Professional Documents
Culture Documents
(F) Chapter 11 - Principles of Antimicrobial Action and Resistance
Uploaded by
Gerald John PazOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(F) Chapter 11 - Principles of Antimicrobial Action and Resistance
Uploaded by
Gerald John PazCopyright:
Available Formats
(Finals) MICROBIOLOGY / Principles of Antimicrobial Action and Resistance
Medical Intervention eradicate infecting pathogen
Antibiotics substances that actively inhibit or kill the
organism
Antibiotics maybe:
1. Obtained and purified from other microorganisms
2. Chemically synthesized
Antimicrobial agents
natural and synthesized substances
play a central role in the control and management
of infectious diseases
1. Antibacterial
2. Antifungal
3. Antiparasitic
4. Antiviral
ANTIMICROBIAL ACTION
Principles
Key Steps for antimicrobial agent to inhibit/kill
microorganism:
1. Must be in active form
Ensured through pharmacodynamic design of
drug
2. Must be able to achieve sufficient levels or
concentrations at site of infection
Depends on pharmacokinetic properties of agent
3. Remaining steps relate to direct interactions
between agent and bacterial cell.
Pharmacokinetic properties
1. Distribution
2. Excretion of agents metabolites
3. Rate of absorption
4. Metabolism
** Bactericidal agents are more effective against
organisms that are more difficult to control in combination
with hosts immune system.
** Primary goal is to optimize a drugs ability to achieve
steps for antimicrobial activity.
** Antimicrobial agents are frequently
according to their mode of action.
1.
2.
3.
4.
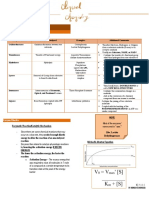
Anatomic Distribution of Some Common
Antibacterial Agents
Norfloxacin and Nitrofurantoin
Therapeutic levels generally not achievable at
Serum-Blood
Gentamicin,
Clindamycin,
Norfloxacin,
Nitrofurantoin
Therapeutic levels generally not achievable at
CSF
Vancomycin and Ciprofloxacin
Moderate
to
poor
therapeutic
levels
achievable at CSF
Urine
Therapeutic levels not achievable at Urine
Bacteriostatic agents inhibit bacterial growth but do
not kill the organism
categorized
Mode of Action of Antibacterial Agents
** Most targets of antibacterial agents are intracellular.
Basic Steps Required for Antimicrobial Activity
1. Active Drug
2. Anatomic approximation
3. Surface binding (Adsorption)
4. Intracellular uptake
5. Target Binding
6. A. Growth Inhibition
B. Lysis and Death
Bactericidal agents usually kill target organisms
Inhibitors of cell wall synthesis
o Beta-lactams
o Glycopeptides
Inhibitors of Cell Membrane Functions
o Lipopeptides
o Polymixins
Inhibitors of Protein Synthesis
o Binds to 30S
Aminoglycosides
Tetracyclines
Glycylcyclines
o Binds to 50S
Macrolide-LincosamideStreptogramin
Oxazolidinone
Chloramphenicol
Inhibitors of DNA & RNA Synthesis
o Fluoroquinolone
o Ciprofloxacin
o Metronidazole
o Rifampin
Inhibitors of Folic Acid Synthesis
o Sulfonamides
o Trimethoprim
A.
Inhibitors of Cell Wall Synthesis
1.
Beta-Lactams
Core - four-member, N containing, Beta-lactam
ring
Largest group of antibacterial agents
Lacks toxicity to humans
Beta-lactam ring
key to the mode of action of Betalactams
similar to acyl-D-alanyl-D-alanine
Beta-lactam binds enzyme, inhibiting
transpeptidation and cell wall synthesis
Penicillin-binding proteins (PBPs)
Acyl-D-Alanyl-D-Alanine normal substrate for synthesis
of linear glycopeptide in the bacterial cell wall.
-
Types:
1. Penicillin
a. Penicillin
b. Ampicillin
c. Meziocillin
d. Piperacillin
2.
Cephalosporins
(Finals) MICROBIOLOGY / Principles of Antimicrobial Action and Resistance
a. Cefazolin
b. Cefuroxime
c. Cefotetan
d. Cefotaxime
e. Ceftriaxone
f. Ceftazidime
g. Cefepime
3. Carbapenems
a. Meropenem
b. Imipenem
c. Doripenem
4. Monobactams
a. Aztreonam
Penicillin-binding Proteins (PBP)
Enzymes essential to produce and maintain their
peptidoglycan layer
B-lactam + PBP = cell wall synthesis is halted due to
osmotic instability
Spectrum of Activity type of bacteria against which a
particular antimicrobial agent does and does not have
activity.
Spectrum of Activity of B-lactams: gram + and gram
bacteria
4 major categories of B-lactamases
1. Class A & D
o Serine peptidases
2. Class C
o Cephalosphorinases
3. Class B
o Requires zinc
o Metallo-B-lactamases
B-lactamase should be located on:
1. Plasmids
2. Transposons
3. within integrons
4. within chromosome
Integron
large cassette region that contains antibiotic
resistance genes
Integrase
required for movement of integrin from one
genetic element to another\
Resistance Mechanisms
1. Genetic mutations in PBP coding sequence
2. Genetic Recombination
3. Overproduction of PBP
4. Acquiring new genetic coding sequence
** Acquired type of B-lactam resistance are commonly
found in Gram + bacteria
2.
Glycopeptides
Inhibit bacterial cell wall synthesis by binding to
end of peptidoglycan
Interferes with transpeptidation
Interferes with PBP enzymes that incorporate
precursors into growing cell wall
a.
b.
3.
Vancomycin
Levels should be monitored
Potential for toxicity
Teicoplanin
Approved
Not available in the US
Lipoglycopeptides
Semi-synthetic molecules
Glycopeptides that contain hydrophobic chemical
groups
Increase cell permeability
Cause depolarization of cell membrane potential
Inhibits transglycosylation
a. Oritavancin
b. Telavancin
Transglycosylation
-
Necessary for cell wall synthesis by complexing
with D-alanyl-D-alanine residues
Spectrum of Activity: VISA (Vancomycin Intermediate
Staphylococcus aureus.
B.
Inhibitors of Cell Membrane Function
1.
Lipopeptides
a. Daptomycin
Recently developed
Bind and disrupts cell membrane of Gram +
bacteria
Has potent activity against Gram + cocci,
MRSA,VRSA
b. Bacitracin
Inhibits recycling of certain metabolites required
for maintaining peptidoglycan synthesis
Only used as tropical antibacterial agent
Internal consumption is avoided
2.
Polymyxins
Cyclic polypeptide agents that disrupt cell
membranes
Acts as detergents (interacts with phospholipids
and increased permeability)
Disruption results to leakage of macromolecules
and ions
Not equally effective agains all bacteria and more
effective against Gram - and poor activity to
Gram +
Pose a risk for toxicity for humans have
membranes
Last resort microbial agents
Spectrum of
Acinetobacter
Major Side effects
1. Neurotoxicity
2. Nephrotoxicity
C.
Inhibitors of Protein Synthesis
1.
Aminoglycosides and Aminocyclitols
Activity:
Gram
-,
P. aeruginosa,
(Finals) MICROBIOLOGY / Principles of Antimicrobial Action and Resistance
a.
-
Aminoglycosides
Inhibit protein synthesis
Irreversible binding to protein receptors on 30S
ribosomal unit
Major toxicity:
1. Nephrotixicity
2. Auditory/Vestibular Toxicity
Interrupts the following:
o Initial formation of protein synthesis
complex
o Reading of mRNA code
o Formation of rRNA complex
Gentamycin
Commonly used aminoglycoside
1. Tobramycin
2. Amikacin
3. Streptomycin
Spectrum of Activity: Not effective against anaerobic
bacteria, Effective against aerobic gram and
Staphylococcus aureus.
2.
Macrolide-Lincosdamide-Sreptogramin
Inhibits protein synthesis by binding to 23s rRNA
on bacteria 50S ribosomal subunit
Disrupts pepide chain (blocks translocation
reaction
Bacteriostatic
Can be bactericidal if organism is low and if used
in high concentrations
Spectrum of Activity: Effective against Gram +,
mycoplasma, Treponemes, Rickettsiae & Not effective
against Gram
Quinupristin- dalfopristin
Dual streptogramin
Targets 2 sites of 50S ribosomal subunit
Toxicity is generally low
Lincosamides, Clindamycin, Lincomycin
Bind to 50S ribosomal subunit
Prevent elongation
Interfere with peptidyl transfer
Spectrum of Activity: Effective against Gram +
Spectrogramins
Naturally occurring cyclic peptides
a. Quinupristin-daltopristin
Enter cell through massive diffusion
Bind irreversibly to 50s subunit that induces
conformational change in the ribosomal structure
Alteration of ribosome
Interferes with peptide bond formation that
disrupts elongation
Toxicity:
1. Low toxicity
2. Localized phlebitis major complication of IV
infusion
Spectrum of Activity: Effective agains Gram + and
some Gram -
3.
Ketolides
Consist of:
1. Chemical derivatives of erithromycn A
2. Other macrolides
Bind to 23s rRNA of 50S ribosomal subunit
Inhibits protein synthesis
4.
Telithromycin
Maintain activity agains most macroled-resistant
gram +
Does not induce common macrolide resistance
mechanism
Effective against respiratory pathogens &
intracellular organisms
Low toxicity
Major side effects:
1. Gastrointestinal symptoms
Spectrum of Activity: Effective against gram +, some
gram -, mycoplasma, mycobacteria, chlamydia,
rickettsia, Francisella tularensis
5.
Oxazolidinones
Represented by linezolid
Linezolid
o Synthetic agent
o Inhibits protein synthesis by interactive
with 23s rRNA in 50S ribosomal subunit
o Interfere with binding of tRNA for
formylated-methionine
Low toxicity
Gastrointestinal symptoms
Spectrum of Activity: Effective against Gram +,
mycobacteria
6.
Chloramphenicol
Inhibits addition of amino acid to growing peptide
chain
Reversibly bind to 50S ribosomal subunit
Inhibits transpeptidation
Highly active
Uses has dwindled because of drug toxicity and
development of new effective and safer drugs
Bone marrow toxicity
Major side effect: Aplasia
Spectrum of Activity: Effective against Gram and
Gram +
7.
Tetracyclines
Broad spectrum bacteriostatic
Inhibit protein synthesis by binding reversibly to
30S ribosomal subunit
-
Toxicity:
o Upper gastrointestinal effects
o Cutaneous phototoxicity
o Photoallergic immune reaction
Spectrum of Activity: Effective against Gram and
Gram +, Intracellular pathogens (Rickettsia and
Chlamydia), Protozoa, N. gonorrhoeae, Mycoplasma,
Spirochetes
(Finals) MICROBIOLOGY / Principles of Antimicrobial Action and Resistance
8.
Glycylglycines
Semi-synthetic tetracycline derivatives
Tigecycline
o 12st agent of glycylglycines approved
for clinical use
o Inhibits protein synthesis by binding
reversibly to 30S ribosomal subunit
o Has advantage of being refractory to
most common tetracycline resistance
o Most common effects are:
Nausea
Vomiting
Diarrhea
D.
Inhibitors of DNA and RNA Synthesis
1.
Fluoroquinolones
Simply quinolones
Derivatives of Nalidixic acid
o Ciprofloxacin
o Ofloxacin
Bind and interfere with DNA gyrase enzymes
regulating DNA supercoiling
Also inhibit topoisomerase IV
Topoisomerase IV
o Unlinks DNA after replication
Potent bactericidal agents
Toxicity:
o Tendinitis
o Rupture of Achilles tendon
2.
3.
Spectrum of Activity: Effective against gram
(topoisomerase is targeted) and gram + (DNA gyrase
is targeted)
Metronidazole
Antibacterial activity is related to the presence of
nitro group in chemical structure
Nitro group
o Reduced by nitroreductase in bacterial
cytoplasm
o Generates:
Autotoxic compounds
Free radicals
Activation requirements
o Reduction under low redox potentials
(anaerobic)
Low toxicity
Side effects: Mild gastrointestinal symptoms
Spectrum of Activity: Effective against Anaerobic,
Microaerophilic
gram
and
Protozoans
(Trichomonas, Giardia, Entamoeba histolytica)
Rifamycin
Include Rifampin (Rifampicin)
Semisynthetic
Bind to the enzyme
o DNA dependent
o RNa polymerase
Inhibits RNA synthesis
Does not effectively penetrate oputer membrane
of gram (-)
Spontaneous mutation
Rifampin are usually used in combination with
other agents
Side effects:
o Gastrointestinal symptoms
o Hypersensitivity reactions
E.
Inhibitors of Other Metabolic Processes
1.
Sulfonamides
Disrupts folic acid pathway
Bind to dihydropteroate synthase
Moderate toxicity
Side effects:
o Vomiting
o Nausea
o Hypersensitivity reactions
Antagonistic for other medications
Spectrum of Activity: Effective against Gram and
Gram +
2.
Trimethoprim
Targets folic acid pathway
Inhibits dihydrofolate reductase
Usually
combined
with
sulfonamide
(sulfamethoxazole) to simultaneously attack 2
targets
Mild toxicity
Adverse side effects:
o Person with AIDS develop side effects
more often
3.
Nitrofurantoin
Consists of nitrogroup on heterocyclic ring
Mechanism is diverse and multifaceted
Used to treat uncomplicated UTI
Side effects:
o Gastrointestinal infections or symptoms
Diarrhea
Nausea
Vomiting
o Chronic pulmonary condition
o Irreversible pulmonary fibrosis
Spectrum of Activity: Effective against Gram and
Gram +
MECHANISMS OF ANTIBIOTIC RESISTANCE
Principles
Resistance requires: interruption or disturbance
of one or more steps
Result is:
o Partial loss of effectiveness
o Complete loss of effectiveness
Aspects
1.
2.
3.
Biologic vs. Clinical
Environmentally-mediated
Microorganism-mediated
(Finals) MICROBIOLOGY / Principles of Antimicrobial Action and Resistance
A.
Biologic vs. Clinical Resistance
Biologic resistance
Changes that result in observed
susceptibility to a particular agent
Clinical resistance
Most laboratory
resistance
methods
S. pneumoniae
Inhibited by penicillin
B.
Environmentally
Mediated
Resistance
Antimicrobial Resistance
1. Drug
2. Microorganisms
3. Environment
used
to
2 subcategories of Organism based resistance
a. Intrinsic/inherent
b. Acquired
Intrinsic Resistance
Results from the normal genetic, structural or
physiologic state of microorganism
Considered as natural inherited characteristic
Resistance pattern may be predictable
Intrinsic resistance profiles are also useful
markers to aid identification of certain bacteria
reduced
detect
Antimicrobial
Intrinsic Resistance
Anaerobic bact vs.
aminoglycosides
Enterococci vs.
aminoglycosides
Gram + vs. Aztreonam
Enterococci vs.
cephalosporin
Gram vs. Vancomycin
P. aeruginosa vs.
Sulfonamides
Klebsiella spp vs.
ampicillin
Stenotrophomonas
maltophilia vs. imipenem
Aerobic bact vs.
metronidazole
Lactobacilli and
Leuconostoc sp. vs.
vancomycin
**These three factors coexist
Environmentally mediated resistance
Resistance directly resulting from physical or
chemical changes of environment
Alters:
o Microbial agent
o Microorganisms normal physiological
response
Environmental factors
1. pH
2. anaerobic atmosphere
3. cation concentration
4. thymidine content
pH
Erythromycin & Aminoglycosides
o Low pH; Low effect of agent
Tetracycline
o High pH; Low effect of agent
Aminoglycoside mediated shutdown of bacterial protein
synthesis
-
Requires intracellular uptake
Driven by oxidative process
No oxygen, low uptake
Affected by Ca++ and Mg++
o P. aeruginosa has negative net charge
in cell membrane
o Cations compete with aminoglycoside
for negative charged binding sites
o High cations, low effect of agent
Antimicrobial resistance that results from
genetically encoded traits of the microorganisms
C.
Presence of Metabolites
Enterococci
o Uses thymine and exogenous folic acid
to circumvent activities of sulfonamides
and trimethoprim
o Absence
of
metabolites,
full
susceptibility to antibiotics
Microorganism Mediated Resistance
Lack of PBP
Lack of uptake
Production of enzymes
Inability to anaerobically
reduce to active form
Lack of appropriate cell
wall precursor target
Acquired Resistance
Results from altered cellular physiology and
structure caused by changes in microorganism
genetic makeup
Trait associated with specific strains of particular
organism
Unpredictable
May be acquired by:
o Genetic mutation
o Acquisition of genes
o Combination of mutational and gene
transfer events
COMMON PATHWAYS FOR ANTIMICROBIAL
RESISTANCE
1.
2.
Mechanism
Lack
of
ocidative
metabolism
3.
4.
5.
6.
Enzymatic degradation or modification of
antimicrobial agent
Decreased
uptake
or
accumulation
of
antimicrobial agent
Altered antimicrobial agent
Circumvention
of
the
consequences
of
antimicrobial action
Uncoupling
of
antimicrobial
agent-target
interactions and subsequent effects on bacterial
metabolism
Any combination of mechanisms 1 to 5
(Finals) MICROBIOLOGY / Principles of Antimicrobial Action and Resistance
Resistance mechanisms against:
1. B-lactams
a. Enzymatic destruction
- B-lactamase
b. Altered target
- Mutational changes in PBP
c. Decreased uptake
- Porin channels change in number
2. Glycopeptides
a. Altered target
- Alteration in molecular structure
b. Target overproduction
- Excess peptidoglycan
3. Aminoglycoside
a. Enzymatic modification
- Modifying enzymes
b. Decreased uptake
- Porin channels change in number
c. Altered target
- Mutational changes in ribosomal
binding site
4.
5.
Quinolones
a. Decreased uptake
- Alterations in the outer membrane
b. Altered target
- Changes in DNA gyrase subunits
Macrolides
a. Efflux
- Pumps drugs out of cell
b. Altered target
- Enzymatic alteration
Factors contributing to the emergence and
dissemination of antimicrobial resistance among
bacteria
1. Emergence of new genes
2. Spread of old genes to new hosts
3. Mutations of old genes resulting in more potent
resistance
4. Emergence of intrinsically resistant opportunistic
bacteria
You might also like
- Antimicrobial DrugsDocument44 pagesAntimicrobial Drugsreza tavayefNo ratings yet
- Antibiotics NotesDocument7 pagesAntibiotics NotesmuhammadridhwanNo ratings yet
- Hematology Written SummariesDocument6 pagesHematology Written SummariesDrexler Ray EukanNo ratings yet
- Urease Test - Principle, Media, Procedure and ResultDocument11 pagesUrease Test - Principle, Media, Procedure and ResultAlisha KhanNo ratings yet
- Immunopharmacology: Dr. Hamad AlshabiDocument8 pagesImmunopharmacology: Dr. Hamad AlshabiHamad Alshabi100% (1)
- Role of Drugs That Affect Renin Angiotensin SystemDocument22 pagesRole of Drugs That Affect Renin Angiotensin Systemash ashNo ratings yet
- 33-Hemostasis and Coagulation ProfileDocument40 pages33-Hemostasis and Coagulation ProfileOsman Mohamed MuhumedNo ratings yet
- Intro To TDM and ToxicologyDocument46 pagesIntro To TDM and ToxicologyAl-hadad AndromacheNo ratings yet
- Vancomycin Protocol RQHRDocument15 pagesVancomycin Protocol RQHRl1o2stNo ratings yet
- Microanatomy pt1Document27 pagesMicroanatomy pt1poopziNo ratings yet
- Microbiology Summary 13 - 14 Part 1Document13 pagesMicrobiology Summary 13 - 14 Part 1Jessica MalinNo ratings yet
- Interpretation of Liver Enzyme Tests - A Rapid GuideDocument3 pagesInterpretation of Liver Enzyme Tests - A Rapid Guidesserggios100% (2)
- Clinical Chemistry 2 Lecture Notes in Trace ElementsDocument6 pagesClinical Chemistry 2 Lecture Notes in Trace ElementsMoira Pauline LibroraniaNo ratings yet
- Disorders of Coagulation and Thrombosis NotesDocument16 pagesDisorders of Coagulation and Thrombosis NotesleeNo ratings yet
- Therapeutic Drug MonitoringDocument8 pagesTherapeutic Drug MonitoringLourdette TorrefielNo ratings yet
- Component Therapy-Transfusion of TheDocument8 pagesComponent Therapy-Transfusion of TheGennelyn Ross Delos ReyesNo ratings yet
- Preload and AfterloadDocument28 pagesPreload and Afterloadapi-19916399100% (1)
- Diuretic DrugsDocument2 pagesDiuretic DrugsEngku ElisaNo ratings yet
- 'Aliah's Microbiology Notes1Document54 pages'Aliah's Microbiology Notes1Luqman Al-Bashir Fauzi100% (1)
- CC1 - Topic 1Document11 pagesCC1 - Topic 1Marie MontemarNo ratings yet
- Antibiotics in ActionDocument1 pageAntibiotics in Actionjuan esteban MonroyNo ratings yet
- 2023.PharmacologyLab - Trans14.CancerChemotherapyPart1 2Document5 pages2023.PharmacologyLab - Trans14.CancerChemotherapyPart1 2Lloyd LinNo ratings yet
- Mu 002Document10 pagesMu 002chandanNo ratings yet
- CBCDocument12 pagesCBCDaNa Al-jomah100% (1)
- Chapter 6 (Adrenergic Agonists)Document44 pagesChapter 6 (Adrenergic Agonists)Aneeza AhmadNo ratings yet
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDocument12 pagesRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Platelet Storage Pool Disorders PDFDocument4 pagesPlatelet Storage Pool Disorders PDFMano CempakaNo ratings yet
- Pharmacology: Fast and Dirty Board ReviewDocument7 pagesPharmacology: Fast and Dirty Board ReviewRochelleth7278No ratings yet
- Hemophilia and Coagulation Disorders: DR Nishant VermaDocument68 pagesHemophilia and Coagulation Disorders: DR Nishant VermaЮлия ЦыгановаNo ratings yet
- Toxicology and TDMDocument121 pagesToxicology and TDMteppie0917No ratings yet
- All Objectives HematologyDocument45 pagesAll Objectives HematologyNursing200980% (5)
- Carbapenams Uses And: ResistanceDocument89 pagesCarbapenams Uses And: Resistancetummalapalli venkateswara raoNo ratings yet
- Gene - Molecular and FunctionDocument81 pagesGene - Molecular and FunctionNadia Nur FitriaNo ratings yet
- Cytochrome P450 ChartDocument2 pagesCytochrome P450 ChartCristinaNo ratings yet
- Plasma ProteinsDocument8 pagesPlasma ProteinsAaryan50% (2)
- AntimicrobialsDocument1 pageAntimicrobialsRomaine Barrett100% (1)
- Disorders of Iron Kinetics and Heme MetabolismDocument12 pagesDisorders of Iron Kinetics and Heme MetabolismJoanne JardinNo ratings yet
- Chronic Myelogenous Leukemia (CML) - Causes, Symptoms, TreatmentDocument10 pagesChronic Myelogenous Leukemia (CML) - Causes, Symptoms, Treatmentnurul auliaNo ratings yet
- Systemic Lupus Erythematosus Lecture Salah Abdel BakyDocument8 pagesSystemic Lupus Erythematosus Lecture Salah Abdel Bakyahmed gabrNo ratings yet
- What Is The Oral Glucose Tolerance TestDocument2 pagesWhat Is The Oral Glucose Tolerance TestBianca Camille100% (1)
- Hypertension and Angina DrugsDocument158 pagesHypertension and Angina DrugsMelissa SalayogNo ratings yet
- HAEMOPOIESISDocument6 pagesHAEMOPOIESISDiyana ZahariNo ratings yet
- Clinical Chemistry Lecture KayzardnDocument3 pagesClinical Chemistry Lecture KayzardnHenry QuimbaNo ratings yet
- Genetic Polymorphisms Dan Its Role On Clinical ApplicationDocument104 pagesGenetic Polymorphisms Dan Its Role On Clinical ApplicationyuslipahNo ratings yet
- Carbapenamses in Antibiotic ResistanceDocument53 pagesCarbapenamses in Antibiotic Resistancetummalapalli venkateswara raoNo ratings yet
- Lecture Notes in Medical Technology - Lecture #5 - THYROID FUNCTION TESTSDocument14 pagesLecture Notes in Medical Technology - Lecture #5 - THYROID FUNCTION TESTSKat JornadalNo ratings yet
- Non Protein CompoundsDocument64 pagesNon Protein CompoundsAbigail Mayled LausNo ratings yet
- Innate ImmunityDocument9 pagesInnate Immunitynascha dumpNo ratings yet
- Antiviral DrugsDocument24 pagesAntiviral DrugsBurhan Nabi0% (1)
- BacteriaDocument168 pagesBacteriadenekeNo ratings yet
- Obese Patients - Medication Dosing RQHR - 3Document8 pagesObese Patients - Medication Dosing RQHR - 3Sarah Zielda NajibNo ratings yet
- CC Partii&III NotesDocument30 pagesCC Partii&III NotesAnielle Mongaya100% (1)
- Clinical Methods For Detecting Carbapenemases: What Should Your Lab UseDocument12 pagesClinical Methods For Detecting Carbapenemases: What Should Your Lab UseAlexandru MunteanNo ratings yet
- Molecular Diagnosis in HaematologyDocument23 pagesMolecular Diagnosis in HaematologyUmar'Farouq Oni100% (1)
- Thalassemia and HaemoglobinopathiesDocument28 pagesThalassemia and HaemoglobinopathiesJared Khoo Er HauNo ratings yet
- Overview of Immune SystemDocument49 pagesOverview of Immune SystemleeNo ratings yet
- Mixing Studies 1pp 08-13-15.pptx 0 PDFDocument49 pagesMixing Studies 1pp 08-13-15.pptx 0 PDFKholifah LintangNo ratings yet
- COMPLETE BLOOD COUNT Lecture GuideDocument9 pagesCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaNo ratings yet
- Problem Based Learning PDFDocument1 pageProblem Based Learning PDFGerald John PazNo ratings yet
- Phlebotomy: Phlebos - Greek Word Meaning "Vein" & Tome - "To Cut"Document5 pagesPhlebotomy: Phlebos - Greek Word Meaning "Vein" & Tome - "To Cut"Gerald John PazNo ratings yet
- Gene Therapy May Prevent Retinoschisis in Boys: ReviewDocument2 pagesGene Therapy May Prevent Retinoschisis in Boys: ReviewGerald John PazNo ratings yet
- GROUP11 Section1 PBL2 Gerald John PazDocument1 pageGROUP11 Section1 PBL2 Gerald John PazGerald John PazNo ratings yet
- The Impact of Teacher Presentation Style: (Please Email Me at For A References List.)Document5 pagesThe Impact of Teacher Presentation Style: (Please Email Me at For A References List.)kashanpirzadaNo ratings yet
- Problem BasedDocument3 pagesProblem BasedLady KweeNo ratings yet
- Videos On Drug Abuse. Guidelines For Finals Quiz 3 - 5Document1 pageVideos On Drug Abuse. Guidelines For Finals Quiz 3 - 5Gerald John PazNo ratings yet
- Concepts of Culture MediaDocument1 pageConcepts of Culture MediaGerald John PazNo ratings yet
- Biobanking For Human Microbiome Research Promise, Risks, and EthicsDocument15 pagesBiobanking For Human Microbiome Research Promise, Risks, and EthicsGerald John PazNo ratings yet
- Role of Microbiota in Immunity and InflammationDocument12 pagesRole of Microbiota in Immunity and InflammationGerald John PazNo ratings yet
- Case Studies On CoagulationDocument3 pagesCase Studies On CoagulationGerald John PazNo ratings yet
- Geopolitical Challenges For Infectious Disease Prevention and ControlDocument17 pagesGeopolitical Challenges For Infectious Disease Prevention and ControlGerald John PazNo ratings yet
- 1 s2.0 S0167701216302627 MainDocument8 pages1 s2.0 S0167701216302627 MainGerald John PazNo ratings yet
- Different Laboratory Service ModelsDocument1 pageDifferent Laboratory Service ModelsGerald John PazNo ratings yet
- Chapter 024Document49 pagesChapter 024Gerald John PazNo ratings yet
- Host Microbiomes and Their Interactions With Immune SystemDocument9 pagesHost Microbiomes and Their Interactions With Immune SystemGerald John PazNo ratings yet
- Chapter 021Document49 pagesChapter 021Gerald John PazNo ratings yet
- Chapter 022Document100 pagesChapter 022Gerald John PazNo ratings yet
- Chapter 002Document68 pagesChapter 002Gerald John PazNo ratings yet
- Managment and Planning PDFDocument53 pagesManagment and Planning PDFGerald John PazNo ratings yet
- Chapter 023Document34 pagesChapter 023Gerald John PazNo ratings yet
- Chapter 025Document31 pagesChapter 025Gerald John PazNo ratings yet
- Chapter 023Document34 pagesChapter 023Gerald John PazNo ratings yet
- Chapter 4Document39 pagesChapter 4Gerald John PazNo ratings yet
- The First Blind Man On Top of The WorldDocument1 pageThe First Blind Man On Top of The WorldGerald John PazNo ratings yet
- Managment and PlanningDocument53 pagesManagment and PlanningGerald John PazNo ratings yet
- Papa Bear of The Berenstain BearsDocument1 pagePapa Bear of The Berenstain BearsGerald John PazNo ratings yet
- Chapter 001Document83 pagesChapter 001Gerald John PazNo ratings yet
- Short Report: Genetics Islet Autoantibodies Can Discriminate Maturity-Onset Diabetes of The Young (MODY) From Type 1 DiabetesDocument7 pagesShort Report: Genetics Islet Autoantibodies Can Discriminate Maturity-Onset Diabetes of The Young (MODY) From Type 1 DiabetesGerald John PazNo ratings yet
- GROUP 6-Micro Biochem ResultsDocument2 pagesGROUP 6-Micro Biochem ResultsGerald John PazNo ratings yet
- Understanding Basics of EKG: by Alula A. (R III)Document37 pagesUnderstanding Basics of EKG: by Alula A. (R III)sky nutsNo ratings yet
- SofradexDocument3 pagesSofradexWahidNo ratings yet
- Application Technique Traction PDFDocument25 pagesApplication Technique Traction PDFAZOZ 19No ratings yet
- Functions of Liver and GallbladderDocument10 pagesFunctions of Liver and GallbladderSabiha WaseemNo ratings yet
- 8 Surgical Anatomy of TMJDocument11 pages8 Surgical Anatomy of TMJArchanaShenoyNo ratings yet
- Lung Scan: Safuan Awang Nuclear MedicineDocument19 pagesLung Scan: Safuan Awang Nuclear MedicineVeraaaNo ratings yet
- 4 2Document39 pages4 2Anonymous GWPdocUtNo ratings yet
- KS4 Physical Education: The Circulatory SystemDocument36 pagesKS4 Physical Education: The Circulatory SystemAjay Pal NattNo ratings yet
- Apsy 603 Dual Relationship Assignment 4Document18 pagesApsy 603 Dual Relationship Assignment 4api-161848380100% (1)
- URINARY SYSTEM 1 Copyright RevisedDocument5 pagesURINARY SYSTEM 1 Copyright RevisedSherida GibbsNo ratings yet
- Alatrol: Cetirizine Hydrochloride BPDocument1 pageAlatrol: Cetirizine Hydrochloride BPAfsana AfrinNo ratings yet
- Final Abstract and Paper Edit 26 April 2020 อ เปรม แก้แล้ว PDFDocument22 pagesFinal Abstract and Paper Edit 26 April 2020 อ เปรม แก้แล้ว PDFchanakarn Vipusmith100% (2)
- The African Roots of La Santa Muerte PDFDocument33 pagesThe African Roots of La Santa Muerte PDFAli Sarwari-Qadri67% (3)
- + +Sandra+Carter +TMJ+No+More+PDF+ (Ebook) PDFDocument49 pages+ +Sandra+Carter +TMJ+No+More+PDF+ (Ebook) PDFMassimiliano Marchionne0% (1)
- Aortic AneurysmDocument26 pagesAortic Aneurysmchetanm2563100% (1)
- NCM 106 IntroductionDocument126 pagesNCM 106 IntroductionYra JhaneNo ratings yet
- Sports NutritionDocument78 pagesSports NutritionnpurdonNo ratings yet
- Ineffective Health MaintenanceDocument6 pagesIneffective Health MaintenanceRYAN SAPLADNo ratings yet
- MSDS Refrigerant R407CDocument8 pagesMSDS Refrigerant R407Chambali bimatamaNo ratings yet
- WEB VTH 01292009Document28 pagesWEB VTH 01292009Dave L100% (1)
- Chapter 11 Occlusal Adjustment PDFDocument8 pagesChapter 11 Occlusal Adjustment PDFDavid ColonNo ratings yet
- Rosary Med BottleDocument2 pagesRosary Med BottlescrugglenampNo ratings yet
- Family Therapy For Autism Spectrum Disorders (Cto)Document21 pagesFamily Therapy For Autism Spectrum Disorders (Cto)Julie Rose AlboresNo ratings yet
- LT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewDocument3 pagesLT 2 Members: Raazia Jalil, Ali Amjad & Ali Raza: Project 2 Doctors InterviewfatimaNo ratings yet
- Aubf Chemical Examination Credits To The OwnerDocument19 pagesAubf Chemical Examination Credits To The Ownerchippai100% (2)
- Padlet 5z3qwhf8dn00Document2 pagesPadlet 5z3qwhf8dn00api-266658713No ratings yet
- Aplicación de Un Programa de Entrenamiento de Fuerza en Futbolistas Jovenes PDFDocument16 pagesAplicación de Un Programa de Entrenamiento de Fuerza en Futbolistas Jovenes PDFEsteban LopezNo ratings yet
- Integrated Application Form 97 2003 Compatible PDFDocument15 pagesIntegrated Application Form 97 2003 Compatible PDFdrchughNo ratings yet
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Tales from Both Sides of the Brain: A Life in NeuroscienceFrom EverandTales from Both Sides of the Brain: A Life in NeuroscienceRating: 3 out of 5 stars3/5 (18)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsFrom EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsRating: 4 out of 5 stars4/5 (5)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceFrom EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceRating: 4.5 out of 5 stars4.5/5 (516)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- A Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouFrom EverandA Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouRating: 4.5 out of 5 stars4.5/5 (62)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionFrom EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionRating: 4 out of 5 stars4/5 (811)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessFrom Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessRating: 4 out of 5 stars4/5 (33)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedFrom EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedRating: 4 out of 5 stars4/5 (11)
- Fast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperFrom EverandFast Asleep: Improve Brain Function, Lose Weight, Boost Your Mood, Reduce Stress, and Become a Better SleeperRating: 4.5 out of 5 stars4.5/5 (15)
- The Invention of Tomorrow: A Natural History of ForesightFrom EverandThe Invention of Tomorrow: A Natural History of ForesightRating: 4.5 out of 5 stars4.5/5 (5)
- Lymph & Longevity: The Untapped Secret to HealthFrom EverandLymph & Longevity: The Untapped Secret to HealthRating: 4.5 out of 5 stars4.5/5 (13)
- Who's in Charge?: Free Will and the Science of the BrainFrom EverandWho's in Charge?: Free Will and the Science of the BrainRating: 4 out of 5 stars4/5 (65)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorFrom EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorNo ratings yet
- All That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesFrom EverandAll That Remains: A Renowned Forensic Scientist on Death, Mortality, and Solving CrimesRating: 4.5 out of 5 stars4.5/5 (397)
- Wayfinding: The Science and Mystery of How Humans Navigate the WorldFrom EverandWayfinding: The Science and Mystery of How Humans Navigate the WorldRating: 4.5 out of 5 stars4.5/5 (18)
- Good Without God: What a Billion Nonreligious People Do BelieveFrom EverandGood Without God: What a Billion Nonreligious People Do BelieveRating: 4 out of 5 stars4/5 (66)
- Crypt: Life, Death and Disease in the Middle Ages and BeyondFrom EverandCrypt: Life, Death and Disease in the Middle Ages and BeyondRating: 4 out of 5 stars4/5 (4)
- The Lives of Bees: The Untold Story of the Honey Bee in the WildFrom EverandThe Lives of Bees: The Untold Story of the Honey Bee in the WildRating: 4.5 out of 5 stars4.5/5 (44)
- Human: The Science Behind What Makes Your Brain UniqueFrom EverandHuman: The Science Behind What Makes Your Brain UniqueRating: 3.5 out of 5 stars3.5/5 (38)
- Change Your Brain, Change Your Life (Before 25): Change Your Developing Mind for Real-World SuccessFrom EverandChange Your Brain, Change Your Life (Before 25): Change Your Developing Mind for Real-World SuccessRating: 4 out of 5 stars4/5 (18)
- Moral Tribes: Emotion, Reason, and the Gap Between Us and ThemFrom EverandMoral Tribes: Emotion, Reason, and the Gap Between Us and ThemRating: 4.5 out of 5 stars4.5/5 (115)