Professional Documents
Culture Documents
Early Events in The Pathogenesis of Epithelial Ovarian Cancer-Printed
Uploaded by
doddydrOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Early Events in The Pathogenesis of Epithelial Ovarian Cancer-Printed
Uploaded by
doddydrCopyright:
Available Formats
VO L UM E 26 NUM B ER 6 F EB RUA RY 20 2 008
JOURNAL OF CLINICAL ONCOLOGY BIOLOGY OF NEOPLASIA
Early Events in the Pathogenesis of Epithelial
Ovarian Cancer
Charles N. Landen Jr, Michael J. Birrer, and Anil K. Sood
F ro m t h e De par t me nt of G yneco log ic
ABSTRACT
O nco log y and t h e De par t me nt of
Ovarian carcinogenesis, as in most cancers, involves multiple genetic alterations. A great deal
has been learned about proteins and pathways important in the early stages of malignant
M .D . An de r son Can cer Cen t er , Hou stransformation and metastasis, as derived from studies of individual tumors, microarray data,
t on , TX ; an d t he Cent e r f or Cance r
animal models, and inherited disorders that confer susceptibility. However, a full understandRe sear ch, Nat i onal Cancer I nst i t ut e,
S ub mit t e d Janu ar y 8, 200 7; accept e d ing of the earliest recognizable events in epithelial ovarian carcinogenesis is limited by the lack
Be t hesd a, M D.
M ay 25, 2 007 ; p ubl ishe d on lin e ahe ad of a well-defined premalignant state common to all ovarian subtypes and by the paucity of data
o f p r int at w w w . jco .o r g on Januar y 1 4, from early-stage cancers. Evidence suggests that ovarian cancers can progress both through
2S 008
. t e d in par t by t h e Rep r odu ct ive a stepwise mutation process (low-grade pathway) and through greater genetic instability that
up por
leads to rapid metastasis without an identifiable precursor lesion (high-grade pathway). In this
S cien t ist De velo pm ent P r og r am
t hr o ug h NI H G ran t No. 5 K1 2HD 008 49 review, we discuss many of the genetic and molecular disorders in each key process that is
an d t he Ovar i an Cance r Resear ch Fun d altered in cancer cells, and we present a model of ovarian pathogenesis that incorporates the
( C. N. L. ); Gr an t s No. CA 11 079 301 and role of tumor cell mutations and factors in the host microenvironment important to tumor
Clin Oncol
initiation
and 26:995-1005.
progression. 2008 by American Society of Clinical Oncology
CA 1 092 980 1 f r om t he N at ion al I nst i- J
Can cer Bio log y, U nive r sit y of T exas
t ut e s of He alt h ( A. K. S . ); Gr an t N o. P5 0
CA0 836 39 f r o m t he M. D. And er son
Can cer Cen t er O var ian Can cer S peci aliz ed Pr o gr am o f Rese ar ch E xcell ence ; a Ovarian
INTRODUCTION
cancer is the fifth leading cause of cancer deaths among women, and it is the most
f r om t he O var ian Cance r R esear ch
common cause among gynecologic malignanF und
In s
c; di
t hsclosu
e M arr cus
Au
t hor
es ofFop und
ot enatt ion
ial co n- cies.1 The poor ratio of survival to incidence in
( ict
A. K.
and
nt r hamu
r alntRese
ar chepithelial ovarian cancer (EOC) results from
s ofSin.) t; er
estt hane dI aut
or co
r ib ur og
he dNat
t uts es o f the high percentage of cases diagnosed at an
tPio
ns ram
ar e of
f otun
at tiohenal
endI nst
of ti hi
Het al
t h, Na t io na l C a nc er Ins t it u te (M .Jadvanced
. B. ) .
stage. Despite advances in surgery
icl
Co r re spo ndiarng
au e.
t hor : Ani l K . S oo d,
and
chemotherapy,
survival of patients with
M D, Pr o f essor , De par t me nt s of G yneEOC
stands
at
just
45%
at 5 years.1 Although
co log ic O ncol ogy an d Cance r Biol ogy,
the
age
of
biologic
therapies
holds the potential
Un ive rsi t y of Te xas M. D. And er so n
of
improved
responses
in
advanced
and recurCan cer Cen t er , 115 5 He r man P r essl er ,
rent
EOC,
a
greater
impact
could
be
made by
Un it 13 62 , H oust o n, TX 770 30; e- mai l:
20 08 b y Amer i can S ocie t y of Cli nical recognition of high-risk patients and by offeraso od@ md ande r son. or g .
O nco log y
ing risk-reducing surgery, a strategy that has
0 732 -1 83X / 08/ 26 06- 99 5/ $20 .0 0
demonstrated effectiveness in patients with geDO I : 1 0. 12 00/ JCO .2 006 .0 7. 997 0
netic predispositions.2 However, there is significant heterogeneity within the EOC group. For
example, histologically defined subtypes such
as serous, endometrioid, mucinous, and lowand high-grade malignancies all have variable
clinical manifestations and underlying molecular signatures.3 Substantial advances have been
made in understanding the genetic alterations
and biologic processes in ovarian cancer; however, the etiology remains poorly understood.
In this article, we will focus on the current
understanding of the early events in EOC.
P r og ram Pr o ject D evel op men t Gr ant
ETIOLOGY OF SPORADIC
EOC
The ovary is surrounded by a single-cell layer of
peritoneal mesothelium, which is derived from the
coelomic layer during development and which has
the potential to undergo metaplastic transformation
to a more differentiated state.4 Unlike most malignancies, as this epithelium transforms into a malignant phenotype, it becomes more differentiated,
and it can differentiate toward many of the different
cell types found in the mullerian tract, including
those in the fallopian tube, uterus, cervix, and
ovarian stroma.5 It is widely thought that most
ovarian cancers develop from the surface epithelium or postovulatory inclusion cysts that were
subjected to prolonged exposure to hormones or
other chemokines.4
Primary peritoneal
and fallopian tube carcinomas have similar clinical, molecular, and genetic
profiles to ovarian cancers, though some small differences in frequency of specific protein expression
have been described.6 -11 Primary peritoneal carcinomas may,in fact, have a multifocal and polyclonal
origin.12 Therefore, although these entities are often
lumped together with ovarian cancer, there may be
some significant, but currently poorly defined, differences. In fact, recent pathologic examination of
consecutive cases of ovarian, primary peritoneal,
and fallopian tube cancers suggests that a greater
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on March 25, 2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
995
Landen, Birrer, and Sood
percentage of ovarian cancers than originally thought may actually
increased risk of EOC by a factor of 2.8, and of borderline tumors by
have a fallopian origin with metastasis to the ovary.13 However, be4.0,compared with infertile women who were not usingfertility drugs.
cause of the changes in definition, inconsistent reporting of subtypes,
However, subsequent case-control and cohort studies demonstrated
and the paucity of direct comparative studies, these entities will be
inconsistent associations between gonadotropin use and epithelial
considered as variations within a disease and will be considered toovarian carcinoma.25 These studies collectivelysuggest that the condigether in this review.
tion of infertility (or the predisposing condition), rather than fertility
There have been several proposed hypotheses about the under- drug use, is responsible for the increased risk.2 6 From a basic science
perspective, receptors for FSH and LH have been found on 100% of
normal ovarian surface epithelial cells and on 60% of malignant tuhave a known genetic component (Table 1). Importantly, these may
mor cells.27 FSH, LH, and human chorionic gonadotropin (hCG) all
also play a role in the 10% of cases in women with a genetic susceptistimulate proliferation of EOCs and may activate mitogen-activated
bility through BRCA or mismatch-repair gene mutations. These hykinase (MAPK).28 Furthermore, induced overexpression of the FSH
potheses will be reviewed brie y, and they are discussed in greater
receptor led to upregulation of epidermal growth factor receptor
depth inThe
otherobservation
excellent reviews.14,
,1 4b
that14a
women
with a greater number of ovulatory(EGFR), human epidermal growth factor receptor 2 (HER2), and
lying physiological processes that increase the risk of malignant transformation of the ovarian epithelium in the 90% of EOCs that do not
C-MYC.29 Other potential oncogenes upregulated by FSH or LH
cycles have an increased risk of ovarian cancer led to the incessant
treatment in vitro include -catenin, Meis-1, cyclin G2, insulin-like
ovulation hypothesis by Fathalla in 1971.15 According to this hypoth-
growth factor 1 (IGF-1), and -1 integrin.30, 31 To date, no study has
esis, as ovulation occurs, ovarian surface epithelial cells are internal-
demonstrated that exposure to gonadotropins is capable of inducing
ized and damaged, and the subsequent repair mechanisms place the
transformation of ovarian surface epithelium (OSE) cells to a malig-
cells at an increased risk of developing mutations and subsequent
nant phenotype. However, in animal models of implanted tumors,
malignancies. Consistent with this hypothesis, women with a history
exposure to gonadotropins promotes tumor growth,32 angiogenesis,32
vascular endothelial growth factor (VEGF) expression,33 and adhesion.34
of multiple pregnancies,16-1 8Collectively,
increased time of lactation,19
and oralsuggest
these studies
a role for gonadotropins in promoting
rather than of the causation.
ovarian cancer decreases further with the increased occurrence of
Notable hormones have also been implicated in ovarian carcinogenesis. On the basis of epidemiologic studies, progestin-only contraeach of these factors. There is also experimental evidence from
ceptives are as effective as combined oral contraceptive pills in the
primate and other animal models that supports the incessant ovureduction of ovarian cancer risk,23 ,35 and progesterone is the domilation hypothesis.21, 22 However, this theory is somewhat weakened
nant hormone during pregnancy, which also reduces risk.23 Interestby observations that progesterone-only oral contraceptives, which
ingly, use of progestin contraceptives can also decrease ovarian
do not inhibit ovulation, are at least as effective as ovulationtestosterone levels.36 In vitro studies have not, however,demonstrated
inhibiting contraceptives.23 Moreover, women with polycystic
a clear inhibition of cancer cell growth.37 Conditions of increased
ovarian syndrome, who have decreased ovulatory cycles, are at an
Weaknesses in the incessant ovulation theoryand observations of
androgens (eg, polycystic ovarian syndrome, hirsutism, acne) are asincreased risk of EOC.24
an increased risk in infertile women who use fertility drugs led to the
sociated with an increased risk of EOC.24 Androgens represent the
gonadotropin hypothesis, which theorizes that stimulation of the
greatest hormone concentration within a developing follicle,3 8which
ovarian surface epithelium by follicle-stimulating hormone (FSH)
prolongs exposure to the epithelial cells. Androgen receptors are
and by luteinizing hormone (LH) may place the cells at an increased
present on human OSEcells,and they stimulate proliferation.39 There
risk of developing EOC. In 1992, Whittemore et al16 reported a caseis no strong evidence, however, that exposure to androgens induces
control studyin which infertile patients who used fertilitydrugshad an
malignant transformation.
contraceptive use16, 20 are allthe
at a decreased
risk. Moreover,
the riskcancer,
for
progression
of ovarian
Table 1. Hypotheses on Physiologic Susceptibilities to Epithelial Ovarian Cancer
Hypothesis
Proposed Mechanism
Best Evidence
Incessant ovulation OSE damaged during ovulation, with repair making
Risk of EOC decreases with decreased number of
cells susceptible to mutations
cycles, such as pregnancy, lactation, and OCP use
Gonadotropin stimulation Stimulatory effect of FSH and LH promote growth,
Increased EOC risk with infertility, PCOS; Decreased
increased cell divisions, and mutations
risk with progesterone-only OCPs; FSH upregulates
many oncogenes and promotes growth in preclinical
Hormonal stimulation High concentrations of androgens in the tumor models
hirsutism, acne) associatedmicroenvironment
with increased risk,promote carcinogenesis,
Conditions of high circulating androgens (PCOS,
androgens are the dominantwhereas
hormone
progestins
in the decrease risk
inclusion cyst; progestin use decreases risk of EOC,
In ammation Damaged
OSE apoptosis
with ovulation induces in ammation,
induces OSE
which promotes reconstruction and mutation
Possible reduced risk with NSAID use; increased risk
with talc or asbestos; abundance of in ammatory
susceptibility
mediators in tumors
Abbreviations: OSE, ovarian surface epithelium; EOC, epithelial ovarian cancer; OCP, oral contraceptive pill; FSH, follicle-stimulating hormone; LH, luteinizing
hormone; PCOS, polycystic ovarian syndrome.
996
URN AL OF CL I N ICA L O N COL O GY
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on MarchJO 25,
2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
Carcinogenesis of Ovarian Cancer
There is growing interest in the etiologic role of in ammation, Earliest Recognizable Events in Tumor Progression
EOCs, like most cancers, are thought to arise from a single
which accompanies each ovulation, with an associated cytokine release, in ux of in ammatory cells, and tissue reconstruction.26 This multidysfunctional cell in 90% of occurrences. Evidence for the
mechanism has been postulated to stress OSE cells such that they clonality of ovarian cancer lies in the similarity between primary
are predisposed to genetic damage and malignant transformation. and metastatic lesions during the examination of the loss of hetConsistent with this hypothesis,patients with chronic aspirin,nonste-erozygosity (LOH), X-chromosome inactivation, and specific gene
mutations.4 2 The difficulty in describing the earliest events in ovarroidal anti-in ammatory drug, or acetaminophen use have a reduced risk of EOC.40 Downstream effectors of the nonsteroidal ian cancer is in the limited availability of early-stage tumors, the
heterogeneity among individuals, and the genetic instability of
anti-in ammatory drug pathway, such as nitric oxide synthase,
tumors, which makes it difficult to know if detected mutations are
cyclooxygenase-2, VEGF, and NF- B, have been implicated in carcinogenic pathways.40 Patients exposed to in ammation-inducing early or late occurrences.
Genomic comparison of early- versus late-stage, high-grade ovarian
agents, such as talc and asbestos, have been shown in some studies to
cancers. Genomic analysis of high-grade tumors has identified ambe at an increased risk.26 Although talc particles have been found
plification and/or over-expression of numerous genes thought to be
on human and murine ovaries after perineum exposure,41 no
important in the development of ovarian cancer.However,the precise
animal model of ovarian carcinogenesis has been proven with talc
role of these genes in earlycarcinogenesis remains unclear. The applior asbestos exposure.
cation of new genomic technologies, such as comparative genome
Although any of the above mechanisms may play a role in ovarhybridization (CGH) and microarray expression profiling, has helped
ian carcinogenesis in some patients, the modest association with each
elucidate many of the important genetic events that may lead to
suggests that multiple other processes are involved, which cannot be
predicted by clinically recognizable conditions such as nulliparity, ovarian cancer. The ability of these technologies to simultaneously
infertility, or hormone exposure. To detect EOC early or to identifymeasure thousands of genes allows not only the identification of
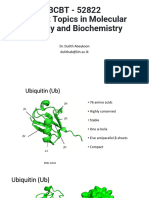
individual genes but also the delineation of dominant pathways that
at-risk patients, a search must therefore continue for genetic or epigefor cancer pathogenesis43
(Fig 1). cells to earlyA responsible
study that compared
normal ovarian,44epithelial
netic conditions that predispose patients to the development of EOCmay be
and late-stage cancers found several differentially expressed genes
or for proteins that may allow for early detection.
Thrombin
Beta-3
integrin Alpha-5
integrin
MT-SP1
PAR1
PAR2
Extracellular
matrix
MAGP2
GG
G
HEF1
SNX1 GPRK5
FAK YES
Fig 1. Pathway identification by microar-
ARHI
ERK
ray analysis. Schematic representation of
potential signaling pathways in ovarian
Cell cycle
progression
RACI CDC42
GD P
GTP GD P
G TP
cancer, identified by incorporating the mi-
VAV3
croarray results (genes differentially expressed between normal and malignant
C CND 1
ovarian epithelial cells) into PathwayAssist.
CCND1
Genes in red are upregulated in cancer
compared with normal ovarian epithelium;
genes in green are downregulated in can-
GATA6
D OC-2
DOC-2
MMP
production
Cytoskeleton
modulation and G
IAP
enhanced
motility
TSP-1
cer; genes in yellow did not show a signif-
MTI-MMP
icant difference between specimens.
Reproduced with permission.43
RECK
Invasion
ETAR
ET-1
www.jco.org
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on March 25, 2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
997
Landen, Birrer, and Sood
been well studied beyond a description of mismatch repair defects.
between normal and malignant tissues.4 5 However, the early- and
Other familial syndromes associated with an increased risk of ovarian
late-stage tumors were remarkably similar. This seems to be at odds
cancer include Peutz-Jeghers Syndrome (ie, mutation in the STK11
with the concept of early-stage tumors that evolve into late-stage ones.
gene; 21% lifetime risk) and Gorlin Syndrome (ie, mutation in PTCH;
20% lifetime risk), but these tumors are usually stromal cancers and
gene abnormalities in late-stage tumors, which was more consistent
fibromas, respectively.
with tumor evolution.Another study that compared tumors collected
Animal models. In an attempt to better understand ovarian
from the several
ovary or theanimals
omentum identified
signature
that
carcinogenesis,
modelsa 27-gene
have been
developed.
Orsulic
could
differentiate
between
the
and
metastatic
Many
of the
genes
areprimary
involved
intransgenic
thetumor.46
p53 pathway,
which suggests
et al5 9 introduced
various
oncogenes
into
ovarian surface
is important
for the peritoneal
metastasis.
The chalepithelial that
cellsthis
thatpathway
expressed
the avian receptor
TVA. These
cells
lenge is in determining
a noted
difference
is truly responsible
became tumorigenic
when two of whether
three genes
(C-MYC,
K-RAS,or
for a particular function, such as malignant transformation or metas-AKT) were overexpressed in p53-deficient cells. After inducing
changes in vitro, they were implanted into the bursal sac that surtasis.For example, metastasized tumors with genetic instability would
continue to acquire genetic mutations that could be erroneously as- rounds the ovary of recipient mice, and they developed a carcinomatosis pattern similar to human ovarian cancer. Subsequently,
signed to causingmetastasis. Additionally, early genetic perturbations
would persist in metastasized tumors and would not be identified asConnolly et al60 generated de novo ovary-specific tumors in transgenic mice that expressed the transforming region of the SV40
an earlyevent when comparing early-and late-stage tumors. However,
llerian inhibitory
T-antigen under control of the ovary-specific Mu
with validation by additional studies that use larger sample sizes, substance
type II receptor gene promoter.In these mice, poorlydiffervarious array platforms to account for methodologic inconsistencies,
entiated tumorsof both ovaries developed in 50% of transfected mice
and microdissected samples to differentiate tumoral and stromal al-and often led to carcinomatosis and ascites formation. A model of
terations, these technologies willallowmore information to be gained
endometrioid ovarian carcinogenesis was described by Dinulescu et
on the
earliest disorders.
events in ovarian
Inherited
A studycancer.
of genetic disorders can provide al,6 1 in which adenoviral vectors were injected into the bursal sac that
great insight into the etiology and early events in carcinogenesis. Heinduced K-RAS overexpression and PTEN inactivation.61 Although
K-RAS overexpression alone induced lesions that were histologically
reditary genetic disorders account for approximately 10% of ovarian
compatible with endometriosis, the combination of both mutations
cancers, and 90% of these are either BRCA1 or BRCA2 mutations.
led to the rapid development of carcinomatosis of endometrioid hisEvaluation of BRCA1 and BRCA2 mutant and sporadic tumors with
tology. Although these models have limited applicability to de novo
gene expression profiling has demonstrated that the greatest contrast
human ovarian cancers because of their different genetic composition,
in expression patterns wasbetween that of BRCA1 and BRCA2 mutant
such as greater homogeneity, diploid status (rather than aneuploid),
tumorsand that sporadic tumorsshared characteristicsof both.47 This
and progression with few mutations, they can provide useful insights
intriguing finding suggests that BRCA1 and BRCA2 tumors may have
into specific gene functions.
variable pathways in carcinogenesis and that even sporadic tumors
may develop as a result of alterations in either pathway. Clinically,
TWO-PATHWAY MODEL OF OVARIAN CANCER
patients with BRCA mutations tend to have highly proliferative tumorsbut more favorable outcomes when adjusted for stage.48 BorderWith the recognition that ovarian tumors are heterogeneous and
line tumors have a much less frequent incidence of BRCA mutations
generate a wide spectrum of disease states, there is growing clinical,
(4.3% v 24.2% in a Jewish population),49 which also suggests a differtranslational, and genetic evidence to support at least two broad cateent molecular
Other thanorigin.
in hereditary syndromes, BRCA genes are rarely muHowever, in the same study, CGH analysis demonstrated acquired
tated in sporadic ovarian cancers,50 although epigenetic changes, alternate splicing,and othergenetic factors mayaffect BRCA function in
as manyas 82% of sporadic occurrences.5 1-53 The BRCA1 and BRCA2
proteins are considered caretakers of the genome,and playkey roles in
the signaling of DNA damage, the activation of DNA repair, the
induction of apoptosis, and the monitoring of cell cycle checkpoints.54 -56 Cells that lack functional BRCA have increased aneu-
gories of carcinogenesis.62 High-grade malignanciesare rapidlygrowing, relatively chemosensitive, and without a definitive precursor
lesion. In contrast, low-grade tumors grow more slowly, are less responsive to chemotherapy, and share molecular characteristics with
low-malignant potential (LMP) neoplasms. Clinically, in a large series
of 112 low-grade patients observed for a median of 71 months, the
average age at diagnosis was 43 years (compared with 61 years for all
ovarian cancers), and the median survival was 81 months63much
ploidy, centrosome amplification, and chromosomal aberrations,57
which make them susceptible to further mutations. BRCA appears to
longer than the 57- to 65-month survival observed in phase III trials
function as a cofactor for a variety of transcription factors, including
that define the standard of care in EOC.64 ,65 Pathologic analysis has
p53, STAT1, c-Myc, JunB, ATF-1, and others.57
found that approximately 60% of low-grade serous carcinomas also con-
Defects in mismatch repair in patients with Lynch syndrome ortain areas of serous LMP tumors compared with just 2% of high- grade,66
and LMP tumors recur as a low-grade carcinoma in 75% of cases.67
hereditary nonpolyposis colon cancer (HNPCC) account for approx- Molecular and protein analyses of tumors of these two different
subtypes also
suggest different
pathogenesiscancers
(Table and
2). Analyses
imately10%
of hereditaryovarian
for 1% toof2% of overall
individualcases.
genesPatients
have found
and however,
BRAF mutations
are carry an
withthat
thisK-RAS
syndrome,
individually
rarely detected
in high-grade
carcinomasovarian
but arecancer.58
present inThe mechaapproximately
12%invasive
risk of developing
30% to 50%
of of
LMP
tumors,risk
in low-grade
and
nism
increased
is through adenocarcinomas,
defects in the mismatch-repair
maoften in the
adjacent
epithelium.62
,68 -70 The
P53
gene cells
is muchinery
andbenign
its resulting
genetic instability
that
places
at risk of
tated in 50%
to 80%
of high-grade
invasive carcinomas,
rarelycancerhas
in
multiple
mutations;
however,carcinogenesis
in but
ovarian
not
998
URN AL OF CL I N ICA L O N COL O GY
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on MarchJO 25,
2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
Carcinogenesis of Ovarian Cancer
Table 2. Variability in Biology of Low- and High-Grade
Tumors
Characteristic LMP/Low-Grade (%) High-Grade (%)
p53 inactivity Rare 50-80
HLA-G overexpression Rare 61
HER2 overexpression Rare 20-66
AKT overexpression Rare 12-30
Apolipoprotein E expression 12 66
B-RAF mutation 30-50 Rare
K-RAS mutation 30-50 Rare
PTEN mutation 20* Rare
MSI
50* 8-28
Abbreviations: LMP, low malignant potential; HER2, human epidermal
growth factor receptor 2; MSI, microsatellite instability.
*Endometrioid.
GENETIC AND PROTEIN ABERRATIONS IN OVARIAN
CANCER
The majority of evidence on genetic or protein alterations in ovarian
cancer is based on studies of late-stage cancers. However, current
understanding of these processes allows speculation that many alterations must occur early to achieve a clinically recognized tumor. It is
believed that, for the majority of malignancies, a cancer cell must
overcome many protective mechanisms to develop into a clinically
evident tumor.84 These include unchecked proliferation, inhibition of
apoptosis, angiogenesis, stromal invasion, separation and survival
away from the primary tumor, and implantation and growth
within new tissues. We examine the evidence for many of the
ever-increasing recognized participants in each of these processes
in ovarian cancer (Table 3).
Self-sufficiency in growth signals. A number of oncogenes have
been identified in ovarian cancer that allow cells to grow independently from the hosts signals. One of the first oncoproteins described
other subtypes or LMPs.71 -73 HER2 and AKT are overexpressed in
was src, a nonreceptor tyrosine kinase that participates in multiple
20% to 67% and 12% to 30% of high-grade carcinomas, respectively,
carcinogenic pathways and promotes proliferation,adhesion, cellsur-
but rarely in low-grade and LMP tumors.74, 75 Overexpression of hu-
vival, and angiogenesis.85-8 7 The overexpression of src has been dem-
man leukocyte antigen-G (HLA-G), which may provide a mechanism
onstrated in 93% of advanced-stage ovarian tumors and in more than
of immune escape for the tumor, hasbeen noted in 61% of high-grade
80% of cell lines.88 This oncoprotein promotes both platinum and
carcinomas but is absent in low-grade or LMP neoplasms.76
taxane resistance and survival in ovarian cancer cell lines.89 FurtherWhole-genome approaches have also provided key insights into
the developmental relatedness of various ovarian tumors. Comparison of whole-genome expression profiles of ovarian tumors of differ-
more, inhibition of src with antisense or with small molecule inhibitors hasThe
reduced
ovarian
cancergrowth
in preclinicalmouse
models.85HER
type
I tyrosine
kinase
receptor family
(ie, Erb) consists
entfour
grades
reveals
that LMPEGFR
tumors
quite distinct
from(encoded
invasive
of
known
monomers:
(ie,are
Erb1/HER1),
HER2
cancers,
and hierarchical
clustering
that they
group on
by
the proto-oncogene
neu),
HER3, demonstrates
and HER4. EGFR
is expressed
closer
to thehuman
normalovarian
ovariansurface
epithelium
than to(as
invasive
cancers.3,
the
normal
epithelium
detected
by immu-77
Furthermore, low-grade invasive cancers were indistinguishable from
nohistochemistry) and is overexpressed in 35% to 70% of EOCs.90
borderline tumors
but were distinct
tumors. More
HER2 has no extracellular
ligand-binding
domain,from
but ithigh-grade
is activated
detailed
analyses
identified
specific
pathways,
when dimerized
with other
typehave
I receptors.
HER2
expression
in which correlate
each
specific
tumor type. One
predominant
pathway
ovarian cancerwith
varies
widely;
overexpression
is found
in 20% to
30% present in
of cases.9 1 LMP tumors and low-grade tumors is a functional wild-type p53
pathway, which is absent in high-grade tumors.3 This suggests that
Many proliferation pathways mediate signals through the RAS
inactivation of p53 is a key branch point, in which an intact p53
oncoprotein, a G-protein attached to the cell membrane and activated
pathway could lead to LMP/low-grade tumors, but disfunctional p53
by many tyrosine kinase receptors. RAS activates a cascade of serine/
threonine and tyrosine nonreceptorkinases, which leads to phosphorcould
lead to high-grade
other genomic
studies,
and CGH79
analyses
have cancers.
foundInsimilar
profiles
inLOH78
benign adenomas
ylation and activation of Erk1 and Erk2 transcription factors that
and in LMP tumors, which supports the concept of a transformation
make their way to the nucleus to initiate signals of growth and profrom benign adenoma to LMP.
Although ovarian adenocarcinomas can be subtyped by grade, gression through the cell cycle. As described above, K-RAS mutations
histologic subtypes also differ. Although differences in clinical outcomes among serous,endometrioid, and mucinous adenocarcinomas
are not as dramatic as those between high- and low-grade cancers,
genomic studies have demonstrated that mucinous adenocarcinomas
often harbor mutations and have differential gene expression similar
to LMP tumors and to benign cystadenomas.80 ,81 Specifically, mutations in K-RAS have been described in 61% of borderline tumors, in
68% of low-grade tumors, and in 50% of mucinous adenocarcinomas,
but only in 5% of high-grade serous carcinomas.7 0,8 2 These studies
suggest that the malignant transformation in mucinous tumors may
follow a sequence of adenoma to LMP tumor to invasive adenocarcinoma8 0,8 1 more frequently than to high-grade serous carcinomas.
Endometrioid adenocarcinomas more frequently harbor PTEN mutations(similar to endometrioid tumorsof the uterine endometrium)
than do serous or mucinous subtypes.83
www.jco.org
are common in adenocarcinomas, and frequency is variable in different histologic
subtypes.7to0,8
2
Resistance
antigrowth
signals. In early-transformed cells, anti-
growth signals must be overcome.Although definitive data are lacking
regarding the sequence of specific genetic events in carcinogenesis,
there is evidence for abnormalities in cell cycle mediators, such as
cyclins, cyclin-dependent kinases (CDKs, which complex with the
cyclins to allow their activity), CDK inhibitors (CDKIs, which inhibit
cyclin/CDK complexes), and other proteins or transcription factors
such as pRb, p53, and E2F. The restriction point, after which a cell is
committed to divide, is controlled by Cyclin D and Es regulation of
E2F release by Rb. Cyclin Eis expressed by only 9% of benign tumors
but by 48% of borderline and by 70% of malignant tumors, and it is
associated with poor survival.92 Similarly, CDK2, which complexes
exclusively with Cyclin E, is expressed more frequently in malignant
ovarian tumors compared with LMPor benign tumors.92 Cyclin D1 is
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on March 25, 2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
999
Landen, Birrer, and Sood
Table 3. Select Contributors to Ovarian Carcinogenesis
Protein/Gene
Function
Rate in EOC (%)
Growth Promotion
EGFR (HER1)
HER2
Src
CSF-1/fms
IGF/IGFR
K-RAS
BRAF
Membrane TK receptor, promotes cell growth
Membrane TK receptor, promotes growth
TK, promotes growth, angiogenesis, survival
Ligand/receptor, inhibits anoikis
Peptide hormone/receptor, promotes growth
G-protein, promotes growth through MAP kinase pathway
Promotes growth through MAP kinase pathway
Insensitivity to Antigrowth Signals
35-70
TGFC-MYC
Cyclin D/CDK4/6
Cyclin E/CDK2
Cyclin B/CDK1
p16
p27 (kip-1)
p21 (WAF-1)
NF B
NOEY(ARHI)
Ligand, inhibits growth through Rb activation
Transcription factor, cell cycle mediator
Advance from G1 to S phase
Advance from G1 to S phase
Advance cell cycle into M phase
Inhibits Cyclin D/Cdk4/6
Inhibits Cyclin E/Cdk2
Inhibits Cyclin B/Cdk1
Transcription factor, effector of many survival pathways
GTPase tumor suppressor, induces apoptosis through p21
Inhibition of Apoptosis and Immune Surveillance
PIP3/AKT
PTEN
p53
BRCA1
BRCA2
MLH1/MSH2
Fas ligand
HLA-G
AKT (activated by PIP3) inhibits apoptosis
Decrease AKT
Promotes cell cycle arrest/apoptosis with DNA damage
Cofactor for transcription factors, caretaker of genome
Cofactor for transcription factors, caretaker of genome
Mediates mismatch repair, promotes genetic stability
Produced by tumor cells to induce apoptosis of T-cells
Secreted by tumor cells to inhibit cytotoxic immune cells
Limitless Replicative Potential
hTERT
Subunit of telomerase, maintains telomere length
Enhanced Angiogenesis
VEGF/VEGFR
IL-8
EphA2
Ligand/receptor complex induces angiogenesis
Cytokine promoting angiogenesis
TK promoting angiogenesis and vasculogenic mimicry
Promotion of Invasion and Metastasis
40-100
Unknown
76
MMPs
v3
FAK
E-cadherin
Degrade extracellular matrix
Integrin, promotes survival and angiogenesis
Cofactor TK promotes adhesion, proliferation, survival
Promotes adhesion
40-100
95
70
90-100
20-66*
80-90
50-70
21-25
30-50
30-50
Lost in 40%
30
30-90
30-70
80
Lost in 30%
Lost in 55%
Lost in 25%40%
Unknown
40
12-18*
20
50-90*
6-82
1-3
30
50-80
61*
80-85
Abbreviations: EOC, epithelial ovarian cancer; EGFR, epidermal growth factor receptor; HER, human epidermal growth factor receptor; TK, tyrosine kinase; IGF,
insulin-like growth factor; TGF, transforming growth factor; CDK, cyclin-dependent kinase; VEGF, vascular endothelial growth factor; MMPs, matrix metalloproteinases; FAK, focal
adhesion kinase.
*High-grade
serous.
Low-grade serous.
40% loss of heterozygocity.
Endometrioid.
Inherited mutation in 6%7% of all cancers; may play a role in 82% of sporadic cancers.
cycle regulation that likely provide an unchecked growth advantage to
ovarian cancer cells.
inent in ovarian cancer cells (89% cytoplasmic; 30% nuclear).93 CDK1
Evading apoptosis. It has been proposed that a more important
complexes with cyclin B to regulate entry into the M phase, and it is
characteristic of cancer than increased cell division is the reduced
expressed at high levels in 80% of ovarian cancers, although absent
apoptosis and prolonged survival seen in these cells. Indeed, cancer
from normal epithelium.94
Other proteins that control the cell cycle include myc (an onco-cells often divide less frequently than their normal equivalents, espegenic transcription factor activated by the RAS-RAF pathway and
cially in epithelial cancers, in which normal epithelial cells have rapid
overexpressed in approximately 30% of ovarian cancers) and AHRI
turnover. Many participants in this process are altered in ovarian
(ie,NOEY2,a GTPase tumor suppressorgene lost in almost all ovarian
cancer to inhibit cell death. Among these is P53, which normally
cancers95, 96).Thus,there are multiple aberrations in the geneticsof cell
promoteseither cell cycle arrest and initiation of repairmechanismsor
expressed at low levels in normal ovarian epithelial cells but is prom-
1000
URN AL OF CL I N ICA L O N COL O GY
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on MarchJO 25,
2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
Carcinogenesis of Ovarian Cancer
the shunting of the cell to an apoptotic pathway.97 It has been hypothsites. Although metastasis is thought of as a late event in carcinogeneesized that cancers that do not have mutations in the P53 gene likelysis, emergingevidence in breast cancer suggests that early tumorsmay
have alterations in the function of p53 in other ways, such as in the already hold the genetic profile needed for metastasis,108 which further
production of p53-binding proteins or the enhanced degradation suggests that factors other than the tumor cell itself may regulate
through ubiquitination. Most P53 mutations in ovarian cancer are metastasis. Similarly, in ovarian cancer, peritoneal and stromal altermissense,9 8 but specific mutations (ie, null mutations) may play a ations
key may be permissive for cancer spread.1 09 An understanding of
role in producing a metastatic phenotype, in that they are seen muchthese factors mayprovide additional insights into tumorpathogenesis
less frequently in stage I ovarian cancers.99 Interestingly, P53 muta-and also may offer unique targets for therapy.
No cells, cancerous or benign,can exist without oxygen and other
tions have been detected in ovarian inclusion cysts adjacent to cystanutrients. Cells must reside within 100 m of a capillary in order to
denocarcinomas, in microscopic ovarian cancer, and even in
tubular intraepithelial carcinomas removed prophylactically from receive oxygen.110 Therefore, in order for a malignancy to grow bepatients with BRCA1 mutations.1 3, 100 The accumulation of evi- yond approximately 1 mm3, it must induce the growth of new vessels
dence suggests that p53 inactivation may be a relatively early eventin or around itself. Regulation of angiogenesis is complex, which
in ovarian
cancer pathogenesis.
The PI3-kinase/AKT
pathway is upregulated in approximately re ects a balance between pro- and antiangiogenic in uences within
the tumor microenvironment. The primary mediator of angiogenesis
30% of ovarian cancers.74 Activators of thispathway inhibit apoptosis,
is VEGF-A,11 1,1 12 which is known to increase vascular permeability,
but they also have been shown to increase neovascularization, enhance
stimulate endothelial cell proliferation and migration, alter endothe-
invasion, and increase resistance to chemotherapeutic agents.101 Con-
lial cell gene expression, and protect endothelial cells from apopto-
trol of the balance in this pathway lies primarily with PTEN, a tumor
sis.113 ,11 4 VEGF expression strongly correlates with ovarian cancer cell
suppressor that dephosphorylates PIP3 back into PIP2, promoting
linesthat induce ascites and carcinomatosis,115 and increased circulat-
apoptosis. The PTEN mutation is a frequent finding in endometrioid
ingand tumor VEGF levels are associated with the clinical outcome of
ovarian cancers, and animal models suggest that it may be an early
event inNF
ovarian
of the endometrioid
subtype.61
B iscarcinogenesis,at
the primaryleast
member
of a family
of five
transcription
of angiogenesis
ovarianMediators
cancer patients.116
,11 7
include tumor-derived factors and
host stromal factors. Interleukin-8 plays a significant role in neovas-
factors that deliver signalsto the nucleus to both increase proliferation
cularization and ovarian cancer growth11 8 and is elevated in patients
and inhibit apoptosis. NF B activation upregulates expression of
with both early- and late-stage cancers.119 The v 3 integrin is pri-
Bcl-2 family members, inhibitor of apoptosis proteins (IAP), and
marilyexpressed on newlydeveloping vascular endothelial cells, but it
additionalgenes identified by cDNA microarrayanalysisthat mayplay
isalso expressed on ovarian tumor cells.12 0 The tyrosine kinase recep-
a role in ovarian cancerpathogenesis.102 NF Bblockade also decreases
tor EphA2 is overexpressed by 75% of ovarian cancers,12 1 and its
VEGF and interleukin-8 production and decreases tumorigenicity of
inhibition reduces tumor growth, at least in part through antiangio-
ovarianLimitless
cancer cell lines
in mice.103 potential.
replicative
genic mechanisms.12 2,1 23 From a translational perspective, patientNormal cells can only divide a set
specific tumor microenvironment characteristics may in uence the
number of timesbefore they achieve senescence and undergo apoptoall-important
first
to antiangiogenic
therapy.1
24,step
125 in metastasis, and the primary feature
sis. The clock for this pathway lies in telomere caps on the ends of responseThe
chromosomes that are made up of DNA and associated proteins. that defines malignancy,isinvasion through the basement membrane,
Without the protection provided by telomeres, exposed chromo- which requires interplay between tumor cells and the permissive unsomes undergo massive defects, activating p53 and other policing derlying stroma. Invasion of malignant cells through the basement
proteins that propela cellinto an apoptotic pathway.Most cancer cells
membrane and endothelial cell migration for angiogenesis require
(75% to 90% of all types; 81% to 86% of those in ovarian cancer) degradation of the extracellular matrix. Matrix metalloproteinases
maintain telomere length byproduction of telomerase, a reverse tran(MMPs) are a family of zinc-dependent endopeptidases that digest
scriptase composed of an RNA component (hTR) and a catalytic collagen and other extracellular matrix components. They also stimsubunit (hTERT).104 The hTR subunit is expressed by all cells, butulate proliferation and induce release of VEGF.126 Ovarian tumors
hTERT expression increases with increasing tumorigenicity, which overexpress MMP-2 and MMP-9,1 27 and this increased expression
suggests that it is the rate-limiting step in telomerase activity.1 05 Findcorrelates with clinical stage12 8 and patient survival.1 29 Interestings that P53 knockdown and hTERT expression alone can transform
ingly, host production of MMPs may be more important than
ovarian surface epithelial cells106 and that functional BRCA inhibits
production by tumor cells, as demonstrated by Huang et al130 in
telomerase activity107 suggest that telomerase activation is an earlyand
MMP-knockout mice. Another potentiator of invasion is host
Earlyevent
events
the tumor microenvironment: angiogenesis, invarequired
forincarcinogenesis.
production of catecholamines through chronic stress. A growing
sion, and metastasis. A growing body of evidence suggests that, albody of preclinical data support the theory that chronic stress
though genetic events in the tumor cells themselves are certainly
contributes to the initiation and progression of cancer though
crucial, host and stromal factors in the tumor microenvironment are
activation of adrenergic receptors, which leads to increased invaequally important. A clinically significant tumor includes not only
sion and metastasis.131 ,1 32 These mechanistic data support epidetumor cells but also matrixcomponents, stromal cells, and in ammamiologic studies that show that patients with poor social support
tory cells. An interplay between tumor cells and surrounding normal In ammatory cellsand associated cytokinesplay significant roles
and increased stress are at greater risk for cancer progression.1 33
in the tumor
microenvironment.
Because
tumor
cells
can
produce
tissue dictates the establishment of a vascular supply through angioproteins that
are
recognized
as
abnormal,theycan
induce
an
immune
genesis, invasion into the surrounding stroma, penetration of lymresponse that
canand
result
in tumor
cell death.
As such,and
many
functions
phatic
vascular
spaces,
and adhesion
growth
at metastatic
www.jco.org
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on March 25, 2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
1001
Landen, Birrer, and Sood
of tumor cells serve to evade recognition and destruction by immune
assess, but positive peritoneal cytologyis detectedinapproximately
cells, such as Fas ligand production to induce lymphocyte apoptosis1 34
30% of stage I cancers.14 1 Given the shedding nature of ovarian
and HLA-G secretion to inhibit natural-killer cell activity.7 6,1 35 Cyto-
cancer, adhesion molecules in particular have been evaluated for
kine production by mesenchymal cells stimulates ovarian epithelium
their role in peritoneal metastasis. Evidence for mediators of this
and activates processes that may participate in malignant transforma-
process playing a role in early carcinogenesis is lacking but may
tion.13 6 Moreover, cytokine production by tumor cells promotes
include such promoters of cell survival as focal adhesion kinase
growth and inhibits apoptosis.137 As a testament to the importance of
(FAK) andE-cadherin.142 -1 45 E-cadherin is uniformly expressed in
the host antitumor immune response, increased T-cell infiltration
ovarian cancer, in lowmalignant-potential tumors, in benign
into the tumor is associated with improved survival.138 The role of
neoplasms, andnotablyin inclusion cysts of normal ovaries,
specific immune cell populations in controlling versus promoting
but not in the normal surface epithelium.1 46
Although
of9an
tumor growth
remainsthe
to bedefinition
fully defined.13
advanced stage requires metastatic spread of cancer cells, recent evidence suggests that metasta- Proposed Model of Ovarian Carcinogenesis
The increasing knowledge about early genetic events in ovarian
sis is an earlier event than previously thought.10 8 However, few (
carcinoma0.01%)
cells has
provided
a
better
understanding
of
factors
that
of shed malignant cells are capable of metastasizing, and
may induce
malignant
transformation
normal
epitheeven
the persistent
presence of
of the
cancer
cellsovarian
in the vasculature
does
lium. However,we
propose
that,
in
a
comprehensive
model
of
not necessarily result in seeding to distant sites.14 0 ovarian
The patterns of
carcinogenesis,
components
thatare
arise
in (or than
are deposited
to) the
metastasis
with EOC
different
those of most
cancers.
stroma, such
as
in
ammatory
cells
and
immune
modulators,
MMPs,
Release of malignant cells by early-stage cancers is
difficult to
Normal ovarian
surface epithelium
and inclusion cysts
Fig 2. Proposed model of ovarian carcinogenesis. Normal ovarian epithelium is exposed to physiologic processes that may
Predisposing events such
predispose to malignant transformation,
as androgen exposure
such as prolonged androgen exposure. A
number of characteristics must be ob-
High-grade
pathway
Low-grade
pathway
EGFR,
KRAS,
HER2
BRAF
Growth
factors
AKT2 PTEN
ulated growth, resistance to antigrowth
signals, inhibition of apoptosis, evasion of
recognition by the immune system,
LMP
Tum or
Angiogenesis VEGF, IL-8
duction of angiogenesis, and invasion of
the basement membrane. Examples of
each of these processes in ovarian cancer
Genetic instability
MSI
Immune escape FasL, HLA-G
are listed in italics. The order in which
these mutations may occur is not well
understood, but the timing and specific
mutations
in lowmay
malignant
potential
protein
affected
be significant
in(LMP)
pro-
Microenvironment effects MMPs
Anoikis resistance FAK, av
achieving limitless replicative potential, in-
specific proteins known to play a role in
Limitless replicative potential hTERT
p53, BRCA
other genetic changes, to be transformed
to a malignant state. These include unreg-
Inhibition of
apoptosis
No perceivable
intermediate
histology
tained, primarily through mutations or
tumors.
A mutation
leadingsubtypes
to geneticand
inducing different
histologic
stability,
as P53,
thatFor
occurred
early
grades
ofsuch
ovarian
cancer.
example,
if
Reattachment and growth
would
predispose
to other
mutations,
mutations
favoringcells
growth
and resistance
andapoptosis
rapid progression
to a metastatic
pheto
occurred early,
before achiev-
Metastasis to
bowel and
omentum
notype,
as seen infor
high-grade
malignaning the potential
invasion and
metastacies.anPermissive
or contributing
factors of
sis,
intermediate
pathologic subtype
the
microenvironment,
such such
as production
would
be noted more often,
as K-RAS
of matrix metalloproteinases (MMPs) by
fibroblasts (pictured in red), infiltration of
in ammatory cells (pictured in blue), and
proliferation of endothelial cells for angiogenesis, may be just as important as mu-
1002
tations in the tumor cells.
URN AL OF CL I N ICA L O N COL O GY
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on MarchJO 25,
2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
Carcinogenesis of Ovarian Cancer
and integrin ligands, may be equally important methods
for tumorfor
establishearly detection and for the targeting of key pathways
ment and growth (Fig 2). Within the broad dualwhile
pathway
patients
model,
are itstill
is amenable to a cure.
clear that several characteristics must be acquired by the tumor cell
and its environment. Although the order in which these occur is likely
AUTHORS
DISCLOSURES
OF
POTENTIAL
variable, early alterations in dominant genes may dictate the specific
OF INTEREST
CONFLICTS
path that is followed, such as K-RAS leading to an LMP tumor and
early occurrence of a P53 or BRCA alteration leading to genetic instaThe authors indicated no potential con icts of interest.
bility and rapid progression to a high-grade phenotype. Characteristics common to both pathways include the evasion of immune
AUTHOR CONTRIBUTIONS
surveillance, the invasion into the stroma, survival in the peritoneal
cavity, attachment to intraperitoneal sites, and continued growth andConception and design:Charles N. Landen, Anil K. Sood
angiogenesis. These additional steps likely require a longer period of
Administrative support: Anil K. Sood
Collection and assembly of data: Charles N. Landen, Michael J. Birrer,
time in LMPand low-grade malignancies, but theyalso occur eventuAnil K. Sood
ally and lead to relentless growth and metastasis. Despite many overData analysis and interpretation: Charles N. Landen, Anil K. Sood
lapping features, every malignancy is unique, and myriad yetManuscript writing: Charles N. Landen,Michael J. Birrer, Anil K. Sood
unidentified genetic alterations probably participate in ovarian
Final approval of manuscript: Charles N. Landen, Michael J. Birrer,
carcinogenesis. The challenge remains to identify the most important
Anil K. Sood
initial alterations in ovarian cancer to allow the development of better
serous carcinoma: Evidence for a causal relation25. Brinton LA, Lamb EJ, Moghissi KS, et
Ovarian2007
cancer risk after the use
ship. Am J Surg Pathol 31:161-169,
al: of ovulation14. Fleming JS, Beaugiestimulating
CR, Haviv
I, Obstet
et al: Gynecol 103:1194-1203,
drugs.
sant
ovulation, in ammation and epithelial ovarian
1. Jemal A, Siegel R, Ward E, et al: Cancer
Inces2004
26. Ness RB, Cottreau C: Possible role of ovarian
statistics, 2007. CA Cancer J Clin 57:43-66, 2007
carcinogenesis: Revisiting old hypotheses. Mol Cell
epithelial in ammation in ovarian cancer. J Natl
2. Rebbeck TR, Lynch HT, Neuhausen SL, et al:
Endocrinol
247:4-21,
14a. Gadducci
A, 2006
Cosio S, Gargini A, et al: Cancer Inst 91:1459-1467, 1999
Prophylactic oophorectomy in carriers of BRCA1 or
27. Zheng W, Lu JJ, Luo F, et al: Ovarian
steroid hormones, gonadotropin
and ovarian carcinoSexBRCA2 mutations. N Engl J Med 346:1616-1622,tumor growth promotion by follicle-stimulating horepithelial
genesis: A review of epidemiological and experimental
2002
3. Bonome T, Lee JY, Park DC, et al: Expression
mone and inhibition of the effect by luteinizing
data. Gynecol Endocrinol
19:216-228,
2004
14b.
Capen CC:
Mechanisms of hormoneprofiling of serous low malignant potential, low- hormone. Gynecol
Oncol 76:80-88, 2000
28. Choi KC, Kang SK, Tai CJ, et al:
mediated carcinogenesis of the ovary. Toxicol
grade, and high-grade
tumors
of the
ovary. Cancer
stimulating
hormone
activates
mitogen-activated
FolliclePathol 32:1-5, 2004 (suppl 2)
Res4.65:10602-10612,
2005AS,
Auersperg
N, Wong
Choi KC, et al:
15. Fathalla MF: Incessant ovulation: a factor in
protein
kinase
in preneoplastic
andOvarian
neoplastic ovarsurface epithelium:
Biology,
endocrinology,
andEndocrinol
paovarian
ian surface
epithelial
cells. J Clin
Metabneoplasia? Lancet 2:163, 1971
16. Whittemore AS, Harris R, Itnyre J: Characterthology. Endocr
Rev 22:255-288,
2001
87:2245-2253,
2002
29. Choi JH, Choi KC, Auersperg N, et al:
5. Naora
H: Developmental
patterning
in the
istics relating
to ovarian cancer
risk: Collaborative
pression
of follicle-stimulating
hormone receptor
wrong context:
The paradox
of epithelial ovarian
Overexanalysis of 12 US case-control studies. II. Invasive
oncogenic pathways
in preneoplastic ovarcancers. Cellactivates
Cycle 4:1033-1035,
2005
epithelial LD,
ovarian
cancersAI,
in white
Am J
6. Kowalski
Kanbour
Price women.
FV, et al:
ian surface epithelial cells. J Clin Endocrinol Metab
case-matched
molecular
comparison
of extraovarian
136:1184-1203,
1992
17. Risch HA, Marrett LD, Howe GR: Parity, conA Epidemiol
89:5508-5516, 2004
30. Tashiro H, Katabuchi H, Begum M, et al: Roles
traception, infertility, and the risk of epithelial ovarversus primary ovarian adenocarcinoma. Cancer 79:
of luteinizing hormone/chorionic gonadotropin re1587-1594,
1997 R, Zehavi S, Hadas E, et al: ian cancer. Am J Epidemiol 140:585-597, 1994
7. Halperin
ceptor in anchorage-dependent
and -independent
18. Riman T, Dickman PW, Nilsson S, et al: Risk
histochemical
comparison of primary peritoneal and
factors for invasive epithelial ovarian cancer: Results
Immunogrowth in human ovarian surface epithelial cell lines.
primary ovarian serous papillary carcinoma. Int J
from a Swedish case-control study. Am J Epidemiol
31. Ji Q, Liu PI, Chen PK, et al: Follicle
Cancer Sci 94:953-959, 2003
Gynecol
Pathol 20:341-345,
growth promotion and gene ex8. Halperin
R, Zehavi 2001
S, Langer R, et al: hormone-induced
156:363-373,
stimulating
19. Gwinn 2002
ML, Lee NC, Rhodes PH, et al: Pregperitoneal
pression
profiles
on ovarian
surface
epithelial cells.
Primaryserous papillary carcinoma: A new epidenancy, breast
feeding,
and oral
contraceptives
and
REFERENCES
miologic trend? A matched-case comparison with
Int
Cancer
112:803-814,
2004
theJrisk
of epithelial
ovarian
cancer. J Clin Epidemiol
32. Schiffenbauer YS, Abramovitch R, Meir G, et
ovarian serous papillary cancer. Int J Gynecol Cancer 43:559-568,
al: Loss of 1990
ovarian function promotes angiogenesis
20. Nasca PC, Greenwald P, Chorost S, et al: An
9. Chen LM,
11:403-408,
2001Yamada SD, Fu YS, et al: Molecular
in human ovarian
carcinoma.
Proc
Natl Acad
Sci U S
epidemiologic
case-control
study
of ovarian
cancer
similarities between primary peritoneal and primary
A
94:13203-13208,
1997
33. Wang J, Luo F, Lu JJ, et al: VEGF
and reproductive factors. Am J Epidemiol 119:705ovarian carcinomas. Int J Gynecol Cancer 13:749and
enhanced
production
by
gonadotropins in ovarexpression
713,
21.1984
Fredrickson TN: Ovarian tumors of the hen.
755,
10.2003
Lacy MQ, Hartmann LC, Keeney GL, et al:
ian epithelial tumors. Int J Cancer 97:163-167, 2002
Environ Health Perspect 73:35-51, 1987
34. Schiffenbauer YS, Meir G, Maoz M, et al:
C-erbB-2 and p53 expression in fallopian tube carciGonadotropin stimulation of MLS human epithelial22. Land JA: Ovulation, ovulation induction and
noma. Cancer 75:2891-2896, 1995
ovarian carcinoma. Baillieres Clin Obstet Gynaecol
11. Pere
H, Tapper
J, Seppala
M, et al:cell
Genomic
ovarian
carcinoma
cells augments
adhesion
alterations in fallopian tube carcinoma: Comparison
7:455-472, 1993
mediated by CD44 and by alpha(v)-integrin. Gynecol
23. Risch HA: Hormonal etiology of epithelial
to serous uterine and ovarian carcinomas reveals
ovarian cancer, with a hypothesis concerning the
35. Rosenberg L, Palmer JR, Zauber AG, et al: A
Oncol 84:296-302, 2002
similarity suggesting likeness in molecular pathocase-control
study of oral
contraceptive
use and
role of androgens
and progesterone.
J Natl
Cancer
12. Muto
MG, Welch WR,
Mok SC, et al: Evidence
genesis. Cancer
Res 58:4274-4276,
1998
invasive
epithelial ovarian cancer. Am J Epidemiol
Inst24.
90:1774-1786,
1998
Schildkraut JM,
Schwingl PJ, Bastos E, et al:
for a multifocal origin of papillary serous carcinoma of
139:654-661,
1994
Epithelial
ovarian
cancer
risk
among women with
36. Gaspard UJ, Romus MA, Gillain D, et al:
the peritoneum. Cancer Res 55:490-492, 1995
13. Kindelberger DW, Lee Y, Miron A, et al:
Plasma
hormone
levels in women receiving new
polycystic ovary syndrome. Obstet
Gynecol
88:554Intraepithelial carcinoma of the fimbria and pelvic
oral contraceptives containing ethinyl estradiol plus
559, 1996
www.jco.org
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on March 25, 2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
1003
Landen, Birrer, and Sood
levonorgestrel or desogestrel. Contraception 27:
cycle in response to DNA damage. Cancer Sci
75. Ross JS, Yang F, Kallakury BV, et al: HERneu
oncogene2004
amplification by uorescence in situ
577-590, 1983
95:866-871,
2/
37. Seeger H, Wallwiener D, Mueck AO: Is there
56. Boulton SJ: Cellular functions of the BRCA
hybridization in epithelial tumors of the ovary. Am J
a protective role of progestogens on the proliferatumour-suppressor proteins. Biochem Soc Trans
Clin Pathol 111:311-316, 1999
76. Singer G, Rebmann V, Chen YC, et al: HLA-G
tion of human ovarian cancer cells in the presence of
34:633-645, 2006
57. Rosen EM, Fan S, Pestell RG, et al: BRCA1
is a potential tumor marker in malignant ascites. Clin
growth factors? Eur J Gynaecol Oncol 27:139-141,
gene in breast cancer. J Cell Physiol 196:19-41,
Cancer Res 9:4460-4464, 2003
38. McNatty KP, Smith DM, Makris A, et al: The 2003
2006
77. Ouellet V, Guyot MC, Le Page C, et al: Tissue
microenvironmentarray
of the
humanof
antral
follicle:microarray
Interanalysis
expression
candidates 58. Aarnio M, Sankila R, Pukkala E, et al:
in mutation carriers of DNA-mismatch-repair
relationships among
the steroid
levels
in antral with
uid, tumor grade and riskCancer
identifies
markers
associated
genes.
Int J Cancer 81:214-218, 1999
the population of outcome
granulosaincells,
andepithelial
the statusovarian
of
serous
cancer. Int J
59. Orsulic S, Li Y, Soslow RA, et al: Induction
ovarian
the oocyte in vivoCancer
and in 119:599-607,
vitro. J Clin Endocrinol
2006
of cancer by defined multiple genetic changes
78. Dodson MK, Hartmann LC, Cliby WA, et al:
39. Edmondson RJ, Monaghan JM,Comparison
Davies BR: of loss
in aof
mouse
model system.
Cancer
heterozygosity
patterns
in Cell 1:53-62,
Metab 49:851-860, 1979
The human ovarian surface epithelium is an andro2002
invasive low-grade
and Connolly
high-grade DC,
epithelial
60.
Baoovarian
R, Nikitin AY, et al:
gen responsive tissue. Br J Cancer 86:879-885,
mice chimeric
for expression
ofFemale
the
virus 40 1993
carcinomas.
Cancer
Ressimian
53:4456-4460,
79. Meinhold-Heerlein I, Bauerschlag D, Hilpert F,
2002
40. Altinoz MA, Korkmaz
R:under
NF-kappaB,
macroTAg
of
the
MISIIR
promoter
develop
et al:control
Molecular
and
prognostic
distinction
between
phage migration inhibitory factor and cyclooxygenaseepithelial
ovarian
cancer.
Cancer Res
63:1389-1397,
serous
ovarian
carcinomas
of varying
grade and
inhibitions as likely mechanisms behind the
61. Dinulescu
DM, Ince
TA, Quade BJ, et al: Role
2003 malignant potential. Oncogene
24:1053-1065,
2005
80. Heinzelmann-Schwarz VA, Gardiner-Garden
acetaminophen- and NSAID-prevention of the ovarof K-ras and Pten in the development of mouse
M, Henshall SM, et al: A distinct molecular profile
Heller DS,
Westhoff C,
Gordon RE, et al: The models
ian cancer.41.
Neoplasma
51:239-247,
2004
of endometriosis and endometrioid ovarian
relationship between perineal cosmetic talc usage
associated with mucinous epithelial ovarian cancer.
cancer.
Nat Med
11:63-70,
2005
Shih
Ie
M,
Kurman
RJ: Ovarian tumorigeneand ovarian talc particle burden. Am J Obstet GyBr 62.
J Cancer
94:904-913,
2006
81. Wamunyokoli FW, Bonome T, Lee JY, et al:
sis: A proposed model based on morphological and
necol
1996 L: Genetics and biology
Expression profiling of mucinous tumors of the
42. 174:1507-1510,
Duggan BD, Dubeau
molecular genetic analysis. Am J Pathol 164:1511of gynecologic cancer. Curr Opin Oncol 10:439-446,
ovary identifies genes of clinicopathologic impor1518,
63. 2004
Gershenson DM, Sun CC, Lu KH, et al:
1998
tance. Clin Cancer Res 12:690-700, 2006
82. Suzuki M, Saito S, Saga Y, et al: Mutation of
43. Donninger H, Bonome T, Radonovich M, et al: behavior
of stage II-IV low-grade serous carcinoma
Clinical
and loss of heterozygosity on
Whole genome expression profiling ofK-RAS
advanceprotooncogene
of the ovary. Obstet Gynecol 108:361-368, 2006
64. Ozols
RF, Bundy
BN, Greer BE, et al: Phase
6q27 inactiserous and mucinous
ovarian
carcinomas.
stage papillary serous ovarian cancer reveals
trial of carboplatin and paclitaxel compared with
III
Genet Cytogenet 118:132-135, 2000
vated
Oncogene
23:8065-8077,
2004
44. pathways.
Bild AH,
Yao
G,with
Chang
JT, et Cancer
al: Oncogenic
83. Obata K, Morland SJ, Watson RH, et al:
cisplatin and paclitaxel
in patients
optimally
pathway signatures in human cancers as a guideFrequent
to
PTEN/MMAC mutations in endometrioid
resected stage III ovarian cancer: A Gynecologic
targeted therapies. Nature 439:353-357, 2006 but not serous or mucinous epithelial ovarian tu45.study.
Shridhar
V, Lee
J, Pandita A, et al:
Oncology Group
J Clin Oncol
21:3194-3200,
mors. Cancer
58:2095-2097,
1998 B, Wenzel L, et al:
analysis
of early- versus late-stage ovarian tumors.
65.Res
Armstrong
DK, Bundy
84. Hanahan D, Weinberg RA: The hallmarks of
Genetic
2003
Intraperitoneal
cisplatin
and paclitaxel in ovarian can- cancer. Cell 100:57-70, 2000
Cancer Res 61:5895-5904, 2001
46. Lancaster JM, Dressman HK, Clarke JP, et al: cer. N Engl J Med 354:34-43, 2006
85. Han L, Landen C, Trevino J, et al:
Identification of genes associated with ovarian can66. Malpica A, Deavers
MT, Lu
K, et al:effects of Src inhibition in
angiogenic
and anti-tumor
Antiovarian
serous carcinoma using a two-tier system.
cer metastasis using microarray expression analyGrading
ovarian carcinoma. Cancer Res 66:8633-8639, 2006
86. Ishizawar R, Parsons SJ: C-Src and cooperatAm J Surg Pathol 28:496-504, 2004
sis.47.
IntJazaeri
J Gynecol
16:1733-1745,
AA,Cancer
Yee CJ,
Sotiriou C, et2006
al: Gene
67. Crispens MA, Bodurka D, Deavers M, et al:
ing partners in human cancer. Cancer Cell 6:209expression profiles of BRCA1-linked, BRCA2-linked,
Response and survival in patients with progressive
214, 2004
87. Silva CM: Role of STATs as downstream
and sporadic ovarian cancers. J Natl CancerorInst
recurrent serous ovarian tumors of low malignant
signal transducers in Src family kinase-mediated
94:990-1000,
2002
potential.
Obstet
Gynecol
99:3-10,
2002
48. Cass I, Baldwin RL, Varkey T, et al:
68. Mok SC, Bell DA, Knapp RC, et al: Mutation
tumorigenesis. Oncogene 23:8017-8023, 2004
survival
in women with BRCA-associated ovarian
K-ras
88. Wiener JR, Windham TC, Estrella VC, et al:
Improved
of protooncogene in human ovarian epithelial
carcinoma. Cancer 97:2187-2195, 2003
49. Gotlieb WH, Chetrit A, Menczer J, et al:
Demographic and genetic characteristics of patients
tumors
of borderline
malignancy.
Cancer
Resis53:
Activated
SRC protein
tyrosine
kinase
overex1489-1492,
1993
in late-stage
human
cancers.
69.pressed
Teneriello
MG, Ebina
M,ovarian
Linnoila
RI, etGyal:
andp53
Ki-ras
epithelial ovarian neonecol gene
Oncolmutations
88:73-79,in2003
with borderline ovarian tumors as compared to early
plasms.
Cancer Res
tyrosine
kinase
promotes
and resistance
to 53:3103-3108, 1993
stage invasive ovarian cancer.
Gynecol
Oncol
97: survival
70. Singer G, Oldt R, 3rd, Cohen Y, et al:
chemotherapeutics
mousetions
ovarian
cancerand
cellKRAS characterize the develop50. Merajver
TM, Caduff RF,inetaal:
in
BRAF
780-783,
2005 SD, Pham
MutaSomatic mutations in the BRCA1
gene inBiophys
sporadicRes Commun
line. Biochem
309:377-383,
ment of low-grade
ovarian serous carcinoma. J Natl
89. Pengetnze Y, Steed M, Roby KF, et al: Src
ovarian tumours. Nat Genet
9:439-443, 1995
2003
95:484-486,
2003
51. Baldwin RL, Nemeth
E, Tran H, et al: BRCA1Cancer
71. Inst
Kohler
MF, Marks
JR, Wiseman RW, et al:
prognostic
of epidermal
growth
promoter region hypermethylation in ovarian carci- TheSpectrum
ofvalue
mutation
and frequency
offactor
allelic deletion
receptor
mRNA
expression
in
primary
ovarian
can- Inst
noma: A population-based study. Cancer Res 60:
of the p53 gene in ovarian cancer. J Natl Cancer
90. Bartlett JM, Langdon SP, Simpson BJ, et al:
cer.85:1513-1519,
Br J Cancer 73:301-306,
1996
5329-5333,
2000
1993 J, Thor
52. Esteller
M, Silva JM, Dominguez G, et al:
72. Kupryjanczyk
AD, Beauchamp R, et al: 91. Leary JA, Edwards BG, Houghton CR, et al:
Amplification
Promoter hypermethylation and BRCA1 inactivation
p53 gene mutations and protein
accumulationofinHER-2/neu oncogene in human
ovarian
Int J Gynecol Cancer 2:291-294,
in sporadic breast and ovarian tumors. J Natl Cancer
human ovarian cancer. Proc Natl Acadcancer.
SciUSA
1992
90:4961-4965,
1993
92. Sui L, Dong Y, Ohno M, et al: Implication
73. Skilling JS,
Sood A, Niemann T, et al: An
malignancy
and
prognosis
of
abundance of p53 null mutationsp27(kip1),
in ovarian Cyclin
carci- E, and of
Cdk2
expression
in epithelial
ovarian tumors. GyJ Natl Cancer Inst 94:1396-1406, 2002
noma.
Oncogene
13:117-123,
1996
54. Venkitaraman AR: Cancer susceptibility and
74. Cheng JQ, Godwin AK, Bellacosa A, et al:
necol
Oncol
83:56-63,
2001
AKT2,the
a putative
functions
oncogene
of BRCA1
encoding
and BRCA2.
a member
Cellof108:171a
93. Dhar KK, Branigan K, Parkes J, et al:
sion and subcellular localization of cyclin D1
protein
subfamily
182,of2002
protein-serine/threonine kinases, is amExpres55. Yoshida K, Miki Y: Role of BRCA1 and BRCA2
in
epithelial
ovarian
tumour
cells.
Br
J
Cancer
81:
plified as
in regulators
human ovarian
carcinomas.
Proc Natl Acad
of DNA
repair, transcription,
and cell
1174-1181,
1999
SciUSA89:9267-9271, 1992
Inst53.
92:564-569,
2000
Hilton JL,
Geisler JP, Rathe JA, et al:
vation
of BRCA1 and BRCA2 in ovarian cancer.
Inacti-
1004
URN AL OF CL I N ICA L O N COL O GY
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on MarchJO 25,
2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
Carcinogenesis of Ovarian Cancer
94. Barrette BA, Srivatsa PJ, Cliby WA, et al:
Overexpression of p34cdc2 protein kinase in epithe-
111. Folkman J: The role of angiogenesis in tumor
growth.
Cancer
Biol 3:65-71,
TheSemin
clinical
relevance
of stromal1992
matrix metallopro112. Frumovitz M, Sood A: Vascular Endothelial
lial ovarian carcinoma. Mayo Clin Proc 72:925-929,
teinase expression in ovarian cancer. Clin Cancer
Growth Factor (VEGF) Pathway as a Therapeutic
1997
12:1707-1714, 2006
95. Bao R, Connolly DC, Murphy M, et al: TargetRes
in Gynecologic Malignancies. Gynecol Oncol
tion
of cancer-specific gene expression
by the sur-of stromal metalloproteinase-9 to anContributions
Activa104:768-778,
2007
113. Connolly
DT, Heuvelman DM, Nelson R, et
vivin promoter. J Natl Cancer Inst 94:522-528,
2002growth of
giogenesis
and
humanvascular
ovarianpermeability
carcinoma factor stimulates
96. Yu Y, Xu F, Peng H, et al: NOEY2
(ARHI),
al: Tumor
in
mice.
J
Natl
Cancer
Inst
94:1134-1142,
2002
imprinted
putative
tumor
suppressor
gene
in
ovarian
an
endothelial cell growth
and angiogenesis. J Clin
129. Kamat AA, Fletcher M, Gruman LM, et al:
130. Huang S, Van Arsdall M, Tedjarati S, et
al:
131. Thaker PH, Han LY, Kamat AA, et al: Chronic
stress promotes
growth and angiogenesis in
Invest
1989SJ,tumor
114.84:1470-1478,
Senger DR, Galli
Dvorak AM, et al: Tumor
mouse model
of ovarian
carcinoma.
Nat Med
96:214-219,
1999 D, Halevy O, Oren M: p53 muta- cells secrete aa vascular
97. Michalovitz
permeability
factor
that
tions: Gains or losses? J Cell Biochem 45:22-29,
12:939-944,of2006
promotes accumulation
ascites uid. Science
132. Sood AK, Bhatty R, Kamat AA, et al: Stress
and breast carcinomas. Proc Natl Acad Sci U S A
1991
hormone-mediated invasion of ovarian cancer cells.
98. Skilling JS, Squatrito RC, Connor JP, et al: 219:983-985,
115. Yoneda1983
J, Kuniyasu H, Crispens MA, et al:
Clin Cancer Res 12:369-375, 2006
gene
mutation
analysis
and
antisense-mediated
Expression
of
angiogenesis-related
genes
and
prop53
133. Antoni MH, Lutgendorf SK, Cole SW, et al:
growth inhibition of human ovarian carcinoma cell
gression of human ovarian
carcinomas
in
nude
mice.
The in uence of bio-behavioral factors on tumor
lines.
Oncol
60:72-80,
J Natl Cancer
Inst
90:447-454,
1998KA,and
biology:
Pathways
mechanisms.
Nat Rev Can99. Gynecol
Marks JR,
Davidoff
AM,1996
Kerns BJ, et al:
116.
Paley
PJ, Staskus
Gebhard
K, et al:
Overexpression and mutation of p53 in epithelial
Vascular endothelial
growth
factor expression in
cer 6:240-248, 2006
134. Ben-Hur H, Gurevich P, Huszar M, et al:
ovarian cancer. Cancer Res 51:2979-2984,
1991
early stage
ovarian
Cancer 80:98-106,
Apoptosis and
apoptosis-related
proteins
(Fas,carcinoma.
Fas
100. Kerner R, Sabo E, Gershoni-Baruch
R, et al:
1997
Expression of cell cycle regulatory proteinsligand,
in ova-Blc-2, p53) in lymphoid
117.elements
Cooperof
BC,
Ritchie JM, Broghammer CL, et
human
al:
Preoperative
serum vascular endothelial growth
ries prophylactically removed from Jewishovarian
Ash- tumors. Eur J Gynaecol
Oncol 21:141-145,
factor levels: Significance in ovarian cancer. Clin
135. Paul P, Rouas-Freiss N, Khalil-Daher I, et
Cancer
Res
8:3193-3197,
2002
HLA-G
expression
melanoma:
A way
forInterleukin
tumor
118. in
Xu
L, Fidler
IJ:
8: an
Correlation with histopathology. Gynecol Oncol 99:
al:
101. Hu L, Hofmann J, Lu Y, et al: Inhibition
growth
for human ovarian
cells to escape
from factor
immunosurveillance.
Proccancer.
Natl Oncol Res
autocrine
367-375, 2005
phosphatidylinositol
3 -kinase increases efficacy of
of
12:97-106, 2000 1998
Acad SciUSA95:4510-4515,
136. Bukovsky A: Immune system involvement in
119. Lokshin AE, Winans M, Landsittel D, et al:
paclitaxel in in vitro and in vivo ovarian cancer
the regulation
of ovarian function and augmentation
Circulating IL-8 and anti-IL-8 autoantibody
in patients
models.
Cancer Res 62:1087-1092,
2002 V, et al:
102. Deregowski
V, Delhalle S, Benoit
of cancer.
Microsc Res Tech 69:482-500, 2006
with ovarian cancer. Gynecol Oncol
102:244-251,
Identification of cytokine-induced nuclear factor137. Nash MA, Ferrandina G, Gordinier M, et al:
2006
120. Davidson B, Goldberg I,The
Reich
role R,
of cytokines
et
in both the normal and maligkappaB target genes in ovarian and breast cancer
AlphaV- and beta1-integrinal:
subunits are commonly
nant ovary. Endocr Relat Cancer 6:93-107, 1999
cells.
Pharmacol
64:873-881,
2002 A, et al:
103.Biochem
Huang S,
Robinson
JB, expressed
Deguzman
138. Zhang L, Conejo-Garcia JR, Katsaros D, et al:
in malignant effusions from ovarian carBlockade of nuclear factor-kappaB signaling inhibits
Intratumoral T cells, recurrence, and survival in epicinoma patients. Gynecol Oncol
90:248-257,
2003 M, Celestino J, et al:
121. Thaker
PH, Deavers
angiogenesis and tumorigenicity of human ovarian
thelial ovarian cancer. N Engl J Med 348:203-213,
EphA2 expression is associated with aggressive
cancer cells by suppressing expression of vascular
2003
139. Coukos G, Conejo-Garcia JR, Roden RB, et
features in ovarian carcinoma. Clin Cancer Res 10:
endothelial growth factor and interleukin 8. Cancer
al: Immunotherapy for gynaecological malignancies.
2004CN, Jr., Chavez-Reyes A, Bucana C,
104. Landen CN, Klingelhutz A, Coffin JE, et 5145-5150,
122. Landen
Res 60:5334-5339, 2000
Expert Opin Biol Ther 5:1193-1210, 2005
Genomic
instability is associated with lack of telomet al: Therapeutic EphA2 Gene Targeting In vivo
140. Fidler IJ: The pathogenesis of cancer metasal:
tasis: The seed and soil hypothesis revisited. Nat
erase activation in ovarian cancer. Cancer Biol Ther
Using Neutral Liposomal Small Interfering RNA Dekenazi BRCA1 and BRCA2 mutation carriers:
2000
Cancer 3:453-458, 2003
3:1250-1253,
2004C, Heine B, Diallo R, et al: Telomlivery. Cancer
65:6910-6918,
2005
105. Poremba
123.Res
Landen
CN, Jr.,
Lu C, Han LY, et al: Rev141.
Emerich J, Konefka T, Dudziak M, et al:
erase as a prognostic marker in breast cancer:
andEfficacy
antivascular effects of EphA2 reduction with an
value of peritoneal
[The cytology in the staging of ovarian
High-throughput tissue microarray analysis of
agonistic antibody in ovarian cancer. J Natl Cancer
cancer]. Ginekol Pol 68:74-77, 1997
142. Hood JD, Cheresh DA: Role of integrins in
hTERT
and
hTR.
J
Pathol
198:181-189,
2002
98:1558-1570,
2006 SA, Akagi Y, et al: Role of
106. Yang G, Rosen DG, Mercado-Uribe I, et al: Inst124.
Jung YD, Ahmad
cell invasion and migration. Nat Rev Cancer 2:91Knockdown of p53 combined with expression of the
the tumor microenvironment in mediating response
100, 2002
catalytic subunit of telomerase is sufficient to imto anti-angiogenic therapy. Cancer Metastasis Rev
143. Carreiras F, Rigot V, Cruet S, et al:
properties of the human
ovarian adenocarcinoma
mortalize primary human ovarian surface epithelial
19:147-157,
Migration
125. Lu 2000
C, Bonome T, Li Y, et al: Gene
cell lineofIGROV1:
importance
of alpha(v)
beta3 inte107. Zhou28:174-182,
C, Liu J:
human
identified
by expression
profiling
in tumorcells. Carcinogenesis
2007Inhibition
alterations
asetelomerreverse transcriptase gene expression
by vitronectin.
grins and
Int J endothelial
Cancer 80:285-294,
associated
cells from1999
invasive ovarian
144. Sundfeldt K: Cell-cell adhesion in the normal
BRCA1 in human ovarian cancer cells. Biochem carcinoma. Cancer Res 67:1757-1768,
2007
and ovarian
tumors of epithelial origin; an
126. Belotti D, Paganoni ovary
P, Manenti
L, et al:
Biophys
Res Commun
303:130-136,
2003 R, et al:
Matrix metalloproteinases
108. Sorlie
(MMP9
T, Perou
and
CM,
MMP2)
Tibshirani
inexception to the rule. Mol Cell Endocrinol 202:89-96,
expression
patterns
of
breast
carcinomas
distinduce the releaseGene
of vascular endothelial growth
2003
145. Halder J, Kamat AA, Landen CN, Jr., et
guish
with
clinical
implications.
factor (VEGF)
by tumor
ovariansubclasses
carcinomaFocal
cells:
Implicaadhesion
kinase targeting using in vivo short
al:
Proc
Natl
AcadE,
SciUSA98:10869-10874,
2001
109.
Wang
Ngalame
Y,
Panelli
MC,
et al: in
Peritions for ascites
formation.
Cancer
Res
63:5224interfering
RNA
delivery
neutral liposomes for
toneal and subperitoneal stroma may facilitate re127. Naylor MS, Stamp GW, Davies BD, et al:
5229, 2003
ovarian carcinoma therapy. Clin Cancer
Res 12:
Expression
and activity of MMPS and their regulagional spread of ovarian cancer. Clin Cancer Res
4916-4924, 2006
146. Sundfeldt K, Piontkewitz Y, Ivarsson K, et al:
tors
in
ovarian
cancer. Int J Cancer 58:50-56, 1994
11:113-122,
2005J: Angiogenesis in cancer, vascular,
110. Folkman
128. Herrera CA, Xu
E-cadherin
L, Bucana
expression
CD, et
in human
al: epithelial ovarian
rheumatoid and other disease. Nat Med 1:27-31,
sion
of metastasis-related genes
human
epithelial
Exprescancerinand
normal
ovary. Int J Cancer 74:275-280,
1995
ovarian tumors. Int J Oncol1997
20:5-13, 2002
www.jco.org
Information downloaded from jco.ascopubs.org and provided by UNIVERSITEITSBIBLIOTHEEK on March 25, 2010 from
131.174.244.21.
Copyright 2008 by the American Society of Clinical Oncology. All rights reserved.
1005
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Sleisenger and Fordtran's Gastrointestinal and Liver Disease Part 1 (PDFDrive)Document1,029 pagesSleisenger and Fordtran's Gastrointestinal and Liver Disease Part 1 (PDFDrive)Emi Valcov100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Genetics of CancerDocument44 pagesGenetics of Cancermruganakshatra8183No ratings yet
- Conf Munique 2012 - Professor Serge JurasunasDocument88 pagesConf Munique 2012 - Professor Serge Jurasunasnomehoda513No ratings yet
- Millenium Development GoalsDocument1 pageMillenium Development GoalsdoddydrNo ratings yet
- Secondary Cytoreductive Surgery For Recurrent Ovarian Cancer in An Asian PopulationDocument9 pagesSecondary Cytoreductive Surgery For Recurrent Ovarian Cancer in An Asian PopulationdoddydrNo ratings yet
- Paclitaxel and Carboplatin in Recurrent Ovarian Carcinoma - A Phase II TrialDocument7 pagesPaclitaxel and Carboplatin in Recurrent Ovarian Carcinoma - A Phase II TrialdoddydrNo ratings yet
- EBCRDocument19 pagesEBCRdoddydrNo ratings yet
- CC 071015 Elly MarlinaDocument5 pagesCC 071015 Elly MarlinadoddydrNo ratings yet
- Evidence Based Practice Tutorial How To Write A Case ReportDocument4 pagesEvidence Based Practice Tutorial How To Write A Case ReportAnastasia TjanNo ratings yet
- 1 PBDocument9 pages1 PBMuliani RatnaningsihNo ratings yet
- Emergency ContraceptionDocument26 pagesEmergency ContraceptiondoddydrNo ratings yet
- Profbiranroadtomaternaldeathpelatihanponekjakarta290812 121128235139 Phpapp02Document55 pagesProfbiranroadtomaternaldeathpelatihanponekjakarta290812 121128235139 Phpapp02doddydrNo ratings yet
- Journal AbortionDocument11 pagesJournal AbortiondoddydrNo ratings yet
- HPP (English)Document118 pagesHPP (English)doddydrNo ratings yet
- Bupati/walikota TIM FASILITATOR AMP ProtectionDocument15 pagesBupati/walikota TIM FASILITATOR AMP ProtectiondoddydrNo ratings yet
- ADENOMYOSISDocument5 pagesADENOMYOSISdoddydrNo ratings yet
- Routine Antenatal Care For Healthy Pregnant Women: Understanding NICE GuidanceDocument24 pagesRoutine Antenatal Care For Healthy Pregnant Women: Understanding NICE GuidanceNoer AsNo ratings yet
- Respon Neoplastik: Program Magister Ilmu Biomedik Fakultas Kedokteran Universitas AndalasDocument66 pagesRespon Neoplastik: Program Magister Ilmu Biomedik Fakultas Kedokteran Universitas AndalasMirna WatiNo ratings yet
- The Reactome BookDocument3,252 pagesThe Reactome BookA RoyNo ratings yet
- MEDICAL BOARD REVIEW 2021 - PATHOLOGY KEY TERMSDocument137 pagesMEDICAL BOARD REVIEW 2021 - PATHOLOGY KEY TERMSten tazapNo ratings yet
- Surgical Oncology OutlineDocument8 pagesSurgical Oncology OutlineGeriz Daniella VigoNo ratings yet
- Phycocyanin A Potential Drug For Cancer TreatmentDocument14 pagesPhycocyanin A Potential Drug For Cancer TreatmentSrivatsava RajagopalanNo ratings yet
- Zeolite StudyDocument4 pagesZeolite StudyAdeel AhmedNo ratings yet
- The Cell Cycle & ApoptosisDocument20 pagesThe Cell Cycle & ApoptosisSathiyaraj100% (4)
- Graphene-Polymer Composites: EditorialDocument5 pagesGraphene-Polymer Composites: Editorialjoe trumpNo ratings yet
- RutaceaeDocument13 pagesRutaceaePiyush RathourNo ratings yet
- Androgen Receptor Suppresses Prostate Cell Growth by Inhibiting c-MYCDocument26 pagesAndrogen Receptor Suppresses Prostate Cell Growth by Inhibiting c-MYCDr. NasrumminallahNo ratings yet
- CardiomyocyteDocument12 pagesCardiomyocyteralli711No ratings yet
- Mir-137 Modulates A Tumor Suppressor Network-Inducing Senescence in Pancreatic Cancer CellsDocument14 pagesMir-137 Modulates A Tumor Suppressor Network-Inducing Senescence in Pancreatic Cancer Cellsh234074No ratings yet
- Nucleolus A Central Hub For Nuclear FunctionsDocument13 pagesNucleolus A Central Hub For Nuclear FunctionsJuan Andres Fernández MNo ratings yet
- Study Guide for Biol 3090/7800 Final ExamDocument9 pagesStudy Guide for Biol 3090/7800 Final ExamanhminhandnamNo ratings yet
- What Is Zeolite and What Are Its BenefitsDocument6 pagesWhat Is Zeolite and What Are Its BenefitsIgor Cverdelj-FogarasiNo ratings yet
- The Peptide-Hormone Glucagon-Like Peptide-1 Activates cAMP and Inhibits Growth of Breast Cancer CellsDocument13 pagesThe Peptide-Hormone Glucagon-Like Peptide-1 Activates cAMP and Inhibits Growth of Breast Cancer CellsRidha Surya NugrahaNo ratings yet
- Cell Bio AssignmentDocument11 pagesCell Bio AssignmentPranay PatnaikNo ratings yet
- Materials Today: Proceedings: Samuel Shiferaw Biresaw, Pankaj TanejaDocument9 pagesMaterials Today: Proceedings: Samuel Shiferaw Biresaw, Pankaj TanejaRapazito RagazzoNo ratings yet
- DNA RepairDocument98 pagesDNA Repairapi-3700537100% (1)
- Seminar: Jonathan D Mizrahi, Rishi Surana, Juan W Valle, Rachna T ShroffDocument13 pagesSeminar: Jonathan D Mizrahi, Rishi Surana, Juan W Valle, Rachna T ShroffNoy FaridaNo ratings yet
- KIMEDDocument8 pagesKIMEDAgung MaulanaNo ratings yet
- Cell Cycle: Dr. Jusuf Fantoni, Sppa, Msc. PathDocument22 pagesCell Cycle: Dr. Jusuf Fantoni, Sppa, Msc. PathdwiandarimaharaniNo ratings yet
- 2020 01 08 898940v1 FullDocument45 pages2020 01 08 898940v1 FullBASKAR RAJNo ratings yet
- Cell Cycle ControlDocument13 pagesCell Cycle ControlCaue LimaNo ratings yet
- Cell Cycle Control A System of Interlinking OscillatorsDocument17 pagesCell Cycle Control A System of Interlinking OscillatorsMaría José Triana TamayoNo ratings yet
- BCBT-52822 - Lecture - Dulith AbeykoonDocument84 pagesBCBT-52822 - Lecture - Dulith Abeykoonkaneeshka namasivayamNo ratings yet
- Stem Cell ReportsDocument24 pagesStem Cell ReportsNguyen Dac Hanh HieuNo ratings yet