Professional Documents
Culture Documents
Rules For Improving Pharmacotherapy in Older Adult Patients - Part 2 (Rules 6-10)
Uploaded by
Aryaldy ZulkarnainiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rules For Improving Pharmacotherapy in Older Adult Patients - Part 2 (Rules 6-10)
Uploaded by
Aryaldy ZulkarnainiCopyright:
Available Formats
See
discussions, stats, and author profiles for this publication at: http://www.researchgate.net/publication/272511766
Rules for Improving Pharmacotherapy in
Older Adult Patients: Part 2 (Rules 6-10).
ARTICLE FEBRUARY 2015
DOI: 10.14423/SMJ.0000000000000243 Source: PubMed
DOWNLOADS
VIEWS
56
51
1 AUTHOR:
James M Wooten
University of Missouri - Kansas City
33 PUBLICATIONS 98 CITATIONS
SEE PROFILE
Available from: James M Wooten
Retrieved on: 23 July 2015
Review Article
Rules for Improving Pharmacotherapy in Older
Adult Patients: Part 2 (Rules 6Y10)
James M. Wooten,
PharmD
Abstract: The population of older adult patients in the United States
is growing each year. Appropriate pharmacotherapy has allowed many
older patients to live longer and maintain healthy lives. Unfortunately,
the inappropriate utilization of medications can be harmful to older
adult patients. Inappropriate pharmacotherapy may lead to overusing
medications and polypharmacy. Polypharmacy can contribute to a higher
incidence of adverse effects, increase the risk of dangerous drug interactions, cause noncompliance with appropriate medication use, and
signicantly increase the cost of health care. The polypharmacy issue
with geriatric patients has been described as an epidemic and this issue
must be addressed. This review provides objective rules that may help
prevent polypharmacy. Consideration of these rules when prescribing,
dispensing, and caring for older adult patients will improve the overall
pharmacotherapy regimens instituted by healthcare providers.
Key Words: Gerontology, pharmacodynamics, pharmacokinetics, pharmacology, pharmacotherapy
n Part 1, which appeared in the February issue, polypharmacy was dened as taking multiple unnecessary medications.1Y4 Because of the variety of medications taken by the
growing older adult population of the United States, as well as
an ever-increasing armamentarium of medications to treat almost all diseases, polypharmacy has become a major healthcare
issue for older patients. Polypharmacy increases the risk of drugrelated adverse effects and harmful drug interactions, reduces
compliance to appropriate pharmacotherapy, and signicantly
increases the level of morbidity and mortality in the geriatric
population.
Rules/guidelines should be established and adhered to by
all healthcare providers so that the polypharmacy epidemic can
be stopped and older adult patients can lead better lives. This
article provides practitioners with specic rules/guidelines that
From the Department of Internal Medicine-Clinical Pharmacology, University
of Missouri-Kansas City School of Medicine; Kansas City.
Reprint requests to Dr James M Wooten, University of Missouri-Kansas City
School of Medicine, 2411 Holmes St, Kansas City, MO 64108.
E-mail: wootenj@umkc.edu
The author has no nancial relationships to disclose and no conicts of interest
to report.
Accepted September 22, 2014.
Copyright * 2015 by The Southern Medical Association
they can use when prescribing medications for their older adult
patients. These rules/guidelines could be printed and posted
where prescribers could easily and readily be reminded of these
important objective concerns. Following these rules greatly
enhances the pharmacotherapy plan for all older patients, prevent potential adverse drug effects, reduce healthcare costs, and
allow patients to lead happier and healthier, productive lives.
Part 2 enumerates the nal ve, rules 6 through 10.
Rule 6: Prescribe and Recommend Only
Those Medications/Drug Classes for Which
You Have a Thorough Understanding
of the Pharmacology
Rule 6 appears obvious, but some medication choices are
better than others. For instance, a patient who is hypertensive
and has systolic heart failure can be treated with an angiotensinconverting enzyme inhibitor, which treats both problems.
Thoroughly assessing the patients medical issues and judiciously prescribing specic medications is an effective way to
approach this rule. Practitioners must realize that if more than
one healthcare provider is managing the patients medication
prole, a consultation with the other providers may be necessary to ensure that the proper pharmacotherapy is prescribed.2,3
Important aspects of a medications pharmacologic prole include the drugs indications for use, mechanism of action, pharmacokinetics, appropriate dosage for most patients,
adverse effects/contraindications; and monitoring parameters.
Because of the extensive number of medications on the market,
it is impossible to know everything about every drug; however,
intimate knowledge of medications commonly prescribed to
older adults can assist practitioners in making safe and effective
pharmacologic decisions for these patients.
Key Points
& Polypharmacy in the geriatric population is an important issue.
& Older adult patients undergo physiologic changes that can
alter a drugs pharmacokinetics and pharmacodynamics.
& Practitioners must take great care when prescribing medications to older adult patients to ensure that every drug prescribed is appropriately assessed and monitored.
0038-4348/0Y2000/108-145
DOI: 10.14423/SMJ.0000000000000257
Southern Medical Journal
& Volume 108, Number 3, March 2015
Copyright 2015 The Southern Medical Association. Unauthorized reproduction of this article is prohibited.
145
Wooten
& Rules for Improving Pharmacotherapy in Elderly Patients
Dosage
Most older adult patients need lower doses of medications
than do other patient populations. This dosing information is
available in some tertiary pharmacotherapy texts (eg, Physicians
Desk Reference) or medical applications for various electronic
devices (Epocrates). The majority of the data were not discovered
during clinical trials. (The Food and Drug Administration does
not mandate that a specic number of older adult subjects be
enrolled in Phase I, II, or III trials before drug approval. Because
older adults have a large number of comorbidities and take many
medications, they are not ideal subjects for trials.5) In general,
postmarketing surveillance is the primary method by which
specic dosing recommendations in older adults is obtained.3Y8
Practitioners should note the following important considerations regarding drug doses in older adults:
& Assess the patients renal function, hepatic function, and nutritional
status (eg, weight, albumin) before any dose is prescribed. Each of
these parameters has a signicant inuence on the precise dosage
for a patient.
& Be aware that changing from one dosage form to another may inuence the bioavailability of the drug, which may affect the dosage.
& Realize that liquid preparations to be delivered via a feeding tube
may interact with various nutrients.
& Understand that controlled-release preparations cannot be crushed,
and the number of doses per day may need to be altered.
& Contact a pharmacist if there is a question regarding a dose or
dosage form.
& Start with lower doses of a drug and titrate to efcacy and tolerability whenever possible.
Adverse Drug Reactions
The older adult population experiences more adverse drug
events (ADEs) than do other patient groups because of the physiologic effects of aging (eg, reduced renal and hepatic function).
One could describe ADEs in older patients as a perfect storm
of issues that come together to make older people extremely
susceptible to ADEs. Because of this, a thorough understanding
of the adverse effect prole of each drug prescribed and the
potential risk involved in using a particular drug in a specic patient are critical. Every drug has associated ADEs. The following
provides suggestions for reducing ADEs in older adults3,4,8Y11:
& Provide proper medication counseling.
& Ensure that the patient receives adequate tutelage in taking medications with exact/complex instructions for use (eg, inhalers, subcutaneous insulin injection).
& Provide written materials or brochures (if available) on the disease(s) being treated and for medications.
& Try to improve patient compliance.
& Use correct dosage based on patients renal and/or hepatic function
and titrate doses up slowly, if possible.
& Know and anticipate the ADEs of all drugs prescribed and monitor
patient (eg, obtain blood levels, international normalized ratio if
patient takes warfarin) for those ADEs.
& Ensure that the pharmacy also counsels the patient.
& Always assess for potential drugYdrug, drugYdisease, drugYfood
interactions and choose drugs/drug classes with reduced interaction risk (see Table 3).
& Train the patients family or caregiver to monitor for ADEs.
146
There are several tools that enumerate the most appropriate
and the least appropriate/most unsafe drugs/drug classes to use
and/or avoid in the geriatric population. The Beers criteria is
a list of medications that details the drugs/drug classes that
have the potential to be dangerous to older adult patients based
on pharmacology (ie, mechanism of action, pharmacokinetics,
ADEs).12 The Beers criteria do not preclude practitioners from
prescribing any of the drugs on the list, but it is an excellent tool
to help guide practitioners in selecting the best and safest medications for their older adult patients.
Similar to, but much more comprehensive than the Beers
criteria, is the STOPP (Screening Tool of Older Persons potentially inappropriate Prescriptions) criteria.13 These criteria were
developed to reduce ADEs in older people with acute illnesses.
STOPP assesses potential adverse drugYdrug interactions and/or
duplicate drug class prescriptions. The STOPP and the Beers
criteria overlap in several areas.
Using various tools can improve the drug selection process
for practitioners prescribing for older adult patients. Whichever
tools are used, there is no substitute for thorough knowledge
regarding the patients history and medical issues.
Rule 7: Identify, Anticipate, and Monitor
Potential Drug Interactions Before They
Become a Problem
It has been estimated that 90% of all individuals 65 years
or older take at least 1 medication per week, 40% use Q5, and
12% use Q10/week. Because of the sheer number of medications that some individuals receive, the risk for drugYdrug
interactions is extremely high. DrugYdrug interactions can be
categorized as either pharmacodynamic or pharmacokinetic
interactions.14,15
Pharmacodynamic Interactions
Pharmacodynamic interactions occur when prescribing
drugs with synergistic actions. These interactions are common
and can occur when a patient has more than one healthcare
provider or the prescriber does not thoroughly understand the
pharmacology of the drugs being prescribed. This can be confusing and dangerous, especially when drugs from completely
different drug classes are prescribed. The presentation in patients
can be insidious as the drugs are added one on top of the other
(drug stacking), until the synergistic effects merge and the
syndrome presents itself; thus, medication reviews by pharmacology experts should be recommended for patients who are
taking several different medications. Two specic examples of
this problem are presented in Table 1.15Y18
Pharmacokinetic Interactions
Because of the physiologic changes associated with aging,
these patients are at greater risk for drugYdrug interactions.
Hepatic metabolism may be signicantly altered for some
drugs. The reasons for various drugYdrug interactions in older
* 2015 Southern Medical Association
Copyright 2015 The Southern Medical Association. Unauthorized reproduction of this article is prohibited.
Review Article
Table 1. Pharmacodynamic drugYdrug interactions
Drug-induced problem/syndrome Drugs/drug classes contributing to problem
Serotonin syndrome
Symptomatology
SSRIs (eg, paroxetine, sertraline, uoxetine)
Spontaneous clonus
Levodopa, carbidopa-levodopa
(indirectly causes release of serotonin)
Inducible clonus and agitation or diaphoresis
SNRIs (eg, desvenlafaxine, duloxetine,
milnacipran, venlafaxine)
Ocular clonus and agitation or diaphoresis
Direct serotonin receptor agonists: tryptans
(eg, sumatriptan, rizatriptan)
Hypertonia
Tremor and hyperreexia
Fentanyl
Temperature above 38-C and ocular clonus
or inducible clonus
Tramadol
Buspirone
Meperidine
Cyclobenzaprine
Cocaine
St Johns wort (hypericum perforatum)
Anticholinergic syndrome
Antihistamines (eg, chlorpheniramine,
cyproheptadine, doxylamine, hydroxyzine,
diphenhydramine, meclizine, promethazine)
Flushing caused by cutaneous vasodilation
(red as a beet)
Anhydrosis (dry as a bone)
Hyperthermia caused by loss of sweat
(hot as a hare)
Blurry vision caused by nonreactive mydriasis
and paralysis of accommodation (blind as a bat)
Agitated delirium (mad as a hatter)
Urinary retention (full as a ask)
Decreased bowel sounds
Tachycardia
SNRIs, serotonin-norepinephrine reuptake inhibitors; SSRIs, selective serotonin reuptake inhibitors.
adult patients include changes in drug absorption and distribution, reduced hepatic clearance and reduced renal function,
polypharmacy, and the high number of comorbidities in these
individuals.15Y18
DrugYdrug interactions cannot always be avoided. Practitioners must be able to anticipate these interactions and create
a monitoring plan to minimize the risk to the patient. Ways
to mitigate these interactions in older adults, beyond those
mentioned earlier in the article, include close monitoring of
drugs with a narrow therapeutic range or index (Table 2) and
Table 2. Common drugs/drug classes with a narrow
therapeutic range
Class
Drug
Anticoagulants
Warfarin
Anticonvulsants
Phenytoin
Antiarrhythmics
Immunosuppressants
Southern Medical Journal
Amiodarone
Cyclosporine
knowledge of the common inducer and inhibitor drugs
(Table 3).14Y18
Another type of interaction prevalent in the geriatric population is drugYdisease interactions, wherein a particular drug
may worsen a specic medical condition (Table 4). Understanding the pharmacologic prole of each drug prescribed to
an older adult patient can reduce the incidence of these types of
interactions.14Y18
Other interaction types occur in older people, including
drugYfood interactions and drugYnutrient interactions. Practitioners must be observant with all drugs prescribed to avoid
these common interaction issues.
Rule 8: Establish a Monitoring Plan for
Each Medication Prescribed for Both
Efcacy and Toxicity
Patient monitoring for a drugs efcacy and toxicity is
critical. Practitioners should address the monitoring plan at the
time a drug is prescribed. A monitoring plan for each medication on the patients prole should be a part of the patients
& Volume 108, Number 3, March 2015
Copyright 2015 The Southern Medical Association. Unauthorized reproduction of this article is prohibited.
147
Wooten
& Rules for Improving Pharmacotherapy in Elderly Patients
Table 3. Common inducer and inhibitor drugs for
cytochrome P450 drugYdrug interactions
Enzyme
Inhibitors
Inducers
CYP1A2
Ciprooxacin, uvoxamine
Phenytoin, rifampin
CYP2C9
Fluconazole
Carbamazepine, rifampin
CYP2D6
Bupropion, uoxetine,
paroxetine
CYP3A
Macrolides (eg, erythromycin,
clarithromycin)
Carbamazepine, modanil,
phenytoin, phenobarbitone,
rifabutin, rifampicin,
St Johns wort
Azole antifungals
(eg, voriconazole, itraconazole,
ketoconazole, uconazole)
and monitor their therapy and take an active role in improving
their health; however, this is challenging for some patients, especially if there are unique barriers that limit effective counseling, such as the following21Y24:
&
&
&
&
&
&
&
&
&
&
Limited cognitive function
Limited education
Literacy issues
Hearing difculties
Vision limitations
Limited nancial resources
Polypharmacy (can complicate medication instruction)
Language barriers
Limited time
Cultural differences
To overcome these barriers, the rst step is identifying which
of them may limit communication and then structuring an effective counseling session with the patient or patients caregiver.
The following provides suggestions to improve communication
with geriatric patients:
Protease inhibitors (eg, indinavir,
ritonavir, saquinavir)
Grapefruit juice
Cimetidine
Ciprooxacin
medical record. Suggestions regarding monitoring include the
following19Y22:
& Understand the pharmacologic prole of every drug prescribed.
& Understand that monitoring for efcacy may be as simple as taking
blood pressure measures (eg, for antihypertensive agents) or as complicated as assessing a chest x-ray for pneumonia (eg, for antibiotics).
& Know which drugs have a narrow therapeutic index; slight changes
in concentration can yield ADEs.
& Know the adverse effect prole for every drug prescribed so that
the patient can be assessed for these effects.
& Double-check doses based on renal or hepatic function using an
appropriate resource. Contact a pharmacist if necessary.
& Individualize doses for each individual patientVone size does not
t all.
Rule 9: Properly Counsel Patients/Caregivers
on All of the Patients Medications and
Ensure That the Patient Understands the
Pharmacotherapy Plan
Effective patient counseling and instruction is an important part of the healthcare plan. Patients who are informed and
understand their own healthcare issues will be able to assess
& Counsel the patient/caregiver in a quiet, well-lighted environment
where the patient/caregiver is comfortable.
& Do not rush.
& Attempt to identify any barriers that may exist with the patient that
will limit communication. Try to correct the issues that are identied (eg, if patient has limited hearing, provide written materials).
& Provide patient/caregiver with an up-to-date medication list and
make sure all parties have the same list.
& Assess language barriers and use interpreters if necessary.
& Use language that is appropriate for patients educational background.
& Use written instruction aides whenever possible.
& Identify and correct any cultural barriers that may exist.
& Identify potential nancial difculties that may limit compliance.
& Maintain a positive attitude and try to motivate the patient to take
an active role.
& Be respectful and refer to patient in an appropriate way (eg, Mrs
Lopez, rather than Fulgenica or Dear).
& Do not be judgmental.
& Use any teaching aides that are available.
& Answer all of the patients/caregivers/familys questions. If certain
questions cannot be answered, then help them nd someone who
can answer the questions.
& Ask the patient to repeat instructions.
& Ensure that the patient knows the possible limitations of treatment
(eg, adverse effects, potential interactions).
& Instruct patient about over-the-counter medications, vitamins, nutritionals, and herbal therapies.
Table 4. DrugYdisease state interactions
Drug/drug class
A-Adrenergic antagonists (eg, propranolol,
metoprolol, carvedilol)
Disease state
Pharmacologic interaction
Asthma/COPD
Blocking the A-2 receptors in the lungs may induce bronchoconstriction,
which may worsen asthma or COPD
Aminoglycosides (eg, gentamicin, tobramycin)
Chronic kidney disease
Aminoglycosides are nephrotoxic and may worsen renal function
NSAIDs (eg, ibuprofen, naproxen)
Nondihydropyridine calcium-channel blockers
(eg, verapamil, diltiazem)
Peptic ulcer disease
Congestive heart failure
NSAIDs can cause peptic ulcers
Verapamil or diltiazem can reduce the inotropic action of the heart
COPD, chronic obstructive pulmonary disease; NSAIDs, nonsteroidal anti-inammatory drugs.
148
* 2015 Southern Medical Association
Copyright 2015 The Southern Medical Association. Unauthorized reproduction of this article is prohibited.
Review Article
The practitioner must ensure that the patient/caregiver
clearly understands that all pharmacotherapy treatment will be
monitored for both efcacy and potential toxicity (include in
the medication list if possible). Objective and specic goals for
the treatment regimens should be set, and the patient/caregiver
should understand the goals and objectives of pharmacotherapy. Ensure that patient clearly understands the plan if a specic
treatment is not successful or proves to be harmful. Follow-up
appointments should be arranged and reminders (eg, telephone
calls, e-mails, texts) provided. Compliance should be assessed
at every visit. All questions should be answered to the patients
satisfaction.21Y24
Rule 10: Assess and Address
Compliance Issues
Compliance can be a major problem in providing effective
health care to older adult patients. There are several reasons for
their poor compliance, including the following25Y29:
& Lack of appropriate discharge planning
& Adverse effects of medication
& Lack of trust in the healthcare provider(s) and/or the treatment plan
&
&
&
&
&
&
&
Poor understanding of illness(es)
Poor patientYprovider relationship
Complexity of treatment regimen
Financial difculties
Cognitive issues (eg, Alzheimer disease)
Psychological problems (eg, psychosis, depression)
Polypharmacy
Compliance should be addressed with the patient/caregiver at the time each drug is prescribed (Table 5).
Conclusions
This article and its predecessor present 10 rules for improving pharmacotherapy in older adults. Rules like these are
necessary because older patients use a higher percentage of
medications than other patient populations and they are extremely vulnerable to drug-related issues that could cause great
harm. Practitioners must be cognizant of the challenges that are
encountered when prescribing drugs to older patients, and
these rules provide a constant reminder to promote safe and
effective pharmacotherapy. These rules help ensure that patients
are aware that their healthcare providers are considering and
implementing the most appropriate pharmacology plan that ts
Table 5. Potential compliance barriers and strategies to improve compliance
Barriers
Strategies
Patient-related issues
Forgetting to take medication
Use pill boxes, medication calendars, smartphone apps
Difculty taking so many medications
Structure times to take medications around daily activities (eg, meals)
Lack of understanding of disease
Reduce number of medications, if possible; address polypharmacy issue
Denial
Ensure patient understands disease being treated and why
Low expectations
Set specic goals for patient (eg, blood pressure goals, blood sugar goals)
Depression
Physical barriers
Find devices to patient overcome physical barriers to compliance (eg, special inhaler)
Sort out nancial barriers and attempt to help patient in whatever way possible
Financial difculties
Use translator
Language literacy issues
Ask patient to write down all questions
Medication-related issues
Complex pharmacotherapy regimen
Review pharmacotherapy plan at each visit
Adverse effects
Check patients medication list and make sure it is appropriate
Change to drug with fewer/different adverse effect prole, if possible
Assess all medication adverse effects
Reduce polypharmacy as much as possible
Discontinue medications that are not useful to patients current regimen
Prescriber-related issues
Prescriber does not explain treatment plan
Use multidisciplinary team to help care for patient
Prescriber does not take time with patient/patients family
Provide verbal and written instructions
Prescriber does not listen to patient
Prescriber provides information that patient/patients family
does not understand
Use training aides
Ensure that patient/caregiver has easy access to provider so that questions are answered
Prescriber will not answer questions
Prescriber does not follow-up with patient/family
Southern Medical Journal
Encourage patient to write down all questions
Ensure that patients medication list is identical to practitioners list
& Volume 108, Number 3, March 2015
Copyright 2015 The Southern Medical Association. Unauthorized reproduction of this article is prohibited.
149
Wooten
& Rules for Improving Pharmacotherapy in Elderly Patients
with their age, comorbidities, and other treatment regimens.
Practitioners should avoid the seven deadly sins of prescribing29:
1. A drug is prescribed to treat a disease or ailment that is actually
caused by an adverse reaction to another drug. Example: Prescribing a drug for a patient who has constipation caused by
overprescribing drugs with anticholinergic properties.
2. A drug is prescribed to treat a problem that should be treated
initially with nonpharmacologic therapy. Example: Prescribing
a sedative for insomnia to a patient who regularly ingests caffeinated products right before bedtime.
3. Attempt to treat a medical problem that may be either self-limited
or unresponsive to pharmacologic treatment. Example: Prescribing
an antibiotic to a patient who has a viral infection.
4. A drug is prescribed for a problem, but instead of the safest, most
effective treatment, the healthcare provider recommends an agent
that is inappropriate for a geriatric patient. Example: Prescribing
diazepam (long-acting benzodiazepine on the Beers list) as a sedative when a mild sedative (trazodone) would be more appropriate.
5. Two drugs are prescribed appropriately, but they interact to cause
serious injury or death, and there was no monitoring plan in place
for the interaction. Example: Prescribing warfarin (for deep vein
thrombosis) along with trimethoprim/sulfamethoxazole (for urinary tract infection). This combination slows the metabolism of
warfarin, which leads to over-anticoagulation and possibly a severe
bleeding episode.
6. Two or more drugs in the same drug class are used to treat separate
problems. The drugs do not improve efcacy, but rather have
additive effects that could harm the patient. Example: Prescribing
a beta-blocker (carvedilol) to slow heart rate, but the patient is
already taking propranolol (prescribed by psychiatrist) to treat
anxiety; this in turn leads to profound bradycardia.
7. The correct drug is selected to treat a problem, but the dosage is
much too high for the patient. Example: Prescribing levooxacin
750 mg/day to treat a urinary tract infection in a patient with renal
insufciency. This occurs often in older adults; typical dosages
are prescribed when older adults should be receiving a lower dose
because of reduced renal or hepatic function.
References
1. Antimisiaris DE. Polypharmacy: a modern day silent epidemic. http://
www.polypharmacyinitiative.com/education.html. Accessed August 4, 2014.
2. Wooten JM. Rules for improving pharmacotherapy in older adult patients:
part 1 (rules 1Y5). South Med J 2015;108:97Y104.
3. Wooten JM. Pharmacotherapy considerations in elderly adults. South
Med J 2012;105:437Y445.
4. Wooten J, Galavis J. Polypharmacy. Keeping the elderly safe. RN 2005;
68:44Y50.
5. Food and Drug Administration. Postmarketing surveillance programs.
http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/
Surveillance/ucm090385.htm. Published August 19, 2014. Accessed
February 18, 2015.
6. Bressler R, Bahl JJ. Principles of drug therapy for the elderly patient. Mayo
Clin Proc 2003;78:1564Y1577.
7. Sieck GC. Physiology of aging. J Appl Physiol (1985) 2003;95:1333Y1334.
8. Seward JB. Physiological aging: window of opportunity. J Am Coll Cardiol
2011;4:243Y245.
150
9. Kim J, Mak M. Geriatric drug use. In: Koda-Kimble MR, Young LY,
Alldredge BK, et al. (eds): Applied Therapeutics: The Clinical Use of Drugs
9th ed. Philadelphia, Lippincott Williams & Wilkins, 2009:99-1Y99-20.
10. Starner CI, Gray SL, et al. Geriatrics. In: DiPiro JT, Talbert RL, Yee GC, et al.
(eds): Pharmacotherapy: A Pathophysiologic Approach. 7th ed. New York,
McGraw-Hill, 2011:57Y66.
11. Pham CB, Dickman RL. Minimizing adverse drug events in older patients.
Am Fam Physician 2007;76:1837Y1844.
12. American Geriatrics Society 2012 Beers Criteria Update Expert Panel.
American Geriatrics Society updated Beers criteria for potentially
inappropriate medication use in older adults. J Am Geriatr Soc 2012;
60:616Y631.
13. Hamilton H, Gallagher P, Ryan C, et al. Potentially inappropriate
medications dened by STOPP criteria and the risk of adverse drug events
in older hospitalized patients. Arch Intern Med 2011;171:1013Y1019.
14. Fanciullo GJ, Washington T. Best practices to reduce the risk of drug-drug
interactions: opportunities for managed care. Am J Manag Care 2011;
17(Suppl 11):S299YS304.
15. Priddle M. Drug-related problems in the elderly. Pharmawise 2011;6:2.
16. Mallet L, Spinewine A, Huang A. The challenge of managing drug
interactions in elderly people. Lancet 2007;370:185Y191.
17. Raich C, Abate M, Dunsworth T. Drug interactions. http://www.wvu.edu/~exten/
infores/pubs/fypubs/wlg410.pdf. Published 1997. Accessed May 23, 2014.
18. Snyder BD, Polasek TM, Doogue MP. Drug interactions: principles and
practice. http://www.australianprescriber.com/magazine/35/3/85/8. Published
2012. Accessed February 18, 2015.
19. Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in
older adults: toward a better understanding of physiology and etiology:
summary from the American Geriatrics Society/National Institute on Aging
Research Conference on Frailty in Older Adults. J Am Geriatr Soc 2006;
54:991Y1001.
20. Fogel RW. Changes in the Physiology of Aging During the Twentieth
Century NBER work paper series 11233. Cambridge, MA, National
Bureau of Economic Research, 2005.
21. Pfaff H, Driller E, Ernsmann N, et al. Standardization through individualization in care for the elderly: proactive behavior through individualized standardization. Open Longev Sci 2010;4:51Y57.
22. Jose J. Promoting drug safety in elderlyVneeds a proactive approach.
Indian J Med Res 2012;136:362Y364.
23. Robinson TE, White GL, Houchins JC. Improving communication with
older patients: tips from the literature. Fam Pract Manag 2006;13:73Y78.
24. Wolfe SM, ed. Misprescribing and overprescribing of drugs. http://
www.citizen.org/documents/HL_201004.pdf. Published April 2010.
Accessed February 18, 2015.
25. Kaye M. Mandating of electronic prescriptions for Medicare patients. http//
:www.ojni.org/12_2/kaye.html. Published June 2008. Accessed May 23, 2014.
26. American Society of Consultant Pharmacists. Adult MEDucation. Improving
medication adherence in older adults. http://www.adultmeducation.com/
downloads/Adult_Meducation.pdf. Published 2006. Accessed May 24, 2014.
27. Wick JY. Adherence issues in elderly patients. http://www.pharmacytimes.com/
publications/issue/2011/January2011/RxFocus-0111. Published January 13,
2011. Accessed May 24, 2014.
28. Kocurek B. Promoting medication adherence in older adults . . . and the rest of
us. Diabetes Spectrum 2009;22:80Y84.
29. Wolfe SM, Sasich LO, Lurie P. Worst Pills, Best Pills: A Consumers Guide to
Avoiding Drug-Induced Death or Illness New York, Simon & Schuster, 2005.
* 2015 Southern Medical Association
Copyright 2015 The Southern Medical Association. Unauthorized reproduction of this article is prohibited.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Marijuana Grow Basics - Jorge CervantesDocument389 pagesMarijuana Grow Basics - Jorge CervantesHugo Herrera100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Wsi PSDDocument18 pagesWsi PSDДрагиша Небитни ТрифуновићNo ratings yet
- Rubric - Argumentative EssayDocument2 pagesRubric - Argumentative EssayBobNo ratings yet
- Global 6000 SystemsDocument157 pagesGlobal 6000 SystemsJosé Rezende100% (1)
- Homo Sapiens ActivityDocument8 pagesHomo Sapiens ActivityJhon Leamarch BaliguatNo ratings yet
- Atypical Manifestations of Medical Conditions PDFDocument8 pagesAtypical Manifestations of Medical Conditions PDFAryaldy ZulkarnainiNo ratings yet
- Electronic Harassment Strahlenfolter - A Short History of Sound Weapons Pt2 - InfrasoundDocument10 pagesElectronic Harassment Strahlenfolter - A Short History of Sound Weapons Pt2 - InfrasoundFrank-BoenischNo ratings yet
- IEC-60721-3-3-2019 (Enviromental Conditions)Document12 pagesIEC-60721-3-3-2019 (Enviromental Conditions)Electrical DistributionNo ratings yet
- The Rich Hues of Purple Murex DyeDocument44 pagesThe Rich Hues of Purple Murex DyeYiğit KılıçNo ratings yet
- Module 4-Answer KeyDocument100 pagesModule 4-Answer KeyAna Marie Suganob82% (22)
- Riedijk - Architecture As A CraftDocument223 pagesRiedijk - Architecture As A CraftHannah WesselsNo ratings yet
- 1 Ajg2010409aDocument7 pages1 Ajg2010409aAryaldy ZulkarnainiNo ratings yet
- Srwa Paper Ok Final - Jurnal Kba FlavonoidDocument12 pagesSrwa Paper Ok Final - Jurnal Kba FlavonoidAryaldy ZulkarnainiNo ratings yet
- Journal of Psychosomatic ResearchDocument6 pagesJournal of Psychosomatic ResearchAryaldy ZulkarnainiNo ratings yet
- Association of Infection With Hepatic Encephalopathy Risk: A Systematic ReviewDocument7 pagesAssociation of Infection With Hepatic Encephalopathy Risk: A Systematic ReviewAryaldy ZulkarnainiNo ratings yet
- 1 s2.0 S0022399914000543 MainDocument11 pages1 s2.0 S0022399914000543 MainAryaldy ZulkarnainiNo ratings yet
- Eur J Intern Med 2011 p597Document6 pagesEur J Intern Med 2011 p597Aryaldy ZulkarnainiNo ratings yet
- Experimental GerontologyDocument8 pagesExperimental GerontologyAryaldy ZulkarnainiNo ratings yet
- 1 s2.0 S0531556515000601 MainDocument9 pages1 s2.0 S0531556515000601 MainAryaldy ZulkarnainiNo ratings yet
- Eur J Clin Pharmacol 2014 p437Document8 pagesEur J Clin Pharmacol 2014 p437Aryaldy ZulkarnainiNo ratings yet
- 2nd Journal ReadingDocument27 pages2nd Journal ReadingAryaldy ZulkarnainiNo ratings yet
- Polypharmacy Optimizing Medication Use in Elderly PatientsDocument7 pagesPolypharmacy Optimizing Medication Use in Elderly PatientsAryaldy ZulkarnainiNo ratings yet
- J Clin Gerontol Geriatr 2015 p30Document4 pagesJ Clin Gerontol Geriatr 2015 p30Aryaldy ZulkarnainiNo ratings yet
- Drugs Aging 2014 p131Document11 pagesDrugs Aging 2014 p131Aryaldy ZulkarnainiNo ratings yet
- Effect of Fenofibrate On Amputation Events in PeopleDocument46 pagesEffect of Fenofibrate On Amputation Events in PeopleAryaldy ZulkarnainiNo ratings yet
- 2nd Journal ReadingDocument27 pages2nd Journal ReadingAryaldy ZulkarnainiNo ratings yet
- 2nd Journal ReadingDocument27 pages2nd Journal ReadingAryaldy ZulkarnainiNo ratings yet
- Disclosing A Diagnosis of Dementia PDFDocument5 pagesDisclosing A Diagnosis of Dementia PDFAryaldy ZulkarnainiNo ratings yet
- Assessing Eyes NCM 103 ChecklistDocument7 pagesAssessing Eyes NCM 103 ChecklistNicole NipasNo ratings yet
- All MeterialsDocument236 pagesAll MeterialsTamzid AhmedNo ratings yet
- CH - 3Document3 pagesCH - 3Phantom GamingNo ratings yet
- Arduino Nano based K1EL Winkeyer compatible CW contest keyerDocument35 pagesArduino Nano based K1EL Winkeyer compatible CW contest keyerSreejith SreedharanNo ratings yet
- PGP TutorialDocument21 pagesPGP TutorialSabri AllaniNo ratings yet
- Plant Air Centrifugal Compressors: Turbo-Air Series Featuring Oil-Free AirDocument20 pagesPlant Air Centrifugal Compressors: Turbo-Air Series Featuring Oil-Free AirSharad KokateNo ratings yet
- Fisher FIELDVUE DVC2000 Digital Valve Controller: Instruction ManualDocument108 pagesFisher FIELDVUE DVC2000 Digital Valve Controller: Instruction ManualsrinuvoodiNo ratings yet
- Daughters of The Storm by Kim Wilkins - Chapter SamplerDocument32 pagesDaughters of The Storm by Kim Wilkins - Chapter SamplerHarlequinAustraliaNo ratings yet
- Merchandise Floor Ready Standards - Supplier InformationDocument46 pagesMerchandise Floor Ready Standards - Supplier InformationGarmentLearner100% (1)
- Conserve O Gram: Understanding Histograms For Digital PhotographyDocument4 pagesConserve O Gram: Understanding Histograms For Digital PhotographyErden SizgekNo ratings yet
- RestrukturisasiDocument17 pagesRestrukturisasimuhammad hayel wallaNo ratings yet
- Ogl422 Milestone Three Team 11 Intro Training Session For Evergreen MGT Audion Recording Due 2022apr18 8 30 PM PST 11 30pm EstDocument14 pagesOgl422 Milestone Three Team 11 Intro Training Session For Evergreen MGT Audion Recording Due 2022apr18 8 30 PM PST 11 30pm Estapi-624721629No ratings yet
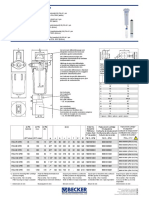
- Medical filter performance specificationsDocument1 pageMedical filter performance specificationsPT.Intidaya Dinamika SejatiNo ratings yet
- Assignment 3 Part 3 PDFDocument6 pagesAssignment 3 Part 3 PDFStudent555No ratings yet
- Operation Guide For The Mercedes-Benz GLA/CLADocument5 pagesOperation Guide For The Mercedes-Benz GLA/CLASantosh TalankarNo ratings yet
- Brooks Instrument FlowmeterDocument8 pagesBrooks Instrument FlowmeterRicardo VillalongaNo ratings yet
- Tutorial 3Document2 pagesTutorial 3prasoon jhaNo ratings yet
- EG-45-105 Material Information Sheet (Textura) V2Document4 pagesEG-45-105 Material Information Sheet (Textura) V2GPRNo ratings yet
- Introduction To Streering Gear SystemDocument1 pageIntroduction To Streering Gear SystemNorman prattNo ratings yet
- Chemical Cleaning Products Are Destroying The Ecosystem and Your Septic Tank - Organica BiotechDocument14 pagesChemical Cleaning Products Are Destroying The Ecosystem and Your Septic Tank - Organica BiotechKrispin FongNo ratings yet