Professional Documents
Culture Documents
PBM Module1 MTP Template 0
Uploaded by
1234chocoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PBM Module1 MTP Template 0
Uploaded by
1234chocoCopyright:
Available Formats
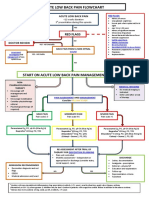
Massive transfusion protocol (MTP) template
The information below, developed by consensus, broadly covers areas that should be included in a local MTP. This
template can be used to develop an MTP to meet the needs of the local institution's patient population and resources
Senior clinician determines that patient meets criteria for MTP activation
Baseline:
Full blood count, coagulation screen (PT, INR, APTT, fibrinogen), biochemistry,
arterial blood gases
OPTIMISE:
oxygenation
cardiac output
tissue perfusion
metabolic state
MONITOR
(every 3060 mins):
Notify transfusion laboratory (insert contact no.) to:
full blood count
coagulation screen
ionised calcium
arterial blood gases
Activate MTP
Laboratory staff
Notify haematologist/transfusion specialist
Prepare and issue blood components
as requested
Anticipate repeat testing and
blood component requirements
Minimise test turnaround times
Consider staff resources
Haematologist/transfusion
specialist
Senior clinician
Request:a
AIM FOR:
o 4 units RBC
o 2 units FFP
Consider:a
o 1 adult therapeutic dose platelets
o tranexamic acid in trauma patients
Include:a
o cryoprecipitate if fibrinogen < 1 g/L
a Or locally agreed configuration
Liaise regularly with laboratory
and clinical team
Assist in interpretation of results, and
advise on blood component support
Bleeding controlled?
YES
NO
Notify transfusion laboratory to:
Cease MTP
temperature > 350C
pH > 7.2
base excess < 6
lactate < 4 mmol/L
Ca2+ > 1.1 mmol/L
platelets > 50 109/L
PT/APTT < 1.5 normal
INR 1.5
fibrinogen > 1.0 g/L
Suggested criteria for activation of MTP
Actual or anticipated 4 units RBC in < 4 hrs, + haemodynamically unstable, +/ anticipated ongoing bleeding
Severe thoracic, abdominal, pelvic or multiple long bone trauma
Major obstetric, gastrointestinal or surgical bleeding
Initial management of bleeding
Identify cause
Initial measures:
- compression
- tourniquet
- packing
Surgical assessment:
- early surgery or angiography to stop bleeding
Specific surgical considerations
If significant physiological derangement, consider
damage control surgery or angiography
Cell salvage
Consider use of cell salvage where appropriate
Resuscitation
Avoid hypothermia, institute active warming
Avoid excessive crystalloid
Tolerate permissive hypotension (BP 80100 mmHg systolic)
until active bleeding controlled
Do not use haemoglobin alone as a transfusion trigger
Special clinical situations
Warfarin:
add vitamin K, prothrombinex/FFP
Obstetric haemorrhage:
early DIC often present; consider cryoprecipitate
Head injury:
aim for platelet count > 100 109/L
permissive hypotension contraindicated
Considerations for use of rFVIIab
Dosage
Platelet count < 50 x 109/L
1 adult therapeutic dose
INR > 1.5
FFP 15 mL/kga
Fibrinogen < 1.0 g/L
cryoprecipitate 34 ga
Tranexamic acid
loading dose 1 g over 10
min, then infusion of 1 g
over 8 hrs
a Local transfusion laboratory to advise on number of units
needed to provide this dose
ABG
INR
DIC
RBC
arterial blood gas
international normalised ratio
disseminated intravascular coagulation
red blood cell
The routine use of rFVIIa in trauma patients is not recommended due to
its lack of effect on mortality (Grade B) and variable effect on morbidity
(Grade C). Institutions may choose to develop a process for the use of
rFVIIa where there is:
uncontrolled haemorrhage in salvageable patient, and
failed surgical or radiological measures to control bleeding, and
adequate blood component replacement, and
pH > 7.2, temperature > 340C.
Discuss dose with haematologist/transfusion specialist
b rFVIIa
FFP
BP
PT
rFVlla
is not licensed for use in this situation; all use must be part of practice review.
fresh frozen plasma
blood pressure
prothrombin time
activated recombinant factor VII
APTT
MTP
FBC
activated partial thromboplastin time
massive transfusion protocol
full blood count
You might also like
- PBM Module1 MTP Template 0Document2 pagesPBM Module1 MTP Template 0Daniela Marie RonquilloNo ratings yet
- Local Media5289763584533511516Document8 pagesLocal Media5289763584533511516Haniya KhanNo ratings yet
- Blood TransfusionDocument58 pagesBlood Transfusionmsat72100% (12)
- MASSIVE TRANSFUSION PROTOCOLDocument17 pagesMASSIVE TRANSFUSION PROTOCOLkrgdurai100% (1)
- Blood TransfusionDocument57 pagesBlood Transfusionibzshan_No ratings yet
- Evaluation of Coagulation Disorders - FINALDocument34 pagesEvaluation of Coagulation Disorders - FINALRatna Stephenson BasimallaNo ratings yet
- BloodDocument49 pagesBloodvruttika parmar100% (3)
- Laboratory Control of Anticoagulant Therapy TestsDocument69 pagesLaboratory Control of Anticoagulant Therapy TestsTusabe FredNo ratings yet
- 4.massive HemorrhageDocument44 pages4.massive HemorrhageyeabsraNo ratings yet
- ATLS Power Point PDFDocument54 pagesATLS Power Point PDFRizky LumalessilNo ratings yet
- 7.hemostasis, Surgical BleedingDocument61 pages7.hemostasis, Surgical Bleedingoliyad alemayehuNo ratings yet
- CLINICAL ASPECTS OF BLOOD TRANSFUSIONDocument37 pagesCLINICAL ASPECTS OF BLOOD TRANSFUSIONRaras P P100% (1)
- Massive Transfusion ProtocolDocument1 pageMassive Transfusion Protocolabinash chihnaraNo ratings yet
- Hemostatic Strategies For Minimizing Mortality in Major Blood LossDocument26 pagesHemostatic Strategies For Minimizing Mortality in Major Blood LossJonathan wiradinataNo ratings yet
- Blood TransfusionDocument52 pagesBlood TransfusionAnonymous GC8uMx367% (3)
- NHS Lanarkshire Major Haemorrhage GuideDocument3 pagesNHS Lanarkshire Major Haemorrhage GuideleicesterbugNo ratings yet
- Emily Antes - 2018 Fall MeetDocument41 pagesEmily Antes - 2018 Fall MeetSyed Shahrul Naz Syed100% (1)
- Blood & Blood Products GuideDocument52 pagesBlood & Blood Products Guidewellawalalasith100% (1)
- Massive Transfusion Protocol 2017Document9 pagesMassive Transfusion Protocol 2017RosNo ratings yet
- Blood and Blood Product (F)Document50 pagesBlood and Blood Product (F)bharat singhNo ratings yet
- Blood Transfusion Guide: Types, Storage, Indications & ComplicationsDocument61 pagesBlood Transfusion Guide: Types, Storage, Indications & ComplicationsshikhaNo ratings yet
- Blood Transfusion Guidelines - 112Document55 pagesBlood Transfusion Guidelines - 112Dhaneswara AdhyatamaNo ratings yet
- 4 Component TherapyDocument50 pages4 Component TherapyJayniel MollenoNo ratings yet
- Anticoagulation For Ecmo 2019Document40 pagesAnticoagulation For Ecmo 2019Hoa Cỏ ĐậuNo ratings yet
- An Overview of Therapeutic Plasma ExchangeDocument65 pagesAn Overview of Therapeutic Plasma ExchangesayednourNo ratings yet
- Peter Hudson Blood TransfusionDocument29 pagesPeter Hudson Blood TransfusionRyan-Jay AbolenciaNo ratings yet
- Coagulopathy in Trauma: Rudy Alvarez, M.DDocument28 pagesCoagulopathy in Trauma: Rudy Alvarez, M.DRudy AlvarezNo ratings yet
- Damage Control ResuscitationDocument24 pagesDamage Control ResuscitationPaulShaneHerreraZorrillaNo ratings yet
- Blood Transfusion Peter HudsonDocument21 pagesBlood Transfusion Peter HudsonWai YanNo ratings yet
- Platelet, FFP and Cryoprecipitate Transfusion in Emergency Room by DR Riaz AhamedDocument31 pagesPlatelet, FFP and Cryoprecipitate Transfusion in Emergency Room by DR Riaz AhamedAETCM Emergency medicineNo ratings yet
- Rational Use of Blood ComponentsDocument43 pagesRational Use of Blood ComponentsMohandoss MurugesanNo ratings yet
- AtlsDocument32 pagesAtlsMahesh RajwalNo ratings yet
- Plasma P Here SisDocument24 pagesPlasma P Here SisDani DanyNo ratings yet
- Massive Haemorrhage PPT en PDFDocument18 pagesMassive Haemorrhage PPT en PDFviaereaNo ratings yet
- Blood TransfusionDocument28 pagesBlood TransfusionPORTRAIT OF A NURSENo ratings yet
- Whole Blood CollectionDocument16 pagesWhole Blood CollectionShemiza BalmacoonNo ratings yet
- Pediatric Hematology Oncology Ward Officer HandbookDocument40 pagesPediatric Hematology Oncology Ward Officer HandbookLetchumana KrishnanNo ratings yet
- Optimal Anesthesia Management for Live Donor Liver Transplantation DonorsDocument38 pagesOptimal Anesthesia Management for Live Donor Liver Transplantation Donorsdrgauravgoyal9275No ratings yet
- DCR PresentationDocument34 pagesDCR PresentationHera YunataNo ratings yet
- Damage Control Resuscitation (DCR) : Respati Suryanto Dradjat Fkub/Rs Saiful Anwar MalangDocument34 pagesDamage Control Resuscitation (DCR) : Respati Suryanto Dradjat Fkub/Rs Saiful Anwar Malangbenny christantoNo ratings yet
- Hemostasis & Blood Coagulation: First Teaching Hospital Zhengzhou UnivDocument46 pagesHemostasis & Blood Coagulation: First Teaching Hospital Zhengzhou Univapi-19916399No ratings yet
- Hemostasis and Transfusion Medicine GuideDocument83 pagesHemostasis and Transfusion Medicine GuideJesserene Mangulad SorianoNo ratings yet
- PT, Aptt, TTDocument44 pagesPT, Aptt, TTswaraj sharmaNo ratings yet
- Disseminated Intravascular CoagulationDocument37 pagesDisseminated Intravascular CoagulationMuhammad Adeeb100% (1)
- Massive Transfusion Protocol: K. Pavenski, MD FRCPC Head, Div. Transfusion Medicine October 31, 2013Document37 pagesMassive Transfusion Protocol: K. Pavenski, MD FRCPC Head, Div. Transfusion Medicine October 31, 2013IlyasHasanNo ratings yet
- PPH Transfusion Strategies NPEC 2017 PDFDocument90 pagesPPH Transfusion Strategies NPEC 2017 PDFRahmayanti YuliaNo ratings yet
- Pediatric Hematology Oncology Ward Officer HandbookDocument40 pagesPediatric Hematology Oncology Ward Officer HandbookAnonymous FSUnLYr4yNo ratings yet
- BT CT PT PTTDocument31 pagesBT CT PT PTTCristineVillablancaNo ratings yet
- Ecmo CoagulationDocument27 pagesEcmo CoagulationblakewilNo ratings yet
- Blood ComponenetsDocument41 pagesBlood Componenetsnighat khanNo ratings yet
- Blood Transfusion KiranDocument34 pagesBlood Transfusion KiranKiran KumarNo ratings yet
- TransfusionDocument3 pagesTransfusionjulissand10No ratings yet
- Nursing Sciences: Pyramid PointsDocument12 pagesNursing Sciences: Pyramid PointsEmmanuel GarciaNo ratings yet
- Transfusión IntraoperatoriaDocument24 pagesTransfusión IntraoperatoriaGiovany Salinas100% (1)
- Terapi Cairan dan Transfusi dalam PerioperatifDocument47 pagesTerapi Cairan dan Transfusi dalam PerioperatifHelend ChildDjNo ratings yet
- Blood Transfusion TherapyDocument38 pagesBlood Transfusion TherapyAnn Merlin JobinNo ratings yet
- PBM (Autosaved)Document36 pagesPBM (Autosaved)dr AmitNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- Pokemon Theme Song 22Document4 pagesPokemon Theme Song 221234chocoNo ratings yet
- Blue Veins Sub Theme TVBDocument4 pagesBlue Veins Sub Theme TVB1234chocoNo ratings yet
- Code Geass - StoriesDocument5 pagesCode Geass - Stories1234chocoNo ratings yet
- Doctor Talk: Communication Practice Role PlaysDocument6 pagesDoctor Talk: Communication Practice Role Plays1234chocoNo ratings yet
- Mbs Quick Guide: JULY 2020Document2 pagesMbs Quick Guide: JULY 20201234chocoNo ratings yet
- Fairy Tail - Main ThemeDocument3 pagesFairy Tail - Main Theme1234chocoNo ratings yet
- QLD Rail Traim PDFDocument1 pageQLD Rail Traim PDF1234chocoNo ratings yet
- Blue BirdDocument7 pagesBlue Bird1234chocoNo ratings yet
- VTE GuidelinesDocument11 pagesVTE Guidelines1234chocoNo ratings yet
- Acute Low Back Pain Flowchart January 2017Document1 pageAcute Low Back Pain Flowchart January 20171234chocoNo ratings yet
- Topical Steroids (Sep 19) PDFDocument7 pagesTopical Steroids (Sep 19) PDF1234chocoNo ratings yet
- Getting the Hospital Job: A Step-by-Step Guide to Applying for Your First PositionDocument41 pagesGetting the Hospital Job: A Step-by-Step Guide to Applying for Your First Position1234chocoNo ratings yet
- # 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in EDDocument7 pages# 3 - Prospective Study of The Diagnostic Accuracy of The Simplify D-Dimer Assay For Pulmonary Embolism in ED1234chocoNo ratings yet
- Topical Steroids (Sep 19) PDFDocument7 pagesTopical Steroids (Sep 19) PDF1234chocoNo ratings yet
- Osteo Infographic FinalDocument1 pageOsteo Infographic Final1234chocoNo ratings yet
- USMLE Flashcards: Anatomy - Side by SideDocument190 pagesUSMLE Flashcards: Anatomy - Side by SideMedSchoolStuff100% (3)
- Herd Immunity'' A Rough Guide PDFDocument6 pagesHerd Immunity'' A Rough Guide PDF1234chocoNo ratings yet
- ImprovingMedAdherenceOlderAdultslyer Final 508CDocument2 pagesImprovingMedAdherenceOlderAdultslyer Final 508CKumar PatilNo ratings yet
- Metro South Intern Training Form (Logan)Document3 pagesMetro South Intern Training Form (Logan)1234chocoNo ratings yet
- 2016 Applicant Guide Web V2Document83 pages2016 Applicant Guide Web V21234chocoNo ratings yet
- A Conceptual Framework For HealthDocument1 pageA Conceptual Framework For Health1234chocoNo ratings yet
- Taking a Social and Cultural History: A Biopsychosocial ApproachDocument3 pagesTaking a Social and Cultural History: A Biopsychosocial Approach1234chocoNo ratings yet
- Managing Mental Illness in Patients From CALD Backgrounds: PsychiatryDocument5 pagesManaging Mental Illness in Patients From CALD Backgrounds: Psychiatry1234chocoNo ratings yet
- Fluids ElectrolytesDocument2 pagesFluids Electrolytes1234chocoNo ratings yet
- FLOWCHART - ARC Adult Cardiorespiratory ArrestDocument1 pageFLOWCHART - ARC Adult Cardiorespiratory Arrest1234chocoNo ratings yet
- Language of PreventionDocument9 pagesLanguage of Prevention1234chocoNo ratings yet
- Clinical Contributions To Addressing The Social Determinants of HealthDocument5 pagesClinical Contributions To Addressing The Social Determinants of Health1234chocoNo ratings yet
- Defining and Assessing Risks To Health PDFDocument20 pagesDefining and Assessing Risks To Health PDF1234chocoNo ratings yet
- The Effects of Social Networks On Disability in Older AustraliansDocument22 pagesThe Effects of Social Networks On Disability in Older Australians1234chocoNo ratings yet
- Postpartal Thrombophlebitis: Client Assessment Data Base Activity/RestDocument8 pagesPostpartal Thrombophlebitis: Client Assessment Data Base Activity/RestLei OrtegaNo ratings yet
- Review of Literature on Prevalence, Causes and Prevention of Dengue FeverDocument16 pagesReview of Literature on Prevalence, Causes and Prevention of Dengue FeverMAHESH KOUJALAGINo ratings yet
- PED2 6.04 Evaluation of The Child With A LimpDocument15 pagesPED2 6.04 Evaluation of The Child With A LimprachelNo ratings yet
- NCMB 312 Rle Week 14 Dengue FeverDocument3 pagesNCMB 312 Rle Week 14 Dengue FeverMada mada DaneNo ratings yet
- DOC-20240110-WA0016.Document176 pagesDOC-20240110-WA0016.Sreeja ReddyNo ratings yet
- Verrucous CarcinomaDocument12 pagesVerrucous Carcinomaanatomimanusia100% (1)
- Batu Saluran Kemih GuideDocument33 pagesBatu Saluran Kemih GuideernamahyuniNo ratings yet
- CASE Study SampleDocument6 pagesCASE Study SampleMary Shane Aragon MoraldeNo ratings yet
- Medical screening tool assesses exercise risksDocument4 pagesMedical screening tool assesses exercise risksRegina MalyszkoNo ratings yet
- Eval Exam - PharmacologyDocument19 pagesEval Exam - Pharmacologysamantha lumapasNo ratings yet
- Tenant Health Declaration FormDocument1 pageTenant Health Declaration FormMirol CapikNo ratings yet
- Rodriguez - Diagnostico Clinico Del Autista PDFDocument6 pagesRodriguez - Diagnostico Clinico Del Autista PDFLuz Dianeth ZapataNo ratings yet
- Cri Du ChatDocument16 pagesCri Du ChatJet LeeNo ratings yet
- Medication SheetDocument4 pagesMedication SheetJasleen AilenNo ratings yet
- T Alimentacion LibroDocument485 pagesT Alimentacion LibrodeadelcarmenNo ratings yet
- Asuhan Keperawatan Pada Lansia Dengan Gangguan Sistem MuskuloskeletalDocument12 pagesAsuhan Keperawatan Pada Lansia Dengan Gangguan Sistem MuskuloskeletalSiti Nuur Jannah100% (1)
- Coagulation DisordersDocument26 pagesCoagulation DisordersLia pramita0% (1)
- Pott DiseaseDocument36 pagesPott DiseaseGiovanna Algu100% (1)
- Jurnal SkoliosisDocument9 pagesJurnal SkoliosisLidya SiahaanNo ratings yet
- Varicose VeinsDocument4 pagesVaricose VeinsNur Hanani KhanNo ratings yet
- ESR Test ExplainedDocument3 pagesESR Test ExplainedbibahNo ratings yet
- Genitourinary UltrasoundDocument215 pagesGenitourinary UltrasoundAnselmus Regie100% (4)
- Renal EmergenciesDocument11 pagesRenal EmergenciesDemuel Dee L. BertoNo ratings yet
- Endo Test Bank 1Document6 pagesEndo Test Bank 1mildred alidon100% (1)
- Older People - Patterns of IllnessDocument4 pagesOlder People - Patterns of IllnessTweenie DalumpinesNo ratings yet
- Dengue Case ReportDocument70 pagesDengue Case ReportGroup 6 MadocsNo ratings yet
- Warfarin: When Taking Warfarin (Blood Thinner)Document2 pagesWarfarin: When Taking Warfarin (Blood Thinner)Mega FebrianaNo ratings yet
- Medicine MCQS JULY 2023 SOLVEDDocument15 pagesMedicine MCQS JULY 2023 SOLVEDLijo JoNo ratings yet
- Uti in WomenDocument8 pagesUti in WomenBhupesh KumarNo ratings yet
- ProstataDocument26 pagesProstatasidney souzaNo ratings yet