Professional Documents
Culture Documents
Brochure Pop
Uploaded by
FilbertaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Brochure Pop
Uploaded by
FilbertaCopyright:
Available Formats
tive tissue e.g.
Marfan syndrome and Ehlers-Danlos
syndrome
Pelvic Organ Prolapse
A Guide for Women
1. What is pelvic organ prolapse?
2. What causes pelvic organs to prolapse?
3. Where can a prolapse occur?
4. How bad is my prolapse?
5. How can prolapse be treated?
6. What surgical approach is right for me?
7. Is it necessary to use a graft material during the
surgery?
8. How successful is surgery?
What is pelvic organ prolapse?
This condition refers to the bulging or herniation of one or
more pelvic organs into or out of the vagina. The pelvic organs consist of the uterus, vagina, bowel and bladder. Pelvic
organ prolapse occurs when the muscles, ligaments and fascia (a network of supporting tissue) that hold these organs
in their correct positions become weakened.
Symptoms include:
a heavy dragging feeling in the vagina or lower back
feeling of a lump in the vagina or outside the vagina
urinary symptoms such as slow urinary stream, a
feeling of incomplete bladder emptying, urinary frequency or urgent desire to pass urine, and urinary
stress incontinence
Where can a prolapse occur?
A prolapse may arise in the front wall of the vagina (anterior
compartment), back wall of the vagina (posterior compartment), the uterus or top of the vagina (apical compartment).
Many women have a prolapse in more than one compartment at the same time.
Normal anatomy, no prolapse
uterus
rectum
bladder
pelvic floor
muscle
pubic bone
Prolapse of the Anterior compartment
This is the most common type of prolapse, and involves the
bladder and /or urethra bulging into the vagina. Your doctor
may refer to it as cystocele or cysto-urethrocele.
Anterior Compartment prolapse
bowel symptoms, such as difficulty moving the bowel
or a feeling of not emptying properly, or needing to
press on the vaginal wall to empty the bowel
uterus
rectum
discomfort during sexual intercourse
What causes pelvic organs to prolapse?
The main cause is damage to the nerves, ligaments and muscles which support the pelvic organs and may result from
the following:
Pregnancy and childbirth are considered to be major factors leading to weakening of the vagina and its
supports. Prolapse affects about one in three women
who have had one or more children. A prolapse may
occur during or shortly after a pregnancy or may take
many years to develop. However, it is important to
emphasize that only 1 out of 9 women (11%) will ever
need surgery for prolapse in their lifetime
Aging and menopause may cause further weakening
of the pelvic floor structures
Conditions that cause excessive pressure on the pelvic floor like obesity, chronic cough, chronic constipation, heavy lifting and straining
Some women may have an inherited risk for prolapse,
while some diseases affect the strength of connec-
bladder
Prolapse of the Posterior compartment
This is when the lower part of the large bowel (rectum)
bulges into the back wall of the vagina (which your doctor
may refer to as rectocele) and / or part of the small intestine bulges into the upper part of the back wall of the vagina
(which your doctor may refer to as enterocele).
I U G A O f f i c e | o f f i c e @ i u g a . o r g | w w w. i u g a . o r g
2011
Posterior Compartment prolapse
rectum
treatment if they have no symptoms or discomfort.
If you have been diagnosed with a prolapse, try and
avoid heavy lifting, chronic straining e.g. with constipation, and gaining excess weight as these can cause
your prolapse to worsen.
Pessary: Pessaries are vaginal devices that come
in various shapes and sizes. Pessaries help by providing mechanical support to the prolapsed organs, thus relieving symptoms. Pessaries are most
suitable if you wish to delay or avoid surgery, e.g.
if your family is not yet complete or if you have
medical problems that will make surgery a risk.
Pessaries require fitting by your health care provider
and may require some trial and error before the most
suitable size and type is found for you. It is possible to
remain sexually active with some types of pessaries
in situ.
Ring Pessary
Prolapse of the apical compartment
Uterine prolapse this occurs when the uterus (womb)
drops or herniates into the vagina. This is the second most
common form of prolapse.
uterus
Uterine prolapse
rectum
bladder
rectum
bladder
uterus
pubic bone
Vaginal vault prolapse following a hysterectomy, the top
of the vagina may collapse downwards, (rather like the toe
of a sock turning inside out) falling towards or out of the
vaginal opening.
How bad is my prolapse?
Many women (up to 40%) have a minor degree of prolapse
with minimal or no symptoms. Your physician will take a
complete medical history and perform a vaginal examination to determine prolapse severity and grade. Different
physicians utilize different grading systems and your doctor will explain this to you.
How can pelvic organ prolapse be treated?
Treatment options can be categorized into non-surgical and
surgical options.
Non Surgical Treatment Options
Do nothing: Prolapse is rarely a life-threatening condition and many women will choose not to have any
Pelvic floor exercises (Kegel exercises): Exercising
your weakened pelvic floor muscles may help improve or prevent the worsening of early stages of prolapse. Just as any exercise program, pelvic floor exercises require time, motivation and proper technique.
Please see the pelvic floor exercises leaflet for more
information.
Surgical Treatment Options
For women with symptomatic prolapse, a surgical repair
may be offered. Your surgeon will recommend the most
appropriate surgical treatment for you based on a number
of factors including your age, previous surgical history, severity of prolapse and your general health. There are two
main options: reconstructive surgery and vaginal closure
surgery.
Reconstructive Surgical Repair
The purpose of pelvic reconstructive surgery is to
restore your pelvic organs to their natural position
while retaining sexual function. There are many different ways to accomplish the surgery including:
Vaginal approach
Abdominal approach (through an abdominal
incision)
Laparoscopic (keyhole)
Robotic
I U G A O f f i c e | o f f i c e @ i u g a . o r g | w w w. i u g a . o r g
2011
Vaginal Closure Surgery (Colpocliesis)
Your doctor may recommend this surgery if you
have a severe prolapse, are not sexually active and
have no intention of becoming sexually active in the
future, or if you are medically unfit for reconstructive surgery. During this procedure your surgeon
will stitch the vaginal walls together thus preventing
the prolapse from re-occurring. The main advantage
of this procedure is its short surgical time and quick
recovery. Success rates for this type of procedure are
90 95%.
What surgical approach is right for me?
There is no single best approach for all patients. The approach for your particular surgery will depend on many
factors, including your history, your surgeons training, and
experience with different approaches and your preference.
Your surgeon will discuss with you the various options and
will recommend the type of surgery best suited to your condition and needs. Each repair is individualized, even two
different women with the same prolapse may have different
needs.
Vaginal approach
This usually involves making an incision in the vagina, separating the prolapsed organ involved from the vaginal wall
and using stitches and / or mesh to strengthen and repair
the vagina. Permanent stitches may also be placed into the
top of the vagina or into the cervix and attached to strong
ligaments in the pelvis to provide support to the uterus or
vaginal vault (these are termed sacrospinous or uterosacral
ligament suspensions).
Abdominal approach
This involves making an incision in the abdomen and using
sutures and / or graft materials to support the vagina, vaginal vault or uterus. In a sacrocolpopexy, a prolapsed vaginal vault is supported using mesh attached to the sacrum.
Again, there are many different procedures and your doctor
will explain these in detail to you.
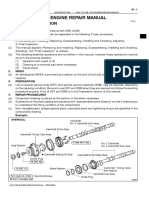
Sacrocolpopexy
L5
hip bone
sacrum
rectum
bladder
vagina
may be due to continued factors which have caused the initial prolapse e.g. constipation and weak tissues.
What if I havent completed my family?
It is generally advised to withhold the definitive prolapse
repair surgery until completion of your family. In the meantime, conservative management such as pelvic floor exercises or the use of vaginal pessary may be employed.
Laparoscopic and robotic approaches
They offer repairs similar procedures to the open abdominal approach but often with quicker recovery time and
smaller scars. At present, robotic surgery is only available
in a few centers.
Is it necessary to use a graft material during the surgery?
Not all repairs require a graft. Traditionally, grafts are used
in repeated surgeries and where significant risk factors for
failure exist. The graft may be absorbable, made from animal tissue (biologic) and will disappear gradually over time,
or non-absorbable synthetic material which stays permanently in your body. Some grafts are a combination of absorbable and non-absorbable materials. You should discuss
the pros and cons of their use in detail with your surgeon.
How successful is surgery?
Approximately 75% of women having vaginal surgery and
90 to 95% having an abdominal approach, will have a longterm cure of their prolapse symptoms. Recurrent prolapse
The information contained in this brochure is intended to be used for educational purposes only. It is not intended to be used for the diagnosis or treatment of
any specific medical condition, which should only be done by a qualified physician or other health care professional.
I U G A O f f i c e | o f f i c e @ i u g a . o r g | w w w. i u g a . o r g
2011
You might also like
- The Saki Monkey: Sakis Are Small-Sized Monkeys With Long, Bushy Tails They Live in The Trees of The Rain ForestsDocument6 pagesThe Saki Monkey: Sakis Are Small-Sized Monkeys With Long, Bushy Tails They Live in The Trees of The Rain ForestsFilbertaNo ratings yet
- 101 Template PPT Cute Lovely Calm Bird FlowerDocument2 pages101 Template PPT Cute Lovely Calm Bird FlowerFilbertaNo ratings yet
- 0021 Timeline PPT TemplateDocument4 pages0021 Timeline PPT TemplateFilbertaNo ratings yet
- Anatomy Physiology PregnancyDocument45 pagesAnatomy Physiology PregnancyFilbertaNo ratings yet
- Jadual Jaga Obgyn FixedDocument1 pageJadual Jaga Obgyn FixedFilbertaNo ratings yet
- Review of Pelvic Anatomy BMJDocument79 pagesReview of Pelvic Anatomy BMJFilbertaNo ratings yet
- Acog TumorDocument58 pagesAcog TumorFilbertaNo ratings yet
- The Female Reproductive SystemDocument40 pagesThe Female Reproductive SystemFilbertaNo ratings yet
- Pelvic Organ Prolapse: Obstetrics & GynecologyDocument46 pagesPelvic Organ Prolapse: Obstetrics & GynecologymanognaaaaNo ratings yet
- 8nutrition in PregnancyDocument16 pages8nutrition in PregnancyFilbertaNo ratings yet
- Jadual Jaga Obgyn FixedDocument1 pageJadual Jaga Obgyn FixedFilbertaNo ratings yet
- 9 HPV and Cervical Mechanisms Johns Hopkins B WellsDocument29 pages9 HPV and Cervical Mechanisms Johns Hopkins B WellsFilbertaNo ratings yet
- Scores Killed in Iraqi Army Raids in Anbar ProvinceDocument2 pagesScores Killed in Iraqi Army Raids in Anbar ProvinceFilbertaNo ratings yet
- PrintDocument3 pagesPrintFilbertaNo ratings yet
- Cervix BenignDocument5 pagesCervix BenignFilbertaNo ratings yet
- TaiwanDocument1 pageTaiwanFilbertaNo ratings yet
- PrintDocument3 pagesPrintFilbertaNo ratings yet
- Pediatric Leukemia Resident Education Lecture SeriesDocument42 pagesPediatric Leukemia Resident Education Lecture SeriesFilbertaNo ratings yet
- France Put On High Alert After Attack On Chemical PlantDocument5 pagesFrance Put On High Alert After Attack On Chemical PlantFilbertaNo ratings yet
- Pediatric Leukemia Resident Education Lecture SeriesDocument42 pagesPediatric Leukemia Resident Education Lecture SeriesFilbertaNo ratings yet
- Greece Referendum to Decide More than Austerity: Future as Western NationDocument7 pagesGreece Referendum to Decide More than Austerity: Future as Western NationFilbertaNo ratings yet
- Pediatric Leukemia Resident Education Lecture SeriesDocument42 pagesPediatric Leukemia Resident Education Lecture SeriesFilbertaNo ratings yet
- Political Fears of A RussiaDocument5 pagesPolitical Fears of A RussiaFilbertaNo ratings yet
- TaiwanDocument1 pageTaiwanFilbertaNo ratings yet
- Sao Paulo Is A SwellingDocument3 pagesSao Paulo Is A SwellingFilbertaNo ratings yet
- Humanitarian CrisesDocument4 pagesHumanitarian CrisesFilbertaNo ratings yet
- Israel's PR Gaffes Expose Its Racist AtmosphereDocument6 pagesIsrael's PR Gaffes Expose Its Racist AtmosphereFilbertaNo ratings yet
- Sri Lankan President Dissolves ParliamentDocument3 pagesSri Lankan President Dissolves ParliamentFilbertaNo ratings yet
- Obama Allows Hostage Families to Pay Ransoms Without Threat of ProsecutionDocument4 pagesObama Allows Hostage Families to Pay Ransoms Without Threat of ProsecutionFilbertaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Page 17 - Word Connection, LiaisonsDocument2 pagesPage 17 - Word Connection, Liaisonsstarskyhutch0% (1)
- Political Philosophy and Political Science: Complex RelationshipsDocument15 pagesPolitical Philosophy and Political Science: Complex RelationshipsVane ValienteNo ratings yet
- An Analysis of Students Pronounciation Errors Made by Ninth Grade of Junior High School 1 TengaranDocument22 pagesAn Analysis of Students Pronounciation Errors Made by Ninth Grade of Junior High School 1 TengaranOcta WibawaNo ratings yet
- Ethnic Conflicts and PeacekeepingDocument2 pagesEthnic Conflicts and PeacekeepingAmna KhanNo ratings yet
- Toxicology: General Aspects, Types, Routes of Exposure & AnalysisDocument76 pagesToxicology: General Aspects, Types, Routes of Exposure & AnalysisAsma SikanderNo ratings yet
- B2 WBLFFDocument10 pagesB2 WBLFFflickrboneNo ratings yet
- The Five Laws of Light - Suburban ArrowsDocument206 pagesThe Five Laws of Light - Suburban Arrowsjorge_calvo_20No ratings yet
- Excel Keyboard Shortcuts MasterclassDocument18 pagesExcel Keyboard Shortcuts MasterclassluinksNo ratings yet
- CH 19Document56 pagesCH 19Ahmed El KhateebNo ratings yet
- Independent Study of Middletown Police DepartmentDocument96 pagesIndependent Study of Middletown Police DepartmentBarbara MillerNo ratings yet
- Joint School Safety Report - Final ReportDocument8 pagesJoint School Safety Report - Final ReportUSA TODAY NetworkNo ratings yet
- Resarch Paper On Franchising Business MacobDocument8 pagesResarch Paper On Franchising Business MacobAngelika Capa ReyesNo ratings yet
- 2010 Economics Syllabus For SHSDocument133 pages2010 Economics Syllabus For SHSfrimpongbenardghNo ratings yet
- Arx Occasional Papers - Hospitaller Gunpowder MagazinesDocument76 pagesArx Occasional Papers - Hospitaller Gunpowder MagazinesJohn Spiteri GingellNo ratings yet
- 12 Preliminary Conference BriefDocument7 pages12 Preliminary Conference Briefkaizen shinichiNo ratings yet
- Obtaining Workplace InformationDocument4 pagesObtaining Workplace InformationJessica CarismaNo ratings yet
- Sangam ReportDocument37 pagesSangam ReportSagar ShriNo ratings yet
- Apple NotesDocument3 pagesApple NotesKrishna Mohan ChennareddyNo ratings yet
- Food Product Development - SurveyDocument4 pagesFood Product Development - SurveyJoan Soliven33% (3)
- Contract Costing and Operating CostingDocument13 pagesContract Costing and Operating CostingGaurav AggarwalNo ratings yet
- Microeconomics Study Guide for CA-CMA-CS ExamDocument14 pagesMicroeconomics Study Guide for CA-CMA-CS ExamCA Suman Gadamsetti75% (4)
- How To Use This Engine Repair Manual: General InformationDocument3 pagesHow To Use This Engine Repair Manual: General InformationHenry SilvaNo ratings yet
- La TraviataDocument12 pagesLa TraviataEljona YzellariNo ratings yet
- TAX & DUE PROCESSDocument2 pagesTAX & DUE PROCESSMayra MerczNo ratings yet
- Barra de Pinos 90G 2x5 P. 2,54mm - WE 612 010 217 21Document2 pagesBarra de Pinos 90G 2x5 P. 2,54mm - WE 612 010 217 21Conrado Almeida De OliveiraNo ratings yet
- Phasin Ngamthanaphaisarn - Unit 3 - Final Assessment Literary EssayDocument4 pagesPhasin Ngamthanaphaisarn - Unit 3 - Final Assessment Literary Essayapi-428138727No ratings yet
- Leku Pilli V Anyama (Election Petition No 4 of 2021) 2021 UGHCEP 24 (8 October 2021)Document52 pagesLeku Pilli V Anyama (Election Petition No 4 of 2021) 2021 UGHCEP 24 (8 October 2021)Yokana MugabiNo ratings yet
- ROCKET STOVE DESIGN GUIDEDocument9 pagesROCKET STOVE DESIGN GUIDEfrola5100% (2)
- Search Inside Yourself PDFDocument20 pagesSearch Inside Yourself PDFzeni modjo02No ratings yet
- IJAKADI: A Stage Play About Spiritual WarfareDocument9 pagesIJAKADI: A Stage Play About Spiritual Warfareobiji marvelous ChibuzoNo ratings yet