Professional Documents
Culture Documents
Vital Information
Uploaded by
letz_90Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Vital Information
Uploaded by
letz_90Copyright:
Available Formats
I.
Vital Information
Client’s Name: Mr. M.G.
Age: 45 yrs. Old
Sex: Male
Weight: 78 kgs
Height: 5’7
Civil Status: Married
Religion: LDS
Nationality: Filipino
Birthplace: Busan, South Korea
Birthday: 05/06/1964
Current Address: Molo, I.C. Iloilo city
Educational attainment: BSME CPU
Occupation: Drilling Engineer
Chief complaints: Right Flank pain
Date and time of admission to ER: January 10, 2010, 7:29am
Manner of admission to the ER: Ambulatory
Accompanied by whom: Mrs. C.G (wife)
Mental/Emotional status upon admission: conscious, alert, oriented, cooperative and
understanding
Admission Vital Signs:
Temperature: 36.8degree celsius
Pulse rate: 89beats/min
Respiratory rate: 22breaths/min
Blood pressure: 140/90 mmHg
Impression/Medical Diagnosis:
T/C Urolithiasis Right. DM2, Deplipidemia
S/P ARF stage 2 to pre-renal azotenia stage 2 to severe DHN (2005)
S/P HDx4 (2005)
Attending Physicians: Dr. C and Dr. M
Number of previous hospitalizations: 1 – year 2005 because of renal failure
Food/drug allergy: Aspirin
Source of information: Patient – Primary
Person to be contacted incase of emergency: Mrs. C.G.
Contact number: 09194486282
II. History of present Illness
Last January 8, 2010 at around 4pm in the afternoon patient felt slight gnawing pain in
his right flank area rated as 3 base on the pain rating scale, the pain was tolerable and was felt by
the client in their house at Molo, I.C. Ilo-ilo city. Patient verbalize that he doesn’t know of any
aggravating or alleviating factors that could contribute to his pain. As said by the patient there
were no remedies, medications or treatment being utilize to relief the pain he just endure it and
hoping that it will be gone by the next day with some rest and sleep. On the last January 10, 2010
at around 3am in the morning client felt severe gnawing pain in his right flank area rated as 9.
Clients then decided to be admitted and upon arrival to the ER the following laboratory were
ordered as follows: Chest X-ray PA view, IS-APL Xray, FPS, UA, iP and Ultrasound of KUB.
Treatments were CBG-TID and Buscopan 1amp 26H for flank pain. Medications were as
follows: Metforfin – Glucophage, Forte 850mg 1tab (Breakfast and dinner), Acarbose –
Glucobay 100mg 1tab TID, Droglitazone – Prialta 15mg 1tab OD before dinner, Atorvastatin –
Lipitor 20mg 1tab OD, and Fenofiltrate – Tipantyl 200mg 1tab OD. An IV was attached to the
client’s right radial vein PNSS 1Lx100cc/hr and was then transferred to Sacred Heart Unit via
wheel chair accompanied by Mrs. C.G and received by staff nurse and assigned to room 234 as
the client’s room of choice.
III. Past Medical History
The patient claimed that he was in good state of health prior to illness. The immunization
that the client can remember is BCG and polio that was taken but the patient claimed that he had
completed his immunizations. There was one previous hospitalization last year 2005 because of
renal failure and there were no history of accidents/falls or any injuries and no psychiatric illness
IV. Current Health Status
As verbalize by the patient he does not smoke, or take any illegal drugs and occasionally
drinks with only 1 beer and started drinking during his high school days. Client has good appetite
and can consume 100% of his meal; client usually eats vegetables, meat, fish, and rice and also
drinks 2-3 glasses of water per day. Has no bladder/bowel incontinence or difficulty during
bowel movement/urination. Patient’s goes to gym or cycling 3 times a month as form of exercise
and sleeps in supine position with two pillows one on his head and one that he is holding while
sleeping. Usually sleeps 10pm in the evening and wakes up 7am in the morning. The medication
that the client is currently taking is the maintenance medication for his Diabetes Mellitus.
V. Family History
The family of the patient is compose with Him Mr. M.G – 45 yrs. Old, Mrs. C.G – 44 yrs.
Old, Ms. S.G – 20 yrs. Old, Ms. Z.G – 18 yrs. Old, Ms. M.G – 3 yrs. Old. The rest of the family
member is in good health condition. The father of the client died at the age of 69 because of heart
attack and his mother died at the age of 44 because of breast cancer and his brother Mr. R.G died
at the age of 24 because of heart attack. As said by the client his grandmother had Diabetes
mellitus and there were no existence of rare genetic conditions.
VI. Personal History
As claimed by the patient he lived in an urban area and there were no environmental
hazards in their home that could contribute to his present illness or can trigger an illness
response. The patient has no problem in performing activities of daily living such as bathing,
dressing, cooking and eating. The patient has a good relationship with his family and he is the
one who makes the final decision in terms of decision making. The family is independent in
terms of support system in times of needs and also in financial situation as verbalized by the
patient. The monthly income of the patient is 200,000php and according to the patient it is
enough to support the basic needs of the family. The patient claimed has a good relationship
toward his wife.
You might also like
- Module1 Lesson 1Document22 pagesModule1 Lesson 1ARLENE NORICONo ratings yet
- Pretest Quarter 3Document1 pagePretest Quarter 3Leizette Zuniga TacangNo ratings yet
- Application of Proper DrapingDocument9 pagesApplication of Proper DrapingNovelyn Ganela50% (2)
- Powerpoint TesdaDocument21 pagesPowerpoint TesdaNarie Pinon-BanaNo ratings yet
- Task Sheet 2.2-2 Taking Vital SignsDocument2 pagesTask Sheet 2.2-2 Taking Vital SignshanniemaelimonNo ratings yet
- Unit 1 Introduction To CookeryDocument7 pagesUnit 1 Introduction To CookeryRavi BhollahNo ratings yet
- Tve 12 - Beauty Care 1ST Semester Finals Module 2 (Dela Cruz)Document11 pagesTve 12 - Beauty Care 1ST Semester Finals Module 2 (Dela Cruz)Aneza Jane Juanes100% (2)
- Family Case Week 3Document25 pagesFamily Case Week 3Luiezt BernardoNo ratings yet
- Assessor'S Script: Conducting Competency AssessmentDocument14 pagesAssessor'S Script: Conducting Competency AssessmentWilmer100% (1)
- TLE-Q3 LasDocument18 pagesTLE-Q3 LasHelena CaballeroNo ratings yet
- SHD Form 1 Etc Aug 7Document8 pagesSHD Form 1 Etc Aug 7ROLANDO SOLONNo ratings yet
- Competency Based Learning MaterialDocument22 pagesCompetency Based Learning MaterialCresly PinedaNo ratings yet
- LESSON 7.1:: Maintain A Healthy and Safe EnvironmentDocument71 pagesLESSON 7.1:: Maintain A Healthy and Safe EnvironmenthanniemaelimonNo ratings yet
- Bread and Pastry Quarter 3 Week 6: CustardDocument5 pagesBread and Pastry Quarter 3 Week 6: CustardMean MirafuentesNo ratings yet
- Laws On ElderlyDocument8 pagesLaws On ElderlySoleil MaxwellNo ratings yet
- Grade 10 Tle 4TH Monthly ExamDocument4 pagesGrade 10 Tle 4TH Monthly ExamJovelyn Takilid0% (1)
- Kitchen Safety and Sanitation PowerPoint - 1Document15 pagesKitchen Safety and Sanitation PowerPoint - 1EgaSuharnoNo ratings yet
- GROUP 5 Maintaining High Standards of Client ServicesDocument30 pagesGROUP 5 Maintaining High Standards of Client ServicesGraziela Calam GutierrezNo ratings yet
- NCM 107 - MCN I Michelle E. Flores, RN ManDocument62 pagesNCM 107 - MCN I Michelle E. Flores, RN ManAko Si Christian100% (1)
- Ossining Children's Center CampaignDocument18 pagesOssining Children's Center CampaignDon HeymannNo ratings yet
- Quarter 1 Perform Hand SpaDocument10 pagesQuarter 1 Perform Hand SpaDrexler LabagalaNo ratings yet
- CG Preparing Hot and Cold MealsDocument67 pagesCG Preparing Hot and Cold MealsBanoyJellie CañeteNo ratings yet
- Module 4 Bread and PastryDocument3 pagesModule 4 Bread and PastryMagelyn NBNo ratings yet
- Family Survey ToolmiriamDocument9 pagesFamily Survey ToolmiriamMushy_ayaNo ratings yet
- Role of The Youth On Drug Detection and PreventionDocument1 pageRole of The Youth On Drug Detection and PreventionpotaotNo ratings yet
- Caregiver ResumeDocument4 pagesCaregiver ResumeEric Antolijao100% (7)
- NCM 101Document2 pagesNCM 101Ianne Sandra Sorrosa100% (1)
- K To 12 Commercial Cooking Learning ModuleDocument98 pagesK To 12 Commercial Cooking Learning ModulePilarica Lotho ManejaNo ratings yet
- Sdoquezon Adm JHS9 Tle BPP M2Document29 pagesSdoquezon Adm JHS9 Tle BPP M2Rey Mark OrdillanoNo ratings yet
- Caregivi NG: Explorato Ry CourseDocument8 pagesCaregivi NG: Explorato Ry CourseClarisseJoy LobendinoNo ratings yet
- Module 1 FinalsDocument7 pagesModule 1 FinalsLemuel AyingNo ratings yet
- LM - Cookery G10Document363 pagesLM - Cookery G10gleezel anneNo ratings yet
- Ethnic Cooking in The PhilippinesDocument3 pagesEthnic Cooking in The PhilippinesAngeli Merced100% (1)
- Hilot PPT 1 4th QuarterDocument11 pagesHilot PPT 1 4th Quarterann AngelesNo ratings yet
- 2nd Quarter Food ProcessingDocument3 pages2nd Quarter Food ProcessingJeziel Gapor100% (1)
- Concept of Healthy Community 1Document43 pagesConcept of Healthy Community 1Rose AnnNo ratings yet
- Bread and Pastry Production: Technology and Livelihood EducationDocument28 pagesBread and Pastry Production: Technology and Livelihood Educationkarl elordeNo ratings yet
- HilotDocument2 pagesHilotRodel Agapito100% (2)
- Composition and Nutritional Value of Eggs and MilkDocument27 pagesComposition and Nutritional Value of Eggs and MilkaqsaNo ratings yet
- Trompang ElepanteDocument3 pagesTrompang ElepanteAivee SisonNo ratings yet
- CBLM OhsDocument84 pagesCBLM OhsMarwin NavarreteNo ratings yet
- Deworming BlankDocument1 pageDeworming BlankLov EllaNo ratings yet
- Activity Worksheet 1 10Document33 pagesActivity Worksheet 1 10Jennifer Faji-MangaNo ratings yet
- I. MULTIPLE CHOICE: Choose The Letter of The Correct Answer. Use The Answer Sheet ProvidedDocument2 pagesI. MULTIPLE CHOICE: Choose The Letter of The Correct Answer. Use The Answer Sheet ProvidedayensantosNo ratings yet
- Input ! Let Us Explore!Document3 pagesInput ! Let Us Explore!Maxicris SlowerNo ratings yet
- Task SheetDocument4 pagesTask SheetJussa Leilady AlberbaNo ratings yet
- CBLM 2 Week 1Document16 pagesCBLM 2 Week 1Joanne Cristie TolopiaNo ratings yet
- CAREGIVING LAS 5 and 6Document17 pagesCAREGIVING LAS 5 and 6Florame OñateNo ratings yet
- Study Caregiving in PhilippinesDocument7 pagesStudy Caregiving in PhilippinesCleverlearn CebuNo ratings yet
- Hairdressing SummativeDocument3 pagesHairdressing SummativeMelanie Marquez - FernandezNo ratings yet
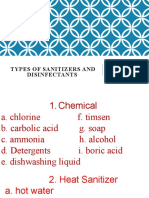
- Types of Sanitizers and DisinfectantsDocument17 pagesTypes of Sanitizers and DisinfectantsJaideHizoleSapulNo ratings yet
- Sim-Bpp History of Baking1Document15 pagesSim-Bpp History of Baking1Lea Galano ManarpaacNo ratings yet
- Self-Assessment Guide (Full Qualification) Food Processing NC IiDocument3 pagesSelf-Assessment Guide (Full Qualification) Food Processing NC IiMarjun CeledonioNo ratings yet
- Fostering Social, Intellectual, Creative and EmotionalDocument59 pagesFostering Social, Intellectual, Creative and EmotionalDinda RamosNo ratings yet
- SALGIE SERNAL - 02C-Identifying-Training-GapsDocument6 pagesSALGIE SERNAL - 02C-Identifying-Training-GapsSalgie MasculinoNo ratings yet
- Group 8 CBLM Meeting The Nutrition ChallengeDocument47 pagesGroup 8 CBLM Meeting The Nutrition ChallengeJhon alfred T. TalosaNo ratings yet
- Lesson Plan in Tvl-Caregiving: Senior High School DepartmentDocument4 pagesLesson Plan in Tvl-Caregiving: Senior High School DepartmentJroybej BejonaNo ratings yet
- CASE PRESentationDocument30 pagesCASE PRESentationllanelli.graciaNo ratings yet
- Last Name: Full Name Middle NameDocument4 pagesLast Name: Full Name Middle NameMiss GNo ratings yet
- I. Vital Information: Cardiologist/IMDocument5 pagesI. Vital Information: Cardiologist/IMChristina Isabel MijaresNo ratings yet
- Class Notes On Questionnaires For Pharmacology in The Gastrointestinal TractDocument12 pagesClass Notes On Questionnaires For Pharmacology in The Gastrointestinal TractMarqxczNo ratings yet
- Perinatal Care Manual 3rd Edition 2013Document251 pagesPerinatal Care Manual 3rd Edition 2013Anonymous 9dVZCnTXS100% (3)
- Drug Study MetoclopramideDocument2 pagesDrug Study MetoclopramidePrince Rupee Gonzales100% (2)
- Assignment of Nursing Process FinalDocument43 pagesAssignment of Nursing Process FinalSandhya GuptaNo ratings yet
- Gaucher DiseaseDocument27 pagesGaucher DiseaseWahida PutriNo ratings yet
- Daftar PustakaDocument3 pagesDaftar PustakaNahrijah JahrinaNo ratings yet
- Fonlanan - AE - Dergi - Listesi (Tem2023 - Ara2024)Document30 pagesFonlanan - AE - Dergi - Listesi (Tem2023 - Ara2024)Taha EtemNo ratings yet
- Integrative Medicine PresentationDocument35 pagesIntegrative Medicine Presentationюрий локтионовNo ratings yet
- UWorld Step 3 DARKDocument43 pagesUWorld Step 3 DARKfreddawes100% (2)
- Us HealthcareDocument49 pagesUs HealthcareJerald FernandezNo ratings yet
- AMEKN3 - 03 - B - 05. HDocument1 pageAMEKN3 - 03 - B - 05. Hmary medinaNo ratings yet
- Sourav Das, Roll No 23, Hospital PharmacyDocument17 pagesSourav Das, Roll No 23, Hospital PharmacySourav DasNo ratings yet
- Acute Febrile IllnessesDocument96 pagesAcute Febrile IllnessesHAlid mohammed100% (1)
- Immunisation History Statement 3Document2 pagesImmunisation History Statement 3Fordham JessNo ratings yet
- FASENRA - PFS To Pen Communication Downloadable PDFDocument2 pagesFASENRA - PFS To Pen Communication Downloadable PDFBrîndușa PetruțescuNo ratings yet
- 3rd Mid CaseDocument32 pages3rd Mid CaseHarshini MakkenaNo ratings yet
- PHARMEVODocument3 pagesPHARMEVOFariha AnsariNo ratings yet
- RG 241 Hospital Practice Correct 2018 2019Document10 pagesRG 241 Hospital Practice Correct 2018 2019Jude ChinecheremNo ratings yet
- Visudyne Verteforpin Inj FDADocument13 pagesVisudyne Verteforpin Inj FDAUpik MoritaNo ratings yet
- Panduan Kesehatan OlahragaDocument1 pagePanduan Kesehatan OlahragaVidini Kusuma AjiNo ratings yet
- 136 ADocument5 pages136 AMarcelitaTaliaDuwiriNo ratings yet
- Clinical Approach To Optic Neuropathies: DiagnosisDocument14 pagesClinical Approach To Optic Neuropathies: Diagnosiskmathewjames100% (1)
- 108 217 1 SMDocument13 pages108 217 1 SMAnastasia FebruestiNo ratings yet
- Acute Care PT For Covid 19 PatientsDocument17 pagesAcute Care PT For Covid 19 PatientsSelvi SoundararajanNo ratings yet
- New Freedom Ops LLC Iop P&PDocument51 pagesNew Freedom Ops LLC Iop P&Pmike iovinoNo ratings yet
- Coxsackievirus: Presented By: LKCDocument18 pagesCoxsackievirus: Presented By: LKCLeang KarichakNo ratings yet
- DR Craig WeilDocument14 pagesDR Craig WeilPaula OwensNo ratings yet
- 24 Oet Full TestsDocument212 pages24 Oet Full TestsJoe Single86% (7)
- TMDDocument170 pagesTMDVinaya Srinivasan100% (2)
- Dr. Jigar PatelDocument6 pagesDr. Jigar PatelJigar PatelNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (31)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)