assesses Chronic Pain and Quality of Life After Hernia RepairWilliam SonyoNo ratings yet
- A Prospective Randomized Study Comparing Laparoscopic TransabdominalDocument18 pagesA Prospective Randomized Study Comparing Laparoscopic TransabdominalWilliam SonyoNo ratings yet
- Bilateral and Unilateral Total Extraperitoneal Inguinal HerniaDocument8 pagesBilateral and Unilateral Total Extraperitoneal Inguinal HerniaWilliam SonyoNo ratings yet
- Evaluation of Complications of Extracapsular Cataract Extraction Performed by TraineesDocument3 pagesEvaluation of Complications of Extracapsular Cataract Extraction Performed by TraineesWilliam SonyoNo ratings yet
- Randomised Clinical Trial Conventional Lichtenstein vs.Document6 pagesRandomised Clinical Trial Conventional Lichtenstein vs.William SonyoNo ratings yet
- BahanDocument5 pagesBahanWilliam SonyoNo ratings yet
- Terapi HerniaDocument2 pagesTerapi HerniaWilliam SonyoNo ratings yet
- Status EpilepticusDocument8 pagesStatus EpilepticusWilliam SonyoNo ratings yet
- Narcissistic Personality Disorder: Diagnostic and Clinical ChallengesDocument8 pagesNarcissistic Personality Disorder: Diagnostic and Clinical ChallengesWilliam SonyoNo ratings yet
- Ultrasound Prediction of Placenta Accreta AccuracyDocument7 pagesUltrasound Prediction of Placenta Accreta AccuracyRaisa AriesthaNo ratings yet
- NILAI AKHIR BLOK 23 SEMESTER GENAP 2014/2015Document9 pagesNILAI AKHIR BLOK 23 SEMESTER GENAP 2014/2015William SonyoNo ratings yet
- Preop Syl Lab UsDocument50 pagesPreop Syl Lab UsWilliam SonyoNo ratings yet
- Pre Op 2010Document37 pagesPre Op 2010Tawona DhlakamaNo ratings yet
- 1678 Pre-Operative Preparation Policy Feb12Document7 pages1678 Pre-Operative Preparation Policy Feb12William SonyoNo ratings yet
- Early Oral-Motor InterventionsDocument15 pagesEarly Oral-Motor InterventionsPhysio EbookNo ratings yet
- 37213Document29 pages37213William SonyoNo ratings yet
- BOLT! Mobile WiFi MF90 Update Tool v1.1 Manual Instruction For WindowsDocument7 pagesBOLT! Mobile WiFi MF90 Update Tool v1.1 Manual Instruction For WindowsSonia LimousNo ratings yet
- CadesDocument1 pageCadesWilliam SonyoNo ratings yet
- Dna FP 1Document40 pagesDna FP 1Satyam SinghNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- AMREF Virtual Training School Exam QuestionsDocument6 pagesAMREF Virtual Training School Exam QuestionsRita PrinceNo ratings yet
- Maternity Nursing Course Outline - Clinical PDFDocument24 pagesMaternity Nursing Course Outline - Clinical PDFAshraf NoriNo ratings yet
- CMA - Culture - First Aid BMP - MCHDocument8 pagesCMA - Culture - First Aid BMP - MCHSauharda DhakalNo ratings yet
- Analysis of Clinical Nursing JudgementDocument6 pagesAnalysis of Clinical Nursing Judgementapi-508102663No ratings yet
- Chiu 2019Document8 pagesChiu 2019Erika WulandariNo ratings yet
- Keamanan/Perlindungan: Resiko Perdarahan: Rencana Asuhan Keperawatan (Nursing Care Plan)Document3 pagesKeamanan/Perlindungan: Resiko Perdarahan: Rencana Asuhan Keperawatan (Nursing Care Plan)Ranap CempakaNo ratings yet
- Traditional Midwifery CareDocument9 pagesTraditional Midwifery Caremedicina tradicionalNo ratings yet
- Midwifery and Obstetric NursingDocument9 pagesMidwifery and Obstetric NursingANUM NOORINo ratings yet
- "Behold, Children Are A Heritage From The Lord, The Fruit of The Womb Is A Reward". - King DavidDocument16 pages"Behold, Children Are A Heritage From The Lord, The Fruit of The Womb Is A Reward". - King DavidInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Complications and minor ailments of the puerperiumDocument61 pagesComplications and minor ailments of the puerperiumMohammed AbdNo ratings yet
- Nursing Care Plan Risk For Uterine InfectionDocument4 pagesNursing Care Plan Risk For Uterine Infectionderic97% (30)
- Pediatrics - Allergy & Immunology TopicsDocument40 pagesPediatrics - Allergy & Immunology TopicspreethamNo ratings yet
- EMREE. UAE Emirates BluePrintDocument32 pagesEMREE. UAE Emirates BluePrintDhienda Laddy NasrulNo ratings yet
- Newborn Journal PDFDocument8 pagesNewborn Journal PDFRose Ann ManalastasNo ratings yet
- Professional Portfolio RussellDocument2 pagesProfessional Portfolio Russellapi-514966812No ratings yet
- Akal College Nursing Hours TeachersDocument3 pagesAkal College Nursing Hours TeachersDiksha chaudharyNo ratings yet
- Lesson Plan: Central ObjectivesDocument10 pagesLesson Plan: Central Objectivesprabha krishnanNo ratings yet
- Neonatal mortality risk factors in urban PakistanDocument7 pagesNeonatal mortality risk factors in urban PakistanDavid OlarinloyeNo ratings yet
- P1 Ginecoobstetricia IIDocument15 pagesP1 Ginecoobstetricia IICastro Erwis50% (2)
- The Effect Back Massage To The Height of UterineDocument4 pagesThe Effect Back Massage To The Height of UterineMuhamammad Salamuddin Al-AzhafNo ratings yet
- Community WrittenDocument23 pagesCommunity WrittenImPrint CenterNo ratings yet
- WHT Pangantucan 1Document21 pagesWHT Pangantucan 1Anonymous S4BuZ7uNo ratings yet
- OBS HC PROTOCOL 2021 - FinalDocument152 pagesOBS HC PROTOCOL 2021 - FinalWorkineh GizawNo ratings yet
- Health Talk TopicsDocument3 pagesHealth Talk Topicsvarshasharma0562% (13)
- NSDDocument44 pagesNSDabyssodeep100% (1)
- Maternal LEC - Week 4 - TransesDocument11 pagesMaternal LEC - Week 4 - TransesEcka- EckaNo ratings yet
- Sexual Life During Pregnancy and After Childbirth:a Survey of 540 Women in MoroccoDocument8 pagesSexual Life During Pregnancy and After Childbirth:a Survey of 540 Women in MoroccoIJAR JOURNALNo ratings yet
- Maternity and Women Chapter 21Document7 pagesMaternity and Women Chapter 21Sam JonesNo ratings yet
- Maria Carmina Lorenzana Santiago (Maria Antonia Esteban HabanaDocument49 pagesMaria Carmina Lorenzana Santiago (Maria Antonia Esteban HabanaMichelle VelascoNo ratings yet
- Ob Ward Duty Day 1Document29 pagesOb Ward Duty Day 1Kristil ChavezNo ratings yet