Professional Documents
Culture Documents
Critical Result Reporting
Uploaded by
Safiqulatif AbdillahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Critical Result Reporting
Uploaded by
Safiqulatif AbdillahCopyright:
Available Formats
Pathology Consultation / Special Article
Pathology Consultation on Reporting of Critical Values
Jonathan R. Genzen, MD, PhD,1 and Christopher A. Tormey, MD,2 for the Education Committee
of the Academy of Clinical Laboratory Physicians and Scientists
Key Words: Pathology consultation; Critical values; Critical results; Panic values; Laboratory results; Results reporting
DOI: 10.1309/AJCP9IZT7BMBCJRS
The ASCP is accredited by the Accreditation Council for Continuing
Medical Education to provide continuing medical education for physicians.
The ASCP designates this educational activity for a maximum of 1 AMA PRA
Category 1 Credit per article. This activity qualifies as an American Board
of Pathology Maintenance of Certification Part II Self-Assessment Module.
The authors of this article and the planning committee members and staff
have no relevant financial relationships with commercial interests to disclose.
Questions appear on p 643. Exam is located at www.ascp.org/ajcpcme.
Abstract
Case Scenario
Among the most important functions of a pathology
or laboratory medicine service is the clear, accurate,
and rapid communication of critical test results (critical
values) to patient care providers. Pathologists and
laboratory professionals are often confronted with
many obstacles in the reporting of such critical values,
including establishing clinically relevant criteria for
critical values, resolving difficulties in locating an
ordering provider when a critical value is obtained,
and ensuring that the provider understands the severity
and implications of a critical result when he or she
has questions. This article presents a hypothetical (yet
fairly common) clinical case scenario regarding critical
values and then provides an up-to-date discussion and
review of the literature on the reporting of critical
results.
A patient with atrial fibrillation who is receiving warfarin has an afternoon cardiology appointment for routine care
and anticoagulant monitoring. A basic metabolic profile and
prothrombin time are ordered. The specimen is transported to
the laboratory by courier, and laboratory testing is completed
at 7:30 PM. All values are within normal limits except for an
elevated potassium level (K+) of 6.9 mEq/L (6.9 mmol/L;
reference range, 3.2-5.2 mEq/L [3.2-5.2 mmol/L]) and a
prothrombin time of 64.7 seconds (reference range, 11.1-13.2
seconds), corresponding to an international normalized ratio
of 7.4. These results qualify as critical values by your clinical
laboratory policy, and the laboratory technologist attempts to
contact the ordering clinician by telephone. Calls to the physicians office are not forwarded to an answering service or
covering clinician, but rather directed to an office answering
machine. The ordering physician does not respond to pages
or telephone calls made to the contact numbers listed in the
hospital telephone directory or laboratory information system
(LIS). The laboratory technologist contacts the on-call pathology resident and asks for assistance.
Questions
1. What are laboratory critical values?
2. What are the requirements for critical value reporting?
3. How should clinical laborattories establish critical value
lists and determine appropriate thresholds?
4. Who should make and receive critical value
notifications?
5. How might critical value reporting be improved?
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:505-513
505
DOI: 10.1309/AJCP9IZT7BMBCJRS
505
505
CME/SAM
Upon completion of this activity you will be able to:
define the terms critical value and critical diagnosis.
examine obstacles associated with reporting critical values and
diagnoses in a laboratory setting.
discuss practical solutions for problems associated with critical value
reporting.
Genzen and Tormey / Critical Values
6. What are the responsibilities of pathologists and
laboratory directors in the critical value process?
Background
Lundberg1 first outlined the fundamental components
of critical value reporting in a Medical Laboratory Observer
article, describing critical laboratory values as values
which reflect pathophysiological derangements at such
variance with normal as to be life threatening if therapy is
not instituted immediately. They have more recently been
described as laboratory results that indicate a life-threatening situation for the patient. Because of their critical nature,
urgent notification of a critical value to the appropriate
healthcare professional is necessary.2 Alternative terms for
critical values include critical results, panic values, and alert
values. The term panic values carries a suggestion of emotional stress and runs against the thoughtful and organized
process of communicating important information clearly. Its
use is therefore discouraged.
Laboratories are required by numerous regulatory agencies to develop and put into practice critical value policies.3-6
Although the content of these policies varies according to
institutional needs, the core components are often quite similar. This article begins by describing the current regulatory
requirements for critical value reporting. This information
will be followed by a detailed analysis of the fundamental
components of critical value notification. Aspects of critical
value reporting that have been evaluated in the literature are
emphasized, as are current technological advances that may
change the way in which critical value reporting takes place.
Regulations
Critical value reporting is required by a variety of laws,
regulations, and accreditation programs. In the United States,
the Clinical Laboratory Improvement Amendments of 1988
(CLIA 88) include requirements on critical value reporting.
Current regulations specify that the laboratory manual must
address critical values (when applicable to test procedures),
along with protocols for reporting critical value results [see
493.1251 (b; 11 and 13); and 493.1291 (g)].6 The Joint
Commission (TJC) National Patient Safety Goals also address
critical value reporting. Specifically, Goal 2improve the
effectiveness of communication among caregiversincludes
report critical results of tests and diagnostic procedures in a
timely basis. This goal and its specific performance elements
were updated in 2010 and are available online.4 Of note, the
read-back requirement for results conveyed by telephone is
being changed to a formal standard. Read-back is imperative
506
506
Am J Clin Pathol 2011;135:505-513
DOI: 10.1309/AJCP9IZT7BMBCJRS
because significant error rates have been detected in the
process of telephone result communications.7,8 Additional
state, provincial, and local regulations regarding critical value
reporting may also exist and can be relevant to an individual
laboratorys performance requirements.
Critical value reporting is addressed by the College
of American Pathologists (CAP) Laboratory Accreditation
Program as part of several checklist components.3 These
items delineate the specific requirements for critical value procedures, including documentation of reporting and read-back
of verbally communicated results. Finally, the International
Organization for Standardization also includes critical value
reporting in its clinical laboratory standard ISO 15189:2007.5
Establishing a Critical Values List
Although there are many regulations specifying that laboratories must define and communicate critical values, it may
seem surprising that regulations do not state which laboratory
tests require critical value limits and notification. Indeed, individual clinical laboratories face unique challenges that reflect
institutional organization, clinical demand, patient population,
instrumentation, and staffing. Such variations have hindered
the development of universal standards for critical value
reporting across laboratories.
The idea of a universal critical value list is appealing
to many laboratorians and clinicians. For example, many
clinicians would likely consider a sodium (Na+) level of
168 mEq/L (168 mmol/L) a critical value regardless of
which laboratory performs the test. Indeed, the practice of
assigning the laboratory director responsibility for creating
and refining the critical value list has led to similar overall
inclusion of tests between laboratories without there being a
universal mandate or requirement. As an example, virtually
all laboratories include Na+ on their critical value list precisely because it is important for patient care. Furthermore,
not communicating a critically elevated Na+ level could
have medicolegal ramifications if an adverse clinical outcome occurred. Defining (and then mandating) a universal
set of thresholds for tests, however, would be a daunting task
given the scarcity of outcomes-based data on critical value
thresholds. Inherent variability in assay-specific reference
intervals between institutions is also a complicating factor.
An individual laboratory director can account for this variability by defining critical ranges consistent with his or her
own assays and instrumentation.
How should a laboratory determine which tests to include
on a critical value list? Moreover, how should the critical high
and low thresholds be established? While ultimately, this
determination is the responsibility of the laboratory director, it
should be made in communication with the clinicians who use
American Society for Clinical Pathology
Pathology Consultation / Special Article
laboratory services, as well as with a medical review board of
the institution, if applicable.3,9 This task may include meeting
with relevant physicians, medical and surgical section chiefs,
hospital administrators, and/or nurse managers to discuss critical value policies and to determine if there are any tests that
should be included (or omitted) and whether any thresholds
should be adjusted according to clinical needs.
Not every laboratory test should have critical values
associated with it. Critical value lists are, by nature, limited to
not hinder the clinical effectiveness of notification.1 Critical
lists that are too inclusive (or that have critical value thresholds that require excessive notification) place an unnecessary
burden on laboratory staff. Such lists annoy clinicians, foster
a negative attitude toward important laboratory services,
and, most important, provide uncertain additional benefit to
patient care. At the other extreme, lists that are too exclusive
(or with thresholds that are too high or low) might not prevent
adverse clinical outcomes, as a delay in the recognition of lifethreatening laboratory results by clinicians can be disastrous.
A balance must be achieved.
The best place to start when establishing or modifying
critical value lists is by comparison with previously published lists, practice parameters, and consensus documents
because these sources have been refined with the benefit of
time, institutional comparison, and clinical performance.2,9-18
Several published studies from CAP (Q-Probes and Q-Tracks)
have compared critical value reporting across hundreds of
institutions and are a valuable resource for critical value
policy assessment. The 1997 American Society for Clinical
Pathology Critical Values Practice Parameter (published in
the Journal) is another outstanding resource.9 Table 1 and
Table 22,3,9,13,14,16-21 present lists of common tests that frequently have critical values defined. Although most published
critical value lists do not include blood bank testing, we have
included a number of transfusion medicinerelated scenarios
that may benefit from rapid communication and discussion
with a responsible clinician.
It should be noted that most published reports focus
on critical value notifications in general laboratory testing,
although several studies of critical diagnoses in surgical
pathology and cytology have recently been published and
will be discussed later in this article. Finally, many institutions place their laboratory policies (including critical value
lists) online, facilitating comparison of lists between peer
laboratories.22-25
Critical Value Notification Procedures
The initial step in the critical value communication process
involves identification of an abnormal result by someone in the
laboratory.9 For automated assays, the instrument, middleware,
or LIS will notify the laboratory staff (usually the performing technologist) of the critical value. Laboratory policies
must clearly indicate whether the assay should be verified
and/or repeated before reporting and, if so, within what time
frame. Repeat testing is not feasible in many circumstances
(eg, blood culture results), and ongoing improvements in
laboratory assays may decrease the clinical usefulness of
routine repeat testing before reporting. This is a topic of
continued clinical interest and debate.
The National Patient Safety Goals state that laboratory
procedures must indicate by whom and to whom critical
results are reported, as well as the acceptable length of time
between the availability and reporting of critical results.4
Documentation is required. The CAP checklist (component
GEN.41330) specifies what information must be documented during critical value notifications, including date, time,
responsible laboratory individual, [and] person notified.3
Laboratory personnel who perform the actual tests are
currently responsible for making the vast majority of critical
value notifications. A 2008 survey of 121 institutions found
that approximately 90% of calls are made by medical technologists/technicians, 1% are made by client services or call
center staff, and 9% are made by a combination of the two.26
A 2002 survey of 623 institutions showed similar results,
with some differences between inpatient and outpatient
notification.13 That study recommended that critical value
notifications should be made by one of the team members
involved in performing the procedure.13 A separate 2008
survey of laboratory professionals and pathologists (at >350
hospitals) revealed that nearly 18% of respondents were
using a call center for critical value notifications.27 The
workflow benefits of centralized call centers (and having a
laboratory technologist or someone with laboratory expertise
involved in the call center mechanism) are well described in
the aforementioned survey and a separate 2008 CAP Today
feature article.27,28 Laboratories face an ever-increasing
dilemma in critical value notificationthe overall volume
of laboratory testing is increasing, but a continued shortage
in the number of laboratory professionals means that fewer
people are expected to do more. Shifting the task of critical
value notification away from laboratory technologists may
be inevitable at many institutions.
Indeed, several hospitals have implemented the use of
automated notification systems for critical value reporting.
At one institution, critical values transmitted from the LIS
to a hospital clinical information system trigger the generation of text messages directed to the responsible clinicians
mobile phone and computer.15 If the clinician does not
confirm receipt in the clinical information system within
60 minutes, results are communicated by telephone. This
approach improved the speed of communication and allowed
for full electronic documentation of critical value reporting.
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:505-513
507
DOI: 10.1309/AJCP9IZT7BMBCJRS
507
507
Genzen and Tormey / Critical Values
Table 1
Examples of Possible Critical Laboratory Values for Chemistry, Hematology/Coagulation, and Pediatric-Specific Ranges*
Chemistry
Blood urea nitrogen, mg/dL (mmol/L)
Calcium, mg/dL (mmol/L)
Total
Ionized
Carbon dioxide, total, mEq/L (mmol/L)
Chloride, mEq/L (mmol/L)
Creatinine, mg/dL (mol/L)
Glucose, mg/dL (mmol/L)
Glucose, CSF, mg/dL (mmol/L)
Lactate, mg/dL (mmol/L)
Magnesium, mg/dL (mmol/L)
Osmolality, mOsm/kg (mmol/kg)
Phosphate, mg/dL (mmol/L)
PO2, mm Hg (kPa)
PCO2, mm Hg (kPa)
pH
Potassium, mEq/L (mmol/L)
Sodium, mEq/L (mmol/L)
Troponin I or T
Uric acid, mg/dL (mol/L)
Hematology/coagulation
Prothrombin time, s
Partial thromboplastin time, s
Fibrinogen, mg/dL (mol/L)
Hemoglobin, g/dL (g/L)
Hematocrit, % (proportion of 1)
Platelet count, 103/L ( 109/L)
WBC count, 103/L ( 109/L)
Blasts
Organisms/parasites detected on smear review (CSF, blood,
or sterile body fluid)
Smear review suggestive of microangiopathic hemolytic
anemia (schistocytes and low platelet count)
Urinalysis (pathologic crystals)
WBC count, CSF (cells/L)
Pediatric-specific ranges
Ammonia, g/dL (mol/L)
Bilirubin, neonatal, mg/dL (mol/L)
Blood urea nitrogen, mg/dL (mmol/L)
Creatinine, mg/dL (mol/L)
Glucose, neonatal, mg/dL (mmol/L)
PO2, neonatal, mm Hg (kPa)
PCO2, neonatal, mm Hg (kPa)
Potassium, neonatal, mEq/L (mmol/L)
Sodium, pediatric, mEq/L (mmol/L)
Hemoglobin, neonatal, g/dL (g/L)
Hematocrit, neonatal, % (proportion of 1)
Platelet count, 103/L ( 109/L)
CSF
Glucose, mg/dL (mmol/L)
Protein, mg/dL (g/L)
WBC count, cells/L
0-1 y
1-4 y
5-17 y
Low Threshold
High Threshold
100 (35.7)
6.5 (1.6)
3.2 (0.8)
10 (10)
75 (75)
45 (2.5)
40 (2.2)
1.0 (0.4)
250 (250)
1.0 (0.3)
40 (5.3)
20 (2.7)
7.2
2.8 (2.8)
120 (120)
13 (3.3)
6.2 (1.6)
40 (40)
125 (125)
6.0 (530.4)
450 (25.0)
200 (11.1)
30.6 (3.4)
4.9 (2.0)
325 (325)
9.0 (2.9)
70 (9.3)
7.6
6.2 (6.2)
160 (160)
See comment
13 (773)
90 (2.6)
7 (70)
20 (0.2)
40 (40)
2 (2)
30
80
800 (23.5)
20 (200)
60 (0.6)
1,000 (1,000)
40 (40)
First observation
First observation
First observation
First observation
5
30 (1.7)
40 (5.3)
20 (2.7)
2.8 (2.8)
121 (121)
10 (100)
33 (0.33)
50 (50)
154 (110.0)
15 (256.5)
55 (19.6)
3.8 (335.9)
325 (18.0)
100 (13.3)
63 (8.4)
7.8 (7.8)
156 (156)
22 (220)
71 (0.71)
900 (900)
30 (1.7)
200 (11.1)
190 (1.9)
30
20
10
CSF, cerebrospinal fluid.
* Information in this table is meant as a starting point for the evaluation of a laboratorys critical value list and not as a strict guideline applicable to all clinical scenarios. The
table incorporates critical value data from the literature, particularly the outstanding reports from Kost,16-18,20,21 the College of American Pathologists Q-Probes studies,13,14
the ASCP Practice Parameter,9 a pediatric study by Gong and Adeli,12 and critical values included in the Tietz Textbook of Clinical Chemistry and Molecular Diagnostics.2
Systme International (SI) conversion factors can be found in textbooks.2 In many cases, SI values have been rounded to 1 decimal point for the purposes of clarity. Because
the table integrates information from multiple studies, tests (and ranges) may vary from individual sources and may not be representative of the original authors opinions. The
table is also not inclusive of all tests that may be considered critical. For example, it does not include toxicology and therapeutic drug monitoring owing to the diversity of tests
performed between individual institutions.
First result observed above an assay or laboratory-defined cutoff for myocardial infarction. A discussion of one laboratorys experience in establishing a troponin critical value
cutoff (in collaboration with the emergency department) can be found in a 2008 CAP Today feature article.19
An international normalized ratio equivalent (eg, >5) may also be used.
508
508
Am J Clin Pathol 2011;135:505-513
DOI: 10.1309/AJCP9IZT7BMBCJRS
American Society for Clinical Pathology
Pathology Consultation / Special Article
Table 2
Examples of Possible Critical Laboratory Values for Microbiology and Transfusion Medicine*
Microbiology
Positive Gram, acid-fast bacillus, or mycology stains of smears (CSF, blood, or sterile body fluid)
Positive blood cultures
Positive CSF cultures
Positive sterile body fluid cultures
Positive stool culture for select organisms
Positive bacterial antigen tests
Transfusion medicine
Gross, visible hemolysis in a posttransfusion reaction specimen
Positive direct antiglobulin test (IgG and/or C3) in a posttransfusion reaction specimen
Evidence of crossmatch incompatibility with a posttransfusion reaction specimen
Discrepancy in identifiers noted on a blood product label, tag, or container during transfusion reaction evaluation
Positive blood cultures from a unit implicated in a transfusion reaction
Discovery of a new alloantibody in a patient undergoing surgery
CSF, cerebrospinal fluid.
* Information in this table is meant as a starting point for the evaluation of a laboratorys critical value list and not as a strict guideline applicable to all clinical scenarios.
We have included possible transfusion medicine scenarios that would benefit from prompt communication with a responsible clinician, although most published critical value
lists do not specifically include blood bank testing.
At another institution, an automated paging system was
developed for critical value notification.11 In that program,
critical values transmitted from the LIS generate a page containing the patient name, medical record number, collection
time, critical result, and reference range. The clinician must
confirm receipt of the critical value by dialing a phone number
listed in the message. If the clinician does not respond within
10 minutes (or rejects the notification), the call is escalated to
a trained group of operators who proceed with telephone notification. Implementation of that system increased documentation of critical value receipt by physicians and decreased the
median time for notification. Several other studies have also
evaluated the role of automated paging systems in critical
value reporting.29,30
It should be emphasized that automated solutions should
allow for an escalation policy (see the next section) to ensure
communication of critical results when clinicians do not
acknowledge receipt.10 Laboratory contact information should
also be available so that clinicians with additional questions
can ask a laboratory professional or medical director as appropriate. Patient privacy requirements should also be considered
with automated solutions because data conceivably might
be transmitted and stored on nonencrypted devices. Finally,
device compatibility with alphanumeric characters (particularly units) and character limits should also be evaluated
because an inaccurate or incomplete notification could lead to
medical error and adverse clinical outcome.
To whom should critical values be reported? The rationale
stated in the National Patient Safety Goals states that results are
to be conveyed to the responsible licensed caregiver.4 The
CAP checklists describe notification to a physician (or other
clinical personnel responsible for patient care) and the appropriate clinical individual.3 CLIA refers to the individual
or entity requesting the test and, if applicable, the individual
responsible for using the test results [493.1291 (g)].6
A 2007 survey of 163 clinical laboratories asked the question Who can receive critical values? for the inpatient and
outpatient settings.14 As expected, answers from virtually all
facilities included any licensed caregiver, ordering physician,
on-call physician, or resident.14 Many laboratories, however,
also permitted administrative personnel (ward clerks or receptionists) to accept critical values for outpatients (48%) and
inpatients (27%). A separate 2008 study showed that almost
18% of institutions authorized release to other staff (eg, ward
clerks and/or unit secretaries).26 In that study, the calls made
to other providers occurred slightly more quickly than those
made to licensed caregivers. Any timesaving was lost, however, when factoring in the subsequent time it took this other
provider to then contact a licensed caregiver. The authorized
agent approach to critical value notification (calling someone
whom a licensed caregiver specifies can receive critical value
notifications but is not necessarily capable or authorized to act
on them independently) should be discouraged. Many facilities allow for reporting of critical values directly to licensed
nurses, who are then responsible for conveying these results
to ordering and/or covering physicians. According to most
regulatory agencies, this would also be an acceptable practice
as long as there is documentation that the critical value was
then conveyed by the nurse to the ordering physician and/or
licensed caregiver.
As an alternative, some hospital networks have adopted
a policy of reporting all critical values generated from the
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:505-513
509
DOI: 10.1309/AJCP9IZT7BMBCJRS
509
509
Genzen and Tormey / Critical Values
outpatient setting during off hours to a hospital emergency
department (ED) or triage center. For example, the standard
operating procedure at many Veterans Administration hospitals is to report critical results to an ED attending physician,
who can then decide whether to act on these results. This
approach works well for Veterans Administration hospitals,
particularly because of the extensive electronic medical record
(EMR) available to all clinicians. Such a call reporting system
may be of limited benefit, however, at institutions with less
robust EMRs. Results would still need to be conveyed to the
responsible clinician for long-term management.
about a patients medical history and the potential ramifications of the critical value.
We ultimately advocate for active involvement of a
pathology resident, an attending pathologist, and/or a medical
director in difficult-to-convey critical value calls. It has been
our experience that this involvement usually opens avenues
(eg, investigations via the EMR) that are not readily available to bench technologists. Such interventions can ultimately
result in more rapid communication to a clinician familiar
with the patient involved.
Repeat Critical Values
Escalation Policies
What should a laboratory do when a technologist is not
able to reach a responsible clinician with the critical value?
In these circumstances, abandoning the call entirely is almost
never an acceptable solution. An escalation policy or a failsafe mechanism can be beneficial in such circumstances. An
escalation policy would direct the laboratory technologist
to contact a supervisor, pathology resident, and/or medical
director to assist in critical value notification.28 This policy
allows the technologist to refocus on the important task of
laboratory testing, and it transfers the responsibility for notification to people who may have greater access to an inpatient
or outpatient EMR and who can put the finding in a broader
clinical context. In our experience, the pathology and laboratory medicine residents are usually able to contact a covering
physician and convey these critical results. Verification of clinician notification should be subsequently conveyed back to
the laboratory technologist (and entered into the LIS) to comply with TJC and CAP requirements. A fail-safe mechanism
(or safety net) can also be used in cases in which notification
continues to be unsuccessful.13,31 For example, if a physician representing the laboratory determines that immediate
care of the patient may be required, the laboratory result and
patient information might be conveyed to a physician in the
ED to contact the patient directly.13
An approach to dealing with unreachable clinicians was
recently proposed in a 2010 article.32 The report included
algorithms for the inpatient and outpatient settings. After trying to contact the ordering provider, the algorithms include
attempting to identify and contact the patients primary care
provider. If still unsuccessful, a chief of service or chief of
staff would ultimately be notified. This system has an added
benefit of bringing the issue of critical value reporting to the
attention of a hospital or departmental administrator who
might not otherwise be aware of problems associated with
the process. However, as with other systems in which the
ordering provider is not the physician ultimately receiving the
call, this process involves clinicians who may know very little
510
510
Am J Clin Pathol 2011;135:505-513
DOI: 10.1309/AJCP9IZT7BMBCJRS
Another common problem in critical value reporting is
how a laboratory should handle repeat critical values, or subsequent critical values for a given assay on the same patient
(but subsequent specimen). Approximately 70% of surveyed
laboratories have a policy on repeat critical values.27 For
those that do not, one is strongly recommended because it
will clarify laboratory technologist responsibility and establish consistency in performance. There are only 3 options: (1)
Call only the first critical value. (2) Call each critical value.
(3) Call critical values once per interval of time.
As clinicians become quickly annoyed by repetitive
calls for critical values, and as such calls may have diminishing value over time, some advocate using interval criteria
(for example, calling once every 24 hours).13 Determining
whether critical results meet interval criteria might add
additional tasks to laboratory technologists, although LIS
or middleware-based rules can be used to perform comparisons automatically. Others have suggested that interval
calling is appropriate for only select analytes.9 Of note,
one study demonstrated that lower rates of undocumented
critical value results in the medical record were associated
with policies that require calling all critical results.33 Such
an approach in high-volume laboratories, however, can be
exceedingly burdensome to technologists and clinical staff,
and there are minimal data to argue the clinical benefit of
one approach vs the other.
Critical value lists and procedures should include not just
critical ranges but also the frequency of when to call for each
given test. A laboratory may determine that some tests should
be called with each critical value, while others (such as a markedly elevated blood urine nitrogen level) may be called using
an interval approach. The laboratory policy should also clarify
how to handle critical value notification after a subsequent
normal result during the same interval (eg, 8 AM, critical high;
9 AM, normal; then 10 AM, critical high). In our policies, if a
normal test result occurs after a critical result, a subsequent
critical result is considered new and would be called again. The
laboratorys policy should be clear for such scenarios.
American Society for Clinical Pathology
Pathology Consultation / Special Article
Critical Value Audits
The importance of using critical value data to better understand laboratory process and preanalytic error cannot be overemphasized. For example, one program identified a specimen
transport issue that led to falsely elevated K+ results in some
patients.27 Changing the transport requirements decreased
the number of critical high K+ results. This change not only
enhanced the quality of the laboratorys performance but also
eased the burden of unnecessary critical value calls. Analysis
of critical value limits can also be used to estimate the impact
on call frequency that would result from changing threshold
requirements.10 Analysis can reveal differences in critical
value patterns by patient location (eg, falling hematocrit values
on surgical services vs low K+ values on medical services).30
This information could be used, for example, in the evaluation
of new point-of-care programs. Others have used critical values analysis in studies of adverse events and clinical activity
at discrete hospital locations.34 Critical value audits provide
tremendous information on laboratory processes, and they are
a great starting point for quality improvement initiatives.
Opt-Out and Specific Lists
Physician opt-out of critical value notifications (or no
call hours) were prohibited by more than 80% of programs surveyed in one study.14 Opt-out is also strongly discouraged in the
CAP checklist.3 The laboratory has a clear mandate to convey
critical values, and permitting physician opt-out runs counter to
the overall patient care objective of the notification process.
Physician- and/or location-specific critical value lists
are another issue of controversy. For example, clinicians at
a dialysis clinic may be concerned about a different range of
electrolyte results than clinicians at an orthopedics rehabilitation unit. Maintaining multiple, separate lists in the laboratory
can be challenging (if not impossible) at most institutions and
would be prone to technologist error in underreporting and
overreporting of critical results. Physician- and/or locationspecific lists are not in widespread use.
Many laboratories, however, include some populationspecific critical values. Critical value lists often include
unique limits for neonates, but these values are easily incorporated onto a single laboratory-wide critical value list and
would not be maintained separately. Tables including pediatrics critical value limits are available,2,14,16 and one study
on interlaboratory variability in pediatric critical values was
recently published.12
Critical Diagnoses in Anatomic Pathology
Anatomic pathologists evaluate organs, tissues, and
cellular specimens and provide diagnoses when abnormal
findings are observed. Preanalytic and analytic processes (eg,
gross examination, tissue slicing, staining, and immunohistochemical analysis) often mean that hours to days may pass
before a diagnosis can be made. In certain circumstances,
the diagnosis suggests that immediate treatment or prompt
evaluation of the patient may be indicated.35 This concept of
critical diagnoses in surgical pathology and cytology (analogous to critical values in the clinical laboratory) has received
significant attention in recent years.35-43
For example, several retrospective reviews and multiinstitutional surveys led to the creation of a list of possible
critical diagnoses in anatomic pathology and cytology Table
3.35-39,42,44 Even though these conditions were suggested as
being important for immediate communication, the authors
found an overall lack of consensus from participants on what
might actually be included on such lists.35-37
In fact, there are no specific national guidelines as to what
types of diagnoses in surgical pathology should qualify as
critical. The concept of critical diagnoses, however, has been
endorsed by the Association of Directors of Anatomic and
Surgical Pathology, and a generic list of possible diagnoses
was published in 2006 based on the aforementioned studies,
with the caveat that any such list needs to be customized
to each individual hospital based on specific requests from
clinicians and institutional factors such as the scope of services provided, case mix, acuity level, and protocols.38,42,44
Finally, there is no consensus on how to actually report these
diagnoses nor on the appropriate time frame for communication.38,40,45,46 In the absence of specific guidelines, it will
remain necessary for institutions to establish local, customized protocols for handling critical diagnoses.
Table 3
Examples of Possible Critical Diagnoses in Anatomic
Pathology35-39,42,44
Surgical pathology
Crescents in >50% of glomeruli in a kidney biopsy specimen
Vasculitis
Bacteria in a heart or bone marrow specimen
Select organisms in immunocompromised patients
Uterine contents without villi or trophoblast
Fat in an endometrial curettage
Mesothelial cells in a cardiac biopsy specimen
Fat in colonic endoscopic polypectomy specimens
Transplant rejection
Malignancy in superior vena cava syndrome
Neoplasms causing paralysis
Significant disagreement between frozen section and
final diagnoses
Cytology
Unexpected malignancy
Malignancy in critical places that can cause spinal cord injury
Disagreement between immediate and final interpretations of
FNA specimens
Fungi in an FNA specimen from an immunocompromised patient
The finding of certain microorganisms in any patient
FNA, fine-needle aspiration.
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:505-513
511
DOI: 10.1309/AJCP9IZT7BMBCJRS
511
511
Genzen and Tormey / Critical Values
Conclusion
Along with the entire team of personnel involved in critical value notifications, pathologists and/or laboratory directors have an important role in many aspects of critical value
reporting. They are involved in establishing and updating the
critical value lists and policies (in consultation with clinicians
and institutional medical boards), they assist in critical value
escalation and interpretations, they are responsible for ensuring compliance with TJC- and CAP-required documentation,
and they can use critical values audits to improve overall
laboratory performance. Technological advancements will
certainly alter the way in which critical value notifications are
made, but these will not change the overall responsibility of
pathologists and laboratory directors for ensuring compliance
with critical value notification requirements. A recent CAP
Today Q&A discussion on critical value notification concluded by stating that a focus on building a patient-centric
system requires strong pathologist leadership to ensure a safe
and reliable system.31 As such, a strong commitment to the
critical value notification process can enhance overall patient
care and should be a focus of ongoing quality improvement.
Case Summary
After being unable to contact a covering physician, the
laboratory technologist paged the on-call pathology resident.
The resident had access to the outpatient EMR and noticed that
a cardiology fellow (and not the patients primary attending
physician) wrote the clinic notes. The on-call cardiology fellow was paged by the resident and stated that she was familiar
with the patient. She accepted the critical results, performed
appropriate read-back, and contacted the patient for clinical
follow-up. The resident called back the laboratory technologist
and provided necessary information for documentation of the
critical value notification. On investigation the next day, it was
determined that a new member of the outpatient office staff did
not know how to set the telephone system appropriately to forward calls to the answering service. The telephone (and pager)
directory was updated for all physicians at this clinic.
From the 1Department of Pathology and Laboratory Medicine,
Weill Cornell Medical College, Cornell University, and New
York-Presbyterian Hospital, New York, NY; and 2Department of
Laboratory Medicine, Yale University School of Medicine, New
Haven, CT, and the Pathology and Laboratory Medicine Service,
VA Connecticut Healthcare System, West Haven.
Address reprint requests to Dr Genzen: Weill Cornell
Medical College, 525 E 68th St, F-705, New York, NY 10065.
References
1. Lundberg G. When to panic over an abnormal value. Med
Lab Obs. 1972;4:47-54.
512
512
Am J Clin Pathol 2011;135:505-513
DOI: 10.1309/AJCP9IZT7BMBCJRS
2. Burtis C, Ashwood E, Bruns D, eds. Tietz Textbook of Clinical
Chemistry and Molecular Diagnostics. 4th ed. St Louis, MO:
Elsevier Saunders; 2006.
3. College of American Pathologists. Laboratory General
Checklist [components GEN.41320, GEN.41330, and
GEN.41340]. Available at www.cap.org. Accessed August 6,
2010.
4. The Joint Commission. Accreditation Program: Laboratory,
National Patient Safety Goals (NPSG.02.03.01). http://www.
jointcommission.org/. Accessed July 12, 2010.
5. International Organization for Standardization. ISO
15189:2007: medical laboratories: particular requirements
for quality and competence [items 5.5.3n, 5.8.7, and 5.8.8].
Available at www.iso.org. Accessed August 7, 2009.
6. Medicare, Medicaid, and CLIA Programs: laboratory
requirements relating to quality systems and certain personnel
qualifications. Fed Regist. 2003;68:3639-3714. Codified at 42
CFR 493.
7. Barenfanger J, Sautter RL, Lang DL, et al. Improving patient
safety by repeating (read-back) telephone reports of critical
information. Am J Clin Pathol. 2004;121:801-803.
8. Rensburg MA, Nutt L, Zemlin AE, et al. An audit on the
reporting of critical results in a tertiary institute. Ann Clin
Biochem. 2009;46:162-164.
9. Emancipator K. Critical values: ASCP practice parameter.
Am J Clin Pathol. 1997;108:247-253.
10. Dighe AS, Rao A, Coakley AB, et al. Analysis of laboratory
critical value reporting at a large academic medical center.
Am J Clin Pathol. 2006;125:758-764.
11. Parl FF, OLeary MF, Kaiser AB, et al. Implementation of a
closed-loop reporting system for critical values and clinical
communication in compliance with goals of the Joint
Commission. Clin Chem. 2010;56:417-423.
12. Gong Y, Adeli K. A national survey on pediatric critical
values used in clinical laboratories across Canada. Clin
Biochem. 2009;42:1610-1615.
13. Howanitz PJ, Steindel SJ, Heard NV. Laboratory critical
values policies and procedures: a college of American
Pathologists Q-Probes study in 623 institutions. Arch Pathol
Lab Med. 2002;126:663-669.
14. Wagar EA, Friedberg RC, Souers R, et al. Critical values
comparison: a College of American Pathologists Q-Probes
survey of 163 clinical laboratories. Arch Pathol Lab Med.
2007;131:1769-1775.
15. Piva E, Sciacovelli L, Zaninotto M, et al. Evaluation of
effectiveness of a computerized notification system for
reporting critical values. Am J Clin Pathol. 2009;131:432-441.
16. Kost GJ. Table of critical limits. MLO Med Lab Obs.
2004;36(13 suppl):6-7.
17. Kost GJ. Critical limits for urgent clinician notification at US
medical centers. JAMA. 1990;263:704-707.
18. Kost GJ. Clinical and professional reference guides: table of
critical limits. MLO Med Lab Obs. 2001;33:12-13.
19. Lusky K. Critical values: looking more closely at calls, cutoffs.
CAP Today. November 2008:80.
20. Kost GJ. Critical limits for emergency clinician notification
at United States childrens hospitals. Pediatrics.
1991;88:597-603.
21. Kost GJ. The significance of ionized calcium in cardiac and
critical care: availability and critical limits at US medical
centers and childrens hospitals. Arch Pathol Lab Med.
1993;117:890-896.
American Society for Clinical Pathology
Pathology Consultation / Special Article
22. Massachusetts General Hospital Pathology Service.
Laboratory Handbook. http://mghlabtest.partners.org/
CriticalValues.htm. Accessed September 27, 2010.
23. Brigham and Womens Hospital. Clinical Laboratory Manual.
http://www.brighamandwomens.org/clinicallabs/medical/
resources.aspx. Accessed October 3, 2010.
24. Mayo Medical Laboratories. Critical Values and Semi-Urgent
Results. http://www.mayomedicallaboratories.com/articles/
criticalvalues/index.html. Accessed October 2, 2010.
25. Yale-New Haven Hospital. Laboratory Manual. https://
labmanual.ynhh.org/. Accessed October 1, 2010.
26. Valenstein PN, Wagar EA, Stankovic AK, et al. Notification
of critical results: a College of American Pathologists
Q-Probes study of 121 institutions. Arch Pathol Lab Med.
2008;132:1862-1867.
27. Dighe AS, Jones JB, Parham S, et al. Survey of critical value
reporting and reduction of false-positive critical value results.
Arch Pathol Lab Med. 2008;132:1666-1671.
28. Dighe AS. Making the right calls on critical values, tests.
CAP Today. August 2008:12.
29. Etchells E, Adhikari NK, Cheung C, et al. Real-time clinical
alerting: effect of an automated paging system on response
time to critical laboratory values: a randomised controlled
trial. Qual Saf Health Care. 2010;19:99-102.
30. Kuperman GJ, Teich JM, Tanasijevic MJ, et al. Improving
response to critical laboratory results with automation: results
of a randomized controlled trial. J Am Med Inform Assoc.
1999;6:512-522.
31. Hernandez JS. Q & A. CAP Today. May 2010:94.
32. Singh H, Vij MS. Eight recommendations for policies for
communicating abnormal test results. Jt Comm J Qual Patient
Saf. 2010;36:226-232.
33. Wagar EA, Stankovic AK, Wilkinson DS, et al. Assessment
monitoring of laboratory critical values: a College of
American Pathologists Q-Tracks study of 180 institutions.
Arch Pathol Lab Med. 2007;131:44-49.
34. Jenkins JJ, Crawford JM, Bissell MG. Studying critical values:
adverse event identification following a critical laboratory
values study at the Ohio State University Medical Center.
Am J Clin Pathol. 2007;128:604-609.
35. Pereira TC, Liu Y, and Silverman JF. Critical values in
surgical pathology. Am J Clin Pathol. 2004;122:201-205.
36. Pereira TC, Clayton AC, Tazelaar HD, et al. Critical values
in cytology. Diagn Cytopathol. 2006;34:447-451.
37. Pereira TC, Silverman JF, LiVolsi V, et al. A multiinstitutional survey of critical diagnoses (critical values)
in surgical pathology and cytology. Am J Clin Pathol.
2008;130:731-735.
38. Silverman JF. Critical diagnoses (critical values) in anatomic
pathology. Am J Clin Pathol. 2006;125:815-817.
39. Silverman JF, Pereira TC. Critical values in anatomic
pathology. Arch Pathol Lab Med. 2006;130:638-640.
40. Visscher DW. What values are critical [editorial]? Am J Clin
Pathol. 2008;130:681-682.
41. Huang EC, Kuo FC, Fletcher CD, et al. Critical diagnoses in
surgical pathology: a retrospective single-institution study to
monitor guidelines for communication of urgent results. Am J
Surg Pathol. 2009;33:1098-1102.
42. Silverman JF, LiVolsi VA, Fletcher CD, et al. Critical
diagnoses (critical values) in anatomic pathology. Am J Surg
Pathol. 2006;30:897-899.
43. Allen TC. Critical values in anatomic pathology? Arch Pathol
Lab Med. 2007;131:684-687.
44. Silverman JF, Fletcher CD, Frable WJ, et al. Critical
diagnoses (critical values) in anatomic pathology. Hum
Pathol. 2006;37:982-984.
45. LiVolsi VA, Leung S. Communicating critical values in
anatomic pathology. Arch Pathol Lab Med. 2006;130:641-644.
46. LiVolsi VA. Critical values in anatomic pathology:
how do we communicate [editorial]? Am J Clin Pathol.
2004;122:171-172.
American Society for Clinical Pathology
Am J Clin Pathol 2011;135:505-513
513
DOI: 10.1309/AJCP9IZT7BMBCJRS
513
513
You might also like
- Principles and Applications of Clinical Mass Spectrometry: Small Molecules, Peptides, and PathogensFrom EverandPrinciples and Applications of Clinical Mass Spectrometry: Small Molecules, Peptides, and PathogensNader RifaiNo ratings yet
- Microbiology and Molecular Diagnosis in Pathology: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeFrom EverandMicrobiology and Molecular Diagnosis in Pathology: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Safe Blood: Purifying the Nations Blood Supply in the Age of AFrom EverandSafe Blood: Purifying the Nations Blood Supply in the Age of ANo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Tietz's Applied Laboratory MedicineFrom EverandTietz's Applied Laboratory MedicineMitchell G. ScottRating: 3 out of 5 stars3/5 (1)
- IMMUNOHEMATOLOGY AND BLOOD BANKING: Passbooks Study GuideFrom EverandIMMUNOHEMATOLOGY AND BLOOD BANKING: Passbooks Study GuideRating: 1 out of 5 stars1/5 (1)
- Senior Medical Laboratory Technician: Passbooks Study GuideFrom EverandSenior Medical Laboratory Technician: Passbooks Study GuideNo ratings yet
- Clinical Chemistry, Immunology and Laboratory Quality Control: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeFrom EverandClinical Chemistry, Immunology and Laboratory Quality Control: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeRating: 5 out of 5 stars5/5 (1)
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Transfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeFrom EverandTransfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeRating: 3 out of 5 stars3/5 (1)
- Handbook of Transfusion MedicineFrom EverandHandbook of Transfusion MedicineChristopher HillyerRating: 4 out of 5 stars4/5 (4)
- Medical Laboratory Technician Career JournalDocument2 pagesMedical Laboratory Technician Career Journalapi-406104878100% (1)
- Introduction to Medical Laboratory TechnologyFrom EverandIntroduction to Medical Laboratory TechnologyRating: 2.5 out of 5 stars2.5/5 (7)
- Code of Ethics Guidance DocumentDocument30 pagesCode of Ethics Guidance DocumentASHVINBHAI VACHHANI100% (1)
- Transfusion Medicine and Hemostasis: Clinical and Laboratory AspectsFrom EverandTransfusion Medicine and Hemostasis: Clinical and Laboratory AspectsRating: 4 out of 5 stars4/5 (9)
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListPeng KwanNo ratings yet
- Introduction of Clinical BiochemistryDocument32 pagesIntroduction of Clinical BiochemistryKaren LowNo ratings yet
- Quality Control2Document32 pagesQuality Control2Mustafa KhandgawiNo ratings yet
- Transfusion Medicine, Apheresis, and Hemostasis: Review Questions and Case StudiesFrom EverandTransfusion Medicine, Apheresis, and Hemostasis: Review Questions and Case StudiesRating: 5 out of 5 stars5/5 (2)
- TextbookReferenceList MLA 2017Document3 pagesTextbookReferenceList MLA 2017APNo ratings yet
- Board of Directors: Ascp-Ascp Certification & Qualification Comparison ChartDocument1 pageBoard of Directors: Ascp-Ascp Certification & Qualification Comparison ChartMustaffah KabelyyonNo ratings yet
- Clinical Chemistry - Theory, Analysis, CorrelationDocument344 pagesClinical Chemistry - Theory, Analysis, Correlationaristides.quinteroNo ratings yet
- FlaggingDocument65 pagesFlaggingTony KurniawanNo ratings yet
- Accurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionFrom EverandAccurate Results in the Clinical Laboratory: A Guide to Error Detection and CorrectionRating: 5 out of 5 stars5/5 (1)
- ML7111 MCQs Answers Sep 2019Document10 pagesML7111 MCQs Answers Sep 2019Cleo Salvador100% (2)
- Ascp International Procedures BookDocument25 pagesAscp International Procedures BookDegee O. Gonzales100% (1)
- ABO DiscrepanicesDocument12 pagesABO DiscrepanicesGlenn PerezNo ratings yet
- Essentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationFrom EverandEssentials of ABO -Rh Grouping and Compatibility Testing: Theoretical Aspects and Practical ApplicationRating: 5 out of 5 stars5/5 (1)
- Self-assessment Q&A in Clinical Laboratory Science, IIIFrom EverandSelf-assessment Q&A in Clinical Laboratory Science, IIIRating: 3 out of 5 stars3/5 (1)
- Lab Policies Complete Blood Count of Whole Blood On The Sysmex KX 21N - RB Lab 1535Document20 pagesLab Policies Complete Blood Count of Whole Blood On The Sysmex KX 21N - RB Lab 1535tomNo ratings yet
- CSMLS C2 QuestionsDocument49 pagesCSMLS C2 QuestionsApollo Ochieng100% (1)
- Pathogenesis, Treatment and Prevention of LeishmaniasisFrom EverandPathogenesis, Treatment and Prevention of LeishmaniasisMukesh SamantNo ratings yet
- Hematology and Coagulation: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeFrom EverandHematology and Coagulation: A Comprehensive Review for Board Preparation, Certification and Clinical PracticeNo ratings yet
- Laboratory Quality ControlDocument63 pagesLaboratory Quality Control"DocAxi" Maximo B Axibal Jr MD FPSPNo ratings yet
- Techniques in Clinical Chemistry: A Handbook for Medical Laboratory TechniciansFrom EverandTechniques in Clinical Chemistry: A Handbook for Medical Laboratory TechniciansNo ratings yet
- I JomedDocument23 pagesI JomedSafiqulatif AbdillahNo ratings yet
- I JomedDocument23 pagesI JomedSafiqulatif AbdillahNo ratings yet
- Guide To Surgical Site MarkingDocument24 pagesGuide To Surgical Site MarkingSafiqulatif AbdillahNo ratings yet
- 4612 Early Warning Score (June 2013)Document8 pages4612 Early Warning Score (June 2013)Safiqulatif AbdillahNo ratings yet
- VentilationDocument7 pagesVentilationDodowi CspogNo ratings yet
- 10 Facts On Patient SafetyDocument3 pages10 Facts On Patient SafetySafiqulatif AbdillahNo ratings yet
- QPS Sample GuidelinesDocument23 pagesQPS Sample GuidelinesSafiqulatif AbdillahNo ratings yet
- SkriningDocument6 pagesSkriningSafiqulatif AbdillahNo ratings yet
- Preventing Patient ReboundsDocument11 pagesPreventing Patient ReboundsSafiqulatif AbdillahNo ratings yet
- Reducing Hospital ReadmissionDocument6 pagesReducing Hospital ReadmissionSafiqulatif AbdillahNo ratings yet
- Policy Critical ResultDocument6 pagesPolicy Critical ResultSafiqulatif AbdillahNo ratings yet
- Preventing Patient ReboundsDocument11 pagesPreventing Patient ReboundsSafiqulatif AbdillahNo ratings yet
- Cdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008Document158 pagesCdc-Guideline For Disinfection and Sterilization in Health-Care Facilities-2008fuentenatura100% (1)
- PPI Di HD Versi CDCDocument63 pagesPPI Di HD Versi CDCSafiqulatif AbdillahNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Governance Board Manual QualityDocument22 pagesGovernance Board Manual QualitySafiqulatif AbdillahNo ratings yet
- Board Committees and TOR QPS CommitteeDocument44 pagesBoard Committees and TOR QPS CommitteeSafiqulatif AbdillahNo ratings yet
- TOI Breaking Bad NewsDocument15 pagesTOI Breaking Bad NewsSafiqulatif AbdillahNo ratings yet
- 2013-2014 Clinical Pathway ApplicationDocument7 pages2013-2014 Clinical Pathway ApplicationSafiqulatif AbdillahNo ratings yet
- International Hospital Inpatient Quality MeasuresDocument1 pageInternational Hospital Inpatient Quality MeasuresSafiqulatif AbdillahNo ratings yet
- Practice Guidelines For Chronic Pain Management .13Document24 pagesPractice Guidelines For Chronic Pain Management .13Safiqulatif AbdillahNo ratings yet
- NationalguidelinesDocument26 pagesNationalguidelines18saNo ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Obat YanmedDocument2 pagesObat YanmedSafiqulatif AbdillahNo ratings yet
- Para Lec CombinedDocument83 pagesPara Lec CombinedClent Earl Jason O. BascoNo ratings yet
- Preview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextDocument24 pagesPreview: Proquest Dissertations and Theses 2002 Proquest Dissertations & Theses Full TextFelipe AguilarNo ratings yet
- Practice For Mounting Buses & Joints-374561Document11 pagesPractice For Mounting Buses & Joints-374561a_sengar1No ratings yet
- Orbitol Motor TMTHWDocument20 pagesOrbitol Motor TMTHWRodolfo ErenoNo ratings yet
- Youth Camp Registration Form-2022Document1 pageYouth Camp Registration Form-2022FlerkNo ratings yet
- Kelas ChondrichtyesDocument15 pagesKelas ChondrichtyesanitagustinawatiNo ratings yet
- Principles Involved in Baking 1Document97 pagesPrinciples Involved in Baking 1Milky BoyNo ratings yet
- FactSet London OfficeDocument1 pageFactSet London OfficeDaniyar KaliyevNo ratings yet
- Region 1 - Concreting Works Materials Prices - PHILCON PRICESDocument9 pagesRegion 1 - Concreting Works Materials Prices - PHILCON PRICESMark Gregory RimandoNo ratings yet
- Conceptual Artist in Nigeria UNILAGDocument13 pagesConceptual Artist in Nigeria UNILAGAdelekan FortuneNo ratings yet
- Aquaculture Scoop May IssueDocument20 pagesAquaculture Scoop May IssueAquaculture ScoopNo ratings yet
- Las Tech Drafting 3Q WKDocument13 pagesLas Tech Drafting 3Q WKClemenda TuscanoNo ratings yet
- Goa Daman & Diu Factory Rules PDFDocument141 pagesGoa Daman & Diu Factory Rules PDFmrudang1972100% (1)
- Armadio Presentation-2019Document45 pagesArmadio Presentation-2019Subhash Singh TomarNo ratings yet
- Eco Exercise 3answer Ans 1Document8 pagesEco Exercise 3answer Ans 1Glory PrintingNo ratings yet
- SMAST - 150kW 02190 - 200929091953Document67 pagesSMAST - 150kW 02190 - 200929091953David GarciaNo ratings yet
- Kinder DLL Week 8Document15 pagesKinder DLL Week 8Jainab Pula SaiyadiNo ratings yet
- Ecological Quality RatioDocument24 pagesEcological Quality RatiofoocheehungNo ratings yet
- Rectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Document4 pagesRectifier 5G High Density Embedded Power (3U Power Rack, Three Phase Four Wire) E...Lintas LtiNo ratings yet
- Iso 8033 2016Document9 pagesIso 8033 2016Eric ChuNo ratings yet
- Iec60227-3 (Ed2.1) en DDocument6 pagesIec60227-3 (Ed2.1) en Duntuk donlod aaaNo ratings yet
- EXCEL For Pump DesignDocument2 pagesEXCEL For Pump Designkad-7No ratings yet
- Manuscript FsDocument76 pagesManuscript FsRalph HumpaNo ratings yet
- Qasr Al Sarab Desert Resort Location Map June2012Document1 pageQasr Al Sarab Desert Resort Location Map June2012Anant GârgNo ratings yet
- English2 Q2 Summative Assessment 4 2Document4 pagesEnglish2 Q2 Summative Assessment 4 2ALNIE PANGANIBANNo ratings yet
- The Indian & The SnakeDocument3 pagesThe Indian & The SnakeashvinNo ratings yet
- Javanese PeopleDocument22 pagesJavanese PeopleDenisaNo ratings yet
- Notes Transfer of Thermal EnergyDocument12 pagesNotes Transfer of Thermal Energymahrosh mamoon100% (2)
- 12-Week Off-Season Training Programme Junior Rugby (U18 - U21)Document5 pages12-Week Off-Season Training Programme Junior Rugby (U18 - U21)LeBron JamesNo ratings yet
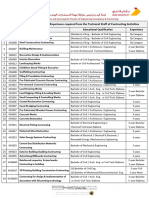
- 5 Contracting Activity and Technical Staff RequirementsDocument2 pages5 Contracting Activity and Technical Staff RequirementsDaniyar KussainovNo ratings yet