Professional Documents
Culture Documents
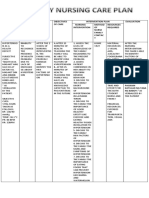
Peripheral Artery Disease
Uploaded by
DrNadia ZubairCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Peripheral Artery Disease
Uploaded by
DrNadia ZubairCopyright:
Available Formats
Peripheral Artery
Disease Legs
Peripheral artery disease is a condition
of the blood vessels that leads to
narrowing and hardening of the
arteries that supply the legs and feet.
The narrowing of the blood vessels leads
to decreased blood flow, which can
injure nerves and other tissues.
See All NEWS & FEATURES
Medicare Payments Surge for Stents to
Unblock Blood Vessels in Limbs
You Name It, and Exercise Helps It
New Priority: Saving Feet of Diabetics
Know Your Numbers and Improve Your
Odds
Health Sleuths Assess Homocysteine as
Culprit
Leg Pains, Bad Veins and Free Screenings
REFERENCE FROM A.D.A.M.
Back to TopAlternative
Names
Peripheral vascular disease; PVD; PAD;
Arteriosclerosis obliterans; Blockage of leg
arteries; Claudication; Intermittent claudication;
Vaso-occlusive disease of the legs; Arterial
insufficiency of the legs; Recurrent leg pain and
cramping; Calf pain with exercise
Back to TopCauses
Peripheral artery disease is caused
by arteriosclerosis, or "hardening of the arteries."
This problem occurs when fatty material (plaque)
builds up on the walls of your arteries. This causes
the arteries to become narrower. The walls of the
arteries also become stiffer and cannot widen
(dilate) to allow greater blood flow when needed.
As a result, when the muscles of your legs are
working harder (such as during exercise or
walking) they cannot get enough blood and
oxygen. Eventually, there may not be enough blood
and oxygen, even when the muscles are resting.
Peripheral artery disease is a common disorder
that usually affects men over age 50. People are at
higher risk if they have a history of:
Abnormal cholesterol
Diabetes
Heart disease (coronary artery disease)
High blood pressure (hypertension)
Kidney disease involving hemodialysis
Smoking
Stroke (cerebrovascular disease)
Back to TopSymptoms
The classic symptoms are pain, achiness, fatigue,
burning, or discomfort in the muscles of your feet,
calves, or thighs. These symptoms usually appear
during walking or exercise and go away after
several minutes of rest.
At first, these symptoms may appear only
when you walk uphill, walk faster, or walk for
longer distances.
Slowly, these symptoms come on more quickly
and with less exercise.
Your legs or feet may feel numb when you are
at rest. The legs also may feel cool to the touch,
and the skin may look pale.
When peripheral artery disease becomes severe,
you may have:
Impotence
Pain and cramps at night
Pain or tingling in the feet or toes, which can
be so severe that even the weight of clothes or bed
sheets is painful
Pain that is worse when you raise the leg and
improves when you dangle your legs over the side
of the bed
Skin that looks dark and blue
Sores that do not heal
In-Depth Symptoms
Back to TopExams
and Tests
During an examination, the health care provider
may find:
A whooshing sound with the stethoscope over
the artery (arterial bruits)
Decreased blood pressure in the affected limb
Loss of hair on the legs or feet
Weak or absent pulses in the limb
When PAD is more severe, findings may include:
Calf muscles that shrink (wither or atrophy)
Hair loss over the toes and feet
Painful, non-bleeding sores on the feet or toes
(usually black) that are slow to heal
Paleness of the skin or blue color in the toes or
foot (cyanosis)
Shiny, tight skin
Thick toenails
Blood tests may show high cholesterol or diabetes.
Tests for peripheral artery disease:
Angiography of the arteries in the legs
(arteriography)
Blood pressure measured in the arms and legs
for comparison (ankle/brachial index, or ABI)
Doppler ultrasound exam of an extremity
Magnetic resonance angiography or CT
angiography
In-Depth Diagnosis
Back to TopTreatment
Balance exercise with rest. Walk or do another
activity to the point of pain and alternate it with
rest periods. Over time, your circulation may
improve as new, small (collateral) blood vessels
form. Always talk to the doctor before starting an
exercise program.
Stop smoking. Smoking narrows the arteries,
decreases the blood's ability to carry oxygen, and
increases the risk of forming clots (thrombi and
emboli).
Take care of your feet, especially if you also
have diabetes. Wear shoes that fit properly. Pay
attention to any cuts, scrapes, or injuries, and see
your doctor right away. Tissues heal slowly and are
more likely to get infected when there is decreased
circulation.
Make sure your blood pressure is well
controlled.
Reduce your weight, if you are overweight.
If your cholesterol is high, eat a lowcholesterol and low-fat diet.
Monitor your blood sugar levels if you have
diabetes, and keep them under control.
Medications may be needed to control the
disorder, including:
Aspirin or a medicine called clopidogrel
(Plavix), which keeps your blood from forming
clots in your arteries. Do NOT stop taking these
medications without first talking with your doctor.
Cilostazol, a medication to enlarge (dilate) the
affected artery or arteries for moderate-to-severe
cases that are not candidates for surgery
Medicine to help lower your cholesterol
Pain relievers
If you are taking medicines for high blood pressure
or diabetes, take them as your doctor has
prescribed.
Surgery may be performed if the condition is
severe and is affecting your ability to work or do
important activities, or you are having pain at rest.
Options are:
Angioplasty and stent placement of the
peripheral arteries (this is similar to the technique
used to open the coronary arteries, but it is
performed on the blood vessels of the affected leg)
Peripheral artery bypass surgery of the leg
Some people with peripheral artery disease may
need to have the limb removed (amputated).
In-Depth Treatment
Back to TopOutlook
(Prognosis)
You can usually control peripheral artery disease
of the legs without surgery. Surgery provides good
symptom relief in severe cases.
For complications, the affected leg or foot may
need to be amputated.
Back to TopPossible
Complications
Blood clots or emboli that block off small
arteries
Coronary artery disease
Impotence
Open sores (ischemic ulcers) on the lower legs
Tissue death (gangrene) -- see gas gangrene
Back to TopWhen
to Contact a Medical
Professional
Call your health care provider if you have:
A leg or foot that becomes cool to the touch,
pale, blue, or numb
Chest pain or shortness of breath with leg pain
Leg pain that does not go away, even when you
are not walking or moving (called rest pain)
Legs that are red, hot, or swollen
New sores/ulcers
Signs of infection (fever, redness, general ill
feeling)
Symptoms of arteriosclerosis of the extremities
You might also like
- Peripheral Arterial DiseaseDocument5 pagesPeripheral Arterial Diseaseampogison08No ratings yet
- Thyroid CrisisDocument11 pagesThyroid CrisisKoka KolaNo ratings yet
- Cardiac TamponadeDocument29 pagesCardiac Tamponadeanimesh pandaNo ratings yet
- Nephrotic Syndrome: Prepared By: Manisha Praharaj Msc. Nursing 2Nd YearDocument28 pagesNephrotic Syndrome: Prepared By: Manisha Praharaj Msc. Nursing 2Nd YearMaria YaseenNo ratings yet
- Drug Used in Skin and Mucus MembraneDocument35 pagesDrug Used in Skin and Mucus MembraneMamta Yadav100% (1)
- Warning Signs of Various DiseasesDocument44 pagesWarning Signs of Various DiseasesamsabavanNo ratings yet
- Drug Heart Failure MDocument24 pagesDrug Heart Failure MAthari KhanNo ratings yet
- TB TreatmentDocument58 pagesTB TreatmentNdayisaba CorneilleNo ratings yet
- BMT ReportDocument26 pagesBMT ReportCaroline AgbayNo ratings yet
- Cardiac ArrythmiasDocument37 pagesCardiac ArrythmiasRubina100% (1)
- Hypertensive Heart DiseaseDocument33 pagesHypertensive Heart Diseaserini_adriani6817No ratings yet
- ElephantiasisDocument23 pagesElephantiasisNitin0% (1)
- Presentation SWINE FLUDocument40 pagesPresentation SWINE FLUdr_hammadNo ratings yet
- Disorders of Parathyroid Glands: Hyperparathyroidism and HypoparathyroidismDocument52 pagesDisorders of Parathyroid Glands: Hyperparathyroidism and HypoparathyroidismDr. Akash GuptaNo ratings yet
- Abdominal IncisionDocument4 pagesAbdominal IncisionMohit KumarNo ratings yet
- Blood CoagulationDocument10 pagesBlood CoagulationgauravkokraNo ratings yet
- Isabela State University City of Ilagan Campus: Care of The Clients With Endocrine and Metabolic DisorderDocument15 pagesIsabela State University City of Ilagan Campus: Care of The Clients With Endocrine and Metabolic DisorderCharlz ZipaganNo ratings yet
- Sickle Cell Disease: Symptoms and TreatmentDocument13 pagesSickle Cell Disease: Symptoms and TreatmentAditya Rangga Fandiarta100% (1)
- Pyogenic MeningitisDocument46 pagesPyogenic MeningitisShahnaaz ShahNo ratings yet
- PLAGUEDocument5 pagesPLAGUEHpu JogindernagerNo ratings yet
- The Effect of Structured Teaching Program On Knowledge About Arterial Blood Gas Analysis Among The Staff Nurses Working in Critical Care UnitDocument7 pagesThe Effect of Structured Teaching Program On Knowledge About Arterial Blood Gas Analysis Among The Staff Nurses Working in Critical Care UnitIJAR JOURNALNo ratings yet
- Inguinal Hernias and Abdominal Wall Defects: Murad Nuserat & Abd AL-Rahman AlhelwDocument51 pagesInguinal Hernias and Abdominal Wall Defects: Murad Nuserat & Abd AL-Rahman AlhelwRashed ShatnawiNo ratings yet
- SepsisDocument33 pagesSepsisv_vijayakanth7656No ratings yet
- Arterial Line Arterial LineDocument13 pagesArterial Line Arterial LineLinamaria Lozano100% (1)
- Different Diagnostic Procedure of Typhoid Fever ADocument8 pagesDifferent Diagnostic Procedure of Typhoid Fever AdjebrutNo ratings yet
- Fat Embolism SyndromeDocument26 pagesFat Embolism SyndromeAzni MokhtarNo ratings yet
- HypertensionDocument21 pagesHypertensionM RaisNo ratings yet
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesFrom EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNo ratings yet
- Renal TransplantationDocument50 pagesRenal Transplantationregie cuaresmaNo ratings yet
- Pemphigus vulgarisPPTDocument23 pagesPemphigus vulgarisPPTSiti HanisaNo ratings yet
- Cirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDocument21 pagesCirrhosis in Adults: Overview of Complications, General Management, and Prognosis - UpToDateDan ChicinasNo ratings yet
- GB SyndromeDocument17 pagesGB Syndromehajra StudentNo ratings yet
- Essential Hypertension ManagementDocument5 pagesEssential Hypertension Managementspicychips7No ratings yet
- PancreatitisDocument59 pagesPancreatitisAarif RanaNo ratings yet
- CKD Overview: Causes, Symptoms and Stages of Chronic Kidney DiseaseDocument15 pagesCKD Overview: Causes, Symptoms and Stages of Chronic Kidney Diseasejames100% (1)
- Kidney Function TestDocument21 pagesKidney Function TestVinoantonyNo ratings yet
- ArrhythmiasDocument48 pagesArrhythmiasHarshan JeyakumarNo ratings yet
- Clinical Examination of Genitourinary SystemDocument43 pagesClinical Examination of Genitourinary SystemKeamina .aNo ratings yet
- Child Ear Infection CausesDocument9 pagesChild Ear Infection CausesMona Santi NainggolanNo ratings yet
- Congenital Heart DiseaseDocument106 pagesCongenital Heart DiseaseHarold DiasanaNo ratings yet
- Rheumatic Fever: DR: Kaem Shir AliDocument24 pagesRheumatic Fever: DR: Kaem Shir AliMwanja Moses100% (1)
- Neurology - : Approach To Headache DisordersDocument8 pagesNeurology - : Approach To Headache DisordersKarenNo ratings yet
- Endocarditis, Pericarditic, Myocarditis: TopicDocument104 pagesEndocarditis, Pericarditic, Myocarditis: TopicOM VERMANo ratings yet
- Endosco Py: Diploma IV Nurs Ing 201 6Document27 pagesEndosco Py: Diploma IV Nurs Ing 201 6Tri Juniarti Sr.No ratings yet
- Universal Immunization ProgrammeDocument8 pagesUniversal Immunization ProgrammeNagaraj ReddyNo ratings yet
- CryptococcosisDocument25 pagesCryptococcosisinvisibleyetinvincibleNo ratings yet
- Drugs Affecting Calcium BalanceDocument63 pagesDrugs Affecting Calcium BalanceRd Chandane100% (1)
- ARDS Care Respiratory Care Plan PDFDocument2 pagesARDS Care Respiratory Care Plan PDFeric parlNo ratings yet
- Preoperative Preparation of Patient For SurgeryDocument23 pagesPreoperative Preparation of Patient For SurgeryFauzi SebunyaNo ratings yet
- CholeraDocument4 pagesCholeraBeth AvelinoNo ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- Understanding Low Blood PressureDocument6 pagesUnderstanding Low Blood PressureRajeev Nechiyil100% (1)
- Eye ExaminationDocument23 pagesEye Examinationcynthia167No ratings yet
- Rheumatology Notes and Learning ObjectivesDocument7 pagesRheumatology Notes and Learning Objectiveskep1313No ratings yet
- EC2021-Medical Electronics Notes For All Five UnitsDocument147 pagesEC2021-Medical Electronics Notes For All Five UnitsJason Jackson100% (1)
- Acute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CDocument29 pagesAcute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CEdelrose Lapitan100% (1)
- Manage Head InjuriesDocument18 pagesManage Head InjuriesChellamani UmakanthanNo ratings yet
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Peripheral Artery Disease - LegsDocument6 pagesPeripheral Artery Disease - LegsCecil Bhang-i Cacay - PabloNo ratings yet
- Decriptive Book PDFDocument160 pagesDecriptive Book PDFKarthik RamNo ratings yet
- Socioeconomic Status of HypertensionDocument3 pagesSocioeconomic Status of HypertensionDrNadia ZubairNo ratings yet
- Hse - JDDocument1 pageHse - JDDrNadia ZubairNo ratings yet
- Guide For Precis WritingDocument2 pagesGuide For Precis WritingAbdul Haadi ButtNo ratings yet
- Time ManagementDocument11 pagesTime ManagementDrNadia Zubair100% (1)
- About Drap & Drug LawsDocument4 pagesAbout Drap & Drug LawsDrNadia ZubairNo ratings yet
- Job Order CostingDocument5 pagesJob Order CostingDrNadia ZubairNo ratings yet
- Popular Poems of William ShakespeareDocument11 pagesPopular Poems of William ShakespeareDrNadia ZubairNo ratings yet
- Popular Poems of William ShakespeareDocument11 pagesPopular Poems of William ShakespeareDrNadia ZubairNo ratings yet
- Lower Portfolio Risk through Optimal DiversificationDocument4 pagesLower Portfolio Risk through Optimal DiversificationDrNadia ZubairNo ratings yet
- International Diversity WorksDocument23 pagesInternational Diversity WorksDrNadia ZubairNo ratings yet
- Basics of Demand & SupplyDocument7 pagesBasics of Demand & SupplyDrNadia ZubairNo ratings yet
- Target MarketDocument7 pagesTarget MarketDrNadia ZubairNo ratings yet
- Interview Questions For Pharmaceutical Industry Related JobsDocument41 pagesInterview Questions For Pharmaceutical Industry Related JobsDrNadia Zubair86% (22)
- How Diversification Reduces RiskDocument3 pagesHow Diversification Reduces RiskDrNadia ZubairNo ratings yet
- AngelmarPharmaMktgStratMay June07Document12 pagesAngelmarPharmaMktgStratMay June07pinakindpatelNo ratings yet
- Purette Milk. 1Document18 pagesPurette Milk. 1DrNadia ZubairNo ratings yet
- Managers Vs LeadersDocument2 pagesManagers Vs LeadersDrNadia ZubairNo ratings yet
- Feasibility Report of BakeryDocument38 pagesFeasibility Report of BakeryDrNadia Zubair75% (52)
- Role of Packaging On Consumer Buying BehaviorDocument93 pagesRole of Packaging On Consumer Buying BehaviorDrNadia ZubairNo ratings yet
- Reasons for International Trade: Benefits and DrawbacksDocument4 pagesReasons for International Trade: Benefits and DrawbacksDrNadia ZubairNo ratings yet
- Negotiable InstrumentsDocument15 pagesNegotiable InstrumentsDrNadia ZubairNo ratings yet
- Presentation Tactics: Seminar in Business CommunicationDocument14 pagesPresentation Tactics: Seminar in Business CommunicationDrNadia ZubairNo ratings yet
- Comparison of Islamic and Conventional (Abdul Ghafoor Awan)Document36 pagesComparison of Islamic and Conventional (Abdul Ghafoor Awan)Muhammad FurqanNo ratings yet
- Pakistan Golden MomentsDocument58 pagesPakistan Golden MomentsDrNadia ZubairNo ratings yet
- Human Resource ManagementDocument34 pagesHuman Resource Managementnrp8409No ratings yet
- Functions of Management - AssignmentDocument27 pagesFunctions of Management - Assignmenttunali2132184% (61)
- mgt1 1232526946801622 3Document27 pagesmgt1 1232526946801622 3DrNadia ZubairNo ratings yet
- Principles of Behavior ChangeDocument10 pagesPrinciples of Behavior ChangeGuillermo ThomasNo ratings yet
- Acute Service Pain Handbook 2011Document116 pagesAcute Service Pain Handbook 2011Iskandar414No ratings yet
- LOG BOOK For Objective Assessment C-P I & II KMUDocument13 pagesLOG BOOK For Objective Assessment C-P I & II KMUFarhaanKhanHaleem100% (3)
- Trauma Brain Injury, Kuliah PakarDocument40 pagesTrauma Brain Injury, Kuliah PakarveninoriaNo ratings yet
- Edaic 3Document16 pagesEdaic 3DsdNo ratings yet
- LT033 PDFDocument38 pagesLT033 PDFAlexandr ChuvakovNo ratings yet
- Chapter 18 Personality DisordersDocument10 pagesChapter 18 Personality DisordersCatia Fernandes100% (2)
- Close Fracture Radius Ulna Distal Sinistra: Case ReportDocument30 pagesClose Fracture Radius Ulna Distal Sinistra: Case ReportyoyokNo ratings yet
- Referat CA PancreasDocument25 pagesReferat CA PancreasPamela VasikhaNo ratings yet
- Rectal ProlapseDocument2 pagesRectal ProlapseSalem ZoghbyNo ratings yet
- Dengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaDocument3 pagesDengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaReju VijayandranNo ratings yet
- B SCAN PPPDocument92 pagesB SCAN PPPSiva Wurity100% (1)
- Nelson FNCPDocument2 pagesNelson FNCPDenisse Shazz Mae MaretNo ratings yet
- Print - Chapter 13. Bilirubin Formation and Excretion by The LiverDocument11 pagesPrint - Chapter 13. Bilirubin Formation and Excretion by The LiverbelaginaNo ratings yet
- The Genetics of MicrocephalyDocument6 pagesThe Genetics of MicrocephalyErsya MuslihNo ratings yet
- Renr Study GuideDocument57 pagesRenr Study GuideJerilee SoCute Watts92% (12)
- Nursing Care Plan PrenatalDocument5 pagesNursing Care Plan PrenatalKim Galamgam100% (2)
- Short Sightedness Vs Long SightDocument1 pageShort Sightedness Vs Long SightDevill DavajNo ratings yet
- Competency Based EducationDocument33 pagesCompetency Based EducationAncy Varkey100% (1)
- Increased ICP and Neurological Trauma GuideDocument14 pagesIncreased ICP and Neurological Trauma GuideMhoy CostesNo ratings yet
- Perioperative Nursing Care IssuesDocument7 pagesPerioperative Nursing Care IssuesAziil LiizaNo ratings yet
- Health Care Industry Crystal Report ScenariosDocument2 pagesHealth Care Industry Crystal Report ScenariosKishore KumarNo ratings yet
- 8 Emergency Formative Clinical Evaluation ChecklistDocument1 page8 Emergency Formative Clinical Evaluation Checklistمهند الرحيليNo ratings yet
- Bone Tumour Synovial Sarcoma Imaging FindingsDocument28 pagesBone Tumour Synovial Sarcoma Imaging FindingsAnonymous bE4VegCcNo ratings yet
- CC.14.01 Pre and Post Operative CareDocument3 pagesCC.14.01 Pre and Post Operative CareKrupaNo ratings yet
- MMT LL DR Barinov Reply Limb Lengthening RussiaDocument3 pagesMMT LL DR Barinov Reply Limb Lengthening RussiaAaron GohNo ratings yet
- ICNCDRS Blindness Registry FormDocument4 pagesICNCDRS Blindness Registry FormAprilAngeliRobleNo ratings yet
- Introduction To AnesthesiologyDocument68 pagesIntroduction To AnesthesiologyOzza AlhudaNo ratings yet
- Survival Strategies For Parenting The Child & Teen With BipolarDocument236 pagesSurvival Strategies For Parenting The Child & Teen With Bipolarseptiadhi wirawanNo ratings yet
- Application CoopMED Health Insurance Plan BarbadosDocument2 pagesApplication CoopMED Health Insurance Plan BarbadosKammieNo ratings yet