Professional Documents
Culture Documents
Chapter 1: Introduction To Psychiatric Nursing
Uploaded by
WarrenPeaceOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 1: Introduction To Psychiatric Nursing
Uploaded by
WarrenPeaceCopyright:
Available Formats
Keltner: Psychiatric Nursing, 5th Edition
Chapter 1: Introduction to Psychiatric Nursing
Chapter Focus
The human cost of psychiatric health care is great when one considers that mental and
addictive disorders affect more than 25% of Americans 18 years of age or older annually.
Consequently, psychiatric nurses provide some of the most important services in health
care today.
Four major benchmarks have contributed to the evolution of modern psychiatric care:
1. The Period of Enlightenment. This was initiated by the institution of humane care
advanced by Phillippe Pinel and William Tuke in 1793, which ultimately led to the
asylum (sanctuary) movement and, under the influence of Dorothea Dix, the
development of the state hospital system in the United States. It was during this
period that psychiatric nursing had its origins. Within 100 years of the origin of the
asylum movement, the hospitals created had evolved from places of refuge to places
of torment as the ideals of the reformers were lost on a new generation of caretakers.
2. The Period of Scientific Study. This was initiated by the work of Sigmund Freud,
Emil Kraepelin, Eugen Bleuler, and others who sought to understand the mind and
mental illness and who shifted the focus of care from sanctuary to treatment.
Therapies such as psychoanalysis, psychotherapy, and psychosurgery were developed
during this era. A classification of mental illness was developed.
3. The Period of Psychotropic Drugs. In the 1950s, this initiated a radical shift in the
care and treatment of mental illness. Patients who had seemed beyond help became
calmed and accessible. Dramatic cures took place. Hospital stays shortened, the
number of patients confined for long-term institutional care declined, and the
availability of community-based treatment increased.
4. The Period of Community Mental Health. This movement emerged from the
interaction of multiple dynamic forces, culminating in the enactment of federal
legislation that shifted funding from institutional care to extrainstitutional care (the
Community Mental Health Centers [CMHC] Act) and provided income for the
mentally disabled (currently, Supplemental Security Income [SSI] and Social Security
Disability Insurance [SSDI]). These shifts in funding, plus changes in commitment
laws that made involuntary commitment difficult, resulted in a rapid and dramatic
reduction of the state hospital population and the closure of many state hospitals.
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc. All rights reserved.
Instructor's Manual
1-2
The advances and changes in psychiatric care have had far-reaching effects. Most
notably, mental health has become a concern for all. Social and emotional problems have
become a legitimate focus for mental health care professionals. New challenges in
psychiatric care have arisen: recidivism (reflected in increased admission rates), growing
demands on general hospital emergency departments for crisis intervention and acute
outpatient treatment, expansion of the need for psychiatric services by general hospital
inpatient psychiatric facilities and community agencies, and an increased complexity of
problems presented by psychiatric patients (e.g., assaultiveness, homelessness, and
substance abuse).
Parallel to developments in psychiatric treatment, the practice of psychiatric nursing has
evolved from custodial care in the late nineteenth century to interdisciplinary
collaboration in the treatment of the mentally ill, from dependent caregiver to
independent practitioner, and from exclusive focus on the needs of psychotic individuals
to the inclusion of the social and emotional needs of the worried well who are
experiencing situational reactions. Through the influence of leaders such as Hildegarde
Peplau, psychiatric nursing has gained direction, recognition, and professional
accountability, and psychiatric nursing education has advanced. Psychiatric nurses will
increasingly have a major role in resolving problems in mental health care and in
developing a seamless continuum of care designed to meet the needs of the mentally ill.
Key Terms
asylum
community mental health
continuum of care
deinstitutionalization
homelessness
psychotropic drugs
Learning Objectives
After reading this chapter, you should be able to:
1. Describe the enormity of mental health concerns in both human and financial
contexts.
2. Explain the history of psychiatry as a foundation for current psychiatric nursing
practice.
3. Identify the significant changes that occurred during the Period of the Enlightenment.
4. Relate the contributions of early scientists to the current understanding of mental
illness.
5. Explain the impact of psychotropic drugs on psychiatric care.
6. Analyze the immediate and long-term effects of the community mental health
movement.
7. Describe the impact of the Decade of the Brain on psychiatric care.
8. Identify the specific strengths that enable psychiatric nurses to become effective in
the new continuum of care.
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc. All rights reserved.
Instructor's Manual
Chapter Outline
Benchmarks in Psychiatric
History
Benchmark I: Period of
Enlightenment
1-3
Teaching Strategies
Pre-Enlightenment: ABCsassistance, banishment, and
confinement
Important figures:
Tuke: an English Quaker who started York Retreat
Pinel: a Frenchman responsible for unchaining the
mentally ill
Asylum
Two meanings: protection, sanctuary; a place of
maltreatment, hopelessness, and abuse
Dorothea Dix: developed concept of asylum in United States,
resulting in beginning of state hospital system
Benchmark II: Period of
Major scientists who emerged had an unquenchable curiosity
Scientific Study
about the mind and human behavior:
Sigmund Freud (18561939): introduced psychoanalysis
Emil Kraepelin (18561926): made detailed
observations and descriptions of mentally ill patients
Eugen Bleuler (18571939): coined term schizophrenia
Benchmark III: Period of Approximate beginning: 1950s
Psychotropic Drugs
Chlorpromazine (Thorazine): first antipsychotic
Imipramine (Tofranil): first tricyclic antidepressant (~1958)
Lithium: introduced in late 1940s but not used in the United
States until ~1970
Benchmark IV: Period of Convergence of forces led to mental health legislation:
Community Mental Health Publics declining confidence in state hospital system
Failure of various treatment approaches
Progressive legislative climate
Faith in psychotropic drugs
Negative effect: confusion about the boundaries of mental
illness
Deinstitutionalization
Depopulation of State Hospitals began in 1955, but
deinstitutionalization movement was fostered by CMHC Act
of 1963 and federal legislation that provided mentally
disabled persons with an income while living in the
community (SSI and SSDI).
Shifting the Cost of Mental State governments found that using federal monies
Illness
supplemented by state funds to provide aid to disabled
mentally ill individuals resulted in huge cost savings.
Commitment laws underwent change out of new concern for
individual civil rights. It became more difficult to effect
involuntary commitment to a state hospital.
Depopulation of State
Peak population (1955): 558,922 patients
Hospitals
Current population: 70,000
Many state hospitals have closed. Former patients live in
nursing homes, prisons, homes with families, groups of
similarly affected individuals, boarding homes, or on their
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc. All rights reserved.
Instructor's Manual
Community Effects
Benchmark V: Decade of
the Brain
1-4
own.
Hospitalized patients require a high level of care, have few
social relationships, are psychotic and are typically acutely ill
young men.
Emergency department use is increased.
General hospital psychiatric units are overwhelmed.
Todays patients are seen to be more aggressive.
During the 1990s, an increase in brain research studies
coincided with increased interest in biologic explanations for
mental disorders.
The Diagnostic and Statistical Manual of Mental Disorders
was revised.
Public awareness of mental disorders grew.
Nursing textbooks began to provide more detailed
information about psychobiology and psychopharmacology.
Issues That Affect the
Delivery of Psychiatric Care
Paradigm Shift in
As interest in psychotherapy and disinterest in severely
Psychiatric Care
mentally ill patients grew during the 1930s and 1940s, public
mental hospitals lost prestige, as did those who worked in
them. Psychiatry changed focus from the severely mentally ill
to the worried well. However, in 1980, publication of the
DSM-III returned the focus to individuals with psychiatric
disorders.
Homelessness
This problem is linked to deinstitutionalization.
About 800,000 are homeless each night, including families
with children and individuals employed in low-paying jobs,
who have been displaced by social policies over which they
have no control. Living arrangements include community
shelters, halfway houses, board-and-care homes, cheap hotels,
rehabilitation programs, prisons, and jails.
As many as 20% to 25% of the homeless have a severe
mental illness.
As many as 50% to 75% of the homeless suffer from alcohol
or drug abuse, many from both.
Community-Based Care
The future of psychiatric care and psychiatric nursing will be
linked to efforts to prevent mental health problems and treat
existing disorders more effectively. Based on economic
reality, much of that effort will be community based as part of
a continuum of care.
Developing a Continuum of Factors leading to unmet needs of SMI:
Care
Liberalization of commitment laws, allowing SMI patients
to go untreated
Restrictive confidentiality rulings to meet needs of SMI
Develop a seamless continuum of care to:
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc. All rights reserved.
Instructor's Manual
Role for Nursing in the
Continuum of Care
The Diagnostic Bible of
Psychiatry
Psychiatric Nursing
Education: Three Firsts
First Psychiatric Nurse
First Psychiatric Nursing
Textbook
First Psychiatric Nursing
Theorist
1-5
coordinate activities of diverse treatment sources.
facilitate movement between and among continuum
entities.
Develop a new conceptualization of system:
Focus more on recovery and reintegration, less on
symptom stabilization
Involve consumers and family members more
Focus on holistic thinking (stabilizing housing, medical
health, finances) rather than on medication management.
CMH role defined in 1982 by ANA: nurse participates with
other members of community in assessing, planning,
implementing, and evaluating mental health services and
community services. These include promotion of continuum
of primary, secondary, and tertiary prevention of mental
illness
Nursing values that fit with concept of a care continuum:
Holistic view of patient
Working with families
Treating patients in own home
Developing relationships over time
Educating patients
Assessing environment for safety, hygiene, and supports
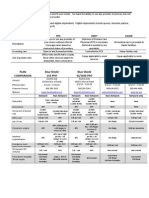
The current manual, DSM-IV-TR provides five axes to use in
patient assessment:
Axis I: clinical disorders
Axis II: personality or developmental disorders
Axis III: general medical conditions that relate to axes 1
and II or have a bearing on treatment
Axis IV: severity of psychosocial stressors
Axis V: global assessment of functioning (scale of 0 to
100)
Linda Richards: first American psychiatric nurse; active in
developing nursing care in psychiatric hospitals; directed a
school of psychiatric nursing ~1880
Written by Harriet Bailey in 1920
1937: NLN recommended that psychiatric nursing become
part of general nursing curriculum
Hildegarde Peplau: developed model for psychiatric nursing;
wrote Interpersonal Relations in Nursing in 1952;
emphasized the interpersonal dimension of practice
Copyright 2007 by Mosby, Inc., an affiliate of Elsevier Inc. All rights reserved.
You might also like
- 1.disagreement With Exiting Mental Health Concepts, Activities and RolesDocument3 pages1.disagreement With Exiting Mental Health Concepts, Activities and RolesAnanya100% (1)
- 1960 To PresentDocument24 pages1960 To PresentpsicandreiaNo ratings yet
- Lecture Notes For Mental Health Nursing Psych NursingDocument88 pagesLecture Notes For Mental Health Nursing Psych Nursingjg369097100% (1)
- Ava Paravati Paradigm Shift PaperDocument15 pagesAva Paravati Paradigm Shift Paperapi-607803514No ratings yet
- Developing Counseling Skills For HealthcareDocument165 pagesDeveloping Counseling Skills For HealthcareHemn HawleryNo ratings yet
- 9 Ohio ST JCrim L53Document37 pages9 Ohio ST JCrim L53manakvariamNo ratings yet
- CHAPTER-1-foundation-of-Psych-Mental-Health-Nsg (1)Document5 pagesCHAPTER-1-foundation-of-Psych-Mental-Health-Nsg (1)Mark dave Francois A. GacutanNo ratings yet
- Mental Health History in U.S.Document3 pagesMental Health History in U.S.lazylawatudentNo ratings yet
- Definitions of Mental IllnessDocument2 pagesDefinitions of Mental Illnessgivemore hoveNo ratings yet
- Assignment #01 Submitted To: Engr. Abdul Hanan Taqi Subject: Psychology (HU-240)Document6 pagesAssignment #01 Submitted To: Engr. Abdul Hanan Taqi Subject: Psychology (HU-240)Shujat AliNo ratings yet
- The Mistreatment of The Mentally Ill in Developing CountriesDocument37 pagesThe Mistreatment of The Mentally Ill in Developing Countriesapi-289502576No ratings yet
- Mental Health Nursing Psych NursingDocument42 pagesMental Health Nursing Psych NursingBheru Lal75% (4)
- PUBH1382 Week 6 2017 - NotesDocument9 pagesPUBH1382 Week 6 2017 - NotesCarleta StanNo ratings yet
- Development of Community PsychologyDocument10 pagesDevelopment of Community PsychologyxyzNo ratings yet
- NCM 105 - Lecture Format in MSWordDocument7 pagesNCM 105 - Lecture Format in MSWordMocking Dawn EvangelistaNo ratings yet
- America's Mental Health Crisis Solution Exists in Community Care ModelDocument6 pagesAmerica's Mental Health Crisis Solution Exists in Community Care ModelTram Do QuynhNo ratings yet
- Paradigm Shift Final DraftDocument11 pagesParadigm Shift Final Draftapi-609632187No ratings yet
- Deinstitutionalization 2Document9 pagesDeinstitutionalization 2api-297149827No ratings yet
- Evolution of Mental Health CareDocument78 pagesEvolution of Mental Health CareAttaullah khan100% (1)
- The Earliest Years: 1. Research On The History or Evolution of Mental Health-Psychiatric Nursing (10 Points)Document3 pagesThe Earliest Years: 1. Research On The History or Evolution of Mental Health-Psychiatric Nursing (10 Points)Kristian Karl Bautista Kiw-isNo ratings yet
- 492 Final RecommendationDocument9 pages492 Final Recommendationapi-405318047No ratings yet
- SSRN Id157834Document100 pagesSSRN Id157834Chirantan KashyapNo ratings yet
- Family Mental Health NursingDocument21 pagesFamily Mental Health Nursinghyunra kimNo ratings yet
- Unit 2 - Mental Health and IllnessDocument12 pagesUnit 2 - Mental Health and IllnessJill MehtaNo ratings yet
- Minoletti Et Al - 20 Yrs MH Policy in Chile - IJMH 2012Document18 pagesMinoletti Et Al - 20 Yrs MH Policy in Chile - IJMH 2012ClaudiaGárateHenríquezNo ratings yet
- Psychiatric and Mental Health NursingDocument10 pagesPsychiatric and Mental Health NursingGlaiza Claire Am-amlan OlayanNo ratings yet
- Defining Abnormal BehaviorDocument3 pagesDefining Abnormal BehaviorJay Sam GarciaNo ratings yet
- Mental Health StudyDocument4 pagesMental Health StudyKrishna SapkotaNo ratings yet
- Running Head: Serious Mental Illness in The Correction System 1Document11 pagesRunning Head: Serious Mental Illness in The Correction System 1api-247059278No ratings yet
- HSS2121 Week 11 Guest Lecture - Mental Illness FinalDocument42 pagesHSS2121 Week 11 Guest Lecture - Mental Illness FinalChiheb DzNo ratings yet
- Mental Health IndustryDocument11 pagesMental Health Industryjordan gallowayNo ratings yet
- Brief History of Mental IllnessDocument41 pagesBrief History of Mental Illnessmamta sahuNo ratings yet
- Abnormal PsychologyDocument9 pagesAbnormal PsychologyHomo CyberneticusNo ratings yet
- Community Mental Health Services in Latin America For People With Severe Mental DisordersDocument23 pagesCommunity Mental Health Services in Latin America For People With Severe Mental DisordersGloria ThomasNo ratings yet
- Mental health guidelines promote oral careDocument21 pagesMental health guidelines promote oral careKathrinaRodriguezNo ratings yet
- Adaptive Patterns of Behavior Care of Clients With Maladaptive Patterns of BehaviorDocument14 pagesAdaptive Patterns of Behavior Care of Clients With Maladaptive Patterns of BehaviorAngel CauilanNo ratings yet
- Psychiatric and Mental Health Nursing - Wikipedia PDFDocument83 pagesPsychiatric and Mental Health Nursing - Wikipedia PDFJanani AmmuNo ratings yet
- Psychology Assessment - I - M1Document42 pagesPsychology Assessment - I - M1Brinda ChughNo ratings yet
- No Room at The Inn-2012Document28 pagesNo Room at The Inn-2012Treatment Advocacy CenterNo ratings yet
- Deinstitutionalization and Crime LevelsDocument28 pagesDeinstitutionalization and Crime Levelsapi-3785090100% (1)
- Abnormal PsychologyDocument12 pagesAbnormal PsychologyDragana ModestyNo ratings yet
- Research Proposal Katherine ZamoraDocument6 pagesResearch Proposal Katherine Zamoraapi-310067380No ratings yet
- Psych Unit 1Document30 pagesPsych Unit 1blancher erNo ratings yet
- Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital DiversionFrom EverandMultimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital DiversionNo ratings yet
- Clinical management and processes in mental healthDocument8 pagesClinical management and processes in mental healthPaula AndreaNo ratings yet
- Bio-Medical Model ArgumentDocument12 pagesBio-Medical Model ArgumentCristín Ní Liatháin0% (1)
- LEXICON International Media Guide For Mental Health - FINAL - LexiconDocument16 pagesLEXICON International Media Guide For Mental Health - FINAL - LexiconVaishnavi JayakumarNo ratings yet
- Community Mental Health Current Scenario Dr. Manish KumarDocument63 pagesCommunity Mental Health Current Scenario Dr. Manish KumarManish KumarNo ratings yet
- DB Week 10 DrugDocument3 pagesDB Week 10 DrugzobiaNo ratings yet
- Rise of Community PsychologyDocument10 pagesRise of Community PsychologySamit RajanNo ratings yet
- Psychiatric Nursing NCLEX ReviewerDocument50 pagesPsychiatric Nursing NCLEX ReviewerJohn Paul Richard MindanaoNo ratings yet
- Research Paper Outline On Mental IllnessDocument5 pagesResearch Paper Outline On Mental Illnessijsgpibkf100% (1)
- Cocept of Community Psychiatry and Community BDocument13 pagesCocept of Community Psychiatry and Community BJOICENo ratings yet
- Counseling From Within: The Microbiome Mental Health ConnectionFrom EverandCounseling From Within: The Microbiome Mental Health ConnectionNo ratings yet
- The Myth of Mental Illness: Foundations of a Theory of Personal ConductFrom EverandThe Myth of Mental Illness: Foundations of a Theory of Personal ConductRating: 3 out of 5 stars3/5 (17)
- Thrive: How Better Mental Health Care Transforms Lives and Saves MoneyFrom EverandThrive: How Better Mental Health Care Transforms Lives and Saves MoneyRating: 3.5 out of 5 stars3.5/5 (2)
- Mental Health Worldwide: Culture, Globalization and DevelopmentFrom EverandMental Health Worldwide: Culture, Globalization and DevelopmentNo ratings yet
- Chapter 5: Legal Issues: Keltner: Psychiatric Nursing, 5 EditionDocument7 pagesChapter 5: Legal Issues: Keltner: Psychiatric Nursing, 5 EditionWarrenPeaceNo ratings yet
- Chapter 4: Models For Working With Psychiatric Patients: Keltner: Psychiatric Nursing, 5 EditionDocument7 pagesChapter 4: Models For Working With Psychiatric Patients: Keltner: Psychiatric Nursing, 5 EditionWarrenPeaceNo ratings yet
- Chapter 3: Continuum of Care: Keltner: Psychiatric Nursing, 5 EditionDocument7 pagesChapter 3: Continuum of Care: Keltner: Psychiatric Nursing, 5 EditionWarrenPeaceNo ratings yet
- CholesistectomyDocument3 pagesCholesistectomyDenjo BonillaNo ratings yet
- Proyecto Sa Araling PalipunanDocument7 pagesProyecto Sa Araling PalipunanWarrenPeaceNo ratings yet
- Tax Suggested Answers (1994-2006) - NoRestrictionDocument138 pagesTax Suggested Answers (1994-2006) - NoRestrictionWarrenPeaceNo ratings yet
- Civil Law Syllabus 2015Document2 pagesCivil Law Syllabus 2015ChiefJusticeLaMzNo ratings yet
- Chapter 2: Psychotherapeutic Management in The Continuum of CareDocument3 pagesChapter 2: Psychotherapeutic Management in The Continuum of CareWarrenPeaceNo ratings yet
- IV Therapy GuideDocument34 pagesIV Therapy GuideWarrenPeaceNo ratings yet
- Leadership & Mngt.Document34 pagesLeadership & Mngt.WarrenPeaceNo ratings yet
- Hematology: Jan Bazner-Chandler CPNP, CNS, MSN, RNDocument80 pagesHematology: Jan Bazner-Chandler CPNP, CNS, MSN, RNWarrenPeaceNo ratings yet
- Biodiversity MeaningDocument34 pagesBiodiversity MeaningWarrenPeaceNo ratings yet
- Drug Study (Isolation Room)Document9 pagesDrug Study (Isolation Room)WarrenPeaceNo ratings yet
- 5CC 2020 Virtual Conference Program PDFDocument29 pages5CC 2020 Virtual Conference Program PDFhuyenthanh1807No ratings yet
- Exploration of Health Status, Illness Perceptions, Coping Strategies, and Psychological Morbidity in Stoma PatientsDocument21 pagesExploration of Health Status, Illness Perceptions, Coping Strategies, and Psychological Morbidity in Stoma Patientssivagiri.pNo ratings yet
- DSM 5 Update 2015 PDFDocument30 pagesDSM 5 Update 2015 PDFFlo RenceNo ratings yet
- Patient at Risk Score (PARS) Clinical Guideline SummaryDocument5 pagesPatient at Risk Score (PARS) Clinical Guideline SummaryValtesondaSilvaNo ratings yet
- A Multidisciplinary Care Map For A Woman in Preterm Labor LazaletaDocument3 pagesA Multidisciplinary Care Map For A Woman in Preterm Labor Lazaletablythe RiveroNo ratings yet
- Hand Hygiene Action Plan - Final Draft For IPCGDocument10 pagesHand Hygiene Action Plan - Final Draft For IPCGAnton NaingNo ratings yet
- Mba20238 A Rosemont CaseDocument2 pagesMba20238 A Rosemont CaseJeevanandam PNo ratings yet
- Multi-Specialty Hospital: Ram Sharada Healthcare Pvt. LTDDocument48 pagesMulti-Specialty Hospital: Ram Sharada Healthcare Pvt. LTDsubhash goelNo ratings yet
- 6.3 FA#3.B (Staffing) : Attempt HistoryDocument8 pages6.3 FA#3.B (Staffing) : Attempt HistoryGil GanibanNo ratings yet
- Medical RealDocument1 pageMedical Realapi-252555369No ratings yet
- Health Promotion Paper Nur 330Document13 pagesHealth Promotion Paper Nur 330api-625175559No ratings yet
- Molecular Imaging: GE HealthcareDocument11 pagesMolecular Imaging: GE HealthcarexibearNo ratings yet
- Effectiveness of Information, Education and Communication Package On Knowledge On Developmental Care Among Mothers of Low Birth Weight BabiesDocument12 pagesEffectiveness of Information, Education and Communication Package On Knowledge On Developmental Care Among Mothers of Low Birth Weight Babiesiaset123No ratings yet
- Weekly Outbreak COVID 19 ReportDocument44 pagesWeekly Outbreak COVID 19 ReportSinclair Broadcast Group - EugeneNo ratings yet
- Doctor Mahavir EnclaveDocument22 pagesDoctor Mahavir EnclaveFortune BuildersNo ratings yet
- Test Bank For Essentials of Dental Assisting 6th Edition by RobinsonDocument8 pagesTest Bank For Essentials of Dental Assisting 6th Edition by Robinsonashleyhaaswxcbmagsde100% (30)
- Overview of pediatric nursing الباب الاولDocument2 pagesOverview of pediatric nursing الباب الاولmathio medhatNo ratings yet
- Critical Appraisal KADocument35 pagesCritical Appraisal KAKentVilandkaNo ratings yet
- Makalah Company Profile Group-6Document11 pagesMakalah Company Profile Group-6Amoysz QheabotNo ratings yet
- Medical Devices VP President CEO in Raleigh Durham NC Resume Scott SpinkaDocument4 pagesMedical Devices VP President CEO in Raleigh Durham NC Resume Scott SpinkaScottSpinkaNo ratings yet
- Public Health Nurse PHN Final Exam Past Questions For WAHEBDocument3 pagesPublic Health Nurse PHN Final Exam Past Questions For WAHEBCharles Obaleagbon86% (7)
- Brgy. Talandang and Baganihan 2022 ConsolidatedDocument6 pagesBrgy. Talandang and Baganihan 2022 Consolidatedevelyn d. pepitoNo ratings yet
- MS Case # 4 - Endo, Uro, Burns, FE & AB ImbalancDocument3 pagesMS Case # 4 - Endo, Uro, Burns, FE & AB ImbalancDemocrito Louierick Plaza VINo ratings yet
- Bahasa Inggris - NurfadilahDocument6 pagesBahasa Inggris - NurfadilahHardianiNo ratings yet
- Med Cert Bataraza-2023Document40 pagesMed Cert Bataraza-2023franchiser6No ratings yet
- PPD Pertemuan 12 (Klasifikasi Tes Psikologi HIMPSI)Document32 pagesPPD Pertemuan 12 (Klasifikasi Tes Psikologi HIMPSI)Pengisi Dompet50% (2)
- Billing and Coding Professional Certification Exam Review: HCPCS Coding and Reimbursement IssuesDocument39 pagesBilling and Coding Professional Certification Exam Review: HCPCS Coding and Reimbursement IssuesEbony CrawfordNo ratings yet
- Peaceful End of Life Theory.Document36 pagesPeaceful End of Life Theory.Resty Patriarca Anibigno75% (8)
- 1) Community PharmacyDocument17 pages1) Community PharmacyDr. Zirwa AsimNo ratings yet
- Management of Preoperative Anemia: Laura Mendez-Pino,, Andrés Zorrilla-Vaca,, David L. HepnerDocument9 pagesManagement of Preoperative Anemia: Laura Mendez-Pino,, Andrés Zorrilla-Vaca,, David L. HepneryenuginNo ratings yet