Professional Documents
Culture Documents
(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)
Uploaded by
Aisle Malibiran PalerOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
(MID) IMMUNOSERO - Chapter 13 - Hypersensitivity (Reviewer)
Uploaded by
Aisle Malibiran PalerCopyright:
Available Formats
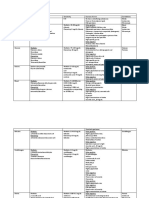
[MID] Chapter 13: Hypersensitivity
Hypersensitivity heightened state of immune responsiveness
Classification:
Immunology & Serology
C.
D.
Promoting the development of mast cells
Stimulating the overproduction of mucus
IL-4 A, C, D
Type 1 cell-bound antibody reacts with antigen to release
physiologically active substances
Type 2 free antibody reacts with antigen associated with cell
surfaces
IL-5 B
IL-9 B, C, D
IL-13 A, D
While cytokines regulate antibody synthesis, MHC genes are
responsible for the response to specific allergens.
MHC Class II molecules such as HLA-DR2, DR4, and DR7 are
associated with a high response to individual allergens.
Type 3 antibody reacts with soluble antigen to form complexes that
precipitate in the tissues
***HLA-D molecules are known to play a role in antigen presentation.
Type 4 - sensitize T cells rather than antibodies are responsible for the
symptoms that develop
People who are prone to allergies exhibit variations in the gene found
on chromosome 11q,that codes for receptor for IgE.
***Complement plays a major role in producing tissue damage in in
Types 2 and 3 reactions.
***Types 1-3 reactions are also called immediate hypersensitivity
(development of symptoms within a few minutes to a few hours)
***Type 4 reaction is also called delayed hypersensitivity (symptoms
develop within 24 to 48 hours)
TYPE 1 HYPERSENSITIVITY
Distinguishing feature = short time lag between exposure to antigens
and the onset of clinical symptoms
Langerhans and Dendritic cells internalize and process allergens
from the environment and transport the allergen-MHC class II complex
to local lymphoid tissue.
Binding of IgE to cell membranes increases the half-life of the IgE
molecule from 2 or 3 days to up at least 10 days.
-
Key reactant = IgE, which are called atopic antigens, or allergens.
-
Atopy inherited tendency to respond into naturally
occurring inhaled and ingested allergens with continue
production of IgE.
Production of large amount of IgE in response to a small
concentration of antigen is often observed in patients who exhibit
allergic or immediate hypersensitivity reactions.
Passive cutaneous anaphylaxis - a reaction that occurs when serum
is transferred from an allergic individual to a nonallergic individual, and
consequently the second individual is challenged with a specific
antigen
Triggering of Type 1 Reactions by IgE:
IgE is primarily synthesized in the lymphoid tissue of the respiratory
and gastrointestinal tracts; with normal values having a range of 150
ng/mL
Type II T helper cells (Th2) are the regulators of IgE production
Type I T Helper cells (Th1) have the function of triggering normal
immune response by the production of interferon gamma
-
Interferon gamma, as well as IL-12 and IL-18 may
suppress production of IgE.
In people with allergies, Th2 will produce IL-3, IL-4, IL-5, IL-9, and IL-
Polymorphism in the beta-chain of such receptors are linked
to atopy.
The high affinity receptors, FCE-RI receptors, bind the Fc
region of the epsilon heavy chain, and are found on
basophils and mast cells.
Once binded, IgE acts as an antigen receptor on mast cells
and basophils, and cross-linking of at least two of the
antibodies by an antigen triggers the release of mediators
from such cells.
o
Once
cross-linking
occurs,
multiple
phosphorylation reactions cause an increase in
calcium, which then promotes sysnthesis of
arachidonic acid from membrane lipids, as well as
promote cytokine synthesis.
Role of Mast Cells and Basophils:
Mast Cells are the principle effector cells of immediate
hypersensitivity. They are prominent in connective tissue, the skin, the
respiratory and the gastrointestinal tract.
-
Histamine comprises 10% of the total weight of granular
constituents, and is found in 10 times greater supply per cell
than in basophils.
Mast cell populations differ in different sites, but they all
release a variety of cytokines and other mediators that
enhance the allergic response.
Basophils represent 1 percent of the WBCs in peripheral blood, with a
half-life of about 3 days.
-
Histamine rich, and they respond to chemotactic stimulation,
and accumulate in tissues during inflammatory reactions.
Mediators Released from Granules:
Preformed Mediators:
13. Such interleukins are encoded by chromosome 5.
Functions of the Interleukins:
A.
B.
Final differentiation that occurs in B cells
Involvement in the development of eosinophils
Cross linking of surface bound IgE by a specific allergen releases
mediators from the cytoplasmic granules.
[MID] Chapter 13: Hypersensitivity
Primary or preformed mediators include:
histamine, heparin,
eosinophil chemotactic factor of anaphylaxis (ECF-A), neutrophil
chemotactic factor, and protease
-
Release of such substances accounts for the early phase
symptoms seen in allergic reactions.
The effects of histamine appear within 30 to 60 seconds, and are
dependent on activation of four different types of receptors found on
cells.
1)
2)
3)
4)
H1 receptors contraction of smooth muscles in bronchioles,
blood vessels, and the intestines, and generally induces
proinflammatory activity
H2 receptors increases gastric acid secretion, airway
mucus production, and permeability of capillaries and
venules
H3 receptors found on central and peripheral neural tissue
H4 receptors involved in immune regulation
Immunology & Serology
IL-4 = recruits T cells, basophils, eosinophils
and monocytes
IL-5 also recruits eosinophils
o
Th2 cells, mast cells, basophils, and macrophages exit the circulation
and infiltrate allergen-filled tissues.
Clinical Manifestations of Immediate Hypersensitivity:
Clinical manifestations vary from a localized skin reaction to a systemic
response known as anaphylaxis (without protection).
-
***Histamine is also responsible for local erythema or redness and
wheal and flare formation.
ECF-A attracts eosinophils to the area and induces expression of
eosinophil receptors for C3b
Tryptase cleaves kininogen to generate bradykinin, which induces
prolonged smooth muscle contraction and increases vascular
permeability and secretory activity
Anaphylaxis most severe type of allergic response
because it is an acute reaction affecting multiple organs.
o
Typically triggered by glycoproteins or large
polypeptides
o
Typical agents include venom from insects, drugs,
and foods such as shellfish, peanuts, or dairy
products
o
Latex sensitivity can also trigger anaphylaxis
o
Clinical signs begin within minutes after antigenic
challenge, and the severity of the reaction
depends on the # of previous exposures to the
antigen with consequent buildup of IgE on
mast cells and basophils
o
Massive release of reactants is responsible for the
ensuing symptoms
o
Death may occur from asphyxiation due to upper
airway edema and congestion, irreversible shock,
or a combination of such symptoms.
Newly Synthesized Mediators:
Synthesized from the breakdown of phospholipids in the cell
membrane, and are responsible for late phase allergic reactions within
6-8 hours after exposure to antigen
Newly formed mediators include: cytokines, platelet-activating
factor (PAF), prostaglandin (PG) D2, leukotrienes (LT) B4, C4, and
E4.
PGD2 is the major product of the cyclooxygenase pathway. It mimics
the effects of histamine, causing bronchial constriction and
vasodilation. It is, however, more potent than histamine, albeit being in
smaller quantities.
The symptoms depend on variables such as route of exposure,
dosage, and frequency of exposure.
Rhinitis is the most common form of atopy. Its symptoms include
paroxysmal sneezing, rhinorrhea, nasal congesting, and itching of the
nose and eyes.
Pollen, mold spores, animal dander and dust mites are examples of
airborne foreign particles that act directly on the mast cells.
Particles no longer than 2-4 um such as pollens, dust, or fumes may
cause asthma.
-
Leukotrienes result from the 5-lipoxygenase pathway of arachidonic
acid metabolism.
-
C4, D4, and E4 were also known as slow-reacting substances
of anaphylaxis (SRS-A), with LTC4 and LTD4 being 1000
times more potent than histamine
LTB4 is a potent chemotactic factor for neutrophils and
eosinophils
PAF is released by monocytes, macrophages, neutrophils, eosinophils,
mast cells and basophils. Its main function include platelet
aggregation, chemotaxis of eosinophils and neutrophils,
increased vascular permeability and contraction of smooth
muscles in the lungs and intestines
Cytokines alter the local microenvironment, leading to increase in
inflammatory cells.
-
IL-3 and IL-4 = increase IgE production
o
IL-3 = growth factor for mast cells and
basophils
Asthma
- recurrent airflow obstruction that leads to
intermittent sneezing, breathlessness, and occasionally a
cough with sputum production.
o
Often treated with a combination of therapeutic
reagents
such
as
antihistamines
and
bronchodilators
followed
by
inhaled
corticosteroids.
Food allergies is also an example of type 1 immediate hypersensitivity,
and may cause eczema, which is an itchy red skin rash.
Treatment of Immediate Hypersensitivity:
Avoidance of known allergens is the first line of defense.
Localized allergic reactions such as hay fever, hives, or rhinitis can
be treated with antihistamines and decongestants.
Hyposensitization small quantities of sensitizing antigen are
injected into the patient with the idea of building up IgG antibodies.
[MID] Chapter 13: Hypersensitivity
Use of anti-IgE monoclonal antibody in order to block sites that IgE
would normally bind to on a mast cell. The blockage can help alleviate
allergic symptoms, as mast cells cant release mediators.
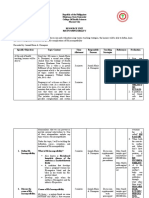
Testing for Immediate Hypersensitivity:
In vivo skin test methods are the least expensive and most specific.
There are two forms cutaneous and intradermal.
-
Cutaneous (lesser amount of antigen are used):
1. Small drop of material is injected into the skin
2. The spot is examined and the reaction is recorded after
15 minutes
o
A (+) reaction is formation of a wheal that is 3mm
greater in diameter than the negative control
(saline)
Intradermal (greater amount of antigen, more sensitive
than cutaneous):
1. Using a 1 mL tuberculin syringe, 0.01 to 0.05 mL of test
solution is administered between layers of the skin
2. After 15-20 minutes, the site is observed for erythema
and wheal formation.
a. A positive result is wheal formation of greater
than 3mm
In vitro tests involve measurement of either total IgE or antigenspecific IgE. These are less sensitive than skin tests.
-
Immunology & Serology
IgG and IgM are the two main reactants responsible
-
Complement plays a major role in Type 2 hypersensitivity.
Transfusion Reactions:
Cellular destruction that result from
heteroantigens
Interpretation of Total IgE Results:
o
Infants: Normal serum level of Ige are less than 2
kIU/L; increase up to 10 kIU/L is indicative of
allergic disease
o
After the age of 14, IgE levels in the range of 400
kIU/L are considered to be abnormally elevated.
Anti-A and Anti-B are naturally occurring antibodies, also
known as, isohemagglutinins
o
Triggered by contact with identical antigenic
determinants on microorganisms
o
Type A blood contains anti-B
o
Type B blood contains anti-A
o
Type O contains both anti-A and anti-B
A transfusion reaction occurs when a patient is given blood
for which antibodies are present, and such reactions are
dependent on the following factors:
1.
2.
3.
4.
5.
6.
Allergen-specific IgE testing is a noncompetitive solid-phase
immunoassay in which the solid phase is coated with
specific allergen and reacted with patient serum.
Microarray Testing allows for multiallergen diagnosis with a low
sample volume and a high throughput capacity.
-
Its principle is the same as noncompetitive immunoassays,
in that patient serum with possible IgE is reacted with the
microarray of allergens, and then an anti-IgE with a
fluorescent tag is added. Presence of color indicates a (+)
result.
TYPE 2 HYPERSENSITIVITY
Temp at which antibody is most active
Plasma concentration of antibody
Particular immunoglobulin class
Extent of complement activation
Density of the antigen on the RBC
Number of RBCs transfused
***It is important to detect antibodies that react at 37C
Acute hemolytic transfusion reactions may occur within minutes or
hours after receipt of incompatible blood.
-
The original commercial testing method for determining specific IgE
was known as radioallergosorbent test (RAST).
-
with
The ABO blood group is an important consideration in transfusion
reactions.
Noncompetitive solid-phase immunoassay, antihuman
igE is bound to a solid phase such as cellulose, a paper disk,
or a microtiter well.
o
Patient serum is added and allowed to react, and
then a labeled anti-igE is added to detect the
bound patient IgE.
Total serum IgE is used as a screening test, as well as aiding
in diagnosis of allergic rhinitis, asthma, or other allergic
conditions.
antibody combining
The major groups involved with transfusion reactions include the ABO,
Rh, Kell, Duffy, and Kidd systems.
The Competitive radioimmunosorbent test (RIST) uses
radiolabeled IgE to compete with patient igE for binding sites
on a solid phase coated with anti-igE.
Triggered by altered self-antigens and heteroantigens,
found on cell surfaces.
Promotes phagocytosis and activation of complement
Reactions that begin immediately are most often associated
with ABO blood group incompatibilities.
Intravascular hemolysis occurs after antigen is introduced to
the patient, due to complement activation
Delayed hemolytic reactions occur within the first 2 weeks
following a transfusion, and are caused by a secondary
response to the antigen
o
IgG is the antibody present
o
Rh, Kell, Duffy, and Kidd blood groups are most
associated with this type of reaction.
o
Intravascular hemolysis does not occur, as IgG is
not efficient in activating the complement
system.
Hemolytic Disease of the Newborn
Appears in infants whose mothers have been exposed to blood-group
antigens on the babys cells that differ from their own
-
As a result, IgG production starts, which destroy fetal red
cells.
Erythroblastosis fetalis severe HDN in which D antigen is the most
common antigen involved
[MID] Chapter 13: Hypersensitivity
-
Immunology & Serology
Treatment involves an exchange transfusion to replace
antibody-coated red cells.
HDN due to ABO compatibility is milder, as IgM antibodies are formed,
which cannot cross the placenta.
Exposure occurs during the birth process, due to fetal cells leak in the
mothers circulation.
-
First child is usually unaffected.
Later children, however, are susceptible due to an
anamnestic response
The extent of the first bleeding influences the amount of
antibodies formed.
o
If enough, memory B-cells develop, which then
mature to IgG to cross the placenta
o
The amount of antibodies formed affects the
childs mortality or its likelihood of developing a
disease.
Kernicterus can occur if there is bilirubin build up
Screening of pregnant women can prevent the consequences of HDN.
Antibody reaction with basement membrane, and the
glomeruli, as well as the pulmonary alveolar membranes
are affected
o
Complement cascade occurs in the two areas, and
inflammation occurs
o
Treatment = corticosteroids
Testing for Type 2 Hypersensitivity:
Direct antiglobulin testing (DAT) performed to detect transfusion
reactions, hemolytic disease of the newborn, and autoimmune
hemolytic anemia
Polyspecific antihuman globulin (mixture of antibodies to IgG and
complement components) initial testing
Indirect Coombs test crossmatching of blood to prevent
transfusion reaction
TYPE 3 HYPERSENSITIVITY
Autoimmune Hemolytic Anemia:
IgM and IgG are the main antibodies involved, however, unlike in Type
2 hypesensitivity, the antigen is soluble.
Type 2 hypersensitivity reaction directed against self-antigens, due to
the production of antibodies to an individuals own RBC.
Complexes that precipitate out of the serum are formed when soluble
antigen combines with antibody
Two groups:
antibodies
Warm
reactive
antibodies
and
Cold
reactive
Warm autoimmune hemolytic anemia accounts for 70% of
autoimmune anemia.
-
Characterized by formation of IgG antibody, which react
strongly at 37C.
May or may not be associated with other diseases
Underlying cause of antibody production is unknown and is
referred to as idiopathic autoimmune hemolytic anemia.
Symptoms of anemia as a result of clarance of antibody
coated RBCs by the liver and spleen
Hemolysis is extravascular
Treated with corticosteroids or splenectomy
Cold autoagglutinins less frequent, found in people in their fifties
and sixties
-
Triggered by antigens on microorganism, as antibodies
form following Mycoplasma pneumonia and infectious
mononucleosis
Antibodies belong to the IgM class and are specific for Ii
blood groups
Reactions are seen only if the individual is exposed to the
cold, and temp of circulation falls below 30C
If complement is activated, intravascular hemolysis occurs
Treatment = keeping the patient warm
Type 2 Reactions Involving Tissue Antigens:
Some type 2 reaction involve destruction of tissues because of
combination with antibody
Goodpastures syndrome an example of an organ specific
autoimmune disease in which antibody is directed against a particular
tissue.
If complexes arent phagocytized, they deposit in the
tissues and bind complement, causing damage
Excess antigen sites on antibody molecules become
filled before cross-linking occurs
Excess antibody no lattice formation
Precipitating complexes occur in mild antigen excess, and
are most likely to deposit in the tissues.
Complement binds to the complexes in the tissues causing the release
of mediators.
If target cells are large, and are unaffected by phagocytosis, granule
and lysosome contents are release by exocytosis
Long-term changes include loss of tissue elements that cannot be
regenerated.
Arthur Reaction:
Localized type 3 reaction characterized by erythema and edema,
which peaks within 3-8 hours, and is followed by a hemorrhagic
necrotic lesion that may ulcerate.
-
Caused by antigen-antibody combination, and formation
of complexes that deposit in small dermal blood vessels
Complement is fixed, attracting neutrophils and causing
aggregation of platelets.
o
Neutrophils release free radicals and proteolytic
enzymes
Activation of complement is essential for such reaction to
occur.
Serum Sickness:
[MID] Chapter 13: Hypersensitivity
Result from passive immunization with animal serum, usually a horse
or bovine, used to treat infections like diphtheria, tetanus, and
gangrene
-
Symptoms (heache, nausea, fever, joint pain etc.) occur 721 days after injection of the animal serum, and recovery
takes between 7 and 30 days
In this disease, the sensitizing and the shocking dose of
antigen are one and the same, because antibodies develop
while antigen is still present
o
High levels of antibody form immune complexes
that deposit in the tissues.
Autoimmune Disease:
Autoimmune diseases that fall into type 3 hypersensitivity reactions
include:
1)
2)
Systemic lupus erythematous antibodies are directed
against constituents such as DNA and nucleohistones.
a. Complex deposition involves multiple organs, but
the main damage occurs at the glomerular
basement membrane of the kidney
Rheumatoid arthritis rheumatoid factor, an antibody, is
directed against IgG.
a. Complex deposition occurs in the membranes of
joints.
Testing for Type 3 Hypersensitivity:
Agglutination reactions detects SLE and rheumatoid arthritis
Fluorescent staining of tissue sections determine deposition of
immune complexes
Measuring complement levels general method determining
immune complex diseases
TYPE 4 HYPERSENSITIVITY
Differs from the other three types of hypersensitivity in that sensitized
T cells, usually a subpopulation of Th1 cells, play the major role in its
manifestations.
***Antibody and complement are not directly involved
Sensitization phase of 1-2 weeks, and symptoms occur several after
subsequent exposure, and peak at 48-72 hours
Immunology & Serology
Reactions are usually due to low-molecular weight compounds that
touch the skin
Most common causes include: poison ivy, poison oak, and poison
sumac
Other common compounds: nickel, rubber, formaldehyde, hair dyes;
cosmetics; antiseptics and antibiotics; latex
Most of the aforementioned substances are haptens that bind to
proteins on skin cells
The Langerhans cell act as the antigen-presenting cell, which migrate
to regional lymph nodes and generate sensitized Th1 cells.
After repeat exposure, cytokine production causes macrophages to
accumulate, and a skin eruption characterized by erythema, swelling,
and formation of papules appear between 6 hours to several days after
exposure.
Dermatitis is initially limited to skin sites exposed to the antigen, but
then it spreads out to adjoining areas. It can last for 3-4 weeks until
antigen has been removed
-
Hypersensitivity Pneumonitis:
Mediated predominantly by sensitized T-lymphocytes that respond to
inhaled allergens. IgG & IgM play a minor role.
It is an allergic disease of the lung parenchyma, characterized by
inflammation of the alveoli and interstitial spaces and is caused by
inhalation of a variety of antigens
The reaction is most likely due to microorganisms, especially bacterial
and fungal spores.
Symptoms include: dry cough, shortness of breath, fever, chills
Alveolar macrophages and lymphocytes trigger a chronic condition
characterized by interstitial fibrosis with alveolar inflammation.
Tuberculin-Type Hypersensitivity:
Testing for exposure to tuberculosis is based on the principle that
soluble antigens from M. tuberculosis induce a reaction in people who
have or have had tuberculosis.
-
Transferred only through the transfer of T-lymphocytes.
Langerhans cells and macrophages capture and present the antigen to
T helper cells of the Th1 subclass, and once activated, the Th1 cells
release cytokines, which recruit macrophages and neutrophils
-
Cytotoxic T cells are also recruited and they bind with
antigen-coated target cells to cause tissue destruction
Allergic skin reactions to bacteria, viruses, fungi and environmental
antigens like poison ivy are examples of this reaction.
Systemic corticosteroids can be used to treat dermatitis
Previously sensitized individuals develop an area of
erythema on the injection sites as a result of T-lymphocytes
and macrophages into the area
Tuberculin skin test use of M. tuberculosis antigen prepared by a
purified filtrate from the cell wall of the organism.
-
The Purified Protein Derivative is injected under the skin
and the reaction is read 48 -72 hours later
o
Positive result indicates that the individual has
been exposed to the bacteria.
Contact Dermatitis:
Testing for Delayed Hypersensitivity:
[MID] Chapter 13: Hypersensitivity
Patch Test gold standard in testing for contact dermatitis
-
Positive result = redness with papules or tiny blisters
Mantoux Method Used for testing Candida albicans, tetanus
toxoid, tuberculin, and fungal antigens.
-
Performed in the same manner as testing for the presence of
IgE
o
Antigen is injected intradermally, and the test site
is read at 48 and 72 hours for the presence of
induration
Immunology & Serology
o
Positive result = >5mm of induration
You might also like
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Vitamin B12 and FolateDocument12 pagesVitamin B12 and FolateAllessandria DimaggioNo ratings yet
- Common Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Document2 pagesCommon Plating Media For Clinical Bacteriology (From Bailey & Scott's Diagnostic Microbiology, 12th Ed)Elizabeth Enjambre HernaniNo ratings yet
- Bacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitDocument3 pagesBacteriostatic Agents: Drugs Which Bind To The 50s Ribosomal UnitJoshua TrinidadNo ratings yet
- COMPLETE BLOOD COUNT Lecture GuideDocument9 pagesCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaNo ratings yet
- Joshua Ty Cayetano 3DMT #15: A B C A B B B A ADocument4 pagesJoshua Ty Cayetano 3DMT #15: A B C A B B B A AJoshua Ty CayetanoNo ratings yet
- My CologyDocument25 pagesMy CologyPlasma CarwashNo ratings yet
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 pagesDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaNo ratings yet
- AUBF Finals Vaginal SecretionsDocument37 pagesAUBF Finals Vaginal SecretionsLyra Dennise LlidoNo ratings yet
- Immunology and Serology ReviewDocument30 pagesImmunology and Serology ReviewEuliz G.100% (1)
- AUBF P1 Examination Questions (1-8Document39 pagesAUBF P1 Examination Questions (1-8Charmaine BoloNo ratings yet
- Clinical Microscopy ReviewerDocument7 pagesClinical Microscopy ReviewerDayledaniel SorvetoNo ratings yet
- Serological TestsDocument2 pagesSerological TestsKimberly EspaldonNo ratings yet
- 2.13.08 Cold Agglutinin RogersDocument27 pages2.13.08 Cold Agglutinin RogersJessica StewartNo ratings yet
- Compre-Quiz For MedtechDocument18 pagesCompre-Quiz For MedtechynaellyNo ratings yet
- Pancreatic Enzymes Help Digest CarbsDocument7 pagesPancreatic Enzymes Help Digest CarbsAngelaAmmcoNo ratings yet
- Physical Examination of UrineDocument4 pagesPhysical Examination of UrineIceNo ratings yet
- ISBB Aaaaa PDFDocument55 pagesISBB Aaaaa PDFSelena de LimaNo ratings yet
- Parasitology ReviewersDocument9 pagesParasitology ReviewersLouije MombzNo ratings yet
- IS Lab Quizzes ReviewerDocument15 pagesIS Lab Quizzes ReviewerMarie MontemarNo ratings yet
- Hematology 2 Lecture Notes Platelet Qualitative DisordersDocument4 pagesHematology 2 Lecture Notes Platelet Qualitative DisorderscccomayogNo ratings yet
- Immunology & Serology Week 1Document2 pagesImmunology & Serology Week 1Romie SolacitoNo ratings yet
- ChlamydiaDocument45 pagesChlamydiaCesar Toribio GamuzoNo ratings yet
- Molbio HandoutDocument29 pagesMolbio HandoutHazel FlorentinoNo ratings yet
- Shifting Exams Reviewer For MEDTECH in ParasitologyDocument12 pagesShifting Exams Reviewer For MEDTECH in ParasitologyIwa RohasNo ratings yet
- ParasitologyLec 3 Nematodes 2 PDFDocument6 pagesParasitologyLec 3 Nematodes 2 PDFDJ RelojNo ratings yet
- MICROBIOLOGY MEDIADocument3 pagesMICROBIOLOGY MEDIAAisle Malibiran PalerNo ratings yet
- Blood Banking Course BookDocument2 pagesBlood Banking Course BookShukr Wesman BlbasNo ratings yet
- Gram Negative Cocci (Lecture Notes)Document5 pagesGram Negative Cocci (Lecture Notes)Dayledaniel Sorveto100% (1)
- Non-Fermenting and Miscellaneous Gram Negative BacilliDocument33 pagesNon-Fermenting and Miscellaneous Gram Negative BacilliLin Sison Vitug100% (1)
- Gram-Negative Rods in Gut FloraDocument2 pagesGram-Negative Rods in Gut FloraJohn TerryNo ratings yet
- Enzymes: Concentration, Kinetics, Classification, AssaysDocument13 pagesEnzymes: Concentration, Kinetics, Classification, AssaysAedren TrillanaNo ratings yet
- Anti-Anemia and Hematopoietic Growth FactorsDocument8 pagesAnti-Anemia and Hematopoietic Growth FactorsIsabel CastilloNo ratings yet
- Chapter15 StreptococciDocument66 pagesChapter15 StreptococciNursheda Abangon AzisNo ratings yet
- Subcutaneous & Systemic MycosesDocument7 pagesSubcutaneous & Systemic MycosesDee GeeNo ratings yet
- Student Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentDocument5 pagesStudent Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentMelody PardilloNo ratings yet
- AnemiaDocument9 pagesAnemiaMila Canoza HerreraNo ratings yet
- Vibrio & Aeromonas & PlesiomonasDocument48 pagesVibrio & Aeromonas & PlesiomonasOscar PeñaNo ratings yet
- ISBB Immunology ReviewDocument9 pagesISBB Immunology ReviewNathan DrakeNo ratings yet
- CCII 8.0 - Clinical EnzymologyDocument2 pagesCCII 8.0 - Clinical EnzymologyWynlor AbarcaNo ratings yet
- Summary of Reagent Strip TestsDocument8 pagesSummary of Reagent Strip TestsDarla YsavelNo ratings yet
- A. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)Document19 pagesA. B. C. A. B. C. D.: Clinical Chemistry II - Prelims (Bandala)IceNo ratings yet
- HaradamoriDocument2 pagesHaradamorinicole castillo100% (1)
- Clinical Microscopy (Fecalysis)Document2 pagesClinical Microscopy (Fecalysis)Sheng Ramos AglugubNo ratings yet
- Chemical Examination of UrineDocument6 pagesChemical Examination of UrinehermanskyNo ratings yet
- MAJOR HISTOCOMPATIBILITY COMPLEX Part 1'Document3 pagesMAJOR HISTOCOMPATIBILITY COMPLEX Part 1'Renzo SalasNo ratings yet
- Cc1-Task 4Document8 pagesCc1-Task 4Joshua TrinidadNo ratings yet
- Blood Group Systems ISBTDocument25 pagesBlood Group Systems ISBTkusumahpratiwi100% (1)
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterDocument4 pagesLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoNo ratings yet
- Immunology & Serology: Preliminaries: Romie Solacito, MLS3CDocument12 pagesImmunology & Serology: Preliminaries: Romie Solacito, MLS3CRomie Solacito100% (2)
- AUB - Renal DiseasesDocument2 pagesAUB - Renal DiseasesJeanne RodiñoNo ratings yet
- Mtap - Virology NotesDocument7 pagesMtap - Virology NotesMoira Pauline LibroraniaNo ratings yet
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocument14 pages1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaNo ratings yet
- Lab Evaluation of PlateletsDocument5 pagesLab Evaluation of PlateletsDennis ValdezNo ratings yet
- MT Laws and Lab ManDocument8 pagesMT Laws and Lab ManGene Narune GaronitaNo ratings yet
- Top 20 Blood Banking ConceptsDocument16 pagesTop 20 Blood Banking ConceptsM CNo ratings yet
- CC Blood CollectionDocument3 pagesCC Blood Collectionlcrujido100% (1)
- Type 1 HypersensitivityDocument38 pagesType 1 Hypersensitivitychocoholic potchiNo ratings yet
- Type I Hypersensitivity: Understanding Allergic ReactionsDocument48 pagesType I Hypersensitivity: Understanding Allergic Reactionsrido rahmad saputraNo ratings yet
- Genpath Midterms1Document3 pagesGenpath Midterms1Aisle Malibiran PalerNo ratings yet
- 2nd Sem - ImmunoSero - Introduction and Natural ImmunityDocument5 pages2nd Sem - ImmunoSero - Introduction and Natural ImmunityAisle Malibiran PalerNo ratings yet
- Pharma NotesDocument4 pagesPharma NotesAisle Malibiran PalerNo ratings yet
- Bacteriology LectureDocument38 pagesBacteriology LectureAisle Malibiran Paler100% (1)
- (MT-RES) Peer Evaluation (New)Document1 page(MT-RES) Peer Evaluation (New)Aisle Malibiran PalerNo ratings yet
- Digestive System Histology GuideDocument5 pagesDigestive System Histology GuideAisle Malibiran PalerNo ratings yet
- (MID) IMMUNOSERO - Chapter 10 - Labeled ImmunoassaysDocument4 pages(MID) IMMUNOSERO - Chapter 10 - Labeled ImmunoassaysAisle Malibiran PalerNo ratings yet
- 2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyDocument3 pages2nd Sem - Hema1 - An Overview of Clinical Laboratory HematologyAisle Malibiran PalerNo ratings yet
- Medical Research Manuscript Evaluation ToolDocument5 pagesMedical Research Manuscript Evaluation ToolAisle Malibiran PalerNo ratings yet
- Bacte Chapt. 16Document4 pagesBacte Chapt. 16Aisle Malibiran PalerNo ratings yet
- Bacte Chapt. 16Document4 pagesBacte Chapt. 16Aisle Malibiran PalerNo ratings yet
- Research ProtocolDocument1 pageResearch ProtocolAisle Malibiran PalerNo ratings yet
- Chapter21 (Acinetobacter, Stenotrophomonas and Similar OrganismsDocument3 pagesChapter21 (Acinetobacter, Stenotrophomonas and Similar OrganismsAisle Malibiran PalerNo ratings yet
- Urinary System - LabDocument1 pageUrinary System - LabAisle Malibiran PalerNo ratings yet
- 1 - Overview of ComputersDocument99 pages1 - Overview of ComputersAisle Malibiran PalerNo ratings yet
- Ra8504 - Aids LawDocument8 pagesRa8504 - Aids LawEnna TrivilegioNo ratings yet
- Carlos Romulo's I am Filipino Essay Theme Learning Past MistakesDocument1 pageCarlos Romulo's I am Filipino Essay Theme Learning Past MistakesAisle Malibiran PalerNo ratings yet
- MICROBIOLOGY MEDIADocument3 pagesMICROBIOLOGY MEDIAAisle Malibiran PalerNo ratings yet
- 1987 Philippine ConstitutionDocument1 page1987 Philippine ConstitutionAisle Malibiran PalerNo ratings yet
- Carlos Romulo's I am Filipino Essay Theme Learning Past MistakesDocument1 pageCarlos Romulo's I am Filipino Essay Theme Learning Past MistakesAisle Malibiran PalerNo ratings yet
- Paler, Aisle M. MT12221: Sonnet 144Document1 pagePaler, Aisle M. MT12221: Sonnet 144Aisle Malibiran PalerNo ratings yet
- Secrets of The New ManilaDocument1 pageSecrets of The New ManilaAisle Malibiran PalerNo ratings yet
- Growth Hormone, Insulin-like Growth Factor 1 (IGF-1), and their Roles in Growth and MetabolismDocument4 pagesGrowth Hormone, Insulin-like Growth Factor 1 (IGF-1), and their Roles in Growth and MetabolismAisle Malibiran PalerNo ratings yet
- HistoryDocument1 pageHistoryAisle Malibiran PalerNo ratings yet
- Description of The BarangayDocument1 pageDescription of The BarangayAisle Malibiran PalerNo ratings yet
- FootnotesDocument6 pagesFootnotesAisle Malibiran PalerNo ratings yet
- Public Health Bylaws Under The Community CharterDocument9 pagesPublic Health Bylaws Under The Community CharterAisle Malibiran PalerNo ratings yet
- Why Cysteine Is SpecialDocument3 pagesWhy Cysteine Is SpecialAisle Malibiran PalerNo ratings yet
- InsulinDocument10 pagesInsulinAisle Malibiran PalerNo ratings yet
- Advanced Neonatal Resuscitation ProceduresDocument14 pagesAdvanced Neonatal Resuscitation ProceduresSanthosh.S.U100% (1)
- Kamara - Factors Associated With Neonatal Hyperbilirubinemia in The First 2weeks of Life in OlaDocument56 pagesKamara - Factors Associated With Neonatal Hyperbilirubinemia in The First 2weeks of Life in OlaJulia StantonNo ratings yet
- Antihuman Globulin Testing - BOOKDocument12 pagesAntihuman Globulin Testing - BOOKANNE CZARINA RAMIELLE DE VILLANo ratings yet
- Heme Synthesis Breakdown HBDocument18 pagesHeme Synthesis Breakdown HBDr.P.NatarajanNo ratings yet
- BiliDocument63 pagesBiliFu Xiao ShanNo ratings yet
- Forum Anthro OPT 2022 Test 8Document19 pagesForum Anthro OPT 2022 Test 8Rimita SahaNo ratings yet
- Module 6 Student Activity SheetDocument7 pagesModule 6 Student Activity SheetJenny Agustin FabrosNo ratings yet
- Compre-5-Supplementary-Lecture 3Document32 pagesCompre-5-Supplementary-Lecture 3Aubrey Jane TagolinoNo ratings yet
- Hellp SyndromeDocument5 pagesHellp SyndromeJmarie Brillantes PopiocoNo ratings yet
- Feline Neonatal IsoerythrolysisDocument18 pagesFeline Neonatal IsoerythrolysisPaunas JoshiNo ratings yet
- Forensic Notes PDFDocument155 pagesForensic Notes PDFSoni Mahendran100% (1)
- Lab Guide: Health Department, HQ AmmanDocument104 pagesLab Guide: Health Department, HQ AmmanNanik AndianiNo ratings yet
- Totalbili Arc ChemDocument8 pagesTotalbili Arc ChemTanveerNo ratings yet
- Imh200s Study Guide Student Lecturer Contract and Lesson Plan 2023Document9 pagesImh200s Study Guide Student Lecturer Contract and Lesson Plan 2023dimphoNo ratings yet
- Hemolytic Disease of NewbornDocument15 pagesHemolytic Disease of Newborncyphochilus100% (1)
- Blood Typing PDFDocument3 pagesBlood Typing PDFFrances Lau Yee ChinNo ratings yet
- Pediatric Nursing NotesDocument12 pagesPediatric Nursing NotesFreeNursingNotes63% (16)
- MLT Blood Bank Exam 2 FullDocument4 pagesMLT Blood Bank Exam 2 Fullkasdf gre bbtNo ratings yet
- Maternal Board Anticipated Close Door Coaching Nle Nov 2023Document10 pagesMaternal Board Anticipated Close Door Coaching Nle Nov 2023Sophian D. DalumaNo ratings yet
- ABO and Rh DiscrepanciesDocument4 pagesABO and Rh DiscrepanciesnicholeNo ratings yet
- Hemolytic Disease of The Fetus and NewbornDocument6 pagesHemolytic Disease of The Fetus and NewbornCj CCNo ratings yet
- Pregnancy Changes and Comfort MeasuresDocument6 pagesPregnancy Changes and Comfort MeasuresGian Carlo de Jesus100% (1)
- Pediatric S: The Journal ofDocument9 pagesPediatric S: The Journal ofFandi ArgiansyaNo ratings yet
- Immunohematology-Lab MidtermsDocument9 pagesImmunohematology-Lab MidtermsRachel PlanillaNo ratings yet
- Herreria, Hannah U. BSN 2 N038Document2 pagesHerreria, Hannah U. BSN 2 N038Hannah Urmeneta HerreriaNo ratings yet
- ABO-RH IncompatiilityDocument6 pagesABO-RH IncompatiilitymarisonaningatNo ratings yet
- Best Blood Group Compatibility For MarriageDocument14 pagesBest Blood Group Compatibility For MarriageTewodros Kassa Ye EtalemahuNo ratings yet
- The RH FactorDocument19 pagesThe RH Factorlisa100% (1)
- Seeley's Ess9e.chapt11 - Lecture.aDocument43 pagesSeeley's Ess9e.chapt11 - Lecture.aJhara100% (1)
- RH Incompatibility Resource UnitDocument6 pagesRH Incompatibility Resource UnitJannah Marie A. DimaporoNo ratings yet