Professional Documents
Culture Documents
Adhesive
Uploaded by
Muaiyed Buzayan AkremyCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Adhesive
Uploaded by
Muaiyed Buzayan AkremyCopyright:
Available Formats
Masters of Esthetic Dentistry
PROFILE
jerd_337
194..199
Adhesive Dentistry. A Full Time
Practitioners Perspective
Jeff Brucia, DDS
JEFF BRUCIA, DDS*
Current Occupation
Private practice
Education
DDS, School of Dentistry, University of the
Pacific, 1988
Academic and Other Affiliations
Assistant Professor, Department of Dental
Care, UOP School of Dentistry
Co-Director, FACE Occlusion Study Club
Visiting faculty, University of Minnesota,
School of Dentistry, Post grad program
in restorative dentistry
Professional Memberships
Associate member of the AAED
Fellowship in the American College of
Dentists
Fellowship in the International College of
Dentists
Fellowship in the Pierre Fachard Academy
Doctoral degree with Delta Sigma Delta
Positions Held
Present Chair, CDA Presents, Board of
Managers, California Dental Association
Chair, Council on ADA Sessions and
Internation Programs, Local arrangements,
20072009
President, San Francisco Dental Society, 1998
Chair, San Francisco Dental Society Program
Committee, 19961998; 20032005
Chair, Program Committee, UOP School
of Dentistry 100-year Alumni Meeting, 1996
dhesive dentistry has provided
techniques and materials for
conservative and esthetic options
in every restorative practice. The
understanding of the process of
etching to form microscopic undercuts and infiltrating these gaps
with resin to create an adhesive
interface between tooth and restorative material has demonstrated
long-term durable and well-sealed
interfaces, resulting in excellent
clinical results. It has offered a
potentially reversible and repairable restoration that may be completed with little to no discomfort
to our patients (Figures 13).
Honors/Awards
Thomas P. Hinman Medallion, 2001
SFDS Presidential Meritorious Award for
Outstanding Leadership Qualities, 1999
CDA Outstanding Leadership and Grassroots
Actions, 1998
Delta Sigma Delta, Distinguished Service and
Meritorious Award, 1998
UOP Outstanding Teaching and Leadership
QualitiesPresented by the Senior class,
1992
Publications
A number of publications in the area of
adhesive and esthetic dentistry
Hobbies/Personal Interests
Competitive sail boat racing, mountain biking,
skiing
Notable Contribution(s)
to Dentistry
Has volunteered in numerous leadership
positions in organized dentistry over the
last 22 years to help promote quality care
and ethics throughout our profession
How has it changed since
1955 when Dr. Buonocore first
presented these concepts to the
dental world?1
In North America, adhesive dentistry in the 1960s80s was completely dependent on the covering
of any exposed dentin structure
prior to the use of a phosphoric
acid solution or gel on the enamel
for periods of a minute or more.
This treatment cleaned the surface
and created microscopic undercuts
in the underlying enamel. Rinsing
and drying the surface produced a
large, high-energy porous surface
that was ideal for bonding. This
junction was most durable if
completed in a completely
dry environment.
Early studies of the action of
different acid concentrations
revealed some interesting findings.
It was demonstrated that the
concentration of phosphoric acid
below 30% resulted in poorer
enamel adhesion. The testing
confirmed a surface layer that
was insoluble and would remain
as a contaminant on the enamel
surface. In concentrations above
30%, a soluble monocalcium salt
was formed, which was easily
removed by rinsing. The conclusion for ideal enamel etching
therefore was a solution of
between 30% and 40% placed
for 12 minutes, rinsed well, and
dried completely. An intermediate
layer of low-viscosity unfilled
resin was placed to improve
surface penetration and
adaption of the composite
restorative material.25
*Private practice, 1606 Stockton Street #305, San Francisco, CA 94133, USA
2010, COPYRIGHT THE AUTHOR
J O U R N A L C O M P I L AT I O N 2 0 1 0 , W I L E Y P E R I O D I C A L S , I N C .
194
DOI 10.1111/j.1708-8240.2010.00337.x
VOLUME 22, NUMBER 3, 2010
BRUCIA
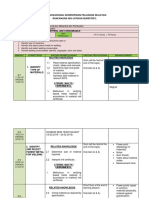
Figure 1. Adhesive procedure successfully applied to replace an older restoration.
Figure 2. Adhesive materials combined with minimally invasive procedures to improve the esthetics.
The early 1990s welcomed the
North American approval by dentists of acid treatment on both
enamel and dentin. Referred to as
total etch, phosphoric acid could
be placed on the dentin surface to
form micro porosities within the
intra-tubular dentin for resin penetration and micro-mechanical
attachment. Just like enamel, the
exchange process for dentin adhesion was the removal of the inorganic tooth material and the
replacement with a synthetic resin.
Etching dentin with 3040% phosphoric acid removes almost all of
the calcium phosphate and leaves
the collagen nearly completely
deprived of hydroxyapatite.68
The first systems to successfully
adhere to this demineralized dentin
surface were the three component
systems, also known as the
multiple-bottle etch and rinse
systems. Table 1. The first
component was the 3040%
phosphoric acid gel. The second
was the primer, and the third,
adhesive. The key material in
the primer is a bifunctional
monomer in a volatile solvent.
A bifunctional monomer has a
hydrophilic end and a hydrophobic
end. Examples would be HEMA
(2-hydroxyethyl methacrylate) or
4-META (4 methacryloxyethyl
trimellitic acid). The hydrophilic
end can infiltrate the demineralized
VOLUME 22, NUMBER 3, 2010
195
M A S T E R S F E AT U R E
Figure 3. Adhesive techniques used to conservatively treat a traumatic injury.
dentin structure with the help
of the solvent. The hydrophobic
end promotes the attachment of
the adhesive resin. The third
component is the adhesive resin.
It is an unfilled or partially
filled resin that binds to the
primer to form a resin
reinforced hybrid layer.7
T A B L E 1 . E T C H A N D R I N S E M U LT I P L E - B O T T L E S Y S T E M S .
Material
Manufacturer
Optibond FL
Scotchbond multi purpose plus
PermaQuik
All Bond II
Kerr
3M/ESPE
Ultradent
Bisco
TA B L E 2 . E T C H A N D R I N S E S I N G L E B O T T L E S Y S T E M S .
Material
Reviewing the research will
support the belief that this delivery
system still represents the gold
standard in adhesive dentistry
today. The newer systems available
present a different mode of action.
One marketed as a faster or more
simplified technique.9,10
The first change in this direction
was the combination of the
primer and adhesives into one
bottle (Table 2). Phosphoric acid
was still used on all surfaces of
the tooth followed by the combined primer/adhesive solution.
196
PQ-1
Prime & bond
Optibond solo plus
Singlebond
Even though the marketing
implied a faster application time,
years of clinical and lab testing
have demonstrated that application time may be equal to or
longer than the three component
systems if used with techniques
to achieve maximum potential.
Multiple coats are often necessary
to achieve adequate resin
2010, COPYRIGHT THE AUTHOR
J O U R N A L C O M P I L AT I O N 2 0 1 0 , W I L E Y P E R I O D I C A L S , I N C .
Manufacturer
Ultradent
Caulk/Dentsply
Kerr
3M/ESPE
thickness as the polymerization
stresses increase at the adhesivecomposite junction.11 Concern also
has been shown when used under
dual or self-cured composite.1214
Evidence of an acid-base reaction
and hydrolytic degradation demonstrated poor adhesion in these
clinical situations. Long-term
studies show more rapid
BRUCIA
T A B L E 3 . S E L F - E T C H I N G M AT E R I A L C AT E G O R I Z E D B Y P H .
Material
Strong pH < 1.0
Tyrian
Surpass
Prompt L-Pop
Moderate pH 12
Peak SE
AdheSE
iBond
Mild pH > 2.0
Clearfil SE
G-Bond
Optibond all-in-one
breakdown of the adhesive junction when these mixed systems
are used.1517
The complex chemistry of these
simplified systems produced an
increase in the post-operative sensitivity as seen by many practitioners. This observation was a major
driving force for the introduction
of a different mode of action.
The new mode of action was
reflected in self-etching or non-rinse
adhesive systems. The first systems
were two-component products. The
first bottle was an acidified primer
that was applied to the tooth structure but not rinsed off. Following
this, the adhesive resin was placed
and light-cured. They are thought
to reduce sensitivity for three reasons.1 The acid is less aggressive as
compared to the 3040% phosphoric acid.2 The resin infiltrates the
dematerialized dentin during the
pH
Manufacturer
0.4
0.6
0.8
Bisco
Apex
3M/ESPE
1.2
1.8
1.9
Ultradent
Ivoclar-Vivadent
Heraeus/Kulzer
2.0
2.3
2.6
Kuraray
GC America
Kerr
etching process, decreasing the
chance for voids.3 The smear plugs
are not removed from the heads
of the dentinal tubules.18
Most of these systems require
water to ionize the acid monomer.
The mineral component of the
smear layer then neutralizes the
acidity making it a non-rinse
system. It is important to understand that not all self-etching
systems work the same.19
I like to subdivide these based on
the aggressiveness of the acids
(Table 3). Strong self-etching
systems have a pH below 1. They
have a similar deep demineralization effect similar to phosphoric
acid on dentin. The collagen
network is completely exposed
and the hydroxyapatite dissolved.
Moderate self-etching systems
have pH levels between 1 and 2.
They produce a shallower demineralized zone and acid penetration, but still expose almost all of
the collagen and dissolve almost
all of the hydroxyapatite.
Mild self-etching systems have
pH levels above 2. They have a
shallow, partial demineralized
effect on dentin with residual
hydroxyapatite still attached
to the collagen. This surface
characteristic has been shown to
promote some chemical bonding
between the calcium and the
carboxylic acid or phosphatebased monomers like Phenyl-P
and 10-MDP. It is only in these
weak pH systems that both micromechanical and chemical adhesion
is seen at the dentin adhesion
interface. Maintaining some
hydroxyapatite for a chemical
bond may protect the collagen
matrix against hydrolysis and
early degradation of the bond.18,19
The most simplified of all the
modes available today are the
all-in-one self-etching systems.
They claim to accomplish all three
steps with a single application.
The thinness of the hybrid layer,
the aggressiveness of most of these
systems, and the incompatibility
with dual or self-cured composites
should cause concern in many
clinical situations. More testing
should be completed before this
material is recommended for
clinical use.
VOLUME 22, NUMBER 3, 2010
197
M A S T E R S F E AT U R E
Recent publications have supported
the use of the two-component mild
self-etching systems with the addition of phosphoric acid treatment
on the enamel only. This approach
may prove to be as good as the
early three component systems, but
care must be taken to not demineralize any of the underlying dentin
with the acid treatment.20,21
6.
7.
Basic understanding of the chemistry combined with some clinical
technique pearls can help achieve
the very best results in many
clinical situations.
8.
1. Isolation is a key component to
restorative success. Any contamination of the adhesive
surface will compromise results.
2. Maximize enamel bonding
whenever possible. (1) Clean the
enamel surface well with
pumice and water, (2) Consider
the placement of a bevel on the
enamel margins, and (3) Consider the use of phosphoric acid
on enamel surface as an additional step with a non-rinse
adhesive system.
3. Avoid over etching all
dentin surfaces.
4. Evaluate the quality and the
depth of the dentin surface and
consider the use of a Glass
Ionomer base or liner.
5. Place multiple layers of the
primer solution on all dentin
surfaces. Allow to remain on
the surface undisturbed for 15+
198
9.
seconds to aid in the complete
saturation of the demineralized
zone and the elimination
of voids.
Gently and thoroughly remove
the remaining solvent using the
lack of fluid movement as an
excellent visual tool.
Avoid over thinning of the
adhesive resin. If thinned
beyond the materials oxygen
inhibition zone thickness, polymerization prior to the placement of the restorative material
will be incomplete and will
adversely affect adhesion.
Review the system chemistry
for incompatibility concerns.
Some adhesive systems are
contraindicated under dual- or
self-cured restorative materials
and cements.
Place all light cured restorative
material in 2 mm increments
or less to allow maximum
polymerization and reduced
shrinkage stress.
A close look at the very best material combined with the perfect
clinical technique still shows need
for improvement. Degradation of
the denuded collagen within the
adhesive resin-infiltrated dentin
is still a major problem in dentin
bonding. This sometimes rapid and
other times slow breakdown leads
to nanoleakage along the dentinrestoration interface and loss of
retention of the composite restoration. What may be in our future to
2010, COPYRIGHT THE AUTHOR
J O U R N A L C O M P I L AT I O N 2 0 1 0 , W I L E Y P E R I O D I C A L S , I N C .
address these areas of concern?
I have been following two areas
of excitement.
1. The use of an antibacterial
agent (MDPB) in the primer
and sodium fluoride in the
adhesive to form an acid-base
resistant zone within the interface. This reinforced acid resistant dentin, or super dentin,
seen under the hybrid layer
could have the potential to
inhibit future demineralization
and help to form a more stable,
longer-lasting bond.22,23
2. Use of amorphous calcium
phosphate nanoprecursors to
remineralize the denuded collagen matrix and strengthen the
rein-dentin bond. There is currently work to study a process
of guided tissue remineralization
using a nanotechnology process
of growing mineral-rich crystals
and guiding then into the
demineralized gaps between
collagen fibers.24
As a full-time private practice
dentist, I need materials and techniques that will provide the very
best results for my patients. I
believe the research is clear in its
direction. The multiple-bottle, etch
and rinse systems are the gold
standards when used properly.10,25
Phosphoric acid etched enamel has
shown great results when evaluating composite placement completed
more than 30 years ago. I fear that
BRUCIA
our profession has committed itself
to the use of these simplified
systems and there is a false belief
that old is not as good and that
newer must be better. We should
be cautious as we read marketing
claims of the material of the
month. If so many new materials
are so good, why will their chemistry need modification in the next
year? When money is speaking, the
truth may be silent.
I do believe that there continues to
be very hard work to improve our
ability to provide our patients with
the very best care. I would ask that
we continue to require long-term
testing results to support marketing
claims. Our patients deserve the
very best, most tested, and proven
material available today.
4. Silverstone LM. Fissure sealants. Laboratory studies. Caries Res 1974;8(1):226.
5. Silverstone LM, Dogon IL. The acid etch
technique: in vitro studies with special
reference to the enamel surface and the
enamel resin interface. Internat sym on
the acid etch technique. St. Paul (MN):
North Central Publishing Co.; 1975,
pp. 1339.
6. Swift EJ, Perdigao J, Heymann HO.
Bonding to enamel and dentin: a brief
history and state of the art. Quintessence
Int 1995;26:95110.
7. Van Meerbeek BV, Vanherle G,
Lambrechts P, Braem M. Dentin
and enamel bonding agents. Curr
Opin Dent 1992;2:11727.
8. Charlton DG, Moore BK. Effects of age
of samples on the shear bond strength of
dentin bonding agents to dentin.
J Indiana Dent Assoc 1991;70:2336.
9. DeMunch J, Van Landuyt K, Peumans
M, et al. A critical review of the durability of adhesion to tooth tissue. Methods
and results. J Dent Res 2005;84(2):
11932.
10. Van Meerbeek B, Peumans M, Poitevin
A, et al. Relationship between bondstrength tests and clinical outcomes.
Dent Mater 2010;26:e10021.
DISCLOSURE
The author does not have any
financial interest in any companies
whose products are mentioned in
this paper.
REFERENCES
1. Buonocore MG. A simple method of
increasing the adhesion of acrylic filling
material to enamel surfaces. J D Res
1955;34(6):84953.
2. Chow LC, Brown WE. Phosphoric acid
conditioning of teeth for pit and fissure
sealants. J D Res 1973;52(5):1158.
3. Soetopo A, Beech DR, Hardwick JL.
Mechanism of adhesion of polymers to
acid etched enamel. J Oral Rehabil
1978;5(1):6980.
11. Hashimoto M, Sano H, Ichinose S,
Tagami J. Effects of multiple adhesive
coatings on dentin bonding. Oper Dent
2004;29:41623.
12. Sanares AM, Itthagarum A, King NM,
et al. Adverse surface interactions
between one-bottle light-cured adhesives
and chemical-cured composite.
Dent Mater 2001;17:54256.
13. Carvalho RM, Garcia FCP, Silva SMA,
Castro FLA. Adhesive-composite incompatibility, Part 1. J Esthet Restor Dent
2005;17:12934.
14. Carvalho RM, Garcia FCP, Silva SMA,
Castro FLA. Adhesive-composite incompatibility, Part 2. J Esthet Restor
Dent 2005;17:2037.
15. Tay FR, Carvalho RM, Pahley DH.
Water movement across bonded
dentintoo much of a good thing.
J Appl Oral Sci 2004;12:1225.
16. Tay FR, Pashley DH, Suh BI, et al.
Single-step adhesives are permeable
membranes. J Dent 2002;30:37182.
17. Yiu CK, King NM, Pashley DH, et al.
Effects of resin hydrophilicity and
water storage on resin bond strength.
Biomaterials 2004;25:578996.
18. Van Meerbeek B, Yoshida Y, DeMunck J,
et al. Correlative morphologic and
chemical interfacial characterization
of tooth-biomaterials interactions.
ProceedingInter Sym in Tokyo.
June 2001.
19. Tay FR, Pashley DH. Aggressiveness of
contemporary self-etching systems. I:
depth of penetration beyond dentin smear
layers. Dent Mater 2001;17:296308.
20. Pashley DH, Tay FR. Aggressiveness of
self-etching adhesives on unground
enamel. Dent Mater 2001;17:43040.
21. Brackett WW, Ito S, Nishitami Y, et al.
The microtensile bond strength of selfetching adhesives to ground enamel.
Oper Dent 2006;313:3327.
22. Shinohara M, De Goes M, Scheider L,
et al. Fluoride-containing adhesives:
durability in dentin bonding. Dent Mater
2009;25(11):12941.
23. Waidyasekera K, Nikaido T, Weerasinghe
D, et al. Reinforcements of dentin in selfetch adhesive technology: a new concept.
J Dent 2009;37:6049.
24. Tay FR, Pashley DH. Biomimetic remineralization of resin-bonded acid-etched
dentin. J Dent Res 2009;88(8):71924.
25. Heymann H, Wilder AD, Ritter A, et al.
12-year clinical evaluation of a dualcured dental adhesive. AIDR meeting.
#1239. 2008.
Reprint requests: Jeff Brucia, DDS, 1606
Stockton Street #305, San Francisco, CA
94133, USA; email: miramarjb@yahoo.com
VOLUME 22, NUMBER 3, 2010
199
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Questions (Multiple Correct Answers, Extended Matching and Ordering)Document111 pagesQuestions (Multiple Correct Answers, Extended Matching and Ordering)gary_singh_198195% (19)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Chapter 9 Refrigerant Containment Recovery Recycling and ReclamationDocument8 pagesChapter 9 Refrigerant Containment Recovery Recycling and ReclamationJose Mendoza100% (1)
- Book - MOSBY'S DENTAL DRUG REFERENCE PDFDocument1,496 pagesBook - MOSBY'S DENTAL DRUG REFERENCE PDFMohamed Faizal78% (9)
- AQUISEL Tubos Instrucciones-EnglishDocument20 pagesAQUISEL Tubos Instrucciones-Englishkukuh100% (1)
- A Molecular Approach Chapter 11Document191 pagesA Molecular Approach Chapter 11Stephen0% (1)
- Teeth Selection PDFDocument70 pagesTeeth Selection PDFMuaiyed Buzayan AkremyNo ratings yet
- Teeth RestorabilityDocument6 pagesTeeth RestorabilityMuaiyed Buzayan AkremyNo ratings yet
- Distraction Osteogenesis For Ridge Augmentation PR PDFDocument11 pagesDistraction Osteogenesis For Ridge Augmentation PR PDFMuaiyed Buzayan AkremyNo ratings yet
- Timonen2020 Article VirtualRealityImprovesTheAccurDocument12 pagesTimonen2020 Article VirtualRealityImprovesTheAccurMuaiyed Buzayan AkremyNo ratings yet
- IPS E-Max Clinical GuideDocument40 pagesIPS E-Max Clinical GuideMuaiyed Buzayan AkremyNo ratings yet
- Timonen2020 Article VirtualRealityImprovesTheAccurDocument12 pagesTimonen2020 Article VirtualRealityImprovesTheAccurMuaiyed Buzayan AkremyNo ratings yet
- Hi Every OnDocument1 pageHi Every OnMuaiyed Buzayan AkremyNo ratings yet
- Accuracy of new elastomeric impression material for complete arch dental implantsDocument1 pageAccuracy of new elastomeric impression material for complete arch dental implantsMuaiyed Buzayan AkremyNo ratings yet
- Accuracy of new elastomeric impression material for complete arch dental implantsDocument2 pagesAccuracy of new elastomeric impression material for complete arch dental implantsMuaiyed Buzayan AkremyNo ratings yet
- Teeth WearDocument7 pagesTeeth WearMuaiyed Buzayan AkremyNo ratings yet
- Ceph DssDocument10 pagesCeph DssMuaiyed Buzayan AkremyNo ratings yet
- Patient 1 DssDocument8 pagesPatient 1 DssMuaiyed Buzayan AkremyNo ratings yet
- Hello 12112Document1 pageHello 12112Muaiyed Buzayan AkremyNo ratings yet
- Rests & Rest Seats-CHAPTER2Document7 pagesRests & Rest Seats-CHAPTER2Muaiyed Buzayan AkremyNo ratings yet
- Patient 1 DssDocument8 pagesPatient 1 DssMuaiyed Buzayan AkremyNo ratings yet
- Patient 1 DssDocument8 pagesPatient 1 DssMuaiyed Buzayan AkremyNo ratings yet
- Ceph DssDocument10 pagesCeph DssMuaiyed Buzayan AkremyNo ratings yet
- Nicks SegiDocument8 pagesNicks SegiMuaiyed Buzayan AkremyNo ratings yet
- Tooth and Pulp Anatomy GuideDocument63 pagesTooth and Pulp Anatomy GuideMuaiyed Buzayan AkremyNo ratings yet
- 7 130p D PDFDocument108 pages7 130p D PDFEzza RiezaNo ratings yet
- Dental Care PDFDocument16 pagesDental Care PDFMuaiyed Buzayan AkremyNo ratings yet
- The Indefinite Articles: A, AnDocument3 pagesThe Indefinite Articles: A, Ansam_kamali85No ratings yet
- Ceph DssDocument10 pagesCeph DssMuaiyed Buzayan AkremyNo ratings yet
- 2015 FDI - Complete - Oral Health - Atlas PDFDocument63 pages2015 FDI - Complete - Oral Health - Atlas PDFBogdanNo ratings yet
- 7 130p D PDFDocument108 pages7 130p D PDFEzza RiezaNo ratings yet
- Tooth and Pulp Anatomy GuideDocument63 pagesTooth and Pulp Anatomy GuideMuaiyed Buzayan AkremyNo ratings yet
- 2015 FDI - Complete - Oral Health - Atlas PDFDocument63 pages2015 FDI - Complete - Oral Health - Atlas PDFBogdanNo ratings yet
- Oral Pathologydd2011-2012 PDFDocument184 pagesOral Pathologydd2011-2012 PDFMuaiyed Buzayan AkremyNo ratings yet
- Technical Information: Glossary of TermsDocument30 pagesTechnical Information: Glossary of Termsjosette_hajjarNo ratings yet
- A Comparative Clinical Study On The Effect of Mrittika Lepa and Lodhradi Lepa in Yuvanapidika W.S.R To Acne VulgarisDocument6 pagesA Comparative Clinical Study On The Effect of Mrittika Lepa and Lodhradi Lepa in Yuvanapidika W.S.R To Acne VulgarisIJAR JOURNALNo ratings yet
- RSL - Modul MTK 1023 Material ConsumableDocument6 pagesRSL - Modul MTK 1023 Material ConsumableGraceLamNo ratings yet
- CCTTC - SCM822H Datasheet, Chemical CompositionDocument3 pagesCCTTC - SCM822H Datasheet, Chemical CompositionSOEN, PETER STANLEYNo ratings yet
- Mcgregor 1996Document13 pagesMcgregor 1996Alrayyan RashidNo ratings yet
- Journal of Chromatographic PDFDocument8 pagesJournal of Chromatographic PDFGustavo Balarezo InumaNo ratings yet
- Identification of AnionsDocument1 pageIdentification of AnionsJevon BrownNo ratings yet
- Water TreatmentDocument12 pagesWater TreatmentSata AjjamNo ratings yet
- Button Head Socket Screws Metric Technical SpecificationDocument1 pageButton Head Socket Screws Metric Technical SpecificationXto PeregrinNo ratings yet
- Sample Paper-01 Scholastic Aptitude Test: SAT AllenDocument8 pagesSample Paper-01 Scholastic Aptitude Test: SAT AllenSachin Kumar100% (1)
- Efek Ekstrak Buah Mengkudu (Morinda Citrifolia) Terhadap Kadar Enzim SGOT Dan SGPT Pada Mencit Dengan Induksi Karbon TetrakloridaDocument7 pagesEfek Ekstrak Buah Mengkudu (Morinda Citrifolia) Terhadap Kadar Enzim SGOT Dan SGPT Pada Mencit Dengan Induksi Karbon TetrakloridaSalsa MoriaNo ratings yet
- ANTHE-2020 - (VIII Moving To IX) - (Code-O) - 13-12-2020Document14 pagesANTHE-2020 - (VIII Moving To IX) - (Code-O) - 13-12-2020Lakshman RaiNo ratings yet
- Question BankDocument19 pagesQuestion BankKUNALNo ratings yet
- Unit Iv Abrasive Processes and Gear Cutting: 4.1 GrindingDocument30 pagesUnit Iv Abrasive Processes and Gear Cutting: 4.1 Grindingrkscad11No ratings yet
- SAFETY DATA Akzo Nobel India LimitedDocument12 pagesSAFETY DATA Akzo Nobel India LimitedSwapneelThombareNo ratings yet
- Corrugated Plate Interceptor: Applications For CPI SystemsDocument2 pagesCorrugated Plate Interceptor: Applications For CPI SystemsFelipe BrainNo ratings yet
- Makrolon LED2245 - en - 81038415 00003726 19218403Document4 pagesMakrolon LED2245 - en - 81038415 00003726 19218403dave judayaNo ratings yet
- Strength & Durability of Pervious Concrete with SCMsDocument14 pagesStrength & Durability of Pervious Concrete with SCMsAnsar AsrNo ratings yet
- Preview ISA+S12.1-1991Document9 pagesPreview ISA+S12.1-1991nelson lozaNo ratings yet
- Materials Science Involves Investigating The Relationships ThatDocument7 pagesMaterials Science Involves Investigating The Relationships ThatGiselle LisondraNo ratings yet
- Molecular DiffusionDocument11 pagesMolecular Diffusionkiran367No ratings yet
- Internship Report, Etihad Sugar Mills Limted, RYKDocument13 pagesInternship Report, Etihad Sugar Mills Limted, RYKMohammad Usman HabibNo ratings yet
- 8273 Dr. A. Santos Ave., Parañaque City Tel. Numbers: 02-820-2222/02-820-4276Document3 pages8273 Dr. A. Santos Ave., Parañaque City Tel. Numbers: 02-820-2222/02-820-4276John Raniel IsidroNo ratings yet
- Hydrogen CHEMHACKDocument7 pagesHydrogen CHEMHACKMonika BoranaNo ratings yet
- Lignin Process Kraft 42400 - v1 - 17Document27 pagesLignin Process Kraft 42400 - v1 - 17V U P RaoNo ratings yet
- Reasoning Based Questions (6 Marks) Section-ADocument4 pagesReasoning Based Questions (6 Marks) Section-ARishi SharmaNo ratings yet
- Self-Etching Adhesives Increase Collagenolytic Activity in Radicular DentinDocument7 pagesSelf-Etching Adhesives Increase Collagenolytic Activity in Radicular DentinPablo BenitezNo ratings yet