Professional Documents
Culture Documents
tmpCD4A TMP
Uploaded by
FrontiersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
tmpCD4A TMP
Uploaded by
FrontiersCopyright:
Available Formats
European Journal of Clinical Investigation (2006) 36, 528 535
Aminoguanidine prevents arterial stiffening in a new rat
model of type 2 diabetes
Blackwell Publishing Ltd
K.-C. Chang*, C.-D. Tseng, M.-S. Wu, J.-T. Liang, M.-S. Tsai, Y.-L. Cho* and Y.-Z. Tseng
*
National Taiwan University, National Taiwan University Hospital, Tapei, Taiwan, Show Chwan Memorial Hospital,
Chang-Hua, Taiwan
Abstract
Background Formation of advanced glycation end-products (AGEs) on collagen within the
arterial wall may be responsible for the development of diabetic vascular injury. This study
focused on investigating the role of aminoguanidine (AG), an inhibitor of AGE formation,
in the prevention of noninsulin-dependent diabetes mellitus (NIDDM)-derived arterial
stiffening and cardiac hypertrophy in rats.
Materials and methods The NIDDM was induced in male Wistar rats, which were
administered intraperitoneally with 180 mg kg1 nicotinamide (NA) 30 min before an
intravenous injection of 50 mg kg1 streptozotocin (STZ). After induction of diabetes
mellitus type 2, animals receiving daily peritoneal injections with 50 mg kg1 AG for 8 weeks
were compared with the age-matched, untreated, diabetic controls.
Results After exposure to AG, the STZ-NA diabetic rats had improved aortic distensibility, as
evidenced by 188% reduction of aortic characteristic impedance (P < 005). Treatment of the
experimental syndrome with AG also resulted in a significant increase in wave transit time
(+237%, P < 005) and a decrease in wave reflection factor (266%, P < 005), suggesting that
AG may prevent the NIDDM-induced augmentation in systolic load of the left ventricle. Also,
the glycation-derived modification on aortic collagen was found to be retarded by AG. The
diminished ratio of left ventricular weight to body weight suggested that prevention of the diabetesrelated cardiac hypertrophy by AG may correspond to the drug-induced decline in aortic stiffening.
Conclusions Long-term administration of AG to the STZ-NA diabetic rats imparts
significant protection against the NIDDM-derived impairment in vascular dynamics, at least
partly through inhibition of the AGE accumulation on collagen in the arterial wall.
Keywords Advanced glycation end-products, aminoguanidine, aortic input impedance,
pulse wave reflection, streptozotocin-nicotinamide diabetic rats.
Eur J Clin Invest 2006; 36 (8): 528535
Introduction
Diabetes mellitus (DM) is one of the most common
problems challenging physicians this century; approximately 140 million people world-wide currently have
diabetes, with the number projected to reach 300 million
by 2025 [1]. Type 2 DM, or noninsulin-dependent diabetes
National Taiwan University (K.-C. Chang, Y.-L. Cho), National
Taiwan University Hospital (C.-D. Tseng, M.-S. Wu, J.-T. Liang,
M.-S. Tsai, Y.-Z. Tseng), Tapei, Taiwan, Show Chwan Memorial
Hospital (Y.-Z. Tseng), Chang-Hua, Taiwan.
Correspondence to: K.-C. Chang, Department of Physiology,
College of Medicine, National Taiwan University, No. 1, Sec. 1,
Jen-Ai Road, Taipei, Taiwan. Tel.: +886 2 2312 3456; fax:
+886 2 2396 4350; e-mail: kcchang@ha.mc.ntu.edu.tw
Received 14 April 2006; accepted 19 May 2006
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd
mellitus (NIDDM), accounts for 90% of all cases. The
NIDDM is a complex metabolic disorder characterized by
hyperglycaemia and is associated with a relative deficiency
of insulin secretion, along with a reduced response of target
tissues to insulin. An important consequence of prolonged
hyperglycaemia is the enhanced formation of irreversible
advanced glycation end-products (AGEs) on long-lived
protein such as collagen within the arterial wall [2]. The
AGEs are a complex and heterogeneous group of compounds
that have been shown to accumulate slowly in vascular and
renal tissues with age and at a more rapid rate in diabetes
[24]. They can react with free-amino groups on an adjacent
collagen to form cross-linkages, which are thought to be one
of the central underlying processes by which they cause
damage [5]. Thus, the diabetes-related increase in AGE
accumulation on collagen in the arterial wall may contribute
to the development of certain physical changes of the blood
vessel wall [3,6,7].
Aminoguanidine and type 2 diabetic arteries
Therapeutic interventions for reducing AGE formation
should target AGE formation by reducing cross-linking
formation [8,9]. Aminoguanidine (AG), a nucleophilic
hydrazine compound, is a prototype of scavenging agents
that inhibit AGE formation and protein-protein crosslinking [10]. It has been shown to decrease methylglyoxalmediated formation of AGEs implicated as a downstream
consequence of oxidative stress, induced by mitochondrial
dysfunction in hyperglycaemia [11,12]. Aminoguanidine
therapy of rats with insulin deficiency prevents the severe
hyperglycaemia-related disorders in systolic loading condition
for the left ventricle coupled to the vasculature [13]. It has
also been reported to improve the age-related deterioration
in the pulsatile nature of blood flows in rat arteries, possibly
through inhibition of the AGE formation [14]. However,
little attention has been given to the haemodynamic response
to AG in imparting significant protection against aortic stiffening and cardiac hypertrophy in rats with NIDDM.
In 1998, Masiello et al. [15] described a new rat model
of type 2 diabetes that shared a number of features with
human NIDDM. This diabetic syndrome was experimentally
induced in adult rats administered streptozotocin (STZ)
and partially protected with a suitable dose of nicotinamide
(NA). It was characterized by moderate and stable
hyperglycaemia, glucose intolerance, altered but significant
glucose-stimulated insulin secretion, in vivo and in vitro
responsiveness to tolbutamide. An earlier report from this
laboratory demonstrated that the AGE-modulated collagen
cross-link within the arterial wall is an import factor responsible for the development of vascular injury in rats at 8 weeks
not 4 weeks after STZ and NA administration [16]. Herein,
the authors have focused on investigating the role of AG in
the prevention of NIDDM-related arterial stiffening and
cardiac hypertrophy in the diabetic syndrome, using aortic
impedance analysis [17,18]. Glycation-derived modification
on aortic collagen was also detected by sodium dodecyl
sulphate polyacrylamide gel electrophoresis (SDS-PAGE).
529
concentrations in plasma were measured by the ELISA
method (Mercodia AB, Uppsala, Sweden). The development of hyperglycaemia was confirmed by blood glucose
determination using a Surestep Test Strip (Lifescan Inc.,
Milpitas, CA). All animals were allowed free access to the
Purina chow and water and housed two or three per cage
in a 12-h light/dark-cycle animal room. The animal experiments were conducted according to the establishments
Guide for the Care and Use of Laboratory Animals, and
were approved by the Animal Care and Use Committee of
the National Taiwan University.
General surgical procedures and measurement of the
haemodynamic variables in anaesthetized rats have been
described in our previous work [19]. In brief, the rats were
anaesthetized with sodium pentobarbital (50 mg kg1, i.p.),
placed on a heating pad, intubated, and ventilated with a
Model 131 rodent respirator (New England Medical Instruments, Medway, MA). The chest was opened through the
second intercostal space of the right side. An electromagnetic
flow probe, Model 100 series of internal circumference 8 mm,
(Carolina Medical Electronics, King, NC) was positioned
around the ascending aorta to measure the pulsatile aortic
flow. A high-fidelity pressure catheter (Model SPC 320, size
2F; Millar Instruments, Houston, TX) was used to measure
the pulsatile aortic pressure via the isolated carotid artery
of the right side. The electrocardiogram (ECG) of lead II
was recorded with an ECG/Biotach amplifier (Gould,
Cleveland, OH). The selective pressure and flow signals of
510 beats were averaged in the time domain, using the
peak R-wave of ECG as a fiducial point. Timing between
the pressure and flow signals, owing to spatial distance
between the flow probe and proximal aortic pressure
transducer, was corrected by a time-domain approach, in
which the foot of the pressure waveform was realigned with
that of the flow [20]. The resulting pressure and flow signals
were subjected to further aortic impedance analysis.
Aortic input impedance spectra
Materials and methods
Animals and catheterization
Two-month-old Male Wistar rats were randomly divided
into four groups (n = 12 in each group) as follows: (i) normal
controls (NC); (ii) rats of DM type 2 (STZ-NA); (iii) NC
treated with AG (NC + AG); and (iv) STZ-NA treated with
AG (STZ-NA + AG). The NIDDM was induced in
animals, which were administered intraperitoneally
180 mg kg1 NA (Sigma, St. Louis, MO) 30 min before an
intravenous injection of 50 mg kg1 STZ (Sigma, St. Louis,
MO) dissolved in 01 M citrate buffer (pH 45) [15]. After
induction of DM type 2, the STZ-NA rats were randomized
into a vehicle-treated diabetic group, and a treatment group
receiving daily injections of 50 mg kg1 AG (Sigma, St.
Louis, MO). The animals were studied 8 weeks after being
induced with diabetes to detect the effects of NIDDM and
AG on the physical properties of the vasculature. Insulin
The aortic input impedance can be obtained from the ratio
of ascending aortic pressure harmonics to the corresponding flow harmonics, using a standard Fourier series
expansion technique (Fig. 1) [17,18]. Total peripheral
resistance of the systemic circulation (Rp) was calculated as
the mean aortic pressure/mean aortic flow. The aortic
characteristic impedance (Zc) was computed by averaging
high-frequency moduli of the aortic input impedance data
points (4th10th harmonics) [21,22]. Taking Zc into
consideration, the systemic arterial compliance (C ) was
calculated at mean aortic pressure (Pm) by expanding the
two-element [23] into the three-element Windkessel model,
which accounts for a nonlinear exponential pressurevolume relationship:
bP
SV b
e m
,
bP
bP
K + Z c SV / Ad
e ie d
where SV is the stroke volume; K is the ratio of total area
under the aortic pressure curve to the diastolic area (Ad);
C( Pm ) =
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
530
K.-C. Chang et al.
Figure 1 Aortic input impedance spectra derived from ascending
aortic pressure and flow signals from a STZ-NA diabetic rat treated
with AG (dashed line) compared with those of an untreated diabetic
animal (solid line). STZ-NA, diabetic rats at 8 weeks after being
administered STZ and NA; AG, aminoguanidine; Rp, total
peripheral resistance; Zc, aortic characteristic impedance.
b is the coefficient in the pressure-volume relation (00131
0009 of aortic arch); Pi is the pressure at the time of
incisura; and Pd is the end-diastolic pressure.
The wave transit time () can be computed by the impulse
response of the filtered aortic input impedance (Fig. 2).
This was accomplished by the inverse transformation of Zi
after multiplication of the first 12 harmonics by a DolphChebychev weighting function of the order of 24 [24].
Meanwhile, the time domain reflection factor (Rf) was
derived as the amplitude ratio of backward-to-forward peak
pressure wave method proposed by Westerhof et al. [25].
Therefore, both the wave transit time and the wave reflection
factor could characterize the wave reflection phenomenon
in the vasculature.
Gel electrophoresis
A method for measuring collagen glycation was proposed
by Turk et al. [26]. Collagen samples from aortic walls,
previously digested by pepsin, proteinase K and collagenase,
were investigated by sodium dodecyl sulphate polyacrylamide
Figure 2 Impulse response function curve derived from filtered
aortic input impedance spectra shown in Fig 1. Long arrow shows
the discrete reflection peak from the body circulation and short
arrow shows the initial peak as a reference. Half the time difference
between the appearance of the reflected peak (long arrow) and the
initial peak (short arrow) approximates the wave transit time in the
lower body circulation. STZ-NA, diabetic rats at 8 weeks after
being administered STZ and NA; AG, aminoguanidine.
gel electrophoresis (SDS-PAGE) on a Mini PROTEAN 3
System (Bio-Rad Laboratory, Hercules, CA). This was
carried out using a 4% stacking and a 10% separating gel,
running buffer system (Tris-HCl, Ph 83/SDS/glycine), and
Coomassie blue staining (Fig. 3). Each lane was loaded with
20 g protein from two or three rats. Protein blotting
analysis was carried out on PVDF membrane, using
anti-AGE antibody 6D12 (Trans Genic Inc., Kumamoto,
Japan).
Statistics
Results are expressed as means SD. A two-way analysis
of variance (anova) was used to determine the effects of
NIDDM and AG on the physical properties of the rat arterial system, using the statistical package SAS (SAS Institute
Inc., Cary, NC). Simple effect analysis was used when significant interaction between NIDDM and AG occurred.
Differences between means within levels of a factor were
determined by Tukeys honestly significant difference
(HSD) method. Significant differences were set at the level
of P < 005.
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
Aminoguanidine and type 2 diabetic arteries
531
Figure 3 Left: data showing SDS-PAGE
electrophoretic profiles of aortic collagen
from the STZ-NA diabetic rats treated with
AG (n = 2) compared with those of the
untreated diabetic animals (n = 2). Right:
corresponding protein blotting analysis on
PVDF membrane, using anti-AGE antibody
6D12. Diabetic collagen samples display
molecular weight fragments 2540 kDa, and
the glycated aortic collagen was diminished
by treatment of the experimental syndrome
with AG for 8 weeks. STZ-NA, diabetic rats
at 8 weeks after being administered STZ and
NA; AG, aminoguanidine.
Results
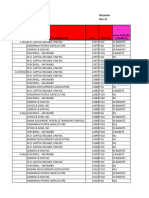
Table 1 shows the effects of NIDDM and AG on bloodglucose level, plasma insulin, body-weight (BW), left
ventricular weight (LVW), and aortic pressure profile in
the STZ-NA rats. The experimental syndrome yielded
a moderate and stable hyperglycaemia and prevented
STZ-induced hypoinsulinaemia and body-weight loss.
Body-weight, blood-glucose level, and plasma insulin of the
STZ-NA diabetic animals did not change in response to AG
treatment. In contrast, the significant increases in LVW and
LVW/BW ratio by prolonged hyperglycaemia were not
observed in the corresponding AG-treated group. Neither
NIDDM nor AG produced a significant change in aortic
pressure profile, nor was there an NIDDM AG interaction
for the arterial blood pressure. No significant differences in
the haemodynamic variables were observed between the
normal controls with or without AG treatment.
Figure 1 shows the effects of AG on the aortic input
impedance spectra from a STZ-NA diabetic rat. Treatment
of this experimental NIDDM with AG showed a decrease
in moduli at lower harmonics, a fall in averaging highfrequency moduli of the aortic characteristic impedance and
a decline in amplitude of the fluctuation between maximum
and minimum impedance moduli. Figure 2 describes the
impulse response function curve derived from the filtered
aortic input impedance spectra shown in Fig. 1. After
exposure to AG, the diabetic animal exhibited an increase
in wave transit time, suggesting that AG may prevent the
NIDDM-derived abnormality in the timing of the pulse
wave reflection along the path. Figure 3 demonstrates the
SDS-PAGE electrophoretic profiles of aortic collagen from
Table 1 Effects of noninsulin-dependent diabetes mellitus and aminoguanidine on body-weight, left ventricular weight, plasma glucose
and insulin level and aortic pressure profile in male Wistar rats (n = 12 per group)
Variable
NC
NC + AG
STZ-NA
STZ-NA + AG
BW (g)
LVW (mg)
LVW/BW (mg g1)
Glucose (mg dL1)
Insulin (IU mL1)
Ps (mmHg)
Pd (mmHg)
Pm (mmHg)
PP (mmHg)
4433 285
8016 507
181 009
1023 179
718 302
121 105
979 82
1067 72
233 29
4425 313
8017 595
181 007
1011 208
713 287
1173 84
934 94
1031 68
24 33
4208 303
863 605*
206 013*
1596 238*
692 280
1189 171
927 169
1077 155
259 34
4117 349
760 643
186 012
1541 256
643 275
1162 95
90 74
1048 88
255 37
All values are expressed as means SD.
*
Statistical difference (P < 005) from the control group (NC).
Statistical difference (P < 005) from the STZ-NA group.
AG, aminoguanidine; BW, body-weight; LVW, left ventricular weight; NA, nicotinamide; NIDDM, noninsulin-dependent diabetes
mellitus; Ps, systolic aortic pressure; Pd, diastolic aortic pressure; Pm, mean aortic pressure; PP, pulse pressure; STZ, streptozotocin;
STZ-NA, diabetic rats at 8 weeks after being administered STZ and NA.
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
532
K.-C. Chang et al.
the animals studied. There was a 62% increase in collagen
AGE content with prolonged hyperglycaemia and the
glycated aortic collagen was diminished by administration
of AG for 8 weeks to the STZ-NA diabetic rats.
Figure 4 shows the effects of NIDDM and AG on the
static haemodynamic data in terms of basal heart rate (HR),
cardiac output (CO), stroke volume (SV ) and total peripheral
resistance (Rp). The HR showed a significant decrease in the
rats with type 2 diabetes; however, HR did not change in
response to AG treatment (Fig. 4a). Moderate hyperglycaemia
after 8 weeks from induction markedly lowered CO
(Fig. 4b) and SV (Fig. 4c) and the NIDDM-derived alterations were retarded by AG treatment. A decrease in CO in
the absence of any significant changes in Pm (Table 1)
caused an increase in Rp in the STZ-NA diabetic animals,
from (554 68 to 660 85) mmHg s mL1 (P < 005)
(Fig. 4d). Administration of AG to this experimental
syndrome for 8 weeks prevented the diabetes-related
deterioration in physical properties of the resistance vessels,
as evidenced by the reduction of 167% in Rp (P < 005).
In contrast, the static components of the ventricular
after-load, including HR, CO, SV and Rp, were unaffected
by treatment of the normal controls with AG.
Figure 5 shows the effects of NIDDM and AG on the
pulsatile nature of blood flows in arteries using aortic
characteristic impedance (Zc), aortic compliance (Cm), wave
transit time (), and wave reflection factor (Rf). Diabetes
contributed to a marked increase in Zc, from 150 026 to
197 030 mmHg s mL1 (P < 005) (Fig. 5a) and a
decrease in Cm, from 104 15 to 82 17 L mmHg1
(P < 005) (Fig. 5b). The AG administered to the diabetic
animals for 8 weeks prevented the NIDDM-induced
decline in aortic distensibility, as manifested by the fall of
188% in Zc (P < 005) and the rise of 263% in Cm
(P < 005). Meanwhile, the experimental syndrome had
increased Rf (046 008 vs. 062 014; P < 005) (Fig. 5c)
and decreased (252 29 vs. 204 27 ms; P < 005)
(Fig. 5d). Early return with the augmented magnitude of
the reflected wave from the peripheral circulation was
retarded by treatment of the diabetic animals with AG, as
evidenced by the increase of 237% in (P < 005) and by
the reduction of 266% in Rf (P < 005). In contrast, the
oscillatory components of the ventricular after-load, including Zc, Cm, and Rf , were not modified by administration
of AG to the normal controls.
Discussion
The major findings of this study were that long-term
treatment of the STZ-NA diabetic rats imparts significant
Figure 4 Effects of NIDDM and AG on: (a) basal heart rate (HR), (b) cardiac output (CO), (c) stroke volume (SV ) and (d) total peripheral
resistance (Rp), (n = 12 per group). Treatment of the experimental syndrome with AG for 8 weeks prevented the NIDDM-related
deterioration in the physical properties of the resistance vessels, as evidenced by the reduction of 167% in Rp. By contrast, AG exerted
no effects on those static haemodynamic variables in age-matched normal controls (NC). STZ-NA, diabetic rats at 8 weeks after being
administered STZ and NA; AG, aminoguanidine.
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
Aminoguanidine and type 2 diabetic arteries
533
Figure 5 Effects of NIDDM and AG on: (a) aortic characteristic impedance (Zc), (b) systemic arterial compliance at mean aortic pressure
(Cm), (c) wave reflection factor (Rf) and (d) wave transit time (), (n = 12 per group). The NIDDM-derived alterations in the mechanical
properties of the Windkessel vessels were retarded by administration of AG to the diabetic animals for 8 weeks, as reflected in the fall of
188% in Zc and the rise of 263% in Cm. The AG also improved the systolic loading condition for the left ventricle coupled to the arterial
system by diminishing 266% of Rf and delaying 237% of . By contrast, AG exerted no effects on the pulsatile nature of blood flows in
arteries in age-matched normal controls (NC). STZ-NA, diabetic rats at 8 weeks after being administered STZ and NA; AG,
aminoguanidine.
protection against the prolonged and moderate hyperglycaemiaderived impairment in vascular dynamics; at least in part,
through inhibition of the AGE formation and accumulation within the blood vessel wall.
Herein, basal heart rate HR showed a significant decrease
in the rats of DM type 2 and HR did not change in response
to AG treatment (Fig. 4a). These results were in accordance with the report from Schmidt et al. [27], who found
that long-term administration of AG to diabetic animals
could not prevent the development of sympathetic neuroaxonal dystrophy, which is responsible for the decrease in
HR.
A decline in cardiac output occurred in the absence of
any significant changes in mean aortic pressure, causing a
rise in total peripheral resistance (Rp) in the STZ-NA
diabetic rats. It has been shown that prolonged hyperglycaemia may enhance the formation of both reversible
amadori intermediate products and irreversible AGEs within
the artery wall [2,4]. The AGEs are reported to induce freeradical production and deplete nitric oxide (NO) concentration, leading to a state of oxidative stress [28]. The ability
of AGEs to quench NO is supposed to diminish the
vasodilatory capacity of the peripheral muscular arteries in
the rats of type 2 diabetes. Therefore, an increase in AGE
accumulation in the STZ-NA diabetic animals may be one
of the several factors responsible for the increased vascular
smooth muscle tone. The NIDDM-derived physical
changes in the resistance vessels were prevented by administration of AG to rats for 8 weeks, as reflected in the
reduction of 167% in Rp. In addition to being an AGE-blocker,
AG could act as a preventative agent in diabetic cardiovascular complications by NO synthase-inhibition pathways
[29]. However, a beneficial effect of AG on resistance to
blood flow in the absence of any significant change in mean
aortic pressure was observed in this report when AG was
administered to the experimental syndrome. These findings
are in agreement with those obtained by Huijberts et al.
[21], who found that arterial blood pressure remained
unaltered and aortic impedance was lower in the AG-treated
diabetic animals. Thus, the prevention of NIDDM-induced
vasodilatory dysfunction may result from inhibition of the
AGE formation by AG to reserve NO production in the
resistance vessels.
As for the pulsatile nature of blood flows in arteries, the
aortic characteristic impedance increased (Zc in Fig. 5a) and
the wave transit time decreased ( in Fig. 5d) in the STZNA diabetic rats. Although being affected by the lumen
radius, Zc is inversely related to the aortic distensibility such
that Zc has been frequently used as an indicator of aortic
stiffness: the higher the aortic characteristic impedance, the
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
534
K.-C. Chang et al.
stiffer the aortic wall [17,18]. Meanwhile, being relatively
independent to body shape, wave transit time (), which is
inversely related to pulse wave velocity, could also be derived
to describe the aortic distensibility: the stiffer the aortic wall,
the shorter the wave transit time and vice versa [17]. Herein,
both the augmented Zc and the shortened suggest that a
decline in aortic distensibility may occur in the STZ-NA
diabetic animals. It has been shown that accumulation of
AGEs in the arterial wall is associated with changes in the
biomechanical properties of collagen characterized by
increasing stiffness of the elastic reservoir [4,10]. There
was a 62% increase in aortic collagen AGE content in the
rats of type 2 diabetes. So, the AGE-modulated collagen
cross-link in the Windkessel vessels could function as
one of the several factors to increase the arterial stiffness
with diabetes. The NIDDM-induced fall in aortic distensibility was prevented by 8 weeks treatment of the
experimental syndrome with AG, as manifested by the
reduction of 188% in Zc and the increase of 237% in .
The AG treatment also contributed to a rise of 263% in
systemic arterial compliance of the rats with prolonged
hyperglycaemia (Fig. 5b). Such prevention of the NIDDMderived arterial stiffness by AG was supported by the fact
that the glycated collagen in the aortic wall was diminished
by administration of AG to this new rat model of type 2 diabetes (Fig. 3).
Interestingly, no significant changes in arterial pulse
pressure were observed in the STZ-NA diabetic animals
with the increased arterial stiffness (Table 1). Several factors
importantly affect the magnitude of the pulse pressure,
including the stroke volume and the aortic compliance [30].
The arterial pulse pressure varies directly with the stroke
volume but inversely with the arterial compliance. Thus, the
decrease in SV (Fig. 4c) may blunt the effect of the diminished Cm (Fig. 5b) on the pulse pressure in the rats with
type 2 DM. After exposure to AG, this experimental
syndrome also showed no significant alteration in arterial
pulse pressure because of its counter-balancing influences
of increasing SV and augmenting Cm on this haemodynamic
parameter.
Changes in timing and/or magnitude of the pulse wave
reflection do impair the loading condition for the left
ventricle when coupled to its arterial system [31]. With the
enhanced wave reflection factor (Rf in Fig. 5c), the experimental syndrome contributed to a reduction in wave transit
time ( in Fig. 5d) in the STZ-NA diabetic rats. The
increased Rf with shortened indicates that prolonged and
moderate hyperglycaemia can modify the timing and
magnitude of the pulse wave reflection to augment systolic
load of the left ventricle. The impaired systolic loading
condition of the left ventricle may cause the heart to adapt
to muscular hypertrophy, as evidenced by the increase in
the ratio of LVW : BW (Table 1). After exposure to AG,
the diabetic animals showed a significant fall of 266% in
Rf , suggesting that the heavy reflection phenomenon may
be alleviated in the circulatory system. The observed
increase in and decrease in Rf indicate that AG, by
preventing the AGE accumulation on collagen in the
diabetic arterial wall, can improve the systolic loading
condition for the left ventricle coupled to the vasculature.
Moreover, the ratio of LVW : BW was decreased by AG
treatment, suggesting that the prevention of NIDDMrelated cardiac hypertrophy may correspond to the druginduced decline in arterial load.
This report has demonstrated that AG ameliorates
vascular complications observed in the experimentallyinduced diabetes type 2 at least partly through inhibition of
the AGE formation. However, when using AG it is important
to be aware of the facts that this drug, apart from preventing
formation of AGEs, also inhibits diamine oxidase (DAO)
[32]. In the in vivo situation inhibition of DAO might lead
to serious vascular and respiratory side-effects owing to
accumulation of histamine in the blood stream. In addition,
AG in high doses may bind to S-adenosylmethionine
decarboxylase (SAMDC) and thereby might affect polyamine
formation. The effects of AG on the mechanical properties
of the vasculature owing to inhibition of DAO and stabilization of SAMDC remains to be determined in rats treated
with STZ and NA.
The authors contribution to this endeavour was to
provide a path to consider the clinical application of an AGE
inhibitor in the prevention of NIDDM-related deterioration
in vascular dynamics. The AG may target elastic arteries
(characteristic impedance), muscular arteries (wave reflection factor) and arterioles (peripheral resistance) by inhibiting the formation of AGEs in the diabetic blood vessel wall.
However, an important limitation of AG and other AGEinhibitors is that they cannot reverse pre-existing AGE
cross-linking, and thus the AGE breakers are supposed
to be noted. Recently, several studies have used the AGE
breaker compound 4,5-dimethyl-3-phenacylthiazolium
chloride (also called ALT-711) for animal and human
studies [9,33]. The results of ongoing clinical studies will
determine if these compounds can become the first specific
therapy for the diabetes-related cardiovascular disorder.
Taken together, it has been demonstrated that moderate
and stable hyperglycaemia produces a detriment to the
physical properties of the resistance vessels and the
Windkessel vessels in rats administered STZ and NA after
8 weeks. Prevention of the NIDDM-induced vasodilatory
dysfunction may in part result from inhibition of the
AGE formation by AG to reserve NO production in the
resistance vessels. Treatment of the experimental syndrome
with AG for 8 weeks may prevent the AGE-modulated
collagen cross-link in the arterial walls so that the aortic
distensibility can be improved in the STZ-NA diabetic
animals. Moreover, AG can retard the NIDDM-derived
augmentation in systolic load of the left ventricle by
delaying the return of the pulse wave reflection associated
with the reduced wave reflection intensity. The prevention
of diabetes-related cardiac hypertrophy by AG may
correspond to the drug-induced decline in left ventricle
after-load. We concluded that long-term treatment of
the STZ-NA diabetic rats with AG imparts significant
protection against the NIDDM-derived impairment in
vascular dynamics, at least partly through inhibition of
the AGE accumulation on collagen within the arterial
wall.
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
Aminoguanidine and type 2 diabetic arteries
Acknowledgements
This study was supported by grants from the National
Taiwan University Hospital (NTUH 94-S017) and from the
National Science Council of Taiwan (NSC 94 2320-B002058).
References
1 King H, Aubert RE, Herman WH. Global burden of diabetes
19952025: prevalence, numerical estimates, and projections.
Diabetes Care 1998;21:1414 31.
2 Brownlee M, Cerami A, Vlassara H. Advanced glycosylation
end products in tissue and the biochemical basis of diabetic
complications. N Engl J Med 1988;318:1315 21.
3 Bucula R, Cerami A. Advanced glycosylation: chemical,
biology, and implications for diabetes and aging. Adv Pharmacol
1992;23:134.
4 Vlassara H, Bucala R, Striker L. Pathogenic effects of advanced
glycosylation: biochemical, biological, and clinical implications
for diabetes and aging. Lab Invest 1994;70:138 51.
5 Bucala R. Lipid and lipoprotein modification by advanced
glycosylation endproducts: role in atherosclerosis. Exp Physiol
1997;82:32737.
6 Vishwanath V, Frank KE, Elmets CA, Dauchot PJ, Monnier
VM. Glycation of skin collagen in type I diabetes mellitus.
Correlation with long-term complications. Diabetes
1986;35:916 21.
7 Cerami A, Vlassara H, Brownlee M. Role of nonenzymatic
glycosylation in atherogenesis. J Cell Biochem 1986;30:11120.
8 Bierhaus A, Hofmann MA, Ziegler R, Nawroth PP. AGE and
their interaction with AGE receptor in vascular disease and
diabetes I. The AGE concept. Cardiovasc Res 1998;37:586
600.
9 Kass DA, Shapiro EP, Kawaguchi M, Capriotti AR, Scuteri A,
Degroof RC et al. Improved arterial compliance by a novel
advanced glycation end-product cross-link breaker. Circulation
2001;104:1464 70.
10 Brownlee M, Vlassara H, Kooney A, Ulrich P, Cerami A.
Aminoguanidine prevents diabetes-induced arterial wall
protein cross-linking. Science 1986;232:1629 32.
11 Edelstein D, Brownlee M. Mechanistic studies of advanced
glycosylation end product inhibition by aminoguanidine.
Diabetes 1992;41:269.
12 Brownlee M. Biochemistry and molecular cell biology of
diabetic complications. Nature 2001;414:813 20.
13 Chang KC, Hsu KL, Tseng CD, Lin YD, Cho YL, Tseng YZ.
Aminoguanidine prevents arterial stiffening and cardiac
hypertrophy in streptozotocin-induced diabetes in rats. Br J
Pharmacol 2006;147:944 50.
14 Chang KC, Hsu KL, Peng YI, Lee FC, Tseng YZ.
Aminoguanidine prevents age-related aortic stiffening in Fisher
344 rats: aortic impedance analysis. Br J Pharmacol
2003;140:10714.
15 Masiello P, Broca C, Gross R, Roye M, Manteghetti M,
Hillaire-Buys D et al. Experimental NIDDM. Development of
a new model in adult rats administered streptozotocin and
nicotinamide. Diabetes 1998;47:2249.
535
16 Chang KC, Tseng CD, Chou TF, Cho YL, Chi TC, Su MJ
et al. Arterial stiffening and cardiac hypertrophy in a new rat
model of type 2 diabetes. Eur J Clin Invest 2006;36:17.
17 Milnor WR. Hemodynamics. Baltimore, MD: Williams &
Wilkins Co., 1989.
18 Nichols WW, ORourke MF. Mcdonalds Blood Flow in Arteries.
London, UK: Arnold, 2005.
19 Chang KC, Hsu KL, Tseng YZ. Effects of diabetes and gender
on mechanical properties of the arterial system in rats: aortic
impedance analysis. Exp Biol Med 2003;228:70 8.
20 Mitchell GF, Pfeffer MA, Westerhof N, Pfeffer JM.
Measurement of aortic input impedance in rats. Am J Physiol
1994; 267 (Heart Circ Physiol 36):H190715.
21 Huijberts MS, Wolffenbuttel BH, Boudier HA, Crijns FR,
Kruseman AC, Poitevin P et al. Aminoguanidine treatment
increases elasticity and decreases fluid filtration of large arteries
from diabetic rats. J Clin Invest 1993;92:140711.
22 Gaballa MA, Raya TE, Hoover CA, Goldman S. Effects of
endothelial and inducible nitric oxide synthases inhibition on
circulatory function in rats after myocardial infarction.
Cardiovasc Res 1999;42:62735.
23 Liu A, Brin KP, Yin FCP. Estimation of total arterial
compliance: An improved method and evaluation of current
methods. Am J Physiol 1986;251 (Heart Circ Physiol
20):H588600.
24 Laxminarayan S, Sipkema P, Westerhof N. Characterization of
the arterial system in the time domain. IEEE Trans Biomed Eng
1978;25:17784.
25 Westerhof N, Sipkema P, VanDen Bos GC, Elzinga G. Forward
and backward waves in the arterial system. Cardiovasc Res
1972;6:64856.
26 Turk Z, Mi5ur I, Turk N, Benko B. Rat tissue collagen modified
by advanced glycation: correlation with duration of diabetes and
glycemic control. Clin Chem Lab Med 1999;37:81320.
27 Schmidt RE, Dorsey DA, Beaudet LN, Reiser KM, Williamson
JR, Tilton RG. Effect of aminoguanidine on the frequency of
neuroaxonal dystrophy in the superior mesenteric sympathetic
autonomic ganglia of rats with streptozotocin-induced diabetes.
Diabetes 1996;45:28490.
28 McCance DR, Dyer DG, Dunn JA, Bailie KE, Thorpe SR,
Baynes JW et al. Maillard reaction products and their relation
to complications in insulin-dependent diabetes mellitus. J Clin
Invest 1993;91:24708.
29 Corbett JA, Tilton RG, Chang K, Hasan KS, Ido Y, Wang JL
et al. Aminoguanidine, a novel inhibitor of nitric oxide
formation, prevents diabetic vascular dysfunction. Diabetes
1992;41:5526.
30 West JB. BEST and TAYLORS physiological basis of medical
practice. In: West JB, editor. Dynamics of the Peripheral
Circulation. Baltimore, MD: Williams & Wilkins;1991.pp. 1479.
31 ORourke MF, Avolio AP, Nichols WW. Left ventricularsystemic arterial coupling in humans and strategies to improve
coupling in disease states. In: Yin FCP, editor. Ventricular/
Vascular Coupling. New York, NY: Springer-Verlag;1987.pp. 1
19.
32 Nilsson BO. Biological effects of aminoguanidine: an update.
Inflamm Res 1999;48:50915.
33 Wolffenbuttel BH, Boulanger CM, Crijns FR, Huijberts MS,
Poitevin P, Swennen GN et al. Breakers of advanced glycation
end products restore large artery properties in experimental
diabetes. Proc Natl Acad Sci USA 1998;95:46304.
2006 The Authors. Journal Compilation 2006 Blackwell Publishing Ltd, European Journal of Clinical Investigation, 36, 528535
You might also like
- Prostaglandins, Platelets, Lipids: New Developments in AtherosclerosisFrom EverandProstaglandins, Platelets, Lipids: New Developments in AtherosclerosisNo ratings yet
- tmp269F TMPDocument7 pagestmp269F TMPFrontiersNo ratings yet
- Beneficial Role of Telmisartan On Cardiovascular Complications Associated With STZ-induced Type 2 Diabetes in RatsDocument11 pagesBeneficial Role of Telmisartan On Cardiovascular Complications Associated With STZ-induced Type 2 Diabetes in RatsAuthor Nauman ShadNo ratings yet
- Cardiorenal Protection in Diabetic Kidney Disease: Review ArticleDocument14 pagesCardiorenal Protection in Diabetic Kidney Disease: Review ArticleveraNo ratings yet
- Anti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsDocument5 pagesAnti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsBarbara Sakura RiawanNo ratings yet
- SezaiDocument13 pagesSezaigarry.soloanNo ratings yet
- Metformin Attenuates Early-Stage Atherosclerosis in Mildly Hyperglycemic Oikawa-Nagao MiceDocument9 pagesMetformin Attenuates Early-Stage Atherosclerosis in Mildly Hyperglycemic Oikawa-Nagao Micegandik danu pramigaNo ratings yet
- The Effect of Combined Aerobic and Resistance Exercise Training On Vascular Function in Type 2 DiabetesDocument7 pagesThe Effect of Combined Aerobic and Resistance Exercise Training On Vascular Function in Type 2 DiabetesZINATUL WIDADNo ratings yet
- A Clinical Evaluation of Statin Pleiotropy: Statins Selectively and Dose-Dependently Reduce Vascular InflammationDocument9 pagesA Clinical Evaluation of Statin Pleiotropy: Statins Selectively and Dose-Dependently Reduce Vascular InflammationzzakieNo ratings yet
- Correos Electrónicos Active Vitamin D3 Protects Against Diabetic Kidney Disease by Regulating The JNK Signaling Pathway in RatsDocument9 pagesCorreos Electrónicos Active Vitamin D3 Protects Against Diabetic Kidney Disease by Regulating The JNK Signaling Pathway in Ratsnoranton7No ratings yet
- UKPDS 39 compares atenolol and captoprilDocument8 pagesUKPDS 39 compares atenolol and captoprilLaila MayangsariNo ratings yet
- 2022-Association of iSGLT2 Use With Cardiovascular and Renal Outcomes in Type 2 Diabetes Mellitus Patients With Stabilized AMIDocument8 pages2022-Association of iSGLT2 Use With Cardiovascular and Renal Outcomes in Type 2 Diabetes Mellitus Patients With Stabilized AMIWENDY JOHANA HENRIQUEZ SEGURA ESTUDIANTE ACTIVONo ratings yet
- Noninvasive Magnetic Resonance Imaging of Microvascular Changes in Type 1 DiabetesDocument6 pagesNoninvasive Magnetic Resonance Imaging of Microvascular Changes in Type 1 DiabetesAndrés Esteban Quezada VenegasNo ratings yet
- Chewcharat2020 Efficacy and Safety of SGLT-2 Inhibitors For Treatment of DM Amog Kidney Transplant Patients A Systematic Review and Meta AnalisisDocument16 pagesChewcharat2020 Efficacy and Safety of SGLT-2 Inhibitors For Treatment of DM Amog Kidney Transplant Patients A Systematic Review and Meta AnalisisLaura GarciaNo ratings yet
- TyG VascularagingDocument8 pagesTyG VascularagingSNo ratings yet
- Packer 2017Document5 pagesPacker 2017Olivia Chandra DeviNo ratings yet
- The Essential Role of Endothelial Nitric Oxide Synthase Activation in Insulin-Mediated Neuroprotection Against Ischemic Stroke in DiabetesDocument9 pagesThe Essential Role of Endothelial Nitric Oxide Synthase Activation in Insulin-Mediated Neuroprotection Against Ischemic Stroke in DiabetesrivandiNo ratings yet
- Georgianos 2023 Therapeutic Advances in Diabetic KiDocument12 pagesGeorgianos 2023 Therapeutic Advances in Diabetic Kiiacob ancutaNo ratings yet
- Derosa 2010 InfDocument5 pagesDerosa 2010 InfJuan Carlos FloresNo ratings yet
- Food and Chemical ToxicologyDocument7 pagesFood and Chemical ToxicologytahamasoodiNo ratings yet
- Kidney News Article p14 - 9Document3 pagesKidney News Article p14 - 9hossein kasiriNo ratings yet
- ISGLT2 Revi3w Nejm2022Document11 pagesISGLT2 Revi3w Nejm2022salvado moyanoNo ratings yet
- MatsutaniDocument12 pagesMatsutanigarry.soloanNo ratings yet
- Nej MR A 2115011Document11 pagesNej MR A 2115011LETICIA CRISTINO FRANCISCONo ratings yet
- Review Article: Acupoint Therapy On Diabetes Mellitus and Its Common Chronic Complications: A Review of Its MechanismsDocument10 pagesReview Article: Acupoint Therapy On Diabetes Mellitus and Its Common Chronic Complications: A Review of Its Mechanismsoscarin123456789No ratings yet
- IL27 CardioprotectoraDocument13 pagesIL27 CardioprotectoraAdrián Asael Rodriguez CortesNo ratings yet
- Challenges of Sodium-Glucose Transporter-2 Inhibitors Use in A Low Socioeconomic SettingDocument11 pagesChallenges of Sodium-Glucose Transporter-2 Inhibitors Use in A Low Socioeconomic SettinglivtbuenoNo ratings yet
- hr2008109 PDFDocument10 pageshr2008109 PDFKumarsai DurusojuNo ratings yet
- MinaDocument6 pagesMinaminamoharebNo ratings yet
- Xue 2021Document11 pagesXue 2021Camilla RequiãoNo ratings yet
- EUA 2019 Outcomes of SGLT2 Inhibitors Use in Diabetic RenalDocument4 pagesEUA 2019 Outcomes of SGLT2 Inhibitors Use in Diabetic RenalLaura GarciaNo ratings yet
- HypertensionDocument7 pagesHypertensionrohayatjohnNo ratings yet
- Quercetin PankreasDocument7 pagesQuercetin PankreasAlmas TNo ratings yet
- Semaglutide and Cardiovascular Outcomes in Patients With Type 2 DiabetesDocument11 pagesSemaglutide and Cardiovascular Outcomes in Patients With Type 2 DiabetesFhirastika AnnishaNo ratings yet
- مقاله انگیسی پایان نامهDocument17 pagesمقاله انگیسی پایان نامهmilad latifiNo ratings yet
- DAPA-HF Full PublicationDocument13 pagesDAPA-HF Full PublicationPutra AchmadNo ratings yet
- Effect of Coenzyme Q10 On Risk of AtheroDocument8 pagesEffect of Coenzyme Q10 On Risk of AtheroKumar KartikeyNo ratings yet
- 10 1016@j Ijcard 2015 05 023Document3 pages10 1016@j Ijcard 2015 05 023Choi Eva Young ShineeNo ratings yet
- Cardiovascular Protection by Sodium Glucose Cotransp 2017 The American JournDocument10 pagesCardiovascular Protection by Sodium Glucose Cotransp 2017 The American JournAlina PopaNo ratings yet
- 2022 Article 1014Document6 pages2022 Article 1014mohammed fayedNo ratings yet
- 2015-Acta PhysiologicaDocument19 pages2015-Acta PhysiologicaFatima Ezzahra ZahrouNo ratings yet
- GliffozinasDocument11 pagesGliffozinasArahiMaflaNo ratings yet
- 228 FullDocument8 pages228 FullJoao GomesNo ratings yet
- Long-Term Follow-Up After Tight Control of Blood Pressure in Type 2 DiabetesDocument12 pagesLong-Term Follow-Up After Tight Control of Blood Pressure in Type 2 DiabetesnovywardanaNo ratings yet
- Angiotensin II-induced UpregulationDocument17 pagesAngiotensin II-induced UpregulationMacarenaNo ratings yet
- Inflammation and Oxidative Stress in Diabetic Kidney Disease: The Targets For SGLT2 Inhibitors and GLP-1 Receptor AgonistsDocument38 pagesInflammation and Oxidative Stress in Diabetic Kidney Disease: The Targets For SGLT2 Inhibitors and GLP-1 Receptor AgonistsPawan MishraNo ratings yet
- Schulman2006 PDFDocument13 pagesSchulman2006 PDFPROF. ERWIN M. GLOBIO, MSITNo ratings yet
- Cilostazol Prevents Foot Ulcers in Diabetic Patients With Peripheral Vascular DiseaseDocument4 pagesCilostazol Prevents Foot Ulcers in Diabetic Patients With Peripheral Vascular DiseaseOcha24 TupamahuNo ratings yet
- Usharani 2008Document8 pagesUsharani 2008sartaeva.aigul1No ratings yet
- 01.cir.90.1.35 6Document8 pages01.cir.90.1.35 6NYONGKERNo ratings yet
- Prof. Yaron Ilan - Glycosphingolipids Improve Glucose Intolerance and Hepatic Steatosis of The Cohen Diabetic RatDocument7 pagesProf. Yaron Ilan - Glycosphingolipids Improve Glucose Intolerance and Hepatic Steatosis of The Cohen Diabetic RatProf. Yaron IlanNo ratings yet
- Effects of Diabetes On Apoptosis and Mitosis in Rat HippocampusDocument9 pagesEffects of Diabetes On Apoptosis and Mitosis in Rat HippocampusFrancelia Quiñonez RuvalcabaNo ratings yet
- Ask - 0804iDocument15 pagesAsk - 0804iDavid Cahyo WibisonoNo ratings yet
- Matsushita 2010Document7 pagesMatsushita 2010Arankesh MNo ratings yet
- Research Article: Improving The Reliability and Utility of Streptozotocin-Induced Rat Diabetic ModelDocument15 pagesResearch Article: Improving The Reliability and Utility of Streptozotocin-Induced Rat Diabetic ModelSipend AnatomiNo ratings yet
- Atorvastatina y HuesosDocument6 pagesAtorvastatina y HuesosdrasabrinavNo ratings yet
- Experimental Biology and MedicineDocument11 pagesExperimental Biology and MedicineYunitasya GuspiraNo ratings yet
- Akizawa 2009Document9 pagesAkizawa 2009PROF. ERWIN M. GLOBIO, MSITNo ratings yet
- The Legacy Effect of Early Intensive Glycemic ControlDocument9 pagesThe Legacy Effect of Early Intensive Glycemic ControlSouradipta GangulyNo ratings yet
- Impact of Type 1 Diabetes Ob CF To Myofibroblasts PDFDocument7 pagesImpact of Type 1 Diabetes Ob CF To Myofibroblasts PDFRaji SivarupaNo ratings yet
- tmp3CAB TMPDocument16 pagestmp3CAB TMPFrontiersNo ratings yet
- tmpCE8C TMPDocument19 pagestmpCE8C TMPFrontiersNo ratings yet
- tmpFFE0 TMPDocument6 pagestmpFFE0 TMPFrontiersNo ratings yet
- tmpE7E9 TMPDocument14 pagestmpE7E9 TMPFrontiersNo ratings yet
- tmp6F0E TMPDocument12 pagestmp6F0E TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- tmp80F6 TMPDocument24 pagestmp80F6 TMPFrontiersNo ratings yet
- tmpEFCC TMPDocument6 pagestmpEFCC TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- tmpF3B5 TMPDocument15 pagestmpF3B5 TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmp72FE TMPDocument8 pagestmp72FE TMPFrontiersNo ratings yet
- tmpF407 TMPDocument17 pagestmpF407 TMPFrontiersNo ratings yet
- tmpC0A TMPDocument9 pagestmpC0A TMPFrontiersNo ratings yet
- tmp60EF TMPDocument20 pagestmp60EF TMPFrontiersNo ratings yet
- tmp8B94 TMPDocument9 pagestmp8B94 TMPFrontiersNo ratings yet
- tmp6382 TMPDocument8 pagestmp6382 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmp4B57 TMPDocument9 pagestmp4B57 TMPFrontiersNo ratings yet
- tmp9D75 TMPDocument9 pagestmp9D75 TMPFrontiersNo ratings yet
- tmp37B8 TMPDocument9 pagestmp37B8 TMPFrontiersNo ratings yet
- tmpC30A TMPDocument10 pagestmpC30A TMPFrontiersNo ratings yet
- tmpD1FE TMPDocument6 pagestmpD1FE TMPFrontiersNo ratings yet
- tmpB1BE TMPDocument9 pagestmpB1BE TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- tmpA0D TMPDocument9 pagestmpA0D TMPFrontiersNo ratings yet
- Tmp75a7 TMPDocument8 pagesTmp75a7 TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmp2F3F TMPDocument10 pagestmp2F3F TMPFrontiersNo ratings yet
- Water Pinch PresentationDocument14 pagesWater Pinch PresentationDafiMaboNo ratings yet
- Operation & Service Manual For Cable Tensiometer: SeriesDocument28 pagesOperation & Service Manual For Cable Tensiometer: SeriesJonatan BernalNo ratings yet
- Lighting SchemesDocument7 pagesLighting SchemesSharath CherryNo ratings yet
- Https WWW - Joinpaknavy.gov - PK Web Checkstatus Rollno 410219516621 PDFDocument1 pageHttps WWW - Joinpaknavy.gov - PK Web Checkstatus Rollno 410219516621 PDFZainab KhatoonNo ratings yet
- Chapter 6 Basic Heat TransferDocument7 pagesChapter 6 Basic Heat TransferGabo MarquezNo ratings yet
- Bio Inorganic ChemistryDocument2 pagesBio Inorganic ChemistryMeghna KumarNo ratings yet
- Mechanical Engineering Conference ProgramDocument40 pagesMechanical Engineering Conference Programirinuca12No ratings yet
- TCP Operational Overview and The TCP Finite State Machine (FSM)Document4 pagesTCP Operational Overview and The TCP Finite State Machine (FSM)Mayank JaitlyNo ratings yet
- Ajmera - Treon - FF - R4 - 13-11-17 FinalDocument45 pagesAjmera - Treon - FF - R4 - 13-11-17 FinalNikita KadamNo ratings yet
- Programming structures if, for and while loopsDocument16 pagesProgramming structures if, for and while loopsFrancisco AristizabalNo ratings yet
- Post GreeDocument15 pagesPost GreeDwi PraptiNo ratings yet
- ISO 11957 1996 en PreviewDocument5 pagesISO 11957 1996 en PreviewHoang TraNo ratings yet
- Pines City National High School Science 10 Quarter 2 Week 1 Answer SheetsDocument8 pagesPines City National High School Science 10 Quarter 2 Week 1 Answer SheetsAaron BalsaNo ratings yet
- Paracetamol Overdose: BW 40 KG Without Fluid RestrictionDocument2 pagesParacetamol Overdose: BW 40 KG Without Fluid RestrictionAndy TanNo ratings yet
- Homework1 PDFDocument3 pagesHomework1 PDFYuanhao LiuNo ratings yet
- BIOLOGY Paper 1 Marking Scheme Asumbi Girls Final Prediction 2022Document4 pagesBIOLOGY Paper 1 Marking Scheme Asumbi Girls Final Prediction 2022balozi training InstituteNo ratings yet
- Problem #1: Session #19: Homework SolutionsDocument4 pagesProblem #1: Session #19: Homework SolutionsMD Abu RaselNo ratings yet
- The I AM 22 Chakra ChartDocument8 pagesThe I AM 22 Chakra ChartMarina G. Giamalidi100% (22)
- Time Signature - WikipediaDocument17 pagesTime Signature - WikipediaDiana GhiusNo ratings yet
- Abstract (Lab 2) Ionization ConstantDocument12 pagesAbstract (Lab 2) Ionization Constantmirdza94No ratings yet
- Chapter 13: The Electronic Spectra of ComplexesDocument42 pagesChapter 13: The Electronic Spectra of ComplexesAmalia AnggreiniNo ratings yet
- Ef TechnologyDocument2 pagesEf TechnologyAdarsha SarpangalaNo ratings yet
- Testing of Semifinished Products of Thermoplastics Bases - Indications Directive DVS 2201-1Document4 pagesTesting of Semifinished Products of Thermoplastics Bases - Indications Directive DVS 2201-1OscarNo ratings yet
- DCT Dual Clutch TransmissionDocument16 pagesDCT Dual Clutch TransmissionSudharshan SrinathNo ratings yet
- Nov. AbwDocument50 pagesNov. Abwjbyarkpawolo70No ratings yet
- Jm-10 Operation Manual Rev02 UnlockedDocument121 pagesJm-10 Operation Manual Rev02 UnlockedAlan Jimenez GonzalezNo ratings yet
- Solidworks Flow SimulationDocument7 pagesSolidworks Flow SimulationpatrickNX94200% (1)
- Richard A. Nyquist and Ronald O. Kagel (Auth.) - Handbook of Infrared and Raman Spectra of Inorganic Compounds and Organic Salts. Infrared Spectra of Inorganic Compounds-Academic Press (1971)Document499 pagesRichard A. Nyquist and Ronald O. Kagel (Auth.) - Handbook of Infrared and Raman Spectra of Inorganic Compounds and Organic Salts. Infrared Spectra of Inorganic Compounds-Academic Press (1971)Patrícia Bodanese PratesNo ratings yet
- Catalogo Carbones Helwig GDE-006Document17 pagesCatalogo Carbones Helwig GDE-006Sergio HernandezNo ratings yet
- 9 CE AmplifierDocument5 pages9 CE AmplifierAnsh PratapNo ratings yet