Professional Documents
Culture Documents
Hpylori
Uploaded by
carlosvalxOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hpylori
Uploaded by
carlosvalxCopyright:
Available Formats
Articles
14-day triple, 5-day concomitant, and 10-day sequential
therapies for Helicobacter pylori infection in seven Latin
American sites: a randomised trial
E Robert Greenberg, Garnet L Anderson, Douglas R Morgan, Javier Torres, William D Chey, Luis Eduardo Bravo, Ricardo L Dominguez,
Catterina Ferreccio, Rolando Herrero, Eduardo C Lazcano-Ponce, Mara Mercedes Meza-Montenegro, Rodolfo Pea, Edgar M Pea,
Eduardo Salazar-Martnez, Pelayo Correa, Mara Elena Martnez, Manuel Valdivieso, Gary E Goodman, John J Crowley, Laurence H Baker
Summary
Background Evidence from Europe, Asia, and North America suggests that standard three-drug regimens of a protonpump inhibitor plus amoxicillin and clarithromycin are significantly less effective for eradication of Helicobacter pylori
infection than are 5-day concomitant and 10-day sequential four-drug regimens that include a nitroimidazole. These
four-drug regimens also entail fewer antibiotic doses than do three-drug regimens and thus could be suitable for
eradication programmes in low-resource settings. Few studies in Latin America have been done, where the burden of
H pylori-associated diseases is high. We therefore did a randomised trial in Latin America comparing the effectiveness
of four-drug regimens given concomitantly or sequentially with that of a standard 14-day regimen of triple therapy.
Methods Between September, 2009, and June, 2010, we did a randomised trial of empiric 14-day triple, 5-day
concomitant, and 10-day sequential therapies for H pylori in seven Latin American sites: Chile, Colombia, Costa Rica,
Honduras, Nicaragua, and Mexico (two sites). Participants aged 2165 years who tested positive for H pylori by a urea
breath test were randomly assigned by a central computer using a dynamic balancing procedure to: 14 days of
lansoprazole, amoxicillin, and clarithromycin (standard therapy); 5 days of lansoprazole, amoxicillin, clarithromycin,
and metronidazole (concomitant therapy); or 5 days of lansoprazole and amoxicillin followed by 5 days of lansoprazole,
clarithromycin, and metronidazole (sequential therapy). Eradication was assessed by urea breath test 68 weeks after
randomisation. The trial was not masked. Our primary outcome was probablity of H pylori eradication. Our analysis
was by intention to treat. This trial is registered with ClinicalTrials.gov, registration number NCT01061437.
Findings 1463 participants aged 2165 years were randomly allocated a treatment: 488 were treated with 14-day
standard therapy, 489 with 5-day concomitant therapy, and 486 with 10-day sequential therapy. The probability of
eradication with standard therapy was 822% (401 of 488), which was 86% higher (95% adjusted CI 26145) than
with concomitant therapy (736% [360 of 489]) and 56% higher (004% to 116) than with sequential therapy
(765% [372 of 486]). Neither four-drug regimen was significantly better than standard triple therapy in any of the
seven sites.
Interpretation Standard 14-day triple-drug therapy is preferable to 5-day concomitant or 10-day sequential four-drug
regimens as empiric therapy for H pylori infection in diverse Latin American populations.
Funding Bill & Melinda Gates Foundation, US National Institutes of Health.
Introduction
Helicobacter pylori infects most of the worlds adult
population and is the principal cause of gastric cancer,
accounting for an estimated 60% of all cases.13 Gastric
cancer is second only to lung cancer as a cause of cancer
death worldwide, and almost all of the nearly 1 million
cases and 075 million deaths each year occur in east
Asia and Latin America.4 Although gastric cancer death
rates have fallen in recent decades, the number of deaths
has actually increased as a consequence of ageing
populations, and gastric cancer is projected to rank
among the ten leading global causes of death by 2030.5,6
H pylori is also the main cause of peptic ulcer disease,
which accounts for the loss of about 46 million disabilityadjusted life-years every year worldwide, with most
of the burden borne by populations in low-income and
middle-income countries.7 Population-wide eradication
programmes seem to offer the most direct approach to
reducing the enormous human and economic con
sequences of H pylori infection; however, none has been
implemented to date.8
Large programmes for H pylori eradication require a
practical and inexpensive antibiotic regimen that is
effective in the specific locale where it will be used.
Standard antibiotic regimens for H pylori usually entail a
proton-pump inhibitor, amoxicillin, and clarithromycin,
taken together over 714 days.911 However, the effective
ness of these triple-therapy regimens seems to have
diminished over time, largely as a result of emerging
resistance of the organism to clarithromycin.12,13 Recent
meta-analyses have shown that regimens that add a
nitroimidazole (metronidazole or tinidazole) to triple
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Published Online
July 20, 2011
DOI:10.1016/S01406736(11)60825-8
See Online/Comment
DOI:10.1016/S01406736(11)61099-4
SWOG Statistical Center, Cancer
Research and Biostatistics,
Seattle, WA, USA
(E R Greenberg MD,
G L Anderson PhD,
J J Crowley PhD); Division of
Public Health Sciences, Fred
Hutchinson Cancer Research
Center, Seattle, WA, USA
(E R Greenberg, G L Anderson,
G E Goodman MD); Division of
Gastroenterology, University
of North Carolina, Chapel Hill,
NC, USA (D R Morgan MD);
Unidad de Investigacin en
Enfermedades Infecciosas,
Instituto Mexicano del Seguro
Social, Mexico City, Mexico
(J Torres PhD); Division of
Gastroenterology, University
of Michigan Medical School,
Ann Arbor, MI, USA
(W D Chey MD); Departamento
de Patologa, Universidad
del Valle, Cali, Colombia
(L E Bravo MD); Hospital
Regional de Occidente, Santa
Rosa de Copn, Honduras
(R L Dominguez MD);
Departamento de Salud
Pblica, Pontificia Universidad
Catlica de Chile, Santiago,
Chile (C Ferreccio MD);
Fundacin INCIENSA, San Jos,
Costa Rica (R Herrero MD);
Screening and Prevention
Group, International Agency
for Research on Cancer, World
Health Organization, Lyon,
France (R Herrero); Instituto
Nacional de Salud Pblica,
Cuernavaca, Mexico
(E C Lazcano-Ponce MD,
E Salazar-Martnez PhD);
Instituto Tecnolgico de
Sonora, Ciudad Obregn,
Mexico
(M M Meza-Montenegro PhD);
Centro de Investigacin en
Demografa y Salud, Len,
Articles
Nicaragua (R Pea PhD,
E M Pea MD); Division of
Gastroenterology, Vanderbilt
Medical Center, Nashville, TN,
USA (P Correa MD); Cancer
Prevention and Control,
University of Arizona Cancer
Center, Tuscon, AZ, USA
(M E Martnez PhD); Division of
Hematology/Oncology,
University of Michigan Medical
School, Ann Arbor, MI, USA
(M Valdivieso MD, L H Baker DO);
and Swedish Cancer Institute,
Seattle, WA, USA
(G E Goodman)
Correspondence to:
Dr E Robert Greenberg, Cancer
Research and Biostatistics,
1730 Minor Ave, Suite 1900,
Seattle, WA, USA 981011468
e.r.greenberg@dartmouth.edu
For more on the
Rome III diagnostic
questionnaire see http://
www.theromefoundation.org
therapy and are given either sequentially for 10 days or
concomitantly for 5 days are significantly more successful
at eradication of H pylori infection than are triple-therapy
regimens.1416 These regimens also require fewer doses of
antibiotics and thus might be more affordable in lowresource settings. Almost all the evidence supporting
these four-drug regimens comes from Europe and Asia;
few data are available from Latin America, a region with
some of the worlds highest rates of gastric cancer
mortality.17 We therefore undertook a randomised trial in
Latin America comparing the effectiveness of four-drug
regimens given concomitantly or sequentially with that
of a standard 14-day regimen of triple therapy. The trial
also provided insights into the feasibility of communitybased programmes of H pylori eradication.
Methods
Study design and patients
The trial (SWOG S0701) was a randomised trial of empiric
14-day triple, 5-day concomitant, and 10-day sequential
therapies for H pylori infection in seven Latin American
sites: Chile (Santiago), Colombia (Tquerres), Costa Rica
(Guanacaste), Honduras (Santa Rosa de Copn), Mexico
(Ciudad Obregn and Tapachula), and Nicaragua (Len).
Between September, 2009, and June, 2010, study research
staff recruited potential participants from the general
population of adult men and women aged 2165 years
and explained the purpose and eligibility requirements
of the study to them. Staff in Colombia, Costa Rica, and
Nicaragua selected individuals from a census of
households, in Chile they selected potential participants
from a list of individuals served by a large public primary
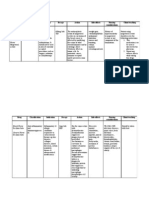
1859 assessed for eligibility
390 excluded
375 UBT negative
8 UBT positive, ineligible
7 withdrew consent
before UBT
1469 randomised
6 excluded because of data
entry errors
488 allocated to standard therapy
489 allocated to concomitant therapy
486 allocated to sequential therapy
488 analysed
475 valid follow-up UBTs
13 missing or invalid
follow-up UBTs
11 withdrew consent or
refused treatment
2 unable to contact
489 analysed
471 valid follow-up UBTs
18 missing or invalid
follow-up UBTs
12 withdrew consent or
refused treatment
5 unable to contact
1 too ill to return
486 analysed
468 valid follow-up UBTs
18 missing or invalid
follow-up UBTs
13 withdrew consent or
refused treatment
2 inconclusive UBTs
3 unable to contact
Figure: Trial profile
UBT=urea breath test.
care clinic, and in Honduras and Mexico (two sites) they
recruited participants by walking house-to-house within
the local community or through announcements at
primary care clinics.
Study participants in Tapachula (Mexico), Nicaragua,
and Chile were predominantly urban, and those in the
other sites were from small, rural communities.
Potential participants were deemed ineligible if they
had been treated in the past for H pylori infection, had
serious illnesses that might end their lives before
completing the study, or had other disorders that
required or precluded treatment with antibiotics or
proton-pump inhibitors. They also had to agree to
abstain from alcohol use for at least 2 weeks. Those
who expressed an interest in participating and gave
signed, informed consent then completed an interview
regarding socioeconomic characteristics and health
history and a detailed gastrointestinal-symptom-history
assessment with the validated Spanish language version
of the Rome III diagnostic questionnaire for the adult
functional gastrointestinal disorders.18,19 The institu
tional review boards for each clinical centre and for the
SWOG Statistical Center, Seattle, WA, USA approved
the study protocol.
Procedures
Participants provided a urea breath test for H pylori
infection by exhaling into foil balloons before, and 30 min
after, consuming a 75 mg dose of C-labelled urea with
water. Staff at each centre analysed the breath samples
using an infrared mass spectrometry device (IRIS,
Wagner Analysen Technik, Bremen, Germany) that
produced a computer-generated result of positive (change
relative to baseline 40%) or negative (change relative to
baseline <25%); intermediate values were classified as
inconclusive. If a participant reported use of an antibiotic
or proton-pump inhibitor within the past 15 days, or if
the result from the urea breath test was inconclusive, the
test was rescheduled for a later date.
Study staff contacted participants at least once during
treatment to encourage adherence and to remind them
to return any unused doses at their follow-up visit, which
was scheduled to occur 68 weeks after randomisation.
During follow-up visits, participants completed another
interview assessing adherence to therapy, their reasons
for missing any doses of the regimens, and the occurrence
of any new or worsened medical disorders that led them
to seek medical attention. Study staff counted the number
of drug doses returned and administered the follow-up
urea breath test.
Randomisation and masking
Participants who had a positive urea breath test and met
all other eligibility criteria were randomly assigned, in
equal proportions, to one of three treatment groups:
standard triple therapy of lansoprazole 30 mg, amoxicillin
1000 mg, and clarithromycin 500 mg taken twice a day for
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Articles
14 days; concomitant therapy of lansoprazole 30 mg,
amoxicillin 1000 mg, clarithromycin 500 mg, and
metronidazole 500 mg taken twice a day for 5 days; or
sequential therapy of lansoprazole 30 mg and amoxicillin
1000 mg taken twice a day for 5 days followed by
lansoprazole 30 mg, clarithromycin 500 mg, and
metronidazole 500 mg taken twice a day for 5 days. Each
clinical centre purchased its own supply of the drugs, as
generic (off-patent) preparations, from suppliers in
country, except the centres in Honduras and Nicaragua,
which both used the same supplier in Honduras. The
drug suppliers provided quality-control data for the
content and dissolution of each drug. Randomisation was
implemented centrally through a dynamic balancing
procedure at the SWOG Statistical Center to ensure
balance within centre by age and sex across the three
regimens. Staff at the clinical centres entered data for
potentially-eligible, consented individuals into the SWOG
Statistical Center computer using a web-based data entry
system. If the participants met all eligibility requirements,
the computer assigned them to a treatment group and
immediately transmitted the treatment assignment to the
clinical centre. All participants were randomly assigned in
a 1:1:1 ratio within 2 weeks after a positive urea-breath-test
result. The trial was not masked.
Statistical analysis
We designed the study to address two primary hypotheses.
The first hypothesis was that 5-day concomitant therapy
was not inferior to 14-day standard therapy, whereby
inferiority was defined as a difference in eradication
probability of 5% or greater in favour of standard therapy.
We reasoned that the shorter duration and lower cost
associated with concomitant therapy would make it
preferable to standard therapy if it were not appreciably
less effective in eradication of H pylori infection. Our
second hypothesis was that 10-day sequential therapy
would be more effective than 14-day standard therapy,
because a four-drug sequential regimen would be
preferred over standard three-drug therapy only if it were
clearly superior in eradication of H pylori infection.
Assuming an eradication rate of 80% for standard
therapy, 10% missing follow-up urea-breath-test results,
and 210 randomised participants per centre (1470 total),
each treatment group comparison would have 82% power
to detect a difference of 8% or greater, based on a twosided, 0025-level test. Although a meta-analysis by Essa
and colleagues16 suggested that concomitant therapy was
about 10% better than sequential therapy, if the therapies
were actually equivalent the trial would have 46% power
to reject the inferiority of concomitant therapy, based on
a one-sided, 0025-level test.
Our primary statistical analyses adhered to the
intention-to-treat principle and included all randomised
eligible participants, with those without a definitive
follow-up urea breath test judged to be treatment failures
(urea-breath-test positive). To compare concomitant
5-day
14-day
concomitant
standard
therapy (N=488) therapy (N=489)
10-day
sequential
therapy (N=486)
Total
(N=1463)
Centre
Santiago (Chile)
69 (14%)
70 (14%)
70 (14%)
Tquerres (Colombia)
71 (15%)
72 (15%)
69 (14%)
209 (14%)
212 (15%)
Guanacaste (Costa Rica)
70 (14%)
70 (14%)
70 (14%)
210 (14%)
Copn (Honduras)
70 (14%)
72 (15%)
71 (15%)
213 (15%)
Tapachula (Mxico)
71 (15%)
69 (14%)
70 (14%)
210 (14%)
Obregn (Mxico)
70 (14%)
69 (14%)
71 (15%)
210 (14%)
Len (Nicaragua)
67 (14%)
67 (14%)
65 (13%)
199 (14%)
Women
287 (59%)
288 (60%)
286 (59%)
861 (59%)
Men
201 (41%)
201 (41%)
200 (41%)
602 (41%)
Sex
Age (years)
2029
66 (14%)
66 (14%)
91 (19%)
223 (15%)
3039
137 (28%)
139 (28%)
117 (24%)
393 (27%)
4049
142 (29%)
117 (24%)
127 (26%)
386 (26%)
50
143 (29%)
167 (34%)
151 (31%)
461 (32%)
Years of education
4
88 (18%)
77 (16%)
80 (17%)
245 (17%)
58
135 (28%)
166 (34%)
143 (29%)
444 (30%)
912
146 (30%)
135 (28%)
136 (28%)
417 (29%)
13
71 (15%)
71 (15%)
70 (14%)
212 (14%)
Not reported
48 (10%)
40 (8%)
57 (12%)
145 (10%)
Chronic dyspeptic symptoms
Present
125 (26%)
121 (25%)
127 (26%)
373 (26%)
Absent
363 (74%)
368 (75%)
359 (74%)
1090 (75%)
Data are n (%).
Table 1: Participant characteristics by treatment group
Standard
therapy (N=475)
Concomitant
therapy (N=471)
Sequential
therapy (N=470)
Total
(N=1416*)
427 (90%)
442 (94%)
437 (93%)
1306 (92%)
7 (2%)
0 (0)
Most (5080%)
24 (5%)
14 (3%)
Less than half (<50%)
Amount of drugs taken
All (100%)
Nearly all (>80%)
2 (<1%)
21 (4%)
9 (<1%)
59 (4%)
10 (2%)
8 (2%)
5 (11%)
23 (2%)
Undetermined (but not all)
7 (2%)
5 (1%)
5 (1%)
17 (1%)
None
0 (0)
2 (<1%)
0 (0)
2 (<1%)
Reasons for not taking all drugs
Concern about having or
developing side-effects
Unrelated illness or injury
Forgot or inconvenient
Reason not given
41 (9%)
3 (1%)
36 (8%)
0 (0)
28 (6%)
1 (<1%)
25 (5%)
3 (<1%)
33 (7%)
5 (1%)
37 (8%)
2 (<1%)
102 (7%)
9 (<1%)
98 (7%)
5 (<1%)
Data are n (%). *Includes 1414 participants with a valid follow-up urea breath test and two (from the sequential
therapy group) whose urea breath test results were inconclusive. Based on count of returned drugs and self-report
among participants who returned for a follow-up urea breath test. Multiple responses allowed.
Table 2: Adherence to treatment of patients that returned for 6-week follow-up, by treatment group
versus standard therapy, we used a two-sample Z test of
the null hypothesis, in which the difference in the
estimated probabilities of eradication was 5% or greater
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Articles
in favour of the standard regimen, based on a one-sided
test of non-inferiority. Comparison of sequential versus
standard therapies was based on a two-sample Z test for
no difference between eradication probabilities. Sensi
tivity to missing data assumptions was examined by
N
Helicobacter pylori
eradication
Difference from standard group
(adjusted 95% CI for difference)
14-day standard therapy
488
401 (822% [785 to 855])
5-day concomitant therapy
489
360 (736% [695 to 775])
86% (26 to 145)
10-day sequential therapy
486
372 (765% [725 to 802])
56% (04 to 116)
Intention to treat (N= 1463)
Definitive 6-week UBT (N=1414)
14-day standard therapy
475
401 (844% [808 to 876])
5-day concomitant therapy
471
360 (764% [723 to 802])
80% (22 to 137)
10-day sequential therapy
468
372 (794% [755 to 831])
49% (09 to 108)
Adherent to therapy (N=1314)
14-day standard therapy
434
378 (871% [836 to 901])
5-day concomitant therapy
442
348 (787% [746 to 825])
84% (27 to 140)
10-day sequential therapy
438
355 (811% [771 to 846])
60% (03 to 118)
Data are number (% [95% CI]) unless otherwise indicated. UBT=urea breath test.
Table 3: Helicobacter pylori eradication by treatment group for three definitions of analysis population
N
Sex
Women
14-day standard
Helicobacter pylori
eradication
Difference from standard p value for
group (adjusted 95% CI) interaction*
861
287
234 (815%)
091
5-day concomitant
288
207 (719%)
97% (18 to 175)
10-day sequential
286
214 (748%)
67% (14 to 148)
Men
602
14-day standard
201
167 (831%)
201
153 (761%)
70% (20 to 159)
10-day sequential
200
158 (790%)
41% (52 to 133)
Age
2140 years
663
021
14-day standard
222
5-day concomitant
220
164 (745%)
74% (13 to 162)
10-day sequential
221
160 (724%)
96% (03 to 189)
4165 years
800
182 (820%)
14-day standard
266
219 (823%)
5-day concomitant
269
196 (729%)
95% (14 to 175)
10-day sequential
265
212 (800%)
23% (56 to 103)
Chronic dyspeptic symptoms
Absent
1090
363
5-day concomitant
368
277 (753%)
65% (02 to 133)
10-day sequential
359
281 (783%)
35% (34 to 105)
Present
14-day standard
373
297 (818%)
038
14-day standard
125
104 (832%)
5-day concomitant
121
83 (686%)
146% (25 to 267)
10-day sequential
127
91 (717%)
115% (09 to 240)
(Continues on next page)
Role of the funding source
The sponsors of the study had no role in study design,
data collection, data analysis, data interpretation, or
writing of the report. All authors had full access to the
data in the study and participated in the decision to
submit for publication.
Results
5-day concomitant
excluding data from participants without a conclusive
follow-up urea breath test. To establish how poor
adherence could have affected our conclusions, we
further restricted the analyses to participants with a
definitive urea breath test who had taken at least 80% of
their assigned study drugs.
Secondary analyses assessed variability in treatment
outcome by sex, age, presence of chronic dyspeptic
symptoms, and clinical centre. Tests of interaction were
calculated as deviance tests comparing logistic regression
models with the treatment group indicators, the
designated covariate, and their interaction terms, with
those without the interaction terms.
All analyses were done with SAS version 9.2 and
R version 2.12.2 statistical software. Bonferroni-adjusted
95% CIs were used to account for the two primary
comparisons, and p values less than 0025 were classed
as statistically significant. No corrections for multiplicity
were applied to secondary analyses, because they were
considered to be exploratory. All p values were twosided except the test of non-inferiority.
This trial is registered with ClinicalTrials.gov, regis
tration number NCT01061437.
1859 potentially-eligible adults agreed to participate in the
study and completed the screening interview and intake
questionnaire, but seven withdrew before the urea breath
test (figure). The test was positive for 1471 (79%) of
1852 tested participants. Eight patients with a positive test
were not randomly assigned because they opted not to be
treated, could not be randomly assigned within 2 weeks of
their urea breath test, or had a disqualifying factor
(eg, pregnancy). Six participants with a negative urea
breath test, who were randomly assigned incorrectly
because of data entry errors, were withdrawn from the
study before receiving treatment, and their data were not
included in any of the following analyses. Of the eligible
participants who were randomised, 861 (59%) of 1463 were
women, 847 (58%) of 1463 were age 40 years or older, and
373 (25%) of 1463 had chronic dyspeptic symptoms as
classified by the Rome III criteria. Participant characteristics
were balanced between the three treatment groups (table 1).
47 participants did not return for their follow-up urea
breath test, and two participants had follow-up tests that
were inconclusive after two repeat tests. Thus, we obtained
definitive follow-up urea-breath-test results for 1414 (97%)
of 1463 of the randomised eligible participants (figure).
Table 2 shows adherence to treatment of patients
that returned for 6-week follow-up. 1313 (92%) of
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Articles
1416 participants who returned for their follow-up visit
had taken at least 80% of their assigned drugs, as
assessed by pill count and self-report (table 2). Five
participants had new, therapy-related symptoms
(stomach discomfort, nausea or vomiting, or fatigue or
weakness) that led them to seek medical attention; one
in the standard treatment group and two each in the
concomitant and sequential treatment groups.
In intention-to-treat analyses, the estimated probability
of H pylori eradication was higher with 14-day standard
triple therapy than with 5-day concomitant therapy and
10-day sequential therapy (table 3). The null hypothesis
of inferiority of concomitant therapy to standard therapy
could not be rejected (one-sided p=091); thus, the data
are consistent with 5-day concomitant therapy being
inferior to 14-day standard therapy. The difference
between 10-day sequential therapy and standard therapy
was not significant (p=004) at the p=0025 level, but the
near statistical significance of this two-sided test suggests
that sequential therapy was not as effective as standard
therapy. Sensitivity analyses that excluded participants
without a definitive follow-up urea breath test and those
that were confined to participants who had adhered to
the prescribed regimens showed similar patterns of
treatment contrasts as the intention-to-treat analysis, but
with somewhat higher estimated eradication probabilities
(table 3). Secondary analyses examining potential inter
actions showed no significant interactions between
treatment and sex, age, presence of chronic dyspeptic
symptoms at baseline, or study centre (table 4).
Differences between study sites occurred in the overall
probability of eradication in both the intention-to-treat
populations (table 4) and the adherent-to-therapy popu
lation (webappendix), but nowhere was either four-drug
regimen clearly better than standard triple therapy.
Discussion
Our principal outcome measure, the probability of
H pylori eradication, was higher for 14-day standard triple
therapy than for both four-drug regimens, and these
results did not vary significantly by age, sex, study site, or
history of chronic dyspeptic symptoms. The prevalence
of H pylori infection in screened participants was high,
and nearly all individuals who had a positive urea breath
test were randomly assigned into the trial. Participants
tended to adhere closely to the protocol by returning for
their follow-up urea breath test and taking their prescribed
tablets. In the three treatment groups, the difference in
adherence and serious side-effects was small.
H pylori presents a major global health challenge,
which can probably best be addressed through practical,
inexpensive, and population-based interventions in the
resource-limited countries where it is most prevalent.
From this perspective the size of our trial, technical
simplicity, broad geographic coverage within Latin
America, community-based population, use of locally
sourced generic drugs, and statistically robust findings
Helicobacter pylori
eradication
Difference from standard p value for
group (adjusted 95% CI) interaction*
(Continued from previous page)
Study site
Santiago (Chile)
14-day standard
209
69
59 (855%)
028
5-day concomitant
70
46 (657%)
10-day sequential
70
59 (843%)
Tquerres (Colombia)
212
14-day standard
71
58 (817%)
5-day concomitant
72
58 (806%)
11% (135 to 158)
10-day sequential
69
54 (783%)
34% (132 to 200)
Guanacaste (Costa Rica)
14-day standard
210
70
61 (871%)
198% (39 to 357)
12% (136 to 161)
5-day concomitant
70
54 (771%)
100% (44 to 244)
10-day sequential
70
63 (900%)
29% (163 to 106)
Copn (Honduras)
213
14-day standard
70
66 (943%)
5-day concomitant
72
62 (861%)
10-day sequential
71
58 (817%)
Tapachula (Mxico)
210
14-day standard
71
55 (775%)
5-day concomitant
69
50 (725%)
10-day sequential
70
47 (671%)
Ciudad Obregn (Mxico)
210
82% (29 to 192)
126% (08 to 26)
50% (114 to 214)
104% (79 to 285)
14-day standard
70
5-day concomitant
69
47 (681%)
90% (78 to 259)
10-day sequential
71
47 (662%)
109% (74 to 292)
Len (Nicaragua)
14-day standard
199
67
54 (771%)
48 (716%)
5-day concomitant
67
43 (642%)
74% (106 to 255)
10-day sequential
65
44 (677%)
39% (155 to 234)
Subgroup analyses for age, sex, and study site were prespecified; subgroup analyses for chronic dyspeptic symptoms
were not. *p value for drop-in-deviance test for significance of interaction with treatment regimen in a logistic
regression model controlling for main effects of treatment and baseline covariate.
Table 4: Summary of Helicobacter pylori eradication by treatment group and selected baseline
characteristics for intention-to-treat population
across important subgroups reflect the realities of a
region where diseases associated with H pylori are
especially burdensome. Our results are important
because they challenge those of meta-analyses showing
that four-drug regimens (triple therapy plus a
nitroimidazole) given concomitantly or sequentially
were clearly better than triple therapy,1416 and they
suggest that findings based primarily on data from
Europe and other high-income regions might not be
readily generalisable to lower-income countries (panel).
We reported probabilities of H pylori eradication of less
than 80% with 5-day concomitant and 10-day sequential
regimens by the intention-to-treat analysis, whereas
meta-analyses had reported probabilities greater than
90% for both.1416 Investigators of a trial from Taiwan
comparing 10-day regimens of concomitant versus
sequential four-drug therapies also reported that both
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
See Online for webappendix
Articles
regimens were more than 90% successful.20 The
estimated effectiveness of our three-drug regimen (82%)
in the intention-to-treat analysis was only modestly
greater than that reported in the meta-analyses
(7779%).1416 Thus, the divergence between our findings
and those of the meta-analyses represents the substantially
worse performance of the four-drug regimens.
Geographical variations in the pattern of H pylori
resistance to antibiotics might account for some of the
discrepancies between the results. In clinical series from
several countries included in our trial, clarithromycin
resistance in H pylori isolates has been reported to be less
prevalent than in Europe, and metronidazole resistance
substantially more prevalent (as high as 80%).2124
Clarithromycin resistance strongly diminishes the
effectiveness of triple therapy, so a better outcome with
triple therapy would be expected if the prevalence of
resistance in our trial population was actually low.13,21,25 A
high prevalence of resistance to metronidazole in our
study population is a plausible, but less certain,
explanation for the worse-than-expected success of the
four-drug regimens.25 Results according to antibiotic
resistance are available from only two trials of sequential
therapy versus triple therapy; the combined data showed
that 68 of 71 (96%) patients with metronidazole-resistant
Panel: Research in context
Systematic review
Consensus groups that represent both global and Latin
American perspectives have designated triple-drug regimens
of a proton-pump inhibitor plus amoxicillin and clarithromycin
taken for 714 days as a standard approach for eradicating
Helicobacter pylori.10,11 However, the effectiveness of these
regimens seems to have diminished to unacceptably low levels
over time,12,13 and recent meta-analyses of clinical trials from
Europe and Asia show that four-drug regimens that add
metronidazole or tinidazole to triple therapy achieve superior
results.1416 The reported meta-analyses have not included any
trials that were undertaken in Latin America, an area where
H pylori-associated diseases are common and where wide-scale
eradication programmes might be needed. We did a Medline
search of all publications up to 2010, with no language
restrictions, using the search terms Helicobacter in
combination with the term for each country in Latin America.
No publications of clinical trials that compared 14-day triple,
5-day concomitant, and 10-day sequential therapies for
Helicobacter pylori infection were identified.
Interpretation
Our findings showed that in the Latin American populations
we studied, by contrast with those for European and some
Asian populations, 14-day standard triple therapy is more
effective than 5-day concomitant or 10-day sequential
four-drug regimens that include metronidazole for eradication
of H pylori. Thus, effectiveness of H pylori eradication regimens
in one area might not be as equally effective elsewhere.
organisms were treated successfully with sequential
therapy compared with 46 of 59 (78%) treated with triple
therapy.16,26 No comparable data from trials of concomitant
versus triple therapy are available. The presence of
organisms resistant to both antibiotics would likely cause
treatment to fail for all three studied regimens, but data
for this topic from Latin America are scarce.
We used a 14-day regimen of triple therapy in our trial,
whereas previous trials of the four-drug regimens
generally compared them to 7 days or 10 days of triple
therapy. In one meta-analysis 14-day triple therapy
regimens were slightly, but significantly, superior to
those of 7 days or 10 days; thus, longer duration
conceivably enhanced the performance of triple therapy
in our trial.27 Success with the four-drug regimens
perhaps would also improve with longer duration;13,20,28
however, this would increase their cost.
We recruited our participants from the general adult
population in the community, whereas previous trials
studied patients with gastrointestinal symptoms.1416 The
success of H pylori treatment with triple therapy or
sequential therapy has not been shown to be affected by a
diagnosis of peptic-ulcer disease or dyspepsia, and the
superiority of triple therapy over the four-drug regimens
in our trial did not vary significantly according to history
of chronic dyspeptic symptoms.14
Our trial was undertaken in the general population in
community settings where it was not feasible to mask
the study or to obtain bacterial specimens for antibiotic
sensitivity testing. We also obtained generic drugs from a
variety of sources and did not have a completely objective
way of determining adherence to therapy. Each of these
factors is a potential limitation of the trial, but we doubt
that any of them represents a serious threat to the validity
of our results. Despite the absence of masking, our
principal outcome measure (urea breath test) was
objectively measured and seems unlikely to be biased.
The absence of antibiotic sensitivity data also should not
affect study validity, but it does make it more difficult to
generalise our results to other regions where sensitivity
patterns could be different. Inaccuracies in patient
reports of adherence to therapy could have lowered our
estimates of treatment effectiveness in the subgroup of
participants classified as adherent, but these inaccuracies
would not compromise the validity of the main results
from our intention-to-treat analyses comparing the
relative effectiveness of the three regimens. Lastly,
although we cannot guarantee that the locally available
generic drugs were of uniform efficacy, differences in
treatment response between centres cannot be easily
attributed to variable drug quality, since some of the
greatest differences were seen between Nicaragua and
Honduras, where investigators obtained drugs from the
same source.
For individuals with H pylori infection in much of Latin
America, 14 days of triple therapy is probably the preferred
empiric treatment. Nevertheless, the 87% eradication
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Articles
success in participants who adhered to the regimen is
suboptimum in the clinical setting, and its effectiveness
might decrease over time as clarithromycin resistance
increases. Improved H pylori treatment regimens for
Latin American populations could conceivably be
designed on the basis of local antibiotic resistance data.
However, the small number of published reports of
antibiotic resistance in this region generally pertain to
H pylori isolates obtained from symptomatic patients
undergoing endoscopy in urban academic centres, and
thus the results might not be applicable to broader
populations.21 In view of the paucity of representative
data for resistance, and the daunting technical and
financial challenges of obtaining these data, treatment
guidelines for Latin America and other regions with
limited resources might have to rely primarily on the
results of large, simple clinical trials of empiric therapies
in the specific populations to which the guidelines would
apply. These data could be supplemented by subsequent
monitoring of effectiveness in practice over time and by
the results of antibiotic-resistance testing in selected
patients, when feasible.
We designed our study as a preliminary step towards
implementation of programmes of gastric cancer
prevention in Latin America. H pylori-associated gastric
cancer results from a long progression from normal
mucosa to invasive cancer.3,29 The most promising
preventive approach seems to be eradication of H pylori
infection before cancer develops, and several randomised
trials have assessed this strategy. The results show that
eradication of this infection slows or reverses progression
of premalignant histological lesions, but no trial has been
large enough to show a definitive cancer-preventive
effect.30,31 Nevertheless, analyses have suggested that
H pylori eradication programmes would be cost effective
over the long term if they prevented only 10% of gastriccancer deaths; over the short term they would reduce
costs of care for peptic ulcers and dyspepsia symptoms.3234
Eradication programmes are potentially even more cost
effective in regions such as Latin America, where the
burden of H pylori-associated diseases is high.
Our results suggest that population-wide clinical trials
or public health programmes of H pylori eradication are
feasible in Latin America. Individuals with a positive
urea breath test readily agreed to be randomly assigned
to antibiotic treatment, and all three regimens of generic
drugs resulted in probabilities of eradication comparable
to those reported in previous prevention programmes.31
The 14-day triple-drug regimen had superior results, but
the lower cost of the shorter duration regimens might
make them acceptable for use in prevention programmes,
where resources are particularly scarce. Other consider
ations, including risks of recrudescence and reinfection
after eradication, will also be important.
Contributors
All the authors participated in the design and oversight of the trial and
in the interpretation and reporting of results, and have seen and
approved the final report. LEB, RLD, CF, RH, MMM-M, RP, and ES-M
directed the clinical activities at the study centres. GLA had principal
responsibility for the statistical analyses of the data.
Conflicts of interest
DRM has submitted a patent application through the University of
North Carolina for a technique using molecular endoscopy to detect
cancer in the gastrointestinal tract, and has received funding from Axcan
for his participation in a speakers bureau; he has also received a
research grant from AstraZeneca, for a proton-pump inhibitor study in
Hispanic populations in the USA, and from Given Imaging, for ongoing
efficacy studies of colon endocapsule efficacy. All other authors declare
that they have no conflicts of interest.
Acknowledgments
The Bill & Melinda Gates Foundation provided financial support for the
trial, and the National Institutes of Health (Grant number CA037429)
supported the SWOG administrative and statistical infrastructure. We
thank the trial participants for making this study possible and recognise
the many contributions of the investigative team members: SWOG
Statistical Center, Seattle, WA, USAVanessa Bolejack, Susie Carlin,
Dacia Christin, Evonne Lackey, and Rachael Sexton; Division of
Gastroenterology, University of North Carolina, Chapel Hill, CA, USA
Paris Heidt; Universidad del Valle, Cali, ColombiaLuz Stella Garca,
Yolanda Mora; Hospital Regional de Occidente, Santa Rosa de Copn,
HondurasJean Paul Higuero, Glenda Jeanette Euceda Wood,
Lesby Maritza Castellanos; Pontificia Universidad Catlica de Chile,
Santiago, ChileMara Paz Cook, Paul Harris, Antonio Rolln; Fundacin
INCIENSA, San Jos, Costa RicaSilvia Jimnez, Paula Gonzlez,
Ana Cecilia Rodrguez, Lidiana Morera, Blanca Cruz Reyes; Instituto
Nacional de Salud Pblica, Cuernavaca, MexicoRogelio Danis,
Erika Marlen Hurtado Salgado, Maria del Pilar Hernndez Nevres;
Instituto Tecnolgico de Sonora, Ciudad Obregn, MexicoMyriam Bringas,
Araceli Molina, Claudia Osorio, Mara de Jess Lpez Valenzuela;
Centro de Investigacin en Demografa y Salud, Len, Nicaragua
Yesenia Zapata; and also Charles A Coltman, David S Alberts, and
Jesse Nodora for their help during the course of the study.
References
1 Infection with Helicobacter pylori. IARC working group on the
evaluation of carcinogenic risks to humans. IARC monographs
on the evaluation of carcinogenic risks to humans. Vol 61.
Schistosomes, liver flukes and Helicobacter pylori. Lyon, France:
International Agency for Research on Cancer, 1994: 177240.
2 Lochhead P, El-Omar EM. Gastric cancer. Br Med Bull 2008;
85: 87100.
3 Parkin, DM. The global health burden of infection-associated
cancers in the year 2002. Int J Cancer 2006; 118: 303044.
4 Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM.
Estimates of worldwide burden of cancer in 2008: GLOBOCAN
2008. Int J Cancer 2010; 127: 2893917.
5 Marugame T, Dongmei Q. Comparison of time trends in stomach
cancer incidence (19731997) in East Asia, Europe and USA, from
cancer incidence in five continents Vol IVVIII. Jpn J Clin Oncol
2007; 37: 24243.
6 Mathers CD, Loncar D. Projections of global mortality and burden
of disease from 2002 to 2030. PLoS Med 2006; 3: e442.
7 WHO. World Health Report 2003, statistical annex, table 3: sex and
mortality stratum in WHO regions, estimates. http://www.who.int/
whr/2003/en/Annex3-en.pdf (accessed June 28, 2011).
8 Graham DY, Shiotani A. The time to eradicate gastric cancer is now.
Gut 2005; 54: 73538.
9 Malfertheiner P, Mgraud F, OMorain C, et al. Current concepts
in the management of Helicobacter pylori infectionThe
Maastricht III Consensus Report. Gut 2007; 56: 77278.
10 Coelho LG, Len-Bara R, Quigley EM. Latin-American Consensus
Conference on Helicobacter pylori infection. Latin-American
National Gastroenterological Societies affiliated with the
Inter-American Association of Gastroenterology (AIGE).
Am J Gastroenterol 2000; 95: 268891.
11 Chey WD, Wong BCY, Practice parameters committee of the
American College of Gastroenterology. American College
of Gastroenterology practice guidelines on the management of the
Helicobacter pylori infection. Am J Gastroenterol 2007; 102: 180825.
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Articles
12 Malfertheiner P, Selgrad M. Helicobacter pylori infection and current
clinical areas of contention. Curr Opin Gastroenterol 2010; 26: 61823.
13 Graham DY, Fischbach L. Helicobacter pylori treatment in the era
of increasing antibiotic resistance. Gut 2010; 59: 114353.
14 Jafri NS, Hornung CA, Howden CW. Meta-analysis: sequential
therapy appears superior to standard therapy for Helicobacter pylori
infection in patients naive to treatment. Ann Intern Med 2008;
148: 92331.
15 Gatta L, Vakil N, Leandro G, Di Mario F, Vaira D. Sequential
therapy or triple therapy for Helicobacter pylori infection: systematic
review and meta-analysis of randomized controlled trials in adults
and children. Am J Gastroenterol 2009; 104: 306979.
16 Essa AS, Kramer JR, Graham DY, Treiber G. Meta-analysis:
four-drug, three-antibiotic, non-bismuth-containing concomitant
therapy versus triple therapy for Helicobacter pylori eradication.
Helicobacter 2009; 14: 10918.
17 Bertuccio P, Chatenoud L, Levi F, et al. Recent patterns in gastric
cancer: a global overview. Int J Cancer 2009; 125: 66673.
18 Morgan DR, Squella FE, Pena E, et al. Multinational validation of
the Spanish Rome III questionnaire: comparable sensitivity and
specificity to the English instrument. Gastroenterology 2010;
138: S-386.
19 Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal
disorders. Gastroenterology 2006; 130: 146679.
20 Wu DC, Hsu PI, Wu JY, et al. Sequential and concomitant therapy
with four drugs is equally effective for eradication of H pylori
infection. Clin Gastroenterol Hepatol 2010; 8: 3641.
21 Mgraud F. H pylori antibiotic resistance: prevalence, importance,
and advances in testing. Gut 2004; 53: 137484.
22 Torres J, Camorlinga-Ponce M, Prez-Prez G, et al. Increasing
multidrug resistance in Helicobacter pylori strains isolated from
children and adults in Mexico. J Clin Microbiol 2001; 39: 267780.
23 Alvarez A, Moncayo JI, Santacruz JJ, Santacoloma M, Corredor LF,
Reinosa E. Antimicrobial susceptibility and mutations involved in
clarithromycin resistance in Helicobacter pylori isolates from
patients in the western central region of Colombia.
Antimicrob Agents Chemother 2009; 53: 402224.
24 Vallejos C, Garrido L, Cceres D, et al. Prevalencia de la resistencia
a metrodinazol, claritromicina y tetraciclina en Helicobacter pylori
aislado de pacientes de la Regin Metropolitana. Rev Med Chil 2007;
135: 28793.
25 Fischbach L, Evans EL. Meta-analysis: the effect of antibiotic
resistance status on the efficacy of triple and quadruple first-line
therapies for Helicobacter pylori. Aliment Pharmacol Ther 2007;
26: 34357.
26 Zullo A, De Francesco V, Hassan C, Morini S, Vaira D. The
sequential therapy regimen for Helicobacter pylori eradication:
a pooled-data analysis. Gut 2007; 56: 135357.
27 Fuccio L, Minardi ME, Zagari RM, Grilli D, Magrini N, Bazzoli F.
Meta-analysis: duration of first-line proton-pump inhibitor based
triple therapy for Helicobacter pylori eradication. Ann Intern Med
2007; 147: 55362.
28 Graham DY, Shiotani A. New concepts of resistance
in the treatment of Helicobacter pylori infections.
Nat Clin Pract Gastroenterol Hepatol 2008; 5: 32131.
29 Correa P, Houghton J. Carcinogenesis of Helicobacter pylori.
Gastroenterology 2007; 133: 65972.
30 Parsonnet J, Forman D. Helicobacter pylori infection and gastric
cancerfor want of more outcomes. JAMA 2004; 291: 24445.
31 Fuccio L, Zagari RM, Eusebi LH, et al. Meta-analysis: can
Helicobacter pylori eradication treatment reduce the risk for gastric
cancer? Ann Intern Med 2009; 151: 12128.
32 Parsonnet J, Harris RA, Hack HM, Owens DK. Modelling
cost-effectiveness of Helicobacter pylori screening to prevent gastric
cancer: a mandate for clinical trials. Lancet 1996; 348: 15054.
33 Mason J, Axon AT, Forman D, Leeds HELP Study Group.
The cost-effectiveness of population Helicobacter pylori screening
and treatment: a Markov model using economic data from
a randomized controlled trial. Aliment Pharmacol Ther 2002;
16: 55968.
34 Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P.
A community screening program for Helicobacter pylori saves
money: 10-year follow-up of a randomized controlled trial.
Gastroenterology 2005; 129: 191017.
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)60825-8
Comment
Mass eradication of Helicobacter pylori: feasible and advisable?
In The Lancet, E Robert Greenberg and colleagues1 present
an Article about the efficacy of three different therapeutic
regimens for the eradication of Helicobacter pylori in
several Latin American countries. A large sample of
adults with symptomatic and asymptomatic disease was
studied. Besides aiming to identify the best therapeutic
regimen, the study also served as a preliminary step to
support future programmes of gastric cancer prevention
in the Latin American population. Gastric cancer is the
fifth most common cause of cancer in this region (figure)
and is the leading cause of cancer mortality among males
in many Latin American countries. The study showed
that the 14-day standard therapy with lansoprazole,
amoxicillin, and clarithromycin was superior to both
the 5-day concomitant and sequential four-drug
regimens (lansoprazole, amoxicillin, clarithromycin,
and metronidazole).
Generic (off-patent) preparations of the study drugs
were used in this trial. The use of low-cost generic drugs
is an important factor for public health strategies in
Latin America. These preparations were validated in the
USA2 and the results from the study done by Greenberg
and colleagues show that good quality generic drugs
were used. However, if these drugs are used in large
populations for H pylori eradication, quality control of
these drugs will be crucial. Recent reports have brought
attention to problems related to the quality of generic
drugs, including antibiotics.3,4
Importantly, Greenberg and colleagues study confirms
that the standard therapy, which includes generic drugs,
remains effective in Latin America, by contrast with
developed countries where resistance to clarithromycin
has been identified.5 We believe however, that costs
could be reduced and the potential for development
of resistant bacterial strains could be decreased, if the
standard therapy could be prescribed over a short period
of time. Findings from two studies done 10 years apart
in Brazil using standard therapy over a 10-day period
showed H pylori eradication rates of about 90%.6,7
H pylori affects around 50% of men, with prevalence
much higher in developing countries than in developed
countries (ie, prevalence in North America is 30%,
in Central America 7090%, and in South America
7090%).8 In 1994, the International Agency for Research
on Cancer defined H pylori as a human carcinogen for
gastric adenocarcinoma, raising concerns about how to
treat people with asymptomatic infection.9
A disturbing issue presented by Greenberg and
colleagues is the suggestion of developing a mass
eradication programme for H pylori in Latin America,
aimed at long-term prevention of at least 10% of gastric
cancer cases, and short-term gain of saving money by
reducing care costs associated with peptic ulcer and
dyspepsia symptoms.
Although the role of H pylori in gastric carcinogenesis
is well defined, no definitive evidence shows that mass
eradication could reduce incidence of gastric cancer.10
Wong and colleagues11 showed no benefit in the
prevention of gastric cancer with the eradication of
H pylori. By contrast, a recent meta-analysis suggested that
eradication could indeed reduce the risk of gastric cancer.12
Policies aimed at population-wide H pylori eradication
could have individual and social repercussions.
Amoxicillin could cause fatal anaphylactic reactions,
while clarithromycin has been associated with
increased mortality in patients with ischaemic heart
disease.13 Furthermore, almost all antibiotics can
cause Clostridium difficile infection, which could
eventually become life threatening. Even if infrequent,
these complications could become important when
eradicating H pylori at a population level. Another
Published Online
July 20, 2011
DOI:10.1016/S01406736(11)61099-4
See Online/Articles
DOI:10.1016/S01406736(11)60825-8
Age-standardised mortality
rates per 100 000
Age-standardised mortality
rates per 100 000
0 29 52 85 138 37
0 17 33 49
73
23
Figure: Mortality of gastric cancer in men and women in Latin America (2008)
(A) Number of deaths in men per 100000 people=128. (B) Number of deaths in women per 100000 people=69.
Modified from GLOBOCAN 2008, International Agency for Research on Cancer.
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)61099-4
Comment
key point to address is the probability of reinfection.
Annual recurrence of H pylori infection is about 12% in
developing countries.14 However, the most serious issue
relates to development of bacterial resistance for not
only H pylori but potentially many other bacteria.
Thus, we believe that although any public policy aimed
at decreasing the prevalence of H pylori infection could
lead to reductions in gastric cancer and peptic ulcer, the
risks associated with antibiotic use might represent an
important limitation to such a strategy. Furthermore,
restricted financial resources in Latin America represent
a major public health challenge. Therefore, appropriate
studies are needed that compare the effect of investment
in sanitation, hygiene, and education with the effect of
mass eradication of H pylori, to assess which options will
be most beneficial to the Latin American population.
Another possible approach is the development of
effective immunisation as a safer method of decreasing
rate of H pylori infection.15 On the one hand, we are aware
that sanitation and immunisation will not reduce the
risk of H pylori-associated disease for people who are
already infected. On the other hand, doubts exist about
the reversibility of already established precursor lesions
in the carcinogenesis cascade in infected patients. Wong
and colleagues11 showed that eradication significantly
decreased the development of gastric cancer only in the
subgroup of H pylori carriers without precancerous lesions.
Mass eradication is a major issue requiring further
investigation. We agree with Greenberg and colleagues
that future properly designed studies addressing
this issue are essential to assess the balance between
positive and negative effects of each strategy. Local
epidemiological data, among other factors, will dictate
allocation of public health resources: countries with
high mortality rates secondary to gastric cancer, such as
Colombia, Chile, and Guatemala, should discuss whether
development of a programme for mass eradication of
H pylori is worthwhile.
In conclusion, mass eradication of H pylori is potentially
feasible but in view of the differing socioeconomic
realities of Latin American countries, doubts remain
about the advisability of such a policy.
*Luiz Edmundo Mazzoleni, Carlos Fernando Francesconi,
Guilherme Becker Sander
Universidade Federal do Rio Grande do Sul, School of Medicine,
Porto Alegre, Brazil (LEM, CFF); Hospital de Clnicas de Porto
Alegre, Department of Gastroenterology, Ramiro Barcelos 2350,
Porto Alegre, Brazil 90035903 (LEM, CFF, GBS); and Post
Graduation Program: Gastroenterology and Hepatology,
Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil
(LEM, CFF)
lemazzoleni@yahoo.com.br
We declare that we have no conflicts of interest.
1
2
3
4
5
6
8
9
10
11
12
13
14
15
Greenberg ER, Anderson GL, Morgan DR, et al. 14-day triple, 5-day
concomitant, and 10-day sequential therapies for Helicobacter pylori
infection in seven Latin American sites: a randomised trial. Lancet 2011;
published online July 20. DOI:10.1016/S0140-6736(11)60825-8.
Davit BM, Nwakama PE, Buehler GJ, et al. Comparing generic and innovator
drugs: a review of 12 years of bioequivalence data from the United States
Food and Drug Administration. Ann Pharmacother 2009; 43: 158397.
Zuluaga AF, Agudelo M, Cardeo JJ, et al. Determination of therapeutic
equivalence of generic products of gentamicin in the neutropenic mouse
thigh infection model. PLoS One 2010; 5: e10744.
Nightingale CH. A survey of the quality of generic clarithromycin products
from 18 countries. Clin Drug Investig 2005; 25: 13552.
Graham DY, Fischbach L. Helicobacter pylori treatment in the era
of increasing antibiotic resistance. Gut 2010; 59: 114353.
Mazzoleni LE, Sander GB, Ott EA, et al. Clinical outcomes of eradication
of Helicobacter pylori in nonulcer dyspepsia in a population with a high
prevalence of infection: results of a 12-month randomized, double blind,
placebo-controlled study. Dig Dis Sci 2006; 51: 8998.
Mazzoleni LE, Sander GB, Francesconi CF. Dyspeptic symptoms after
eradication of Helicobacter pylori in patients with functional dyspepsia.
Heroes-12 Trial (Helicobacter Eradication Relief Of Dyspeptic Symptoms).
Gastroenterology 2010; 138 (suppl 1): S-719.
Everhart JE. Recent developments in the epidemiology of Helicobacter pylori.
Gastroenterol Clin North Am 2000; 29: 55978.
International Agency for Research on Cancer Working Group on the
evaluation of carcinogenic risks to humans. Schistosomes, liver flukes, and
Helicobacter pylori: views and expert opinions of an IARC working group on
the evaluation of carcinogenic risks to humans. Lyon, France: IARC Press,
1994: 177240.
Parsonnet J, Forman D. Helicobacter pylori infection and gastric cancer
for want of more outcomes. JAMA 2004; 291: 24445.
Wong BC, Lam SK, Wong WM, et al. Helicobacter pylori eradication to
prevent gastric cancer in a high-risk region of China: a randomized
controlled trial. JAMA 2004; 291: 18794.
Fuccio L, Zagari RM, Eusebi LH, et al. Meta-analysis: can Helicobacter pylori
eradication treatment reduce the risk for gastric cancer? Ann Intern Med
2009; 151: 12128.
Winkel P, Hilden J, Fischer Hansen J, et al. Excess sudden cardiac deaths after
short-term clarithromycin administration in the CLARICOR trial: why is this
so, and why are statins protective? Cardiology 2011; 118: 6367.
Niv Y. H pylori recurrence after successful eradication. World J Gastroenterol
2008; 14: 147778.
Del Giudice G, Malfertheiner P, Rappuoli R. Development of vaccines
against Helicobacter pylori. Expert Rev Vaccines 2009; 8: 103749.
www.thelancet.com Published online July 20, 2011 DOI:10.1016/S0140-6736(11)61099-4
You might also like
- Health Policy in Portugal July 2016Document2 pagesHealth Policy in Portugal July 2016carlosvalxNo ratings yet
- Health Policy in Slovak Republic March 2017Document2 pagesHealth Policy in Slovak Republic March 2017carlosvalxNo ratings yet
- Health Policy in United Kingdom July 2016Document2 pagesHealth Policy in United Kingdom July 2016carlosvalxNo ratings yet
- Health Policy in Germany July 2016Document2 pagesHealth Policy in Germany July 2016carlosvalxNo ratings yet
- (Vladimir LolitaDocument216 pages(Vladimir Lolitacarlosvalx75% (4)
- 1407 AustraliaDocument46 pages1407 AustraliacarlosvalxNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Pranic Healing PrincipleDocument6 pagesPranic Healing Principleapi-26172340100% (2)
- Main Idea and Text Structure 3Document1 pageMain Idea and Text Structure 3Anjo Gianan TugayNo ratings yet
- .0. Cognitive Behavioral ManagementDocument2 pages.0. Cognitive Behavioral ManagementMarcela PrettoNo ratings yet
- Mental Health of GNM PDFDocument133 pagesMental Health of GNM PDFSuraj Solanki0% (1)
- Basic Principle of Electrotherapy1Document61 pagesBasic Principle of Electrotherapy1drng480% (1)
- What Is Aquatic TherapyDocument5 pagesWhat Is Aquatic TherapyHaslindaNo ratings yet
- NCP For Chronic PainDocument11 pagesNCP For Chronic PainRYAN SAPLADNo ratings yet
- Malignant 2021 480p WEB-DL x264 400MB-Pahe inDocument59 pagesMalignant 2021 480p WEB-DL x264 400MB-Pahe inBranislav IvanovicNo ratings yet
- Templates AnaDocument16 pagesTemplates AnaWilfredo DecasaNo ratings yet
- Endocrinology: Diabetes: Courses in Therapeutics and Disease State ManagementDocument59 pagesEndocrinology: Diabetes: Courses in Therapeutics and Disease State Managementnuttiya_w3294No ratings yet
- SyncopeDocument105 pagesSyncopeJohn DasNo ratings yet
- A Topical Approach To Life-Span Development Chapter 1Document51 pagesA Topical Approach To Life-Span Development Chapter 1randy100% (5)
- Sigmund Freud Essay - WordDocument9 pagesSigmund Freud Essay - Wordapi-2493113410% (1)
- HERNIIDocument4 pagesHERNIISeceleanu MarianNo ratings yet
- RobynneChutkan MicrobiomeSolutionDocument20 pagesRobynneChutkan MicrobiomeSolutionAdarsh GuptaNo ratings yet
- Drugs: What Is A Drug??Document9 pagesDrugs: What Is A Drug??Alyzza BorrasNo ratings yet
- Hall Adolescent Assessment ReportDocument3 pagesHall Adolescent Assessment Reportapi-404536886No ratings yet
- Isolation 1Document16 pagesIsolation 1Surabhi RairamNo ratings yet
- 21 Nursing ProblemDocument32 pages21 Nursing Problemjessell bonifacioNo ratings yet
- Drug Study - CaDocument3 pagesDrug Study - Casaint_ronald8No ratings yet
- New Problem StatementDocument2 pagesNew Problem Statementrenuka rathore100% (2)
- Drug Study FormatDocument2 pagesDrug Study FormatEmilie CajaNo ratings yet
- Risedronate SodiumDocument3 pagesRisedronate Sodiumapi-3797941No ratings yet
- Manajemen NyeriDocument8 pagesManajemen Nyeriagung yulisaputraNo ratings yet
- The Mental Health Review GameDocument134 pagesThe Mental Health Review Gamemeanne073No ratings yet
- Proofed - Nurs 3021 Final EvaulDocument20 pagesProofed - Nurs 3021 Final Evaulapi-313199824No ratings yet
- Neurosurgical Emergencies: Craig Goldberg, MD Chief, Division of Neurosurgery Bassett HealthcareDocument44 pagesNeurosurgical Emergencies: Craig Goldberg, MD Chief, Division of Neurosurgery Bassett HealthcareTolaniNo ratings yet
- @medicalbookpdf Preeclampsia PDFDocument286 pages@medicalbookpdf Preeclampsia PDFgalihsupanji111_2230No ratings yet
- Initial Management of Blood Glucose in Adults With Type 2 Diabetes Mellitus - UpToDateDocument24 pagesInitial Management of Blood Glucose in Adults With Type 2 Diabetes Mellitus - UpToDateJessica ArciniegasNo ratings yet
- TTSH Nursing Survival GuideDocument96 pagesTTSH Nursing Survival GuideSarip Dol100% (2)