Professional Documents
Culture Documents
HSRA: Fourmula One for Health Reform Agenda
Uploaded by
MadsOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HSRA: Fourmula One for Health Reform Agenda
Uploaded by
MadsCopyright:
Available Formats
Health Sector Reform Agenda (HSRA)
The Health Sector Reform Agenda (HSRA) describes the policies, public investments, and organizational changes
needed to improve the way health care is delivered, regulated, and financed in the country. Specifically, the HSRA
seeks to undertake the following:
Provide fiscal autonomy to government hospitals. The conversion of government hospitals into corporate entities
will promote fiscal autonomy by allowing them to collect socialized user fees. This move will take a great chunk off
the DOH's yearly appropriation for hospital operations. Thus, the DOH could use this savings to finance preventive
public health programs. However, there is a need to enhance the capacities of government hospitals such as their
diagnostic equipment, laboratory and medical staff to effectively exercise fiscal autonomy. Such investment must be
cognizant of complimentary capacity provided by public-private networks. Most importantly, safety measures shall
be carefully put into place to protect the interest of the indigents such as enrolling them in the National Health
Insurance Program.
Secure funding for priority public health programs. Budget on a multi-year basis must be provided to eliminate
or significantly reduce the incidence of infectious diseases. The government should also allocate funds to effectively
address emerging health concerns and to advance health promotion and prevention programs. At the same time, the
management capacity and infrastructure of public health programs must be upgraded to ensure that these
investments are effectively utilized. Capacity building is likewise required for these programs to provide technical
leadership over local health systems.
Promote the development of local health systems and ensure their effective performance. Local government
units must enter into cooperative and cost-sharing arrangements to improve local health services. Funds must be
secured to upgrade local health facilities and build local human resource capacities. For more effective performance,
participation of the private sector and volunteer groups must also be tapped. Lastly, appropriate mechanisms for
sustainability and continued delivery of quality care must be developed and institutionalized.
Strengthen the capacities of health regulatory agencies. Health regulatory agencies, namely, the Bureau of Food
and Drug (BFAD), the Bureau of Health Devices and Technology (BHDT), the Bureau of Health Facilities and
Services (BHFS), and the Bureau of Quarantine and International Health Surveillance (BQIHS) must be
strengthened to ensure the safety, quality, accessibility and affordability of health services and products. Public
investments must be made to upgrade the facilities and manpower capability of these agencies, particularly in
standards development, technology assessment and enforcement. To achieve all these, amendments to the laws
governing these agencies are called for.
Expand the coverage of the National Health Insurance Program (NHIP). Social health insurance must be
expanded to widen its reach. Health insurance benefits must be improved to make the program more attractive to
members. As membership expands and benefit spending increases, appropriate mechanisms to ensure quality and
cost effective services must be developed and introduced. Capacities and new administrative structures must also be
developed to allow the Philippine Health Insurance Corporation (PhilHealth) to effectively service more members
and manage increased benefit spending.
These five reform areas are highly interdependent, complementary and therefore should be implemented as a
package. Health financing reforms through NHIP expansion will make hospital autonomy viable and will ensure that
the poor remains protected. Hospital reforms, in turn will free up resources for investments in public health program,
and health regulation at the national and local levels. Effective public health programs and local health systems will
relieve the NHIP from paying for hospitalizations that should otherwise have been prevented or better handled at
primary care facilities.
Implementation of the HSRA demands public investments, policy and organizational changes. The HSRA will
require public investments estimated to amount to P112 billion within a five-year period. It will also require
effective implementation of existing laws and policies like the National Health Insurance Act, the National Drug
Policy and the Local Government Code. The organizational changes needed include the continuing re-engineering of
the DOH and PhilHealth and the formation of inter-local health zones.
Ultimately, HSRA aims to: improve the health status of the people through greater and more effective coverage of
national and local public health programs; increase access to health services especially by the poor; and reduce
financial burden on individual families. It shall be the catalyst that will bring the country toward the realization of a
shared vision of health for all Filipinos.
HEALTH SECTOR REFORM AGENDA: FOURmula One for Health
FOURmula One for Health is the DOHs Road Map for Health Sector Reforms in the Philippines from 2005 to
2010. It is designed to implement critical health interventions as a single package, backed by effective management
infrastructure and financing arrangements.
FOURmula One engages every stakeholder in the health sectorthe public and private sectors, national agencies
and local government units, external development agencies, and civil society. The over-all goals are to provide (1)
better health outcomes, (2) a more responsive health system, and (3) more equitable healthcare financing.
Implementation requires achieving critical reforms with speed, precision and effective coordination directed at
improving the quality, efficiency, effectiveness and equity of the Philippine health system in a manner that is felt by
Filipinos, especially the poor.
On a more specific note, in five years, the program aims to:
(1) secure more, better and sustained financing for health;
(2) assure the quality and affordability of health goods and services;
(3) ensure access to and availability of essential and basic health packages; and
(4) improve performance of the health system.
Millennium Development Goals (MDGs)
The Millennium Development Goals (MDGs) are the world's time-bound and quantified targets for addressing
extreme poverty in its many dimensions-income poverty, hunger, disease, lack of adequate shelter, and exclusionwhile promoting gender equality, education, and environmental sustainability. They are also basic human rights-the
rights of each person on the planet to health, education, shelter, and security.
Goal 1: Eradicate Extreme Hunger and Poverty
Goal 2: Achieve Universal Primary Education
Goal 3: Promote Gender Equality and Empower Women
Goal 4: Reduce Child Mortality
Goal 5: Improve Maternal Health
Goal 6: Combat HIV/AIDS, Malaria and other diseases
Goal 7: Ensure Environmental Sustainability
Goal 8: Develop a Global Partnership for Development
Universal Health Care (UHC)
Universal Health Care (UHC) is the call and commitment of the Philippine Government to ensure that every Filipino
has access to quality and affordable health care. In 2011, the Department of Health announced its goal to achieve
UHC by 2016 under the flagship program of President Benigno Aquino III known as Kalusugan Pangkalahatan
(KP) focusing on improving access to health care services and reducing poverty from catastrophic healthcare
expenditures especially for the poor and most vulnerable population.
The Philippine agenda to achieve Universal Health Care (UHC), also referred to as Kalusugan
Pangkalahatan (KP), is defined as the "provision to every Filipino of the highest possible quality of health care that is
accessible, efficient, equitability distributed, adequately funded, fairly financed, and a appropriately used by an
informed and empowered public". The Aquino administration puts it on top of the socioeconomic agenda to improve
the heatlh and quality of life of all Filipinos.
UHC's Three Thrusts
To attain UHC, the DOH defined three strategic thrusts to be pursued from 2011-2016, namely: 1) Achieve the
health-related Millennium Development Goals (MDGs) of improving maternal and child health and combating
priority infectious and non-communicable diseases; 2) Provide financial risk protection through expansion in the
enrollment and benefit delivery of the National Health Insurance Program (NHIP); and 3) Improve access to
quality health care which includes the upgrading of public hospital and health facilities, ensuring adequate health
human resources and securing the availabilty of essential medicines.
UHC and the Philippine Medicines Policy
In line with the goal of providing equitable access to medicines for all Filipinos and attain UHC by 2016 the
Philippine Medicines Strategy was adopted in 2011 anchored on the following key principles:
Access to medicines forms part of the fulfillment of the human right to health where government plays a
primary responsibility;
Medicines are important in a well-functioning health care system as they contribute to the achievement of
the broader health objectives of reducing morbidity, mortality and burden disease;
The state plays the primary role in the progressive realization of equitable access to medicines for all its
citizens, especially the poor. Filipinos shall not be denied access to treatment nor become impoverished because
of the high cost of medicines.
The government, in partnership with all sectors, shall endeavor to provide access of individuals and the
community to medicines and promote their rational use at all levels of care at all times.
You might also like
- What Is Fourmula One For Health Background of How F1 Was Adapted (Administrative Order 2018-0014)Document4 pagesWhat Is Fourmula One For Health Background of How F1 Was Adapted (Administrative Order 2018-0014)Nics PedrezuelaNo ratings yet
- Edoc - Pub Community Health Nursing Notes SummaryDocument9 pagesEdoc - Pub Community Health Nursing Notes SummarySHAH BAZNo ratings yet
- Community Health SurveyDocument14 pagesCommunity Health Surveyapi-273787321No ratings yet
- Historical Backgroud of DOHDocument4 pagesHistorical Backgroud of DOHAna LuisaNo ratings yet
- Module 14Document5 pagesModule 14camille nina jane navarroNo ratings yet
- Aquino Health AgendaDocument41 pagesAquino Health AgendaJannine Mae Zaragosa MosquisaNo ratings yet
- Project NARSDocument3 pagesProject NARSRovefrances ErpeluaNo ratings yet
- The Philippine Health Care Delivery SystemDocument7 pagesThe Philippine Health Care Delivery SystemPatricia SalomonNo ratings yet
- Significant Dates in the Development of Public Health Nursing in the PhilippinesDocument5 pagesSignificant Dates in the Development of Public Health Nursing in the PhilippinesJenylbajado28No ratings yet
- CHN Final PaperDocument151 pagesCHN Final PaperJose Bryan NacillaNo ratings yet
- Health Care Delivery System & COPARDocument52 pagesHealth Care Delivery System & COPARDharylle Cariño100% (1)
- Study-Guide - 4 Chn2 2nd PartDocument6 pagesStudy-Guide - 4 Chn2 2nd PartFrancis Lawrence AlexanderNo ratings yet
- FHSISDocument31 pagesFHSISNezer SorianoNo ratings yet
- Bioethics Application Various Health Situations: AND ITSDocument77 pagesBioethics Application Various Health Situations: AND ITSkathulux lluparNo ratings yet
- Ruhra CarDocument15 pagesRuhra CarNero PaderesNo ratings yet
- The Implementation of Universal Health Law in TH PhilippinesDocument1 pageThe Implementation of Universal Health Law in TH PhilippinesMelchizeder Solis LumanogNo ratings yet
- Abc BSN 4y1-1 Week 9 Course TaskDocument1 pageAbc BSN 4y1-1 Week 9 Course TaskHannah BalunanNo ratings yet
- Standards For Health Information in The Philippines 1999Document133 pagesStandards For Health Information in The Philippines 1999Alvin MarceloNo ratings yet
- History of Community Health NursingDocument3 pagesHistory of Community Health NursinghannahNo ratings yet
- Evolution of PHN in The PhilippinesDocument34 pagesEvolution of PHN in The PhilippinesRika MaeNo ratings yet
- Week 13 - NCM 108 - Activity - Report - Personalized SexualityDocument7 pagesWeek 13 - NCM 108 - Activity - Report - Personalized SexualityMaria Rhesilyn Kristhel MoranoNo ratings yet
- Learning Guide PHC 2Document20 pagesLearning Guide PHC 2Niña Amato100% (1)
- COPAR community organizing researchDocument8 pagesCOPAR community organizing researchRoeder Max Pangramuyen0% (1)
- Republic ActDocument36 pagesRepublic ActjanNo ratings yet
- Community Diagnosis NCM 113 2Document63 pagesCommunity Diagnosis NCM 113 2Jewenson SalvadorNo ratings yet
- History of Public Health Nursing PDFDocument7 pagesHistory of Public Health Nursing PDFelle belloNo ratings yet
- Essential Primary Health Care ExplainedDocument11 pagesEssential Primary Health Care ExplainedHet rodNo ratings yet
- Elements of FourMULA ONEDocument12 pagesElements of FourMULA ONEkassy yeonNo ratings yet
- Doh Program (HWPSC)Document6 pagesDoh Program (HWPSC)Ednar DayanghirangNo ratings yet
- Examining root causes of poor health and diseaseDocument1 pageExamining root causes of poor health and diseaseDONITA DALUMPINESNo ratings yet
- Community Phc2 RleDocument12 pagesCommunity Phc2 Rleefermin_lovely100% (1)
- The Nursing Process in The Care of The CommunityDocument96 pagesThe Nursing Process in The Care of The CommunityCzarina Aeri RollorataNo ratings yet
- COPAR AssignmentDocument2 pagesCOPAR AssignmentAiron Vince Peralta CalicaNo ratings yet
- The Omaha System-FinalDocument21 pagesThe Omaha System-FinalerajanejNo ratings yet
- PHC: Essential for Universal Health CareDocument24 pagesPHC: Essential for Universal Health CareNathaniel PulidoNo ratings yet
- COPAR EditedDocument4 pagesCOPAR EditedNiko MendozaNo ratings yet
- DEVOLUTION OF HEALTH SERVICES TO LGUsDocument2 pagesDEVOLUTION OF HEALTH SERVICES TO LGUsMarco BaltazarNo ratings yet
- Letter of Instruction 949Document6 pagesLetter of Instruction 949Wynna SegundoNo ratings yet
- Fatima 121 ThesisDocument144 pagesFatima 121 ThesisNecesario BanaagNo ratings yet
- COMMUNITY DIAGNOSIS: THE KEY TO COMMUNITY HEALTHDocument28 pagesCOMMUNITY DIAGNOSIS: THE KEY TO COMMUNITY HEALTHMARICEL BAUTISTA MARAYAG0% (1)
- FHSISDocument14 pagesFHSISSam Raven AndresNo ratings yet
- Community Diagnosis Sample PDFDocument2 pagesCommunity Diagnosis Sample PDFLisaNo ratings yet
- Cfe 103Document10 pagesCfe 103Omar DulayNo ratings yet
- Roles of NursesDocument3 pagesRoles of NursesRI NANo ratings yet
- NURSING CARE PLAN FOR RHEUMATIC HEART DISEASEDocument11 pagesNURSING CARE PLAN FOR RHEUMATIC HEART DISEASECharm TanyaNo ratings yet
- Lesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthDocument2 pagesLesson 1 - Global & National Health Situations, Definition & Focus, Public Health, and Community HealthA CNo ratings yet
- List of Professional Organization and Associations of Nurses in The PhilippinesDocument1 pageList of Professional Organization and Associations of Nurses in The PhilippinesTrixie Adaley Xen Heirencia50% (2)
- PHCDocument30 pagesPHCrichardmd2No ratings yet
- Entrepre NurseDocument14 pagesEntrepre NurseWendy EscalanteNo ratings yet
- Community Health NursingDocument10 pagesCommunity Health NursingBunzay GelineNo ratings yet
- 04 Community Diagnosis Talandang 1 NEW DataDocument43 pages04 Community Diagnosis Talandang 1 NEW DataLeslie Noreen AguilarNo ratings yet
- Philippine Health Agenda - Dec1 - 1 PDFDocument26 pagesPhilippine Health Agenda - Dec1 - 1 PDFreyalene gallegosNo ratings yet
- Unang Yakap: Why Moms Should Include It in Their Birth PlansDocument3 pagesUnang Yakap: Why Moms Should Include It in Their Birth PlansTyron ChuaNo ratings yet
- Health Sector Reform AgendaDocument2 pagesHealth Sector Reform AgendaLhynne Riano Salando100% (1)
- The Philippine Health Care Delivery SystemDocument4 pagesThe Philippine Health Care Delivery SystemKris Elaine GayadNo ratings yet
- Objectives:: Universal Health Care and Philippine Health AgendaDocument10 pagesObjectives:: Universal Health Care and Philippine Health AgendajosephNo ratings yet
- The Anatomy of The Philippine Health Care SystemDocument2 pagesThe Anatomy of The Philippine Health Care SystemIra Jane MintarNo ratings yet
- UHC in the Philippines: Addressing InequityDocument3 pagesUHC in the Philippines: Addressing InequityJofel Laygan Porras RNNo ratings yet
- A Report On The Principles of Health EducationDocument11 pagesA Report On The Principles of Health EducationRoucher PascuaNo ratings yet
- ROCREO - Review of Health Related LawsDocument4 pagesROCREO - Review of Health Related LawsMelisa May Ocampo AmpiloquioNo ratings yet
- Family Health Assessment FormDocument3 pagesFamily Health Assessment FormMadsNo ratings yet
- Hydronephrosis, Renal Artery Stenosis, Urinary IncontinenceDocument6 pagesHydronephrosis, Renal Artery Stenosis, Urinary IncontinenceMadsNo ratings yet
- QuestionnairesDocument2 pagesQuestionnairesMadsNo ratings yet
- English Chapter 1 (Vocabulary)Document4 pagesEnglish Chapter 1 (Vocabulary)MadsNo ratings yet
- The Death Penalty Serves Three FunctionsDocument1 pageThe Death Penalty Serves Three FunctionsMadsNo ratings yet
- Test Papers (Renal System)Document4 pagesTest Papers (Renal System)MadsNo ratings yet
- Drug StudyDocument5 pagesDrug StudyMadsNo ratings yet
- Reading SynthesisDocument2 pagesReading SynthesisMadsNo ratings yet
- Reading SynthesisDocument2 pagesReading SynthesisMadsNo ratings yet
- List of Diseases (Microbiology)Document5 pagesList of Diseases (Microbiology)MadsNo ratings yet
- Psychology (Intro)Document12 pagesPsychology (Intro)MadsNo ratings yet
- Pathophysiology: Vagal StimulationDocument1 pagePathophysiology: Vagal StimulationMadsNo ratings yet
- The Process of Evolution by Carla MaeDocument25 pagesThe Process of Evolution by Carla MaeMads100% (1)
- Spiritual CareDocument1 pageSpiritual CareMadsNo ratings yet
- Drugs Acting On The Respiratory SystemDocument54 pagesDrugs Acting On The Respiratory SystemMads0% (1)
- Women During The Pre-Colonial PeriodDocument29 pagesWomen During The Pre-Colonial PeriodMadsNo ratings yet
- Ideal Mechanical Advantage (Physics Notes)Document4 pagesIdeal Mechanical Advantage (Physics Notes)MadsNo ratings yet
- Basic Soccer SkillsDocument19 pagesBasic Soccer SkillsMadsNo ratings yet
- Drugs Acting On The Respiratory SystemDocument54 pagesDrugs Acting On The Respiratory SystemMads0% (1)
- Vitamins (Lecture For Biochemistry)Document12 pagesVitamins (Lecture For Biochemistry)MadsNo ratings yet
- Reaction Paper StardustDocument3 pagesReaction Paper StardustMads100% (2)
- Epiglottitis ReportDocument4 pagesEpiglottitis ReportMadsNo ratings yet
- Harvest Moon PSP GuideDocument106 pagesHarvest Moon PSP GuideMadsNo ratings yet
- Human Experimentation: A History of Medical Research and EthicsDocument44 pagesHuman Experimentation: A History of Medical Research and EthicsMadsNo ratings yet
- Samples of Medication FormatsDocument2 pagesSamples of Medication FormatsMadsNo ratings yet
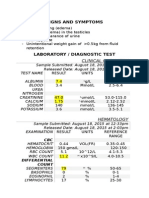
- Nephrotic Syndrome Lab Results PresentationDocument3 pagesNephrotic Syndrome Lab Results PresentationMadsNo ratings yet
- Nursing Care Plan For PcapDocument6 pagesNursing Care Plan For PcapMadsNo ratings yet
- Anatomy and Physiology of PCAPDocument8 pagesAnatomy and Physiology of PCAPMads0% (1)
- Land Securities Group (A)Document13 pagesLand Securities Group (A)Piyush SamalNo ratings yet
- Analysis of Cocoyam Utilisation by Rural Households in Owerri West Local Government Area of Imo StateDocument11 pagesAnalysis of Cocoyam Utilisation by Rural Households in Owerri West Local Government Area of Imo StatePORI ENTERPRISESNo ratings yet
- AdmitCard 1688037Document1 pageAdmitCard 1688037P.Supreeth ReddyNo ratings yet
- JKFBDDocument2 pagesJKFBDGustinarsari Dewi WNo ratings yet
- Eng9 - Q3 - M4 - W4 - Interpret The Message Conveyed in A Poster - V5Document19 pagesEng9 - Q3 - M4 - W4 - Interpret The Message Conveyed in A Poster - V5FITZ100% (1)
- Calvo, G (1988) - Servicing The Public Debt - The Role of ExpectationsDocument16 pagesCalvo, G (1988) - Servicing The Public Debt - The Role of ExpectationsDaniela SanabriaNo ratings yet
- Hays Grading System: Group Activity 3 Groups KH PS Acct TS JG PGDocument1 pageHays Grading System: Group Activity 3 Groups KH PS Acct TS JG PGkuku129No ratings yet
- Management of Dyspnoea - DR Yeat Choi LingDocument40 pagesManagement of Dyspnoea - DR Yeat Choi Lingmalaysianhospicecouncil6240No ratings yet
- Building Materials Alia Bint Khalid 19091AA001: Q) What Are The Constituents of Paint? What AreDocument22 pagesBuilding Materials Alia Bint Khalid 19091AA001: Q) What Are The Constituents of Paint? What Arealiyah khalidNo ratings yet
- Emilia Perroni-Play - Psychoanalytic Perspectives, Survival and Human Development-Routledge (2013) PDFDocument262 pagesEmilia Perroni-Play - Psychoanalytic Perspectives, Survival and Human Development-Routledge (2013) PDFMihaela Ioana MoldovanNo ratings yet
- Class 7 Summer Vacation PDFDocument4 pagesClass 7 Summer Vacation PDFPrince RajNo ratings yet
- EDUC 5240 - Creating Positive Classroom EnvironmentsDocument5 pagesEDUC 5240 - Creating Positive Classroom EnvironmentsMay Phyo ThuNo ratings yet
- Marcos & Sumulong Highway, Rizal Applicant'S Information Sheet (Non-Academic)Document2 pagesMarcos & Sumulong Highway, Rizal Applicant'S Information Sheet (Non-Academic)dummy testerNo ratings yet
- Quatuor Pour SaxophonesDocument16 pagesQuatuor Pour Saxophoneslaura lopezNo ratings yet
- Chippernac: Vacuum Snout Attachment (Part Number 1901113)Document2 pagesChippernac: Vacuum Snout Attachment (Part Number 1901113)GeorgeNo ratings yet
- CLNC 2040 Reflection of Assistant ExperiencesDocument4 pagesCLNC 2040 Reflection of Assistant Experiencesapi-442131145No ratings yet
- Basics of OncologyDocument64 pagesBasics of OncologyCiubotaru Diana -MariaNo ratings yet
- Good Paper On Time SerisDocument15 pagesGood Paper On Time SerisNamdev UpadhyayNo ratings yet
- Bach Invention No9 in F Minor - pdf845725625Document2 pagesBach Invention No9 in F Minor - pdf845725625ArocatrumpetNo ratings yet
- Segmenting, Targeting, and Positioning (STP)Document16 pagesSegmenting, Targeting, and Positioning (STP)Rachmat PutraNo ratings yet
- Understanding Malaysian Property TaxationDocument68 pagesUnderstanding Malaysian Property TaxationLee Chee KheongNo ratings yet
- Lecture Notes - Design of RC Structure - Day 5Document6 pagesLecture Notes - Design of RC Structure - Day 5Tapabrata2013No ratings yet
- Summary Essay Items..EditedDocument8 pagesSummary Essay Items..EditedJoboy FritzNo ratings yet
- Practice Questionnaire For New Omani QAQC Staff - DLQ DeptDocument7 pagesPractice Questionnaire For New Omani QAQC Staff - DLQ DeptSuliman Al RuheiliNo ratings yet
- Fitting A Logistic Curve To DataDocument12 pagesFitting A Logistic Curve To DataXiaoyan ZouNo ratings yet
- Natural Science subject curriculumDocument15 pagesNatural Science subject curriculum4porte3No ratings yet
- CRUSADE of PRAYERS 1-170 Litany 1-6 For The Key To Paradise For DistributionDocument264 pagesCRUSADE of PRAYERS 1-170 Litany 1-6 For The Key To Paradise For DistributionJESUS IS RETURNING DURING OUR GENERATION100% (10)
- KINGS OF TURKS - TURKISH ROYALTY Descent-LinesDocument8 pagesKINGS OF TURKS - TURKISH ROYALTY Descent-Linesaykutovski100% (1)
- 19-Year-Old Female With Hypokalemia EvaluatedDocument5 pages19-Year-Old Female With Hypokalemia EvaluatedMohammed AhmedNo ratings yet
- RITL 2007 (Full Text)Document366 pagesRITL 2007 (Full Text)Institutul de Istorie și Teorie LiterarăNo ratings yet