Professional Documents
Culture Documents
IHI Storyboard Adamski The Joint Commission PDF
Uploaded by
Teten RustendiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IHI Storyboard Adamski The Joint Commission PDF
Uploaded by
Teten RustendiCopyright:
Available Formats
13 Strategies for Patient Safety and
Joint Commission Compliance for 2013
Presenter: Patricia Adamski, RN, MS, MBA, FACHE, Director,
Standards Interpretation Group
The Joint Commission, Oakbrook Terrace, IL
Description: Strategies to help organizations focus patient safety and compliance initiatives and improve outcomes are provided along with the incorporation of the tools and resources that are available on The Joint Commission website and through
Joint Commission Connect.
Aim: To assist organizations in making the most of their compliance and patient safety initiatives
Actions Taken/Summary of Results: Ensuring patient safety and quality of care can be supported and achieved by compliance with Joint Commission Standards (which also incorporate the Medicare Conditions of Participation) and National Patient
Safety Goals. Looking at issues in isolation can cause additional issues and costs. By establishing a framework for compliance and safety efforts, staff, physicians and licensed independent practitioners can learn the expectations and can become
partners in these critical initiatives which in turn improves safety and outcomes for the patients your organization serves.
13 Strategies for Patient Safety and
Joint Commission Compliance for 2013
1. Establish a Culture of Safety
The more staff trust in leadership, the more likely they will report, which enables your organization to improve.
Front line staff know better than anyone where the risks and vulnerabilities reside in your organization. Increasing their comfort in reporting those risks and
vulnerabilities and encouraging them to report enables improvements to be implemented.
Creating a shared need helps everyone understand the focus and the necessity of a culture of safety.
The Three Imperatives of a Patient Safety Culture
Trust
Report
Improve
2. It Takes A Village
Develop a bench when it comes to patient safety and compliance. One person cannot carry all of the responsibility. Everyone needs at least one back-up
person who is knowledgeable and willing to step up and be involved.
Organizations that struggle with safety and compliance can be particularly challenged when the single person responsible suddenly leaves the organization or
has an extended absence. Build a team to initiate, support and sustain your efforts.
Written policies or SOPs can also assist in this regard. All of the important information your organization is dependent on should not reside only in someones
head!
John Smith
Local Hospital
123 Main Street
Anytown, IL 12345
HCO ID# 00000
3. Conduct Honest and Thorough Assessments of High Risk or Previously
Identified Areas
Hospital
What do you lose sleep over, what areas give you an unsettled feeling, what feedback are you hearing from the staff?
Select your team members/leaders based on their willingness to get into the weeds and really assess for problems.
You cant improve an area of risk that you have not identified.
ORGANIZATION SPECIFIC RISK AREAS
Latest PFP Report
Priority Focus Areas
Hospital
12
4. Be Creative in Your Evaluation Approaches
Copyright, The Joint Commission
RISK AREAS IDENTIFIED BY THE JOINT COMMISSION
Involving front line staff (after they have received some training in terms of what to look for, etc.) can be very helpful in identifying vulnerabilities because they
know where the problems are and may feel freer to discuss concerns with a peer.
Use front line staff to evaluate areas they are not as familiar with (staff from one unit evaluate systems and processes on another unit). Fresh eyes and ears can
pick up on nuances that those working the area may no longer be sensitive to.
Conduct tracers that follow a patient through the continuum of services.
Do a deep dive when you uncover potential issues or concerns and return/revisit as often as needed to really analyze the situation (is it an isolated situation or
one that seems to becoming the norm?).
5. Dont Assume Anything
Just because someone has been in their position for a long time or is recognized as knowing what they are doing doesnt mean they are compliant with your
policies and processes. Sometimes staff who have been in positions for a long time are assumed to be competent or current when in reality they are not.
Qualified supervisory or management staff are critical to success. Processes break down when the supervisor of an area does not have the competency to
provide proper oversight and when that happens, patients can be put at risk.
6. Dont Be Afraid of the Proactive Risk Assessment
Using the FMEA process described at the beginning of the Leadership Chapter describes the steps.
Breaking down the proactive risk assessment into manageable segments can be a helpful approach.
Using the Targeted Solutions Tool (TST) accessed through your extranet site is an effective way of meeting the proactive
risk assessment requirement.
The TST is available for the following projects:
Hand Hygiene
Hand-off Communications
Wrong Site Surgery
7. Periodically revisit previously identified areas of
risk and vulnerability
Just because you fixed the issue before doesnt mean you
have been able to sustain compliance. Use the Focused
Standards Assessment and Intracycle Monitoring profile tool
to help accomplish this strategy.
John Smith
PPR changes to FSA
Local Hospital
123 Main Street
Anytown, IL 12345
HCO ID# 00000
! The Rs
! Selectable Views All or required for submission
! Minimum Submission Subset
Whats New in the 2012 Mid-year PPR Update Read More
Coming in November PPR Changes to FSA Read More
14
Copyright, The Joint Commission
2"&H%#%-.:*DI5*0).2**D.62:27.
8. Evaluate Your Organizations Risk as New Data and Resources are Published
Review Sentinel Event Alerts as they are
published to determine applicability in your
organization.
:%050%D.JE%0#.(D%&#).
Review BoosterPaks as they become
available on Joint Commission Connect.
$DD"KJDD"',448G65D7L'
Utilize Leading Practice Library and the Core Measure Solution
Exchange found on Joint Commission Connect for solutions and
approaches to specific risks and vulnerabilities you have identified.
Consider submitting some of your solutions and practices to share
with other organizations.
! 8%G.)#"0-"&-.F%H"0.
Q==>.
#675>?A<@'B45'#4:9;4<8'
Leading Practice Library
! ]:<=^<=@<=@.
! ]:<=^<=@<=Z.
! _,`+ID#.0%G.C&*+%))%).
4*&.%0)I&,0H.#$%.WI"D,#1.
*4.D,+%0)%-.,0-%C%0-%0#.
C&"+55*0%&.+"&%.
Other Resources
Most Frequently Scored Standards
Standards FAQs
Electronic newsletters and alerts.
9. Handoffs and Sharing of Information is Critical to Success
When involving others in the safety and compliance initiatives, it is important to ensure open and honest communication.
Vulnerabilities in systems and processes that support patient safety and compliance frequently span departments, disciplines and chapters in the accreditation
manual.
Understanding the interdependencies is critical to success. Open dialog between groups and those responsible for the evaluation of the issues and areas must
be open to feedback and working together to make improvements.
Dont forget to look at policies that support cross-departmental processes and procedures. It is not uncommon to find discrepancies when policies are not centralized or consolidated. When each area has their own policy to address their part of the process, there can be significant disconnects that can lead to errors and
adverse outcomes.
10. Have the Right People at the Table
Once issues and vulnerabilities are identified, it is important to have stakeholders and those who actually own or contribute to the issues at the table in order to
develop solutions.
Pitting departments or groups against each other, assigning one discipline to oversee a solution or correction that is primarily the responsibility of another
discipline will only add to the problem. Dont create unnecessary conflict.
11. Connect the Dots for Staff and Leaders Alike
If you are leading safety and compliance initiatives it can be easy to forget that not everyone lives in your world.
Share the successes, the failures and most importantly the lessons learned.
Once you have identified the shared need under the Culture of Safety, it is critical to help staff, physicians and leaders see the connection between their
individual and departmental contributions to the initiatives and where the organization is in terms of improvements in patient safety.
12. Avoid the Tendency to Add on to Processes or On Top of Processes
Evaluate current processes and remove redundancies and non value-added work.
Embed the changes needed to improve the outcomes.
Dont be afraid to build the solution from the ground up. Sometimes trying to fix a broken process is far more challenging than just starting over.
Never automate a process until you fix the process, otherwise you just end up with a broken process that is automated and may cause more problems.
13. It Is Easier to Maintain Compliance and Keep Safety Initiatives Front and Center
than it is to Ramp Up and then Back Off
Keep the Statement of Conditions (SOC)
and Plan for Improvement (PFI) current
and use as a working document.
First screen entering the SOC
Become familiar with and monitor Joint Commissions website portals for High Reliability, Healthcare
Associated Infections, and Transitions of Care to name a few.
High Reliability
N%"D#$.!"&%'())*+,"#%-.304%+5*0).
2&"0),5*0).*4.!"&%.
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Swimming Is The Self-Propulsion of A Person Through WaterDocument3 pagesSwimming Is The Self-Propulsion of A Person Through WaterKryzler KayeNo ratings yet
- Group Health Presentation: Trademor Marketing (PVT) LimitedDocument32 pagesGroup Health Presentation: Trademor Marketing (PVT) Limitedkhinsha mujahidNo ratings yet
- Vibitha Joseph Naramvelil: Compassionate - Rehabilitation and Home Care Experience - MultilingualDocument3 pagesVibitha Joseph Naramvelil: Compassionate - Rehabilitation and Home Care Experience - MultilingualSanish ScariaNo ratings yet
- Linee Guida 2023 SCADocument53 pagesLinee Guida 2023 SCAdavidecicerone23No ratings yet
- Challenges and Issues Among FamiliesDocument4 pagesChallenges and Issues Among FamiliesAngela Nicolle ArdidNo ratings yet
- Workplace Wellness StudyDocument165 pagesWorkplace Wellness Studyapi-271658148No ratings yet
- Medinous Hospital Management System - HMS - Solution For HospitalsDocument7 pagesMedinous Hospital Management System - HMS - Solution For HospitalsElia MakhoulNo ratings yet
- Design and Commercialization of An End-to-End Continuous Pharmaceutical Production Process: A Pilot Plant Case StudyDocument16 pagesDesign and Commercialization of An End-to-End Continuous Pharmaceutical Production Process: A Pilot Plant Case Studykishore dasmunshiNo ratings yet
- Gangguan Inpartu - : Partus Lama - Prolaps Tali PusatDocument45 pagesGangguan Inpartu - : Partus Lama - Prolaps Tali PusatWulan Nindira WarasudiNo ratings yet
- GBS Vagus NerveDocument15 pagesGBS Vagus Nerveprintulmiorlau100% (3)
- Social WorkDocument16 pagesSocial WorkLuch Ahlet Ona100% (1)
- Syst Revw Schematic SummaryDocument10 pagesSyst Revw Schematic SummaryTrain-at- ThaurosNo ratings yet
- Role of GP in NHSDocument61 pagesRole of GP in NHSS M Niaz MowlaNo ratings yet
- Dental JurisprudenceDocument6 pagesDental JurisprudenceDeepuNo ratings yet
- KONFERENSI INFID 2013 - Diah - Saminarsih - Pencerah Nusantara Generic Slides - 20131121Document22 pagesKONFERENSI INFID 2013 - Diah - Saminarsih - Pencerah Nusantara Generic Slides - 20131121INFID JAKARTANo ratings yet
- Root Cause Analysis Template 3Document14 pagesRoot Cause Analysis Template 3Timmo KekelwaNo ratings yet
- Guided Self-Help Exercise Program in Total laryngectomy-RCT PDFDocument9 pagesGuided Self-Help Exercise Program in Total laryngectomy-RCT PDFazharbattooNo ratings yet
- Antibiotic Desensitization Protocols - 2Document7 pagesAntibiotic Desensitization Protocols - 2kadekapiklestariNo ratings yet
- Preventest Website PPDocument51 pagesPreventest Website PPapi-256933207No ratings yet
- Skills Laboratory: Shs - Up ManilaDocument14 pagesSkills Laboratory: Shs - Up ManilaAllen Rivera BuenaventuraNo ratings yet
- MGDS III Draft - August - Ed.final Final 16.08.17 (Sam)Document236 pagesMGDS III Draft - August - Ed.final Final 16.08.17 (Sam)AngellaNo ratings yet
- Director Nursing Behavioral Health in Pittsburgh PA Resume Cynthia DeLouisDocument2 pagesDirector Nursing Behavioral Health in Pittsburgh PA Resume Cynthia DeLouisCynthiaDeLouisNo ratings yet
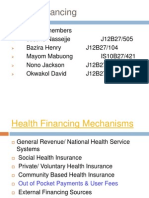
- Health Financing MechanismsDocument11 pagesHealth Financing MechanismsMayom MabuongNo ratings yet
- PostnatalDocument6 pagesPostnatalMadhu BalaNo ratings yet
- Saindhava Lavana - The Rock SaltDocument2 pagesSaindhava Lavana - The Rock SaltprasannarbNo ratings yet
- Health10 LM U1Document38 pagesHealth10 LM U1Che CastilloNo ratings yet
- Application of Principles of Sociology in Health CareDocument85 pagesApplication of Principles of Sociology in Health Caresagar matada vidyaNo ratings yet
- Coping With Stress: "Give Your Stress Wings and Let It Fly Away." Terri GuillemetsDocument24 pagesCoping With Stress: "Give Your Stress Wings and Let It Fly Away." Terri GuillemetsMARGIE MAE GONZALESNo ratings yet
- FORT MCCLELLAN VA S-C Decision Favorable To FT McClellan Vet (Citation #1108696)Document6 pagesFORT MCCLELLAN VA S-C Decision Favorable To FT McClellan Vet (Citation #1108696)Agent Orange Legacy100% (2)
- Triclosan 0410Document1 pageTriclosan 0410TeenahNo ratings yet