Professional Documents
Culture Documents
Immunopathologic study reveals role of T cells and HLA-DR in fixed drug eruption
Uploaded by
Dian Eka PermataOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immunopathologic study reveals role of T cells and HLA-DR in fixed drug eruption
Uploaded by
Dian Eka PermataCopyright:
Available Formats
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
Immunopathologic study of fixed drug eruption
Iman Abd El Fattah Seleit, Mohamed Ahmed Basha, Nansy Youssef Asaad , Ola Ahmed Amin
Department of Dermatology and Andrology* and Pathology, Faculty of Medicine Menoufiya University
drola_2007@yahoo.com
Abstract: Background: Fixed drug eruption (FDE) is a common drug induced dermatosis that can be caused by a
variety of drugs. Although effector and regulatory T cells play a role in progression and resolution of FDE, little in
vivo data exist regarding T cell dynamics in its pathogenesis. Objectives: To through light on the
immunopathogenesis of FDE through studying the participation of CD8+, CD4+ T cells and HLA-DR antigen in the
pathogenesis of lesions. The role of serum Ca was studied. Patients and methods: Thirty skin biopsy specimens from
FDE skin lesions were used (16 active lesions& 14 healed lesions). Thirty biopsy specimens from thirty age and sex
matched healthy subjects were used as a control group. Histopathological examination of hematoxylin& eosinstained sections included analysis and scoring of histopathological parameters was done. Expression of CD4, CD8
and HLA-DR antigens was examined immunohistochemically. Blood samples were collected from patients and
control subjects for assesment of serum calcium. Results: Active lesions showed interface dermatitis and dermal
inflammatory infiltrate. Positive immunostaining was observed in both epidermis and dermis for HLA-DR, CD4 and
CD8 antigens. Healed lesions showed epidermal atrophy and dermal inflammatory infiltrate. Positive
immunostaining was observed in both epidermis and dermis for HLA-DR, CD4 and CD8 antigens. Such results
were absent in control sections. Both total and ionized Ca2+ were significantly lower in patients than control
subjects. Conclusions: Activation of T cells residing in resting FDE lesions by ingestion of the causative drug results
in epidermal injury possibly through the production of IFN-.
[Iman Abd El Fattah Seleit, Mohamed Ahmed Basha, Nansy Youssef Asaad, Ola Ahmed Amin.
Immunopathologic study of fixed drug eruption. Report and Opinion 2011;3(2):14-23]. (ISSN: 1553-9873).
http://www.sciencepub.net.
Keywords: FDE, CD4+T cells, CD8+T cells, IFN-
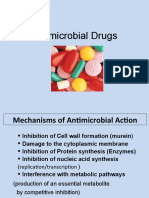
have the key role in mediating the localized
epidermal injury through the production of IFN-
upon stimulation at an early time point (2 to 3h after
challenge).7 In addition, CD8+ T cells might also
contribute to the development of FDE lesions by
directly interacting with other inflammatory cells.8
Recombinant INF- induced the expression
of the class II antigens HLA-DR and HLA-DQ as
well as ICAM-1 on human keratinocytes. Low Ca
level will lead to over expression of HLA-DR, HLADQ and ICAM-1 on keratinocytes. Surface
expression of ICAM-1 is suggested to be of major
importance as recognition molecule by which T cells
bind to IFN- exposed keratinocytes and suggests an
integral role for this molecule in epidermal
lymphocyte traffecking. 9
Shiohara10 postulated that intraepidermal T
cells may represent double-edged swords with
protective
and
destructive
capacity.
The
epidermotropic migration of CD4+ T cells into the
epidermis protect against the tissue damaging effect
of intraepidermal CD8+ T cells residing in the resting
lesions. Interestingly enough, at the same time, other
populations of CD4+ T cells may preserve their
helper function for the CD8+ T cells.
The aim of this work is to investigate the
expression of keratinocytes HLA-DR in fixed drug
1. Introduction
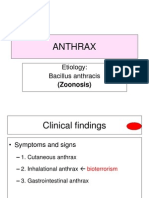
Cutaneous drug eruptions are the most
common adverse reactions attributed to drugs.1 In
1889, Bourns described a patient who had ingested
20 g of antipyrine and then developed a series of
sharply demarcated hyperpigmented lesions on the
lips and tongue. The French term, eruption
erythemato-pigmentee fixe, was coined by Brocq few
years later from which fixed drug eruption was
derived.2 Fixed drug eruption (FDE) is a distinct,
drug-induced dermatosis characterized by relapse of
lesions in the same location every time the drug is
administered,3 a phenomenon referred to as the
recall response or the isotopic response.4
Scherer and Bircher5 stated that although the
pathogenesis of FDE is unknown, many factors had
been claimed to share in lesion development
including antibodies, antibody-dependent cellular
cytotoxicity and serum factors.
Fixed drug eruption had been classified as a
type IV immunologic reaction because of a latent
cytotoxic T cells in the lesions, which may become
reactivated. There is also an association with HLA
class II antigens, suggesting that there may be a
genetic predisposition to these reactions.6
There is a strong evidence that
intraepidermal CD8+ T cells residing in FDE lesions
http://www.sciencepub.net
14
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
eruption and to study the immunological role of
CD8+ and CD4+ effector T cells in the pathogenesis
of
this
disease
entity
through
their
immunohistochemical staining. A spot of light will
by thrown on the role played by extracellular
calcium.
Weak: < 10 % of cells showed positive staining,
mild: 10- 20 % of cells showed positive staining,
moderate: 20-50 % of cells showed positive staining,
and severe: > 50 % of cells showed positive staining
.12
Measurement of total and ionized serum calcium:
Blood samples were collected from patients and
control at the same time of biopsy taking. Samples
were left for half an hour till sedimentation occurs.
Serum was separated from RBCs and centrifugated.
No additive was used.
1- Total Ca: Ca with o-cresolphthalin complex
compound yields a red coloured complex at
alkaline PH whose intensity is proportional to
the Ca concentration. Using kits for Ca
spinreact.10
2- Ionized Ca: Using ion selective electrode method
by VAL 9180 analyzer.10
2. Patients and Methods:
Our study is a case control study that was
carried out on thirty patients presented with FDE
recruited from Dermatology outpatient clinic,
Menoufiya
University
Hospital,
Menoufiya
Governorate, Egypt. The study was performed during
a period of 6 months from September2009 to March
2010.
Patients were divided according to Hindsen et al.11
into:
A) Sixteen patients with active lesions (within 48
hours of appearance of
eruption)
B) Fourteen patients with healed lesions (after 21
days from the appearance of eruption)
Thirty age and sex matched healthy volunteers were
selected as a control group.
Prior to initiation of the study, every subject was
informed about the aim of the study and gave a
written consent. Each case and control was subjected
to brief history taking.
Histopathological evaluation:
Skin biopsies from both patients and controls
were taken by 4 mm punch biopsy under local
anesthesia. They were stained with hematoxylin and
eosin to evaluate FDE pathology and with
monoclonal antibodies: anti HLA class II (DP-DQDR) antigen clone IQug, IgG2a class, lyphilised 1 ml
[Novocastra, UK], Anti CD8 clone 1A5, IgG1 class,
ready to use [Novocastra, UK] and Anti CD4 clone:
IF6, IgG1 class, ready to use [Novocastra, UK] to
detect the immunohistochemical expression of HLADR, CD8+ and CD4+ T cells. The detection kit is
ultravision
Detection
system
antipolyvalent,
HRP/DAB plus, ready to use [Neomarkers' TP-015HDX].
Immunostaining interpretation positivity:
HLA-DR, CD8 and CD4 antigens give
membranous immunostaining positivity. The scoring
of the section was carried out by using binocular
Olympus light microscope (field size of 0.274 mm
and field diameter of 0.59 mm).
The positivity was identified when the cell membrane
showed brown staining whereas negativity was
considered when no staining was identified.12
Statistical analysis:
Data collected, tabulated and then statistically
analyzed by SPSS (SPSS INC. Chicago, IL, USA)
version 13 statistical package and state view
software. Two types of statistics were done:
Descriptive statistics: number, percentage, mean (x)
and standard deviation (SD) Analytical statistics:
difference in proportion was tested by applying
student t test. Level of significance was set as p-value
< = 0.0513.
3. Results
Patient characteristics:
Thirty patients were enrolled into the study.
They were 16 females and 14 males. Their ages
ranged from 6 to 54 years with a mean age of 19.26
years.
The most likely responsible drugs enrolled
in this study were: co-trimoxazole (13/30 cases),
tetracycline (4/30 cases), ibuprofen (3/30 cases),
griseofulvin (3/30 cases), dipyrine (1/30 case),
metronidazole (1/30 case), amoxicillin (1/30 case),
acetyl salicylic acid (1/30 case), belladonna (2/30
cases) and mebendazole (1/30 case).
From the clinical point of view, 22 cases
were presented with macular lesions, 5 cases were
presented with oral and\or genital ulcers, two cases
were presented with bullous lesions and one case was
presented with papular lesions. Lesions were multiple
in 16 cases, few in 12 cases and solitary lesion was
detected in 2 cases. In 11 cases, skin lesions were
associated with oral affection while in 6 cases they
were associated with genital affection.
The intensity of staining was scored as :
0:- ve , 1: weak , 2: moderate, 3: intense
The percentage of positive cells was graded as:
http://www.sciencepub.net
Histopathological results:
Active lesions: Epidermal changes: spongiosis (Fig.
1a), acanthosis, necrotic keratinocytes appearing as
15
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
homogenous hyperesinophilic bodies (Fig. 1b) and
vacoulization of basal layer of the epidermis (Fig. 1c)
with subepidermal bulla (Fig. 1d) (Tab. 1).
Superficial ulceration was detected in 5 cases.
Dermal changes: all cases showed
inflammatory infiltrate in the form of plasma cells,
lymphocytes and macrophages (Fig. 2a) in
angiocentric (Fig. 2b), periadnexal (Fig. 2c) and
epidermotropic localization (Fig. 1a, 1c, 2c) in
addition to melanin incontinence (Fig. 1a, 1c), dermal
edema, angiogenesis and dilated superficial
(a
(c
lymphatics. Lichenoid reaction was noted in some
cases (Fig. 2a) (Tab. 2).
Healed lesions: Epidermal changes: all the 14 cases
of chronic FED showed epidermal atrophy (Fig. 2d)
(Tab. 1).
Dermal changes: dermal inflammatory infiltrate in
the form of plasma cells, lymphocytes and
macrophages in angiocentric distribution (Fig 2d). In
addition there were prominent angiogenesis, dilated
superficial lymphatics and superficial nerve
proliferation (Tab. 2).
(b
(d
Fig. (1): H& E stained sections a) Accumulation of the inflammatory cells within the epidermis [epidermotropism]
with spongiosis [X520]. b) Necrotic keratinocytes appearing as hypereosinophilic bodies in epidermis (green arrow)
[X520]. c) Vaculated basal keratinocytes due to creeping of lymphocytes that focally obliterate dermo-epidermal
junction. Melanin incontinence is also present [X260]. d) Early blister cavity at dermo-epidermal junction [X260].
http://www.sciencepub.net
16
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
(a
(b
(c
(d
Fig. 2: H&E stained sections. a) Dermal inflammatory infiltrate made of lymphocytes in a lichenoid pattern with
epidermotropism [X130]. b) Angiocentric distribution of inflammatory cells [X260]. c) Periadnexyal accumulation
of the inflammatory cells with multifocal epidermotropism [X130]. d) Healed FDE showing epidermal atrophy with
flattening of rete ridges [X260].
Table (1): histopathological epidermal changes in cases of active and healed FDE:
Active
Histopathological finding
Healed
No
No
Atrophy
14
100
Acanthosis
37.5
Spongiosis
11
68.75
Necrotic keratinocytes
50
Hydropic degeneration
31.25
Sub epidermal bulla
12.5
http://www.sciencepub.net
17
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
Table (2): histopathological dermal changes in cases of active and healed FDE:
Histopathological finding
Inflammatory infiltrate
Plasma cells
Lymphocytes
Macrophages
Esinophils
Neutrophils
Density of infiltrate
Mild
Moderate
Severe
Localization
Angiocentric
Lichenoid
Periadnexal
Epidermotropic
Dermal edema
Angiogenesis
Melanin incontinence
Dilated up. Lymphatics
Sup. nerve proliferation
Active
No
16
16
16
16
12
3
%
100
100
100
100
75
18.75
Healed
No
14
14
14
14
10
0
%
100
100
100
100
71.4
0
0
8
8
0
50
50
6
8
0
42.8
57.2
0
16
6
16
16
16
16
16
4
0
100
37.5
100
100
100
100
100
25
0
14
0
6
0
6
14
10
10
8
100
0
42.8
0
42.8
100
71.4
71.4
57.2
up. upper, sup. superficial
4a) (Tab. 3). CD4+ T cells could be identified in
epidermis in 87.5 % of cases and in the dermis in
68.75% of cases (Fig. 4b) (Tab. 3). Such epidermal
and dermal findings were absent in control
specimens.
Immunostaining results:
a) HLA-DR:
- Active lesions:
HLA class II antigens were demonstrated in
93.75% of cases both in the epidermis and dermis
(Fig. 3a) (Tab. 3).
-Healed lesions:
CD8+ T cells were identified in 93.75% and
87.5% in the epidermis and dermis respectively (Fig.
4c) (Tab. 3). CD4+ T cells were detected in
epidermis in (21.4%) of cases while in dermis they
were detected in 50% cases (Fig. 4d) (Tab. 3). Such
epidermal and dermal findings were absent in control
specimens.
- Healed lesions:
HLA class II antigens were positive in 93%
and 87.5% of cases in the epidermis and the dermis
respectively (Fig. 3b) (Tab. 3).
b) CD4+ and CD8+ T cells:
- Active lesions:
CD8+ T cells were identified in 93.75% and
87.5% in the epidermis and dermis respectively (Fig.
http://www.sciencepub.net
18
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
(a
(b
Fig 3: Immunostaining of HLA-DR antigen a) Active FDE with evident strong and moderate expression in dermal
inflammatory cells and basal keratinocytes. [immunoperoxidase with mayer's Hx counter stain X130]. b) Healed
FDE showing strong and severe HLA-DR positivity in both angiocentric and periadnexal inflammatory cells, in
addition to few keratinocytes [immunoperoxidase with mayer's Hx counter stain X 260].
Table (3): HLA-DR, CD8 and CD4 immunostaining results in cases of active and healed FDE:
Immunostaining
Active
Healed
Epidermal
Dermal
Epidermal
Dermal
No
No
No
No
HLA-DR
15
93.75
15
93.75
13
92.8
12
85.7
CD8
15
93.75
14
87.5
13
92.8
12
85.7
CD4
14
87.5
11
68.75
21.4
50
Regarding serum Calcium determination, it was found that both total and ionized Ca2+ were significantly lower
(7.9 1.3 and 3.50 0.5 respectively) in patients as compared to controls (9.2 1.9 and 3.96 0.9 respectively) (Tab.
4).
Table (4): Serum Ca (total & ionized) in patients and control:
Patients
Control
t test
P value
Total Ca
7.9 1.3
9.2 1.9
2.43
<0.05
Ionized Ca
3.5 0.5
3.96 0.9
2.04
<0.05
S , significant.
Normal total Ca, 9-10.5 mg%.
Normal ionized Ca, 4.4-5.6 mg%.
Significant difference was obtained between levels of serum calcium (both total and ionized) in patients and controls
http://www.sciencepub.net
19
editor@americanscience.org
Report and Opinion, 2011;3(2)
(a
(c
http://www.sciencepub.net/report
(b
(d
Fig. 4: a) Immunostaining of CD8 antigen in a case of active FDE showing strong and moderate reactivity in dermal
inflammatory cells and few keratinocytes [immunoperoxidase with mayer's Hx counter stain X130]. b)
Immunostaining of CD4 antigen in active FDE showing strong and moderate reactivity in keratinocytes and dermal
inflammatory cells [immunoperoxidase with mayer's Hx counter stain X130]. c) Immunostaining of CD8 antigen in
a case of healed FDE showing strong and moderate reactivity localized to the angiocentric inflammatory cells
[immunoperoxidase with mayer's Hx counter stain X260]. d) Immunostaining of CD4 antigen in healed FDE
showing strong staining but mild positivity of few keratinocytes and dermal inflammatory cells [immunoperoxidase
with mayer's Hx counter stain X260].
agent used in a given part of the world. So it varies
from country to country and from time to time
according to the drugs in use.13
4. Discussion:
Fixed drug eruption is a very distinctive
variant of drug induced dermatoses with
characteristic recurrence at the same site of the skin
or mucous membrane. The incidence of FDE induced
by a specific drug depends on the frequency of the
http://www.sciencepub.net
20
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
Although the pathogenesis of FDE is
unknown, many factors had been claimed to share in
lesion development.5
In this study, a strong HLA-DR positivity
was observed in keratinocytes, both in active and
healed lesions. This result in acute stage was in
accordance with Hindsen et al.11 & Baran and
Perrin14. In healing stage, HLA-DR positivity was
similar to Smolle15 and contrary to what was found by
Hindsen et al.11 who reported that this positivity was
acquired only during the acute inflammatory phase
and not during the healing phase. This controversy
may be attributed to the difference in the number of
patients included in each study.
HLA-DR positivity may be explained to be
due to synthesis of IFN- by Th cells that stimulates
HLA-DR expression on T lymphocytes and
keratinocytes. The more activated T lymphocytes in
the dermis, the more HLA-DR expression in the
overlying epidermis.16 An association between HLA
types and susceptibility to drug eruption has been
reported on several occasions.17
Immunostaining results demonstrated that in
active lesions, both CD8+ T cells and CD4+ T cells
were detected in the epidermis and dermis in 93.75%,
87.7% and 87.5%, 68.75% respectively. On the other
hand, CD8+ T cells and CD4+ T cells were detected
in the epidermis of healed lesions in 93.75 % and
21.4 % respectively. These results were in
accordance with Mizukawa et al.7 who reported that
CD8+ T cells as well as CD4+ T cells were observed
within the epidermis and dermis during the evolution
phase. CD4+ T cells declined after the resolution
phase and CD8+ T cells are selectively retained in the
chronic FDE lesions. These observations may be
related to the ability of effector memory CD8+ T
cells to be efficiently retained in the epidermis. This
retention ability of CD8+ T cells within the epidermis
was attributed to receptor expression on these cells;
E, a molecule required for retention within the
epidermis which is not found on CD4+ T cells.18
Shiohara et al.8 have shown that
intraepidermal CD8+ T cells phenotypically resemble
effector memory T cells and are greatly enriched in
the resting lesions of FDE. Although these cells have
been implied as the mediators of protection, they
have an opposite action, a detrimental effect on the
epithelial tissue. Mizukawa et al.19 concluded that T
cells residing in the lesions upon activation, by
ingestion of the causative drug, can rapidly produce
large amounts of IFN- followed by localized
epidermal injury. Their activation is probably
essential for the initiation of deletrious inflammatory
responses in the lesions. Such early IFN- production
in situ was only observed in the intraepidermal T
cells resident in the lesions but not those in
http://www.sciencepub.net
perilesional skin and consequently progressed to
localized epidermal injury. IFN - induces the
expression of class II antigen HLA-DR and HLA-DQ
as well as ICAM-1 on human keratinocytes. Koide et
al.20 demonstrated that the expression of HLA-DR on
the surface of keratinocytes by IFN- may be
calcium/calmodulin and not a protein kinase-C
mediated event. IFN- induction of ICAM-1 is also
mediated via calmodulin-dependent pathway.
Gunhild et al.18 reported that there was an association
between the severity of the lesion and co-expression
of ICAM-1 and HLA-DR. This may be due to a
quantitative difference in the amount of T cell
lymphokines present at the lesion as IFN- and IL-1.
The in situ studies indicated that CD8+ T
cells persist in a state of activation in the resting FDE
lesions and are capable of acquiring potent cytotoxic
activity with rapid kinetics on clinical challenge.8
Teraki and Shiohara21 demonstrated that most of the
intraepidermal CD8+ T cells were capable also of
producing IFN- with little IL2 and IL4. On
rechallenge, a significant number of CD4+ T cells
capable of producing IL10 migrate into the lesional
epidermis. These effector IFN- producing CD8+ T
cells and regulatory IL10 producing CD4+ T cells
may be responsible for the progression and resolution
of FDE. Shiohara and Mizukawa22 stated that the
rapid release of IFN- will also initiate the release of
perforin, granzyme B and other cytokines.
In the current study, it was found that both
serum total and ionized Ca were significantly
decreased than their determined values in controls.
The low levels were consistent with previous report
by Griffiths et al.9 who demonstrated that the ability
of IFN- to produce contrasting and distinctive cell
surface and intercellular expression of HLA-DR,
HLA-DQ and ICAM-1 antigens on keratinocytes is
dependent on levels of serum Ca. keratinocytes
grown in medium supplemented with Ca and 10%
fetal calf serum underwent differentiation with a
diminshed expression of all three antigens as
compared to those grown in low calcium and serum
free medium.
Choi et al.23 suggested that the initial
epidermal injury occurs mainly due to CD8+ T cell
activation but the full blown picture requires an
orchestration of multiple mechanisms. Teraki et al.24
added that intraepidermal T cells have a cytolytic
machinery. Thus, granule exocytosis is also likely the
important pathway of cytotoxicity mediated by
intraepidermal CD8+ T cells. The production of early
IFN- burst could prime other immune cells, such as
macrophages, to produce large amounts of TNF-25
which causes extensive epidermal damage by
inducing the expression of apoptosis-associated
proteins such as Fas, Fas L and TNF-related
21
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
apoptosis-inducing ligand (TRAIL).26 TNF- as well
as IFN- was found to be one of the first cytokines to
appear in the bloodstream, followed by IL-6 in a
patient with multiple FDE after clinical challenge.3
8. Hager J L, Mir M R, Hsu S. Fluoroquinoloneinduced generalized fixed drug eruption. DOJ
2009; 15 (12): 8-10.
9. Hindsen M, Christenen OB, Gruic V. Fixed drug
eruption: an immumohistochemical invstigation
of acute and healing phase. British J Dermatol
1987; 116:351-60-68.
10. Koide Y, Ina Y, Nezu N. Calcium influx and the
Ca2+-calmodulin complex are involved in
interferon gamma -induced expression of HLA
class II molecules on HL-60 cells. Proc Nat Acad
Sci 1988; 85:3120-24.
11. Korkij W, Soltani K. Fixed drug eruption. Arch
Dermatol 1984; 120: 520-24.
12. Grafen A, Hails R. Modern statistics for life
sciences. New York: Oxford Univ. Press; 2009.
13. Mizukawa Y, Yamazaki Y, Teraki Y. Direct
evidence for interferon- production by effectormemory-type intraepidermal T cells residing at
an effector site of immunopathology in fixed
drug eruption. Am J Pathol 2002; 161: 1337-47.
14. Nishimura H, Emoto M, Hiromatsu K. The role
of T cells in priming macrophages to produce
tumor necrosis factor-. Eur J Immunol 1995;
25:1465-68.
15. Nordlund JJ, Boissy RE, Hearing VJ. The
Pigmentary
System:
Physiology
and
Pathophysiology. New York: Oxford Univ.
Press; 1998.
16. Raksha MP, Marfatia YS. Clinical study of
cutaneous drug eruptions in 200 patients. IJDVL
2008; 74 (1): 80.
17. Scherer K, Bircher AJ. Hypersensitivity
reactions to fluoroquinolones. Curr Allergy
Asthma.Rep 2005; 5: 15-21.
18. Sehgal VN, Srivastava G. Fixed drug eruption
(FDE) changing scenario of incriminating drugs.
Int J Dermatol 2006; 45(8):897-08.
19. Shiohara T. Fixed drug eruption: pathogenesis
and diagnostic tests. Curr Opin Allergy Clin
Immunol 2009; 9(4):316-21.
20. Shiohara T, Mizukawa Y. Fixed Drug Eruption:
Easily Overlooked but Needing New Respect.
Dermatol 2002; 205:103-04.
21. Shiohara T,
Mizuakwa Y,
Teraki Y.
Pathophysiology of fixed drug eruption: the role
of skin-resident T cells. Curr Opin Allergy Clin
Immunol 2002; 2: 317-23.
22. Shiohara T, Mizukawa Y. Recall phenomenon:
Some skin-resident cells remember previous
insults. Dermatol 2003; 207: 127-29.
23. Smolle J. HLA-DR antigen bearing keratinocytes
in various dermatologic disorders .Acta Derm
Venereol 1985; 65: 69-74.
24. Suk K, Kim S, Jim YH. IFN-/TNF- synergism
as the final effector in autoimmune diabetes: a
Conclusion: activation of residing T cells in the FDE
lesions by ingestion of a causative drug can rapidly
produce localized epidermal injury possibly through
release of large amounts of IFN-. The in situ studies
indicated that these cells persist in a state of
activation in the resting FDE lesions and are capable
of acquiring potent cytotoxic activity with rapid
kinetics on clinical challenge.
Acknoledgement:
We are grateful to the members of the
Biochemistry Department, Faculty of Medicine,
Menoufiya University, Menoufiya, Egypt for their
cooperation and help.
Corresponding author:
Ola Ahmed Amin
Address: Egypt, Menoufiya Governorate, Shibin el
koom, Faculty of Medicine, Department of
Dermatology and Andrology
Email: drola_2007@yahoo.com
References
1. Aubock J, Romani N, Grubauer G. HLA-DR
expression on keratinocytes is a common feature
of diseased skin. British J Dermatol 1986; 114:
465-72.
2. Baran R, Perrin C. Fixed-drug eruption
presenting as an acute paronychia. British J
Dermatol 1991; 125: 592-95.
3. Barker J, Navsaria H, Leigh I. Gamma-interferon
induced
human
keratinocytes
HLA-DR
synthesis: the role of dermal activated T
lymphocytes. British J Dermatol 1988; 119: 56772.
4. Breathnach S M. Drug Reactions. In: textbook of
dermatology (Champion R, Burnor J, Bburnsr D,
eds), 6th edn. Oxford: Blackwell Science Ltd,
1998 ; 3349-517-560.
5. Choi HJ, Ku JK, Kim MY. Possible role of
Fas/Fas ligand-mediated apoptosis in the
pathogenesis of fixed drug eruption. British J
Dermatol 2006; 154: 419-25.
6. Griffiths C, Voorhees J, Nickoloff BJ. Gamma
interferon induces different keratinocytes cellular
patterns of expression of HLA-DR and DQ and
intercellular adhesion molecule-1 (ICAM-1)
antigens; British J Dermatol 1989; 120:1-7.
7. Gunhild L W, Elisabeth R, Steen L. The role of
intercellular adhesion molecules in inflammatory
skin reactions. British J Dermatol 1988; 119:
141-45.
http://www.sciencepub.net
22
editor@americanscience.org
Report and Opinion, 2011;3(2)
http://www.sciencepub.net/report
key role for STAT1/IFN regulatory factor-1
pathway in pancreatic beta cell death. J Immunol
2001; 166: 4481-89.
25. Teraki Y, Moriya N, Shiohara T. Drug-induced
expression of intracellular adhesion molecule-1
on lesional keratinocytes in fixed drug eruption.
Am J Pathol 1994, 145: 550-60.
26. Teraki Y, Shiohara T. IFN gamma producing
effector CD8+ T cells in fixed drug eruption. J
Allergy Clin Immunol 2003; 112(3): 609-15.
12/6/2010
http://www.sciencepub.net
23
editor@americanscience.org
You might also like
- Indoleamine 2,3-Dioxygenase (IDO) Is Frequently Expressed in Stromal Cells of Hodgkin Lymphoma and Is Associated With Adverse Clinical Features: A Retrospective Cohort StudyDocument9 pagesIndoleamine 2,3-Dioxygenase (IDO) Is Frequently Expressed in Stromal Cells of Hodgkin Lymphoma and Is Associated With Adverse Clinical Features: A Retrospective Cohort Studybdvd1007092No ratings yet
- Review of Toxic Epidermal NecrolysisDocument10 pagesReview of Toxic Epidermal NecrolysisNurfitri ZuhruhurNo ratings yet
- Jced 7 E656Document4 pagesJced 7 E656María José VázquezNo ratings yet
- Prevalence and Drug Resistance of Nontuberculous Mycobacteria, Northern China, 2008-2011Document2 pagesPrevalence and Drug Resistance of Nontuberculous Mycobacteria, Northern China, 2008-2011Mark ReinhardtNo ratings yet
- Clinicopathological Significance of Fascin and CD44v6 Expression in Endometrioid CarcinomaDocument7 pagesClinicopathological Significance of Fascin and CD44v6 Expression in Endometrioid CarcinomaelisasusantiNo ratings yet
- The Major Orphan Forms of Ichthyosis Are Characterized by Systemic T-Cell Activation and Th-17/Tc-17/Th-22/Tc-22 Polarization in BloodDocument11 pagesThe Major Orphan Forms of Ichthyosis Are Characterized by Systemic T-Cell Activation and Th-17/Tc-17/Th-22/Tc-22 Polarization in BloodGustavo MartínezNo ratings yet
- Dissecting Interferon-Induced Transcriptional Programs in Human Peripheral Blood CellsDocument13 pagesDissecting Interferon-Induced Transcriptional Programs in Human Peripheral Blood CellsKatyusha21No ratings yet
- Efficacy of Doxycycline in The Treatment of Early Stages of Mycosis Fungoides, A Randomized Controlled TrialDocument29 pagesEfficacy of Doxycycline in The Treatment of Early Stages of Mycosis Fungoides, A Randomized Controlled TrialMelvin Florens Tania GongaNo ratings yet
- Investigation of Intertriginous Infections and Their Clinical PresentationsDocument7 pagesInvestigation of Intertriginous Infections and Their Clinical PresentationsKiki FatmawatyNo ratings yet
- Ye 2014Document8 pagesYe 2014dickypranataNo ratings yet
- MMR 9 1 9 PDFDocument7 pagesMMR 9 1 9 PDFIndira Damar PangestuNo ratings yet
- Glucocorticoids and The Immune Function in The Human Immunodeficiency Virus Infection: A Study in Hypercortisolemic and Cortisol-Resistant PatientsDocument4 pagesGlucocorticoids and The Immune Function in The Human Immunodeficiency Virus Infection: A Study in Hypercortisolemic and Cortisol-Resistant PatientsdocumentosdescribdNo ratings yet
- Nejmoa 1114576Document11 pagesNejmoa 1114576mz zumrodinNo ratings yet
- DermatomiositisDocument7 pagesDermatomiositisCarlos CalvoNo ratings yet
- The Immune System and Head and Neck Squamous Cell Carcinoma: From Carcinogenesis To New Therapeutic OpportunitiesDocument18 pagesThe Immune System and Head and Neck Squamous Cell Carcinoma: From Carcinogenesis To New Therapeutic OpportunitiesGlauce L TrevisanNo ratings yet
- In Silico Leishmania Major in VitroDocument13 pagesIn Silico Leishmania Major in VitroshahabNo ratings yet
- Flow Cytometric Characterization of CD7+ Cell Subsets in Normal Bone Marrow for Diagnosis and Follow-Up of T-ALLDocument10 pagesFlow Cytometric Characterization of CD7+ Cell Subsets in Normal Bone Marrow for Diagnosis and Follow-Up of T-ALLKarla Novoa PérezNo ratings yet
- Contribution of CD8+ T Cells To Control of Mycobacterium Tuberculosis InfectionDocument20 pagesContribution of CD8+ T Cells To Control of Mycobacterium Tuberculosis InfectionhelmiprasNo ratings yet
- Ctla4: Immune Dysregulation in Human Subjects With Heterozygous Germline Mutations inDocument8 pagesCtla4: Immune Dysregulation in Human Subjects With Heterozygous Germline Mutations inArie kusuma WijayaNo ratings yet
- JurnalDocument11 pagesJurnalLaksita Balqis MaharaniNo ratings yet
- En V58n5a22Document13 pagesEn V58n5a22M Nurshaffriaal RusdiNo ratings yet
- Biomedicines 10 02105Document16 pagesBiomedicines 10 02105Fatimah AssagafNo ratings yet
- Immune mechanisms and environmental factors in type 1 diabetesDocument9 pagesImmune mechanisms and environmental factors in type 1 diabetesNiko Hizkia SimatupangNo ratings yet
- Art 5Document4 pagesArt 5Emily YuliethNo ratings yet
- Ceftazidime Induced DRESSDocument1 pageCeftazidime Induced DRESSLidwina ElisabethNo ratings yet
- Meningitis TBDocument11 pagesMeningitis TBErni Yessyca SimamoraNo ratings yet
- Histo-Pathological Spectrum of Skin Lesions in Tertiary Care Centre: A Three Year StudyDocument6 pagesHisto-Pathological Spectrum of Skin Lesions in Tertiary Care Centre: A Three Year StudyIJAR JOURNALNo ratings yet
- Vanduin 2007Document7 pagesVanduin 2007arfikNo ratings yet
- Why Have Clinical Trials in Sepsis FailedDocument9 pagesWhy Have Clinical Trials in Sepsis FailedxiaojianNo ratings yet
- Direct Immmuno Flourescence Study in Auto Immune Bullous DisordersDocument3 pagesDirect Immmuno Flourescence Study in Auto Immune Bullous DisordersInternational Organization of Scientific Research (IOSR)No ratings yet
- Expression of Estrogen and Progesterone Receptors and Ki-67 Antigen in Graves' Disease and Nodular GoiterDocument6 pagesExpression of Estrogen and Progesterone Receptors and Ki-67 Antigen in Graves' Disease and Nodular Goiteryenny handayani sihiteNo ratings yet
- Jcir 23 04Document12 pagesJcir 23 04yakalapunagarajuNo ratings yet
- Review: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseDocument11 pagesReview: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseReynalth Andrew Sinaga100% (1)
- Priyadarshini, 2010Document9 pagesPriyadarshini, 2010AmandaNo ratings yet
- Variant of TYR and Autoimmunity Susceptibility Loci in Generalized VitiligoDocument12 pagesVariant of TYR and Autoimmunity Susceptibility Loci in Generalized VitiligoIvo AfianiNo ratings yet
- Ijcm 13 4 99210Document7 pagesIjcm 13 4 99210Nurul Ulya RahimNo ratings yet
- Autologous: Journal HomepageDocument9 pagesAutologous: Journal HomepageSiddharth DhanarajNo ratings yet
- 2014 Research SummitDocument8 pages2014 Research SummitRo KohnNo ratings yet
- Group 5 Pubmed Accepted Results PDFDocument683 pagesGroup 5 Pubmed Accepted Results PDFDnyanesh LimayeNo ratings yet
- Research ArticleDocument10 pagesResearch ArticlePratama Imanuel RawungNo ratings yet
- After CorrectionDocument22 pagesAfter CorrectionRania GebbaNo ratings yet
- Interferon Gamma Production in The Course of Mycobacterium Tuberculosis InfectionDocument9 pagesInterferon Gamma Production in The Course of Mycobacterium Tuberculosis InfectionAndia ReshiNo ratings yet
- Identifying and Quantifying Heterogeneity in High Content Analysis: Application of Heterogeneity Indices To Drug DiscoveryDocument16 pagesIdentifying and Quantifying Heterogeneity in High Content Analysis: Application of Heterogeneity Indices To Drug DiscoveryMuhammad SatrioNo ratings yet
- Idiopathic CD4 Lymphocytopenia: Natural History and Prognostic FactorsDocument9 pagesIdiopathic CD4 Lymphocytopenia: Natural History and Prognostic FactorsBagus PrawiroNo ratings yet
- Clinical Feature and Etiology of Septic Arthritis and Osteomyelitis in ChildrenDocument5 pagesClinical Feature and Etiology of Septic Arthritis and Osteomyelitis in ChildrenIfit Bagus ApriantonoNo ratings yet
- Acne Vulgaris 3Document27 pagesAcne Vulgaris 3Ridho ForesNo ratings yet
- Prognostic Implications of PD-L1 Expression in Patients With Soft Tissue SarcomaDocument7 pagesPrognostic Implications of PD-L1 Expression in Patients With Soft Tissue SarcomaJemma ArakelyanNo ratings yet
- Out 3Document8 pagesOut 3FanialiahsaniNo ratings yet
- Tran 2021Document12 pagesTran 2021Tzeto Han CongNo ratings yet
- EGFR in MEningiomaDocument7 pagesEGFR in MEningiomaApriyanto LatiefNo ratings yet
- High Prevalence of Altered Immunological Biomarkers in A TransgenderDocument5 pagesHigh Prevalence of Altered Immunological Biomarkers in A TransgenderVallejo Romo Alberto CristianNo ratings yet
- PIIS1074761313004378Document14 pagesPIIS1074761313004378ZadorxsNo ratings yet
- Infect. Immun.-2002-Bacellar-6734-40Document7 pagesInfect. Immun.-2002-Bacellar-6734-40Pedro Henrique De MirandaNo ratings yet
- HIV/AIDS Epidemiology, Pathogenesis, Prevention, and Gene TherapiesDocument6 pagesHIV/AIDS Epidemiology, Pathogenesis, Prevention, and Gene TherapiesAlberto PiasentierNo ratings yet
- Allergic Contact Dermatitis To Topical Antibiotics: Epidemiology, Responsible Allergens, and ManagementDocument21 pagesAllergic Contact Dermatitis To Topical Antibiotics: Epidemiology, Responsible Allergens, and ManagementCrhistian Toribio DionicioNo ratings yet
- Use of ELISPOT Assay for Monitoring Treatment Response in Pulmonary TB PatientsDocument20 pagesUse of ELISPOT Assay for Monitoring Treatment Response in Pulmonary TB PatientsAdel HamadaNo ratings yet
- Original PapersDocument6 pagesOriginal PapersfxkryxieNo ratings yet
- Secreting CD4 T Cells in Direct Ex Vivo Analysis of Antigen-Specific IFNDocument10 pagesSecreting CD4 T Cells in Direct Ex Vivo Analysis of Antigen-Specific IFNEdy NoveryNo ratings yet
- Tumor Immune Microenvironment in Cancer Progression and Cancer TherapyFrom EverandTumor Immune Microenvironment in Cancer Progression and Cancer TherapyPawel KalinskiNo ratings yet
- Parasitic Infections and the Immune SystemFrom EverandParasitic Infections and the Immune SystemFelipe KierzenbaumNo ratings yet
- 10.struvite StonesDocument11 pages10.struvite StonesDian Eka PermataNo ratings yet
- Epidemiology, History and Regional Diversities of UrolithiasisDocument11 pagesEpidemiology, History and Regional Diversities of UrolithiasisRachmad SanjayaNo ratings yet
- CALCULIDocument9 pagesCALCULIRenard ChristianNo ratings yet
- Herpes Zoster - Associated Erythema Multiforme: Uwe Wollina, Astrid GemmekeDocument3 pagesHerpes Zoster - Associated Erythema Multiforme: Uwe Wollina, Astrid GemmekeDian Eka PermataNo ratings yet
- AnthraxDocument13 pagesAnthraxDian Eka Permata100% (1)
- UROLITIASISDocument5 pagesUROLITIASISIkrima Firda MaharaniNo ratings yet
- Jurnal FDE 2Document6 pagesJurnal FDE 2Dian Eka PermataNo ratings yet
- FDE TreatmentDocument6 pagesFDE TreatmentDian Eka PermataNo ratings yet
- Hotel List Ss West Europe 11d (Ek) 23aprDocument1 pageHotel List Ss West Europe 11d (Ek) 23aprDian Eka PermataNo ratings yet
- Administering Emergency OxygenDocument9 pagesAdministering Emergency OxygenDian Eka PermataNo ratings yet
- Jadwal - 2014 Kegawatdaruratan & Traumatologi Reg - 3Document5 pagesJadwal - 2014 Kegawatdaruratan & Traumatologi Reg - 3Dian Eka PermataNo ratings yet
- Administering Emergency OxygenDocument9 pagesAdministering Emergency OxygenDian Eka PermataNo ratings yet
- Digest: Predictors of Failure of Pneumatic Dilatation in AchalasiaDocument3 pagesDigest: Predictors of Failure of Pneumatic Dilatation in AchalasiaDian Eka PermataNo ratings yet
- EtherDocument4 pagesEtherDian Eka PermataNo ratings yet
- TP Mikro ReproDocument2 pagesTP Mikro ReproDian Eka PermataNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- The Contribution of Chemical Engineering To BiotechnologyDocument18 pagesThe Contribution of Chemical Engineering To BiotechnologyMelisa KumlaliNo ratings yet
- Other Blood Group System AssignmentDocument5 pagesOther Blood Group System AssignmentMary ChristelleNo ratings yet
- Lec 3.ascent of SapDocument97 pagesLec 3.ascent of SapAnnadurai PillaiNo ratings yet
- Understanding Plant Kingdom Through AlgaeDocument19 pagesUnderstanding Plant Kingdom Through AlgaeDivyansha Sharma100% (1)
- JSB 142 108 03Document25 pagesJSB 142 108 03Soma GhoshNo ratings yet
- Pre Transfusion Test Flow ChartDocument1 pagePre Transfusion Test Flow ChartCatherine Constantino BaintoNo ratings yet
- MC 3 Lab - KerolDocument43 pagesMC 3 Lab - KerolMa Carolin De LeonNo ratings yet
- The Effects of Nature of Substrate On TH PDFDocument20 pagesThe Effects of Nature of Substrate On TH PDF6A(24) Marsh WongNo ratings yet
- Chemistry of LifeDocument44 pagesChemistry of Life(25) Yahya Kagan AksunNo ratings yet
- AJMR - 20 September, 2012 IssueDocument110 pagesAJMR - 20 September, 2012 Issuesami_bulut542No ratings yet
- AntibioticDocument84 pagesAntibioticDr. Kalavati PrajapatiNo ratings yet
- Chapter 1-5 PDFDocument77 pagesChapter 1-5 PDFEstebanNo ratings yet
- Applications of PCRDocument11 pagesApplications of PCRMustafa KhandgawiNo ratings yet
- Blood and Cell Physiology MCQs With KeyDocument9 pagesBlood and Cell Physiology MCQs With KeyMudassar Roomi87% (63)
- 02 Flow of Energy in Ecosystems Text-MergedDocument14 pages02 Flow of Energy in Ecosystems Text-Mergedsurya narayanaNo ratings yet
- Cytogenetic AbnormalitiesDocument48 pagesCytogenetic AbnormalitiesGlomelyn Rose Ortiz TañedoNo ratings yet
- DJ (Microtubules, Microfilaments and Intermediate Filaments) - DJGFDocument43 pagesDJ (Microtubules, Microfilaments and Intermediate Filaments) - DJGFNick_989893No ratings yet
- Ruthenium in Medicine: Current Uses and Future Prospects: ClinicalDocument8 pagesRuthenium in Medicine: Current Uses and Future Prospects: ClinicalMuhammad Adlan RasyidiNo ratings yet
- GenePix GPR File Pre-Processing Engine PDFDocument50 pagesGenePix GPR File Pre-Processing Engine PDFscjofyWFawlroa2r06YFVabfbajNo ratings yet
- Ocean & EstuariesDocument5 pagesOcean & EstuariesSiva PrasadNo ratings yet
- Bordetella: Bordetella Organisms Are Small, Gram-Negative Coccobacilli Which Are Strict Aerobes. The ThreeDocument7 pagesBordetella: Bordetella Organisms Are Small, Gram-Negative Coccobacilli Which Are Strict Aerobes. The ThreeFlor OMNo ratings yet
- TF1820533 PDFDocument2 pagesTF1820533 PDFPrenoojNo ratings yet
- A New Genetic Form of Autism: Antitumor Duality of ApoeDocument1 pageA New Genetic Form of Autism: Antitumor Duality of ApoeMariana CotaNo ratings yet
- MLE-01 QP 14-7-19 @onlinelibraryindia Neet 2020Document20 pagesMLE-01 QP 14-7-19 @onlinelibraryindia Neet 2020anji shNo ratings yet
- Job Safety Analysis Blood WorkerDocument105 pagesJob Safety Analysis Blood Workermybubbles69No ratings yet
- Evolutionary Dynamics Exploring The Equations of LDocument75 pagesEvolutionary Dynamics Exploring The Equations of LClaudia AndreeaNo ratings yet
- Biochemistry of MuscleDocument68 pagesBiochemistry of MuscleWisnu KuncoroNo ratings yet
- Nutrigenomics PDFDocument32 pagesNutrigenomics PDFpoonam_mittal100% (4)
- Modelling DNADocument6 pagesModelling DNADaniel BerryNo ratings yet
- Energy GenerationDocument4 pagesEnergy GenerationDeena ChadiNo ratings yet