Professional Documents
Culture Documents
Director Health Economics Reimbursement in Memphis TN Resume Michael McCormack
Uploaded by
MichaelMcCormackCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Director Health Economics Reimbursement in Memphis TN Resume Michael McCormack
Uploaded by
MichaelMcCormackCopyright:
Available Formats
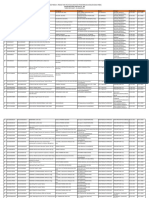
Michael K.
McCormack, FACHE
Arlington, Tennessee 38002
mike.k.mccormack@gmail.com
901-310-9826
www.linkedin.com/in/mikekmccormack
DIRECTOR HEALTH ECONOMICS / POLICY AND REIMBURSEMENT
Extensive experience and highly respected expertise in health care reimbursement, health policy,
market access and health economics. Diligently analyzed federal and commercial payer regulations,
policies, processes and issues. Adeptly developed and executed viable, pragmatic solutions.
Consistently achieved key wins that protected provider reimbursement and facilitated market access
for technologies and procedures. Developed and maintained high performance teams and a climate
of best practices. Areas of expertise include:
Health Care Policy and Reimbursement
Policy Analysis and Solution Development
Sales/Marketing/Customer Service
Strategic Planning/Action Plans
Health Care Administration and Management
Project Management
Budget Planning and Compliance
Cross-Functional Team Building
PROFESSIONAL EXPERIENCE
ACCLARENT, INC., a business unit of Johnson & Johnson, Menlo Park, CA
2012 2014
Director, Health Economics and Reimbursement
Developed and implemented reimbursement strategies that ensured appropriate coding, coverage
and payment for Acclarent technologies and related procedures. Developed reimbursement tools for
use by internal and external customers. Provided coding advocacy, oversaw commercial insurance
market access activities, and advocated for appropriate reimbursement for procedures and
technologies from the Centers for Medicare and Medicaid Services (CMS).
Led advocacy efforts to combat CMS proposal to base physician non-facility PE RVUs and
payments on hospital outpatient or ASC payment rates. Activities resulted in the proposal being
rescinded.
Successfully advocated for APC changes, resulting in a 51% payment increase for Acclarentrelated procedures.
Advocated for policy changes with multiple commercial insurance plans leading to increased
access for over 7.5 million people.
MEDTRONIC, INC., Spinal and Biologics Division, Memphis, TN
2002 2012
Director, Health Policy and Reimbursement
2008 2012
Senior Manager, Reimbursement Planning
2004 2008
Manager, Reimbursement Planning
2002 2004
Provided pre-market reimbursement analyses and developed strategies to ensure appropriate
coding, coverage and payment for products/procedures. Provided management of coding support
resources and coding advocacy. Developed reimbursement support materials for both current and
future technologies, and advocated for appropriate reimbursement for spinal procedures and
technologies from the Centers for Medicare and Medicaid Services (CMS).
Conducted the data analysis and completed the application that led to Medtronic receiving the
first Medicare New Technology Add-on Payment for a medical device.
Appointed to the integration team and performed reimbursement-related due diligence for the
$4.2B acquisition of Kyphon, Inc.
Michael K. McCormack
Page 2 of 2
MEDTRONIC, INC. (Continued)
Advocated for and won approval on several occasions to regroup procedures to more cost
appropriate and better reimbursing MS-DRGs.
Wrote numerous coding proposals that resulted in the establishment of new ICD-9-CM
procedure codes.
Successfully overturned two National Correct Coding Initiative (NCCI) edits that bundled
physician payment for two common spinal procedures, ensuring provider payment for both
services.
Collaborated with two specialty medical societies to put forth a category I CPT code application
for cervical disc arthroplasty, facilitating physician reimbursement for these procedures.
WEST TENNESSEE HEALTHCARE, Jackson, TN
1996 2002
Compliance Officer
1998 - 2002
Oversaw program development and managed ongoing operations. Led efforts to educate and
ensure organization compliance with health care laws and regulations, along with the organization's
ethics culture. Conducted audits to measure compliance with applicable regulations and developed
needed corrective action plans.
Wrote and published an organization-wide Code of Conduct and trained 4,500 employees in
aspects of compliance and ethics, ensuring a thorough understanding and consistent focus on
organizational compliance.
Initiated a review of the Charge Description Masters that resulted in the organization netting an
additional $5-$10M per year in gross revenue plus other benefits in standardization and
reporting.
Developed and implemented new processes that reduced the amount of medical necessity
denials by more than $120K per month.
Implemented new processes for the charging of observation services, reducing the amount of
denials by more than $125K per year and bringing the organization in compliance with
Medicare's requirements.
Developed and implemented new processes, negotiated purchase of new software, and
established reliable billing of claims to Medicare that reduced potential liability for false claim
charges.
Director, Work Partners
1996 - 1998
Drove strategic planning, product and service development, profit and loss responsibility for a
hospital-owned workers compensation managed care organization. Managed the program with a
scope of responsibility that included provider network development, case management, claims
processing, sales, marketing and customer service.
Grew the product to over 10,000 covered employees in 15 months, capturing a 21% market
share for self-funded employers in the region.
Negotiated contracts and reimbursement amounts with providers, building a provider network
that included over 400 physicians practicing in the area.
Served as a key partner in the establishment of a statewide workers' compensation network that
is marketed to employers with multiple locations across the state.
EDUCATION
Master of Health Administration, Georgia State University, Atlanta, GA
Master of Business Administration, Georgia State University, Atlanta, GA
Bachelor of Science, Kinesiology, University of Tennessee, Knoxville, TN
You might also like
- Healthcare Staffing Income Generation Strategies HandbookFrom EverandHealthcare Staffing Income Generation Strategies HandbookNo ratings yet
- Operations Manager in Kansas City MO Resume Rosalind ConnerDocument2 pagesOperations Manager in Kansas City MO Resume Rosalind ConnerRosalindConnerNo ratings yet
- To Taste or Not To TasteDocument3 pagesTo Taste or Not To TasteSpeech & Language Therapy in PracticeNo ratings yet
- Director VP Total Rewards in Northern CA Resume Marguerite RadeffDocument3 pagesDirector VP Total Rewards in Northern CA Resume Marguerite RadeffMargueriteRadoff100% (1)
- Healthcare CFO CPA MBA in Miami/Fort Lauderdale FL Resume Henry BrownDocument3 pagesHealthcare CFO CPA MBA in Miami/Fort Lauderdale FL Resume Henry BrownHenry BrownNo ratings yet
- Chief Executive Officer in Brentwood TN Resume Gary FergusonDocument3 pagesChief Executive Officer in Brentwood TN Resume Gary FergusonGaryFerguson1No ratings yet
- Director Project Management PMO in Washington D.C. Metro Resume Matthew HopwoodDocument3 pagesDirector Project Management PMO in Washington D.C. Metro Resume Matthew HopwoodMatthew HopwoodNo ratings yet
- VP Sales Marketing Health in Raleigh Durham NC Resume Donald SwankieDocument4 pagesVP Sales Marketing Health in Raleigh Durham NC Resume Donald SwankieDonaldSwankieNo ratings yet
- Project Management Pharmaceutical Applications Implementation in Bridgewater NJ Resume Wendell KirbyDocument3 pagesProject Management Pharmaceutical Applications Implementation in Bridgewater NJ Resume Wendell KirbyWendellKirbyNo ratings yet
- Vice President in ST Louis MO Resume Karen Hercules-DoerrDocument2 pagesVice President in ST Louis MO Resume Karen Hercules-DoerrKarenHerculesDoerrNo ratings yet
- Vice President of Operations in Phoenix AZ Resume Carol LivingstonDocument3 pagesVice President of Operations in Phoenix AZ Resume Carol LivingstonCarol LivingstonNo ratings yet
- 2-3. G.R. No. 88265 Del Rosario V Bengzon (Digest)Document2 pages2-3. G.R. No. 88265 Del Rosario V Bengzon (Digest)Iter Mercatabant0% (1)
- Chief Operating Officer CCO in Charlotte NC Resume Ram ManchiDocument2 pagesChief Operating Officer CCO in Charlotte NC Resume Ram ManchiRam ManchiNo ratings yet
- Account Field Reimbursement Manager in CA Resume Roger WortsmanDocument2 pagesAccount Field Reimbursement Manager in CA Resume Roger WortsmanRogerWortsmanNo ratings yet
- Homeopathy Course HpathyDocument35 pagesHomeopathy Course Hpathymazzagra100% (1)
- Incident Near Miss ReportingDocument38 pagesIncident Near Miss ReportingKhaskheli Nusrat100% (3)
- Strategic Healthcare Industry TransformationDocument6 pagesStrategic Healthcare Industry TransformationFreed Maxick CPAsNo ratings yet
- Healthcare Operations Management Consultant in Chicago IL Resume Brenda BehrensDocument2 pagesHealthcare Operations Management Consultant in Chicago IL Resume Brenda BehrensBrendaBehrens2No ratings yet
- Mark E. Locklear ResumeDocument5 pagesMark E. Locklear ResumeMark LocklearNo ratings yet
- VP Client Services Healthcare in Greater Chicago IL Resume Marybeth ReganDocument5 pagesVP Client Services Healthcare in Greater Chicago IL Resume Marybeth ReganMarybeth ReganNo ratings yet
- CFO Controller Manufacturing Distribution in New Haven CT Resume Chet LatinDocument3 pagesCFO Controller Manufacturing Distribution in New Haven CT Resume Chet LatinChetLatinNo ratings yet
- Biotechnology: From Idea To MarketDocument4 pagesBiotechnology: From Idea To MarketTim Sandle100% (1)
- Acyclovir Drug Study WWW RNpedia ComDocument3 pagesAcyclovir Drug Study WWW RNpedia ComJanaica JuanNo ratings yet
- Nurs403 Complete Issue AnalysisDocument12 pagesNurs403 Complete Issue Analysisldhenderson100% (1)
- VP Health Insurance Operations in Boston MA Resume Thomas EverettDocument2 pagesVP Health Insurance Operations in Boston MA Resume Thomas EverettThomas EverettNo ratings yet
- Vice President Managed Care in Sacramento CA Resume Jeffrey BaumeisterDocument3 pagesVice President Managed Care in Sacramento CA Resume Jeffrey BaumeisterJeffreyBaumeisterNo ratings yet
- GirishDocument7 pagesGirishAshwani kumarNo ratings yet
- Director Property Casualty Insurance in Boston MA Resume William KratchDocument2 pagesDirector Property Casualty Insurance in Boston MA Resume William KratchWilliamKratchNo ratings yet
- Sample Resume - CV - Arch2011 - Kevindeysenroth - Working Professional - BestDocument3 pagesSample Resume - CV - Arch2011 - Kevindeysenroth - Working Professional - BestSachin TichkuleNo ratings yet
- Vice President or Executive Director or DirectorDocument4 pagesVice President or Executive Director or Directorapi-77396522No ratings yet
- Pharmaceutical Reimbursement Access Manager in Austin TX Resume Brian BucklesDocument2 pagesPharmaceutical Reimbursement Access Manager in Austin TX Resume Brian BucklesBrian Buckles100% (1)
- Updated CV 2021 Pages 1 7Document7 pagesUpdated CV 2021 Pages 1 7د عبدالجليل نادر محمد عبدالجليلNo ratings yet
- Chief Information Officer CIO in Southeast USA Resume Joseph WoodDocument3 pagesChief Information Officer CIO in Southeast USA Resume Joseph WoodJosephWoodNo ratings yet
- Director Operations in Miami FT Lauderdale FL Resume Fernando GarciaDocument2 pagesDirector Operations in Miami FT Lauderdale FL Resume Fernando GarciaFernandoGarcia2No ratings yet
- VP Director HR Talent Development in OK Resume Tom HillDocument3 pagesVP Director HR Talent Development in OK Resume Tom HillTomHill2No ratings yet
- Director Healthcare IT Management Consulting in United States Resume Patricia TikkanenDocument3 pagesDirector Healthcare IT Management Consulting in United States Resume Patricia TikkanenPatriciaTikkanenNo ratings yet
- VP Business Development Eclinical Applications in Nashville TN Resume John HedbergDocument2 pagesVP Business Development Eclinical Applications in Nashville TN Resume John HedbergJohnHedbergNo ratings yet
- Chief Financial Officer Controller in Colorado Springs CO Resume Steve WarnekeDocument3 pagesChief Financial Officer Controller in Colorado Springs CO Resume Steve WarnekeSteveWarnekeNo ratings yet
- 5 2 Final Project Milestone Three Draft of Billing Marketing and ReimbursementDocument5 pages5 2 Final Project Milestone Three Draft of Billing Marketing and ReimbursementHugsNo ratings yet
- Workers Compensation Risk Manager in Pittsburgh PA Resume Seon PierceDocument3 pagesWorkers Compensation Risk Manager in Pittsburgh PA Resume Seon PierceSeon PierceNo ratings yet
- Employee Benefits Manager Healthcare in Chicago IL Resume Keri BemorasDocument2 pagesEmployee Benefits Manager Healthcare in Chicago IL Resume Keri BemorasKeriBemorasNo ratings yet
- Manager Workers Compensation Claims in Fort Myers FL Resume Gail KrinskyDocument3 pagesManager Workers Compensation Claims in Fort Myers FL Resume Gail KrinskyGailKrinskyNo ratings yet
- Employee Benefits Director Manager in New York City Resume Michael HarrisDocument2 pagesEmployee Benefits Director Manager in New York City Resume Michael HarrisMichael HarrisNo ratings yet
- Director Operations in Kansas City MO Resume Sandra LeaderbrandDocument2 pagesDirector Operations in Kansas City MO Resume Sandra LeaderbrandSandraLeaderbrandNo ratings yet
- Customer Service Operations Manager in Nashville TN Resume Tim HopkinsDocument2 pagesCustomer Service Operations Manager in Nashville TN Resume Tim HopkinsTimHopkinsNo ratings yet
- Senior Human Resources Director Attorney in Milwaukee WI Resume Christiane StandleeDocument3 pagesSenior Human Resources Director Attorney in Milwaukee WI Resume Christiane StandleeChristianeStandlee2No ratings yet
- Senior HR Director Attorney in Milwaukee WI Resume Christiane StandleeDocument3 pagesSenior HR Director Attorney in Milwaukee WI Resume Christiane StandleeChristianeStandleeNo ratings yet
- Innovaccer Case - v1Document4 pagesInnovaccer Case - v1Pranay DatarNo ratings yet
- Operations Manager or Leadership Trainer or Change Management orDocument3 pagesOperations Manager or Leadership Trainer or Change Management orapi-76968634100% (1)
- Business Development Director Healthcare in Ontario Canada Resume Harley RodinDocument4 pagesBusiness Development Director Healthcare in Ontario Canada Resume Harley RodinHarley RodinNo ratings yet
- Dannell MaguireDocument2 pagesDannell MaguireDannellMaguireNo ratings yet
- Vice President Insurance Sales Operations in CT MA Resume Susan HutchinsDocument2 pagesVice President Insurance Sales Operations in CT MA Resume Susan HutchinsSusanHutchinsNo ratings yet
- B-School Case Studies - ConsolidatedDocument11 pagesB-School Case Studies - ConsolidatedAkhil SoniNo ratings yet
- Medicare Healthcare Sales Executive in CA Resume Bren WhitakerDocument2 pagesMedicare Healthcare Sales Executive in CA Resume Bren Whitakerbefoundjobs613No ratings yet
- Director Call Center Operations in Albuquerque NM Resume Kathie LehnerDocument2 pagesDirector Call Center Operations in Albuquerque NM Resume Kathie LehnerKathieLehnerNo ratings yet
- Challeges of Underwriting in USADocument5 pagesChalleges of Underwriting in USAtanvisingh_2007No ratings yet
- Financial Services Health Care Analyst in Baltimore MD Resume Harriet ShrairDocument2 pagesFinancial Services Health Care Analyst in Baltimore MD Resume Harriet ShrairHarrietShrairNo ratings yet
- Michael A. DavisDocument2 pagesMichael A. DavisRandy DavisNo ratings yet
- Case Study SMDCDocument30 pagesCase Study SMDCSonya DewiNo ratings yet
- Human Resource Specialist Benefits Payroll in San Diego CA Resume Lisa CoffeyDocument2 pagesHuman Resource Specialist Benefits Payroll in San Diego CA Resume Lisa CoffeylisacoffeyNo ratings yet
- Vice President Banking Branch Operations in NYC Resume Anthony CarleoDocument2 pagesVice President Banking Branch Operations in NYC Resume Anthony CarleoAnthonyCarleoNo ratings yet
- Clinical Engineering Biomedical Director in Virginia Beach VA Resume Libby MillsDocument2 pagesClinical Engineering Biomedical Director in Virginia Beach VA Resume Libby MillsLibbyMills2No ratings yet
- Senior Financial Analyst in Washington DC VA Resume Joseph TrammDocument2 pagesSenior Financial Analyst in Washington DC VA Resume Joseph TrammJosephTrammNo ratings yet
- Vice President Healthcare Consulting Operations in Seattle WA Resume Robert JablonskiDocument5 pagesVice President Healthcare Consulting Operations in Seattle WA Resume Robert JablonskiRobertJablonski2No ratings yet
- CIO CEO VP Professional Services in Boston MA Resume Henry ThebergeDocument2 pagesCIO CEO VP Professional Services in Boston MA Resume Henry ThebergeHenryTheberge2No ratings yet
- President CEO in Pittsburgh PA Resume Michael HinsonDocument3 pagesPresident CEO in Pittsburgh PA Resume Michael HinsonMichaelHinsonNo ratings yet
- Basil and MigrainesDocument9 pagesBasil and MigrainesEstefania BatemanNo ratings yet
- JCI RequirementsDocument16 pagesJCI RequirementsKenny JosefNo ratings yet
- Healthcare Financing Infrastructure PaperDocument25 pagesHealthcare Financing Infrastructure Papersri_cbmNo ratings yet
- PMLS Lec Lesson 1Document53 pagesPMLS Lec Lesson 1Janna EchavezNo ratings yet
- 2012 - All Levels Glossary: Quality, Safety and Evidence-Based Practice (Ebp)Document6 pages2012 - All Levels Glossary: Quality, Safety and Evidence-Based Practice (Ebp)Hani TuasikalNo ratings yet
- Patient Education and CounselingDocument6 pagesPatient Education and CounselingDheaNo ratings yet
- 9 Nurse AssessmentDocument14 pages9 Nurse AssessmentHielda MariyanaNo ratings yet
- Access To Mammography in New York City'Document43 pagesAccess To Mammography in New York City'NYCCouncilNo ratings yet
- Senarai Produk Yang Diluluskan Dalam PBKD380 5 Januari 2023 WebsiteDocument16 pagesSenarai Produk Yang Diluluskan Dalam PBKD380 5 Januari 2023 Websitearif azaliNo ratings yet
- Gen HospitalDocument1 pageGen HospitalDiztrict GarageNo ratings yet
- My Favorite Childhood Memory EssayDocument7 pagesMy Favorite Childhood Memory Essayezmpjbta100% (2)
- Counselling Psychology SeminarDocument6 pagesCounselling Psychology Seminarmadhu mithaNo ratings yet
- Research in Social and Administrative PharmacyDocument4 pagesResearch in Social and Administrative PharmacyAndrea MendozaNo ratings yet
- Medical Repricing-96105332Document14 pagesMedical Repricing-96105332Mazlynn AmirNo ratings yet
- IND, NDA, ANDA IndiaDocument51 pagesIND, NDA, ANDA IndiakbnarkhedeNo ratings yet
- Quality of Postnatal Care ServicesDocument10 pagesQuality of Postnatal Care Servicessaleha sultanaNo ratings yet
- David BantingDocument35 pagesDavid BantingNishad NTNo ratings yet
- City of Cleveland v. Eli Lilly & Co., Et Al.Document157 pagesCity of Cleveland v. Eli Lilly & Co., Et Al.WKYC.comNo ratings yet
- Silo 1Document4 pagesSilo 1api-372418362No ratings yet
- Theory of Bureaucratic CaringDocument32 pagesTheory of Bureaucratic CaringAnn NiNo ratings yet
- Ptpmcrender FcgiDocument10 pagesPtpmcrender FcgiAndres Felipe Quimbayo CifuentesNo ratings yet
- Medical Coder / BillerDocument1 pageMedical Coder / Billerapi-77384278No ratings yet
- Employee Engagement in MOH-consolidatedDocument30 pagesEmployee Engagement in MOH-consolidatedMalak MagablehNo ratings yet