Professional Documents
Culture Documents
AfrJPaediatrSurg719-4907266 133752
Uploaded by
pawitrajayaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AfrJPaediatrSurg719-4907266 133752
Uploaded by
pawitrajayaCopyright:
Available Formats
[Downloaded free from http://www.afrjpaedsurg.org on Monday, August 17, 2015, IP: 202.80.215.
134]
Original Article
Operative management of typhoid ileal perforation in
children
Ali Nuhu, Samuel Dahwa1, Abdulkarim Hamza1
INTRODUCTION
ABSTRACT
Background: Intestinal perforation resulting from
complicated typhoid fever still causes high morbidity
and mortality. The purpose of the present study is to
evaluate the outcome of its surgical management in
Nigerian children. Materials and Methods: Emergency
laparotomy and repair of the ileum was performed on
46 children with typhoid ileal perforation at the Federal
Medical Centre (FMC), Azare, Nigeria, between January
2004December 2008. This was followed by copious
peritoneal lavage with warm normal saline and mass
closure of the abdomen. Results: There were 28
(60.86%) boys and 18 (39.13%) girls, with a mean age
of 9.5 3.22 (range, 15 months15 years). Abdominal
pain (45), fever (44), and abdominal distention (36) were
the most common presenting symptoms and majority
of the patients (36) perforated within 14 days of illness.
Solitary ileal perforations were the most common
pathology, found in 31 (67.4%) cases. Simple closure
of the perforations after debridement of the edges was
the most frequent operative procedure performed. A
total of 21 patients had one or more complications which
included wound infection (21), postoperative fever (16),
and wound dehiscence (6). Postoperative anaemia
was a problem in 23 (50%) patients. The mortality rate
was (13) 28.3%. The mean duration of hospital stay for
survivors was 22.9 12.3 (range, 646 days). This was
not significantly affected by the location or number of
perforations on the ileum. Conclusions: The clinical
course of typhoid ileal perforation may be different for
the very young. The typically high rate of complications
can be reduced if operation is undertaken earlier.
Solitary ileal perforations can be managed safely with
simple closure.
Key words: Children, management outcome, typhoid
ileal perforation
PMID: *******
DOI: 10.4103/0189-6725.59351
Department of Surgery, University of Maiduguri Teaching Hospital,
PMB 1414 Maiduguri, Borno State, 1Department of Surgery, Federal
Medical Centre, Azare, Bauchi State, Nigeria
Address for correspondence:
Dr. Ali Nuhu,
Department of Surgery, University of Maiduguri Teaching Hospital,
PMB 1414, Maiduguri, Nigeria.
E-mail: nuhualinvwa@yahoo.com
African Journal of Paediatric Surgery
Intestinal perforation resulting from complicated
typhoid fever is a continuing challenge for the
surgeons practicing in an endemic area, because of
the high morbidity and mortality rates associated
with its operative management.[1] Salmonella typhi
and paratyphi infection (causing typhoid fever), is a
serious systemic disease in developing countries and in
countries where unhealthy environmental conditions
prevail. Intestinal perforation, the most common in
the ileum, is the most serious complication of typhoid
fever, with mortality rates ranging between 2060% in
the West African subregions.[1-3] In the endemic areas,
children below the age of 15 years account for more
than 50% of the intestinal perforation cases, with higher
mortality in them than the adult population.[4-6] The
reasons for these high mortality rates and postoperative
complications are, continuing severe peritonitis,
septicaemia, malnutrition, fluid, and electrolyte
derangements. It is agreed that surgical intervention to
seal the source of continuing peritoneal contamination
is the treatment modality with the best outcome, but the
operative technique of choice is not settled. We have
managed 46 children with typhoid ileal perforation
mainly by excision and simple closure followed by
copious peritoneal lavage after adequate resuscitation.
This study reviews the pattern of disease and outcome
of such management in a government referral hospital
in Northeast Nigeria.
MATERIALS AND METHODS
In a retrospective study, children with typhoid intestinal
perforation were identified from the hospital records
of all patients with intraoperative diagnosis of typhoid
perforation treated by the General Surgery Unit of
the Federal Medical Centre, Azare, from January
2004-December 2008. Relevant data regarding clinical
diagnosis, investigations, treatment, and outcome were
obtained from the operating theatre register and other
medical records. Descriptive data were analysed using
the SPSS version 15 for windows (SPSS, Chicago,- IL,
US) and presented in statistical Tables.
January-April 2010 / Vol 7 / Issue 1
[Downloaded free from http://www.afrjpaedsurg.org on Monday, August 17, 2015, IP: 202.80.215.134]
Nuhu, et al.: Operative management of typhoid ileal perforation in children
RESULTS
There were 46 children [28 (60.8%) boys and 18 (39.1%)
girls], with intraoperative diagnosis of typhoid ileal
perforation during the study period. Their mean age was
9.5 3.22 (range, 15 months- 15 years); and male: female
ratio was 1.5:1. Also, 36 (76.1%) patients were between
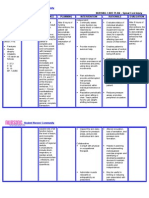
the age range of 915 years [Table 1]. There were 4
(8.7%) children below the age of five years. Almost all
the patients presented with abdominal pain, fever, and
features of peritonitis. The mean time lapse between
onset of symptoms of perforation and presentation to
hospital was 72.44 9.33 hours, (range, 24168). A
total of 44 (95.6%) patients had fever, 36 (78.3%) had
abdominal distention, 25 (54.3%) had vomiting, and
23 (50%) had constipation [Table 2]. Of the 41 patients
recorded, 21 (51.2%) perforated within the first seven
days of illness, 15 (36.6%) within the second week,
and 5 (12.2%) within the third week of illness. Plain
chest and abdominal radiographs were available for 31
(67.4%) patients with 16 (51.6%) showing free gas under
the diaphragm. The main electrolyte derangements were
hypokalaemia and raised serum urea in 13 (28.3%)
patients respectively. The packed cell volume (PCV)
was lower than 30% in 37 (80.4%) children. The widal
test was done in only 5 (10.8%) patients with the titre
higher than 1:160 in all of them. Blood cultures were
not done in any of the patients. A total of 24 (52.2%)
patients had surgery within 24 hours of presentation
to hospital and the rest 16 (34.7%) were operated after
24 hours of admission. The mean time from admission
to laparotomy was 9.4 hours (range, 624). The main
resuscitative measures in all the patients involved
correction of fluid and electrolyte derangements and
giving of pareneteral antibiotics. Those with PCVs below
30% had preoperative blood transfusion. The abdomen
was entered through a transverse subumbilical incision
for those who were five years and below (N = 4), and a
midline incision (long or subumbilical), for the others.
There were 76 ileal perforations in all, (mean = 1.65),
31 (67.4%) of which were single point [Figure 1]. Also,
5 (10.8%) patients had two perforations, another 5
(10.8%) had three, and 3 (6.5%) had four perforations
[Table 3]. There were no caecal perforations. The
highest number of ileal perforations in a single patient
was 14. The mean estimated size of the perforations
was 23.35 13.46 mm (range, 1080). Significant
faecal peritonitis was seen in all the patients with
moderate to massive soilage documented in 32 (69.6%)
of them. Eight (17.4%) patients had mild peritoneal
soilage. The main operative procedure was simple
two-layered transverse closure after a circumferential
excision of the perforation edges in 38 (82.6%) patients
and wedge resection in 1 (2.2%) patient. Six (13%)
patients had segmental ileal resection and primary
anastomosis; while one 8-year-old patient with multiple
ileal perforations, the most distal within 5 cm of the
ileocaecal junction (ICJ), had right hemicolectomy and
Table 1: Age and sex distribution of 46 children with
typhoid ileal perforation
Age (years)
14
58
912
1315
Total
Males
Females
Frequency (%)
4
4
11
10
29 (63.04)
0
3
6
8
17 (37.00)
4 (8.7)
7 (15.2)
17 (37)
18 (39.1)
46 (100)
Six hundred and seventy children were treated for typhoid fever, giving a perforation
rate of 6.8%.
Table 2: Clinical features
Presenting features
Abdominal pain
Fever
Abdominal tenderness
Abdominal distention
Vomiting
Constipation
Diarrhoea
10
January-April 2010 / Vol 7 / Issue 1
Features (%)
45 (97.8)
44 (95.7)
42 (91.3)
36 (78.3)
25 (54.3)
23 (50)
12 (26.1)
Figure 1: Typical single perforation of the terminal ileum due to typhoid fever
in a 10-year-old girl. Note the antemesenteric location and faecal peritonitis
Table 3: Distribution of number of perforations as it
relates to mortality
No. of perforations
1
2
3
4
5
14
Total
Frequency (%)
31 (67.4)
5 (10.8)
5 (10.8)
3 (6.5)
1 (2.2)
1 (2.2)
87 (100)
Mortality No. (%)
8 (25.8)
2 (40)
1 (20)
1 (33.3)
0 (0)
1 (100)
13 (28.3)
NB: There were a total of 87 ileal perforations. The highest number of perforations in
a single child was 14. The overall mortality rate was 28.3%.
African Journal of Paediatric Surgery
[Downloaded free from http://www.afrjpaedsurg.org on Monday, August 17, 2015, IP: 202.80.215.134]
Nuhu, et al.: Operative management of typhoid ileal perforation in children
ileotransverse anastomosis. Multiple adhesions were
noticed and lysed in 17 (36.9%) patients. The mean
estimated distance of the most distal ileal perforation
from the ICJ was 20.23 10.34 cm (range, 560).
Out of 37 documented patients, 19 (51.3%) had their
most dital perforations within 1020 cm of the ICJ.
The most common postoperative complications were:
wound infection 21 (%), postoperative fever 16 (%),
and anaemia 38 (%) [Table 4]. Eight (21.1%) of the 38
patients had simple closure, and 1 (16.7%) of the six had
segmental ileal resection reperforated within 4 to 9 days
(mean, 5.342.89) postoperatively, and reexploration
was done for four patients of which one survived. The
remaining five were managed conservatively of which
two survived. The overall mortality was 13 (28.3%).
Death occured 36 hours to 14 days (mean, 6.25.4
days) postoperatively from septic complications and
multiple organ failure. The mean duration of hospital
stay for survivors was 22.8912.34 days (range, 646).
The mean duration of follow-up was 4.839.36 weeks
(range, 255).
DISCUSSION
Typhoid ileal perforation is frequently seen among
children in our environment. Over this study period,
children aged 15 years and younger constituted 55.4%
of all cases. This is in keeping with earlier reports
from Nigeria where the paediatric age group accounted
for more than half the cases of typhoid intestinal
perforation. [5,6] In one of the report from Western
Nigeria[7] and India,[11] however, typhoid perforation
was the most common in the age group of 2130
years. There was a slight male preponderance (a male
female ratio of 1.7:1); similar to previous series.[6,8] The
prognosis of typhoid ileal perforation still remains
poor, with an overall mortality in this study of 28.3%,
in keeping with most previously reported series in the
tropical environment, including West Africa.[16] We
found, as previously reported, that the perforations are
the most common in the terminal ileum and survivors
were faced with wound infection and high rates of
wound dehiscence and enterocutaneous fistulae.[9]
Table 4: Postoperative complications
Postoperative complications
Wound infection
Postoperative fever
Reperforation
Wound dehiscence
Enterocutaneous fistula
Chest infection
Postoperative adhesions
Intraabdominal abscess
African Journal of Paediatric Surgery
Frequency (%)
21 (45.6)
16 (34.7)
9 (19.7)
6 (13)
4 (8.7)
4 (8.7)
3 (6.5)
1 (2.2)
Symptoms and signs of typhoid ileal perforation in
Nigerian children are not different from those in
other geographical areas,[10,11] with diarrhoea and fever
more prominent in those below five years of age. The
under five also have atypical features of generalised
peritonitis and it may not be easy to make a diagnosis
of peritonitis in them with certainty. Therefore, a high
index of suspicion is needed for a diagnosis in this
age group as demonstrated by other workers.[12] The
youngest child affected by typhoid ileal perforation
in our series was 15 months old; similar to one year[13]
and two years[14] in earlier reports. A report from
Zaria,[5] North Central Nigeria, recorded an incidence
in a two-month-old infant. This is an unusual finding
and may be due to contaminated expressed breast milk
among other possibilities. The older children exhibit
classical features of peritonitis in over 90% of cases,
supporting the diagnosis.[12] Ileal perforations occurred
within the first week of typhoid fever in over 50% of
our patients, with reference to earlier reports from
Northern Nigeria[2] and other parts of tropical Africa.[15]
This is in contrast to the classical description of three
weeks, ten days,[16] or two weeks[17] in other reports.
This may be due to a more virulent strain of Salmonella
typhi among West Africans, coupled with increased
hypersensitivity reaction in the Peyers patches in this
subregion, where the perforation rate is higher than
other endemic areas.[1] Late presentation, with mean
estimated perforation duration of four days (range,
27), and delay in operation (over 30% operated after
24 hours of presentation to hospital), were responsible
for the high mortality and morbidity in all age groups
as reported by other series.[15,18]
The need for aggressive fluid resuscitation and
correction of electrolyte derangements and anaemia;
together with the choice of a suitable antibiotic
combination is crucial to surgical outcome. The antibiotic
protocol that has been used over the years included:
chloramphenicol, gentamycin, and metronidazole;
which are given parenterally at diagnosis and continued
for seven days before conversion to oral preparations of
chloramphenicol and metronidazole. The rationale is to
cover for not only the Salmonella organism but also for
anaerobes and gram negative coliforms. The emergence
of chloramphenicol resistant, Salmonellae, has led to
the use fluoroquinolones (for example, ciprofloxacin),
or third generation cephalosporins.[19] To be certain that
the perforation on the ileum is due to typhoid enteritis,
a positive blood, stool or urine culture is necessary.
However, the yield for blood culture in a patient with
typhoid intestinal perforation is low, ranging from
334%, [3,20] in some reports. Higher yields of the
Salmonella organism is obtained from cultures of the
January-April 2010 / Vol 7 / Issue 1
11
[Downloaded free from http://www.afrjpaedsurg.org on Monday, August 17, 2015, IP: 202.80.215.134]
Nuhu, et al.: Operative management of typhoid ileal perforation in children
perforation edges, bone marrow, or peritoneal aspirates;
but this is often not possible and even when they are
done the results do not significantly alter the operative
treatment given to the patient. The classical disposition
of the typhoid perforation in the longitudinal axis of
the ileum and on the antemesenteric border with an
antecedent history of prolonged febrile illness in a child,
who did not respond to antimalarials, is enough to make
a conclusion as to the aetiology of the perforation. A
plain abdominal or chest radiograph with free air under
the diaphragm is a fairly frequent but variable finding
signifying perforated hollow viscus, but its absence does
not exclude the diagnosis.
The presence of single ileal perforations in majority
(76.4%) of our patients is consistent with other
reports [16] [Figure 1], and moderate to massive
peritoneal contamination favoured the development
of septic complications, such as wound infection,
wound dehiscence, residual intraabdominal abscesses,
and enterocutaneous fistulae, in those patients who
survived. [18] We found multiple perforations with
massive peritoneal soilage in 15 (32.6%) patients.
Prompt surgery after adequate resuscitation, is the
treatment of choice for typhoid perforation; this has
considerably reduced mortality from 3060%[13] to
approximately 6.8% in a recent series.[21] Many surgical
techniques have been used, ranging from simple
peritoneal drainage under local anaesthesia in moribund
patients,[20,22] excision of the edge of the ileal perforation,
and simple transverse closure in two layers; as done for
majority of our patients, segmental ileal resection and
primary anastomosis especially in multiple perforations
or right hemicolectomy where the caecum is involved.
There are conflicting results of the outcome of these
widely practiced techniques. Whereas, better results are
reported with simple closure, in many series;[3,20] others
favour segmental ileal resection and anastomosis.[23,24]
Those that favour simple closure argue, that in such very
ill patients any prolonged procedure may jeopardise the
outcome and that the ileum affected by typhoid fever,
take sutures well without cutting through. This was the
experience of the authors. We carried out segmental
resection and primary anastomosis only when there
were multiple perforations that were in close range
and when the caecum was involved. But any operative
technique that is carried out in good time, and allows
for a swift clearing of peritoneal contamination by a
copious peritoneal lavage is the most likely to give the
best outcome.
Our practice in managing these children is a simple
closure of the perforation, peritoneal lavage with warm
12
January-April 2010 / Vol 7 / Issue 1
normal saline, and closure of the abdominal wall with
drainage. Ceftriazone, metronidazole, and gentamicin
are given perioperatively to cover for the Salmonella,
gram negative organisms, and coliforms, respectively.
The side-effects of the quinolone ciprofloxacin on the
growing cartilage of the child usually make it a second
choice in our practice, except when the benefit clearly
outweighs this risk.
Mortality rate remains high after surgical treatment
for typhoid intestinal perforation; 28.3% in this
study, compare favourably with similar studies from
Nigeria[5,6] and the West African subregion.[3,9] Mortality
is related to endotoxaemia, septicaemia, and multiple
organ failure. There have been reports of very high
mortality, [16] but with early presentation, timely
surgery, and improvement in critical care, this can be
reduced drastically. Exceptionally, low mortality rates of
35% have been reported[25,26] previously. The reason for
the high mortality is multifactorial. In our experience,
late presentation, delay in diagnosis, and inappropriate
or partial treatment of typhoid fever were the main ones.
In conclusion, typhoid ileal perforation in children has
a poor prognosis in our environment. Late presentation,
delayed operation, faecal peritoneal contamination, and
postoperative faecal fistulae are the factors that have
adverse effects on survival. Most deaths occurred during
the early postoperative period, with survivors having
a prolonged hospital stay. There should be a deliberate
community drive towards preventive measures; by
health education, improvement in potable water supply,
sewage disposal, and personal hygiene to stamp out this
public health menace.
ACKNOWLEDGEMENTS
We thank all the consultants and resident doctors of the
Department of Surgery, Federal Medical Centre, Azare for their
cooperation during the period of this study. We appreciate
the contribution of the Nurses on the Surgical and Paediatric
Surgical wards of the Hospital and the Medical records staff
for extracting the folders.
REFERENCES
1.
2.
3.
4.
5.
Archampong EQ. Typhoid ileal perforation: why such mortality. Br
J Surg 1976;63:317-21.
Akoh JA. Prognostic factors in typhoid perforation. East Afr J Med
1992;70:18-21.
Mock CN, Amaral J, Visser LE. Improvement in survival from
typhoid ileal perforation: result of 221 operative cases. Ann Surg
1992;215:244-9.
Ugwu BT, Yiltok SJ, Kidmas AT, Opaluwa AS. Typhoid intestinal
perforation in north central Nigeria. West Afr J Med 2005;24:1-6.
Ameh EA. Typhoid ileal perforation in children: a scourge in
African Journal of Paediatric Surgery
[Downloaded free from http://www.afrjpaedsurg.org on Monday, August 17, 2015, IP: 202.80.215.134]
Nuhu, et al.: Operative management of typhoid ileal perforation in children
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
developing countries. Ann Trop Paedtr 1999;19:267-72.
Uba AF, Chirdan LB, Ituen AM, Mohammed AM. Typhoid intestinal
perforation in children: a continuing scourge in a developing country.
Paed Surg Int 2007;23:33-9.
Ajao OG. Typhoid perforation: factors affecting mortality and
morbidity. Int Surg 1982;4:317-9.
Butler T, Knight J, Nath SK, Speelman P, Roy SK, Azao MA. Typhoid
fever complicated by intestinal perforation: a persisting fatal outcome
requiring surgical management. Rev Infect Dis 1985;7:244-56.
Abatanga FA, Wiafe-Addai BB. Postoperative complications after
surgery for typhoid perforation in children in Ghana. Paediatr Surg
Int 1998;14:55-8.
Atamanalp SS, Aydinli B, Ozturk G, Oren D, Basoglu M, Yildirgan
MI. Typhoid intestinal perforation: twenty-six year experience. World
J Surg 2007;31:1883-8.
Talwar S, Sharma KR, Mittal DK, Prasad P. Typhoid enteric
perforation. Aust N Z J Surg 1997;67:351-3.
Ekenze SO, Ikefuna AN. Typhoid intestinal perforation under 5 years
of age. Ann Trop Paediatr 2008;28:53-8.
Ekenze SO, Okoro PE, Amah CC, Ezike HA, Ikefuna AN. Typhoid
ileal perforation: Analysis of morbidity and mortality in 89 children.
Niger J Clin Pract 2008;11:58-62.
Lizaralde E. Typhoid perforation of the ileum in children. J Paediatr
Surg 1981;16:1012-6.
Archampong EQ, Tandoh JFK, Nwako FA, da Rocha-Afodu JT, Foli
AK, Darko R, et al. Small and large intestine (including rectum and
anus). In: Badoe EA, Archampong EQ, da Rocha-Afodu JT, editors.
Principles and practice of surgery including pathology in the tropics.
3rd ed. Accra: Ghana Publishing Company Tema; 2000. P. 620-32.
16. Kizilcan F, Tanyel FC, Buyukpamukcu N, Hicsonmez A.
Complications of typhoid fever requiring laparotomy during
childhood. J Paediatr Surg 1993;28:1490-3.
17. Keenan JP, Hadley GP. The surgical management of typhoid
perforation in children. Br J Surg 1984;71:928-9.
18. Adesunkanmi AR, Ajao OG. The prognostic factors in typhoid ileal
perforation: A prospective study of 50 patients. J R Coll Surg Edin
1997;42:395-9.
19. Kabra SK, Madhulika, Talati A, Soni N, Patel S, Modi RR. Multi drug
resistant typhoid fever. Trop Doct 2000;30:195-7.
20. Khana AK, Misra MK. Typhoid perforation of the gut. Postgrad Med
J 1984;60:523-5.
21. Karmacharya B, Sharma VK. Results of typhoid perforation
management: experience in Bir Hospital, Nepal. Kathmandu Univ
Med J (KUMJ) 2006;4:22-4.
22. Kim JP, Oh SK, Jarret F. Management of ileal perforation due to
typhoid fever. Am J Surg 1976;181:88-91.
23. Shah AA, Wani KA, Wazir BS. The ideal treatment of typhoid enteric
perforation- resection anastomosis. Int Surg 1999;84:35-8.
24. Ameh AE, Dogo PM, Attah MM, Nmadu PT. Comparison of three
operation s for typhoid perforation. Br J Surg 1997;4:558-9.
25. Vargas M, Penne A. Perforated viscera in typhoid fever: a better
prognosis for children. J Paediatr Surg 1975;10:531.
26. Santillana M. Surgical complications of typhoid fever: enteric
perforation. World J Surg 1991;15:170.
Source of Support: Nil, Conflict of Interest: None.
Author Help: Online submission of the manuscripts
Articles can be submitted online from http://www.journalonweb.com. For online submission, the articles should be prepared in two files (first
page file and article file). Images should be submitted separately.
1)
2)
3)
4)
First Page File:
Prepare the title page, covering letter, acknowledgement etc. using a word processor program. All information related to your identity
should be included here. Use text/rtf/doc/pdf files. Do not zip the files.
Article File:
The main text of the article, beginning with the Abstract to References (including tables) should be in this file. Do not include any information
(such as acknowledgement, your names in page headers etc.) in this file. Use text/rtf/doc/pdf files. Do not zip the files. Limit the file size
to 1 MB. Do not incorporate images in the file. If file size is large, graphs can be submitted separately as images, without their being
incorporated in the article file. This will reduce the size of the file.
Images:
Submit good quality color images. Each image should be less than 2048 kb (2 MB) in size. The size of the image can be reduced by
decreasing the actual height and width of the images (keep up to about 6 inches and up to about 1200 pixels) or by reducing the quality of
image. JPEG is the most suitable file format. The image quality should be good enough to judge the scientific value of the image. For the
purpose of printing, always retain a good quality, high resolution image. This high resolution image should be sent to the editorial office at
the time of sending a revised article.
Legends:
Legends for the figures/images should be included at the end of the article file.
African Journal of Paediatric Surgery
January-April 2010 / Vol 7 / Issue 1
13
You might also like
- Doll-Cupid P MsDocument5 pagesDoll-Cupid P MsMuhammad Bahrian ShalatNo ratings yet
- 29Document3 pages29pawitrajayaNo ratings yet
- Definition Fracture BedahhhhhhDocument6 pagesDefinition Fracture BedahhhhhhpawitrajayaNo ratings yet
- 1 PembukaanDocument3 pages1 PembukaanIsmail YusufNo ratings yet
- 28Document2 pages28pawitrajayaNo ratings yet
- 1475 2875 8 134Document6 pages1475 2875 8 134pawitrajayaNo ratings yet
- Kissing Dolls: Pattern: Notation Key ToolsDocument0 pagesKissing Dolls: Pattern: Notation Key ToolsmyyyyyrNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakatamictrNo ratings yet
- Faktor-Faktor Risiko Yang Berpengaruh Terhadap Persalinan Dengan TindakanDocument135 pagesFaktor-Faktor Risiko Yang Berpengaruh Terhadap Persalinan Dengan TindakanRakhmat Ari Wibowo50% (2)
- Kissing Dolls: Pattern: Notation Key ToolsDocument0 pagesKissing Dolls: Pattern: Notation Key ToolsmyyyyyrNo ratings yet
- 1Document9 pages1Flavia LopesNo ratings yet
- 28Document2 pages28pawitrajayaNo ratings yet
- Typhoid Fever Current Concepts.5Document7 pagesTyphoid Fever Current Concepts.5pawitrajayaNo ratings yet
- Cinnamon bark oleoresin improves skin and bone collagen in aged ratsDocument7 pagesCinnamon bark oleoresin improves skin and bone collagen in aged ratspawitrajayaNo ratings yet
- Hahaha Aah AhahaaaDocument1 pageHahaha Aah AhahaaapawitrajayaNo ratings yet
- Hahaha Aah AhahaaaDocument1 pageHahaha Aah AhahaaapawitrajayaNo ratings yet
- 25Document3 pages25pawitrajayaNo ratings yet
- 27 What Is Medical Professionalism?Document4 pages27 What Is Medical Professionalism?pawitrajayaNo ratings yet
- 26Document3 pages26pawitrajayaNo ratings yet
- 24Document3 pages24pawitrajayaNo ratings yet
- 27 What Is Medical Professionalism?Document4 pages27 What Is Medical Professionalism?pawitrajayaNo ratings yet
- 26Document3 pages26pawitrajayaNo ratings yet
- 24Document3 pages24pawitrajayaNo ratings yet
- Di Susunoleh: Ratri Diana Sari 13700053 Putupartaanantama 13700055 Ida Ayugalih Pertiwi 13700057 Ida Bagus Putra Narendra 13700059Document4 pagesDi Susunoleh: Ratri Diana Sari 13700053 Putupartaanantama 13700055 Ida Ayugalih Pertiwi 13700057 Ida Bagus Putra Narendra 13700059pawitrajayaNo ratings yet
- 18Document3 pages18pawitrajayaNo ratings yet
- 17Document3 pages17pawitrajayaNo ratings yet
- 16Document3 pages16pawitrajayaNo ratings yet
- 31Document3 pages31pawitrajayaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Department of Genetics: Covid-19 RT PCRDocument1 pageDepartment of Genetics: Covid-19 RT PCRAshwin ShajiNo ratings yet
- Functions of Parotid GlandDocument32 pagesFunctions of Parotid GlandAsline JesicaNo ratings yet
- Edema LymphedemaDocument2 pagesEdema LymphedemaAsmat BurhanNo ratings yet
- OBGYN End of Rotation Exam OutlineDocument35 pagesOBGYN End of Rotation Exam OutlinehevinpatelNo ratings yet
- Clinical Profile and Outcome of Myasthenic CrisisDocument13 pagesClinical Profile and Outcome of Myasthenic CrisissyahriniNo ratings yet
- Alzheimer'S Disease Definition: Signs and SymptomsDocument4 pagesAlzheimer'S Disease Definition: Signs and SymptomsMauren DazaNo ratings yet
- 12 Tips For Bedside TeachingDocument4 pages12 Tips For Bedside Teachingbayu100% (1)
- Lesson Plan On Home Visit JKSDocument4 pagesLesson Plan On Home Visit JKSjatheeshNo ratings yet
- DOH STANDARDS (Indicators) For LEVEL 2 HOSPITALDocument55 pagesDOH STANDARDS (Indicators) For LEVEL 2 HOSPITALMOHBARMM PlanningStaffNo ratings yet
- Progyluton-26 1DDocument16 pagesProgyluton-26 1DUsma aliNo ratings yet
- 2 Conversion of Iv To PoDocument27 pages2 Conversion of Iv To PoSreya Sanil100% (1)
- Contoh Soal UKNiDocument4 pagesContoh Soal UKNiNurhaya NurdinNo ratings yet
- Hepatic Disease in PregnancyDocument37 pagesHepatic Disease in PregnancyElisha Joshi100% (1)
- Philippine Nursing Act of 2002Document22 pagesPhilippine Nursing Act of 2002Hans TrishaNo ratings yet
- Full Text 01Document44 pagesFull Text 01ByArdieNo ratings yet
- Simulation Program For Clinical Performance Improvement: Improving Clinical Care and Patient Safety Through SimulationDocument11 pagesSimulation Program For Clinical Performance Improvement: Improving Clinical Care and Patient Safety Through SimulationiloilocityNo ratings yet
- Flap Approaches in Plastic Periodontal and Implant Surgery: Critical Elements in Design and ExecutionDocument15 pagesFlap Approaches in Plastic Periodontal and Implant Surgery: Critical Elements in Design and Executionxiaoxin zhangNo ratings yet
- Cleveland Doctor Disciplined by Medical BoardDocument6 pagesCleveland Doctor Disciplined by Medical BoarddocinformerNo ratings yet
- CGMP GuidelinesDocument4 pagesCGMP GuidelinesMohan KumarNo ratings yet
- Sanction Terms Loan DetailsDocument4 pagesSanction Terms Loan Detailsinfoski khan100% (1)
- BPH - PlanDocument5 pagesBPH - PlanSomesh GuptaNo ratings yet
- Additional Vacancies at CHCs in Health and Family Welfare Services For One Year Government ServicesDocument5 pagesAdditional Vacancies at CHCs in Health and Family Welfare Services For One Year Government ServicesBhavvNo ratings yet
- Guidance To The Internaitonal Medical Guide For Ships 3rd EdDocument14 pagesGuidance To The Internaitonal Medical Guide For Ships 3rd EdSaurabh YadavNo ratings yet
- NCPDocument2 pagesNCPsphinx809100% (2)
- Carboprost Drug StudyDocument3 pagesCarboprost Drug StudyAjay SupanNo ratings yet
- MTLB Debate PRODocument3 pagesMTLB Debate PRORHODA MAE CAPUTOLNo ratings yet
- What Is Infusion Pump?Document4 pagesWhat Is Infusion Pump?BMTNo ratings yet
- Secondary Survey for Trauma PatientsDocument18 pagesSecondary Survey for Trauma PatientsJohn BrittoNo ratings yet
- Medical skills checklist for nursesDocument5 pagesMedical skills checklist for nursesHussain R Al-MidaniNo ratings yet
- Pathophysiology of Shock Sepsis and Organ Failure PDFDocument1,179 pagesPathophysiology of Shock Sepsis and Organ Failure PDFNotInterested100% (1)