Professional Documents
Culture Documents
GHFFG PDF
Uploaded by
George Herland PradiktaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
GHFFG PDF
Uploaded by
George Herland PradiktaCopyright:
Available Formats
British Journal of Anaesthesia 1995; 74: 517-520
Prophylactic i.m. ephedrine in bupivacaine spinal anaesthesia
J.-E. STERNLO, A. RETTRUP AND R. SANDIN
Summary
In a double-blind, placebo-controlled, randomized
study, we have investigated the efficacy of i.m.
ephedrine in 98 elderly patients undergoing hip
arthroplasty under spinal anaesthesia with plain
bupivacaine. Fifty patients received ephedrine
0.6 mg kg"
1
body weight, deep in the paravertebral
muscles immediately after injection of bupivacaine,
and 48 received an equal volume of saline. Patients
in both groups were given the same volumes of
fluid before anaesthesia. Systolic arterial pressure
during the first 60 min after anaesthesia remained
significantly more stable in the ephedrine-treated
group, and there was also a significantly smaller
number of patients in this group who had decreases
in pressure of more than 30% of pre-block levels,
and fewer required rescue i.v. ephedrine. An
increase in heart rate or systolic pressure of ^ 20%
from baseline was found in two patients in the
ephedrine group and in one patient in the placebo
group. We conclude that ephedrine 0.6 mg kg"
1
body weight administered in the paravertebral
muscles immediately after plain bupivacaine spinal
anaesthesia is a simple and effective means of
reducing the incidence of hypotensive episodes in
the elderly patient. (Br. J. Anaesth. 1995; 74:
517-520)
Key wor ds
Anaesthetic techniques, subarachnoid. Sympathetic nervous
system, ephedrine. Complications, hypotension.
Ephedrine is an alkaloid originally extracted from
the Chinese plant Ma Huang, used in traditional
Chinese medicine for centuries. In the late 1920s,
this sympathomimetic amine was introduced as a
vasopressor into anaesthetic practice by Ockerblad
and Dillon [1]. Its modern synthetic congener
remains a drug of choice for treating hypotension
induced by spinal or extradural anaesthesia [2]. The
dose and timing of administration, however, have
not been fully investigated, although the trend today
seems to favour i.v. administration, either in titrated
single doses or as a continuous infusion. The efficacy
of prophylactic i.m. ephedrine has been questioned
and there is concern regarding the potential for
causing harmful hypertension or tachycardia [2-5].
However, Hemmingsen, Poulsen and Risbo
administered a combination of i.v. and i.m. eph-
edrine after bupivacaine spinal anaesthesia, and
found this regimen satisfactory in counteracting
hypotension without undue hypertension or tachy-
cardia [6]. In all previous studies with the i.m. route,
fixed doses of ephedrine have been used.
The aim of our study was to investigate the
efficacy of ephedrine in maintaining haemodynamic
stability in elderly patients when administered in a
single i.m. dose determined by body weight and
given at the same time as spinal anaesthesia.
Patients and methods
This double-blind, placebo-controlled, randomized
study was approved by the Ethics Committee at the
University in Linkoping. We studied 100 consecu-
tive patients undergoing total hip replacement under
spinal anaesthesia with plain bupivacaine. One
patient was excluded as it was not possible to
perform the spinal block, and another because of
incomplete data, leaving 98 patients for evaluation.
Premedication was given approximately 1 h before
anaesthesia with i.m. ketobemidone 5-10 mg and
i.m. dixyrazine 10-20 mg according to age and body
weight (ketobemidone is not available in the UK;
ketobemidone is an opioid, 5 mg is equipotent to
morphine 5-8 mg [7], dixyrazine is a low-dose
phenothiazine with sedative and marked antiemetic
properties [8]). Patients medicated with beta receptor
or calcium channel blockers were given their or-
dinary morning doses. During the 20-min period
before anaesthesia the patients received 3 % dextran
solution (Plasmodex, Pharmacia AB, Sweden) 7 ml
kg"
1
body weight. Systolic arterial pressure (SAP)
was measured with a calibrated aneroid sphyg-
momanometer and radial pulse palpation. Heart rate
(HR) was obtained from a three-lead ECG. Spinal
anaesthesia with 0.5 % plain bupivacaine 20 mg was
performed in the L2-3 or L3-4 interspaces with the
patient in the sitting position. Morphine 0.3 mg was
added to the bupivacaine solution. Immediately after
completion of the spinal injection, the needle was
withdrawn and redirected laterally, and 0.012 ml
kg"
1
body weight of the trial solution was injected
deep into the paravertebral muscles. The solution
comprised either ephedrine 0.6 mg kg"
1
body
weight or saline. The patient was then placed
immediately in the lateral position. After anaesthesia,
J.-E. STERNLO, MD, DEAA, A. RETTRUP, RN, R. SANDIN, MD, PHD,
Department of Anaesthesia, Lanssjukhuset, S-391 85 Kalmar,
Sweden. Accepted for publication: December 2, 1994.
b
y
g
u
e
s
t
o
n
A
u
g
u
s
t
6
,
2
0
1
2
h
t
t
p
:
/
/
b
j
a
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
518 British Journal of Anaesthesia
the 3 % dextran solution was continued at a rate of
1 ml kg"
1
h"
1
and a crystalloid solution with 2.5 %
glucose (Rehydrex Pharmacia AB, Sweden) was
started and continued at a rate of 4 ml kg"
1
h"
1
throughout surgery.
A decrease in SAP of > 30 % from the baseline
recording to less than 100 mm Hg was treated
immediately with i.v. ephedrine in 5-mg increments
until a stable SAP above this threshold level was
established. Plasma volume maintenance with 3%
dextran (in addition to the continuous infusion rate
of 1 ml kg"
1
h"
1
) and packed red cell transfusions to
compensate for intraoperative blood loss were based
on a computer-generated scheme for each individual
patient, taking into account age, sex, body weight
and height, preoperative haemoglobin (Hb) con-
centration and predetermined lowest acceptable
postoperative Hb. In order to provide a comfortable
state during surgery, midazolam was administered as
required in doses of 1.25 mg. In a few patients small
doses of i.v. fentanyl were given to alleviate pain
from unanaesthetized areas caused by the uncomfort-
able lateral position. Dixyrazine was given in i.v.
doses of 5 mg to treat nausea.
SAP and HR were recorded before anaesthesia, 2
and 5 min after anaesthesia, and every 5 min there-
after. All SAP measurements were obtained from the
upper arm. A reduction in SAP > 30 % from the
baseline level was considered a negative outcome in
terms of efficacy, whereas increases in SAP ^ 20 %
to a level ^160 mm Hg, and in HR ^ 20 % to a level
^ 90 beat min"
1
were considered adverse reactions.
The groups were compared by Mann-Whitney U
test and regression analysis, as appropriate. P < 0.05
was considered significant.
Results
There were no differences between the groups in
patient characteristics, baseline haemodynamic state,
time from anaesthesia to surgery, intraoperative
volume replacement or bleeding (table 1). There
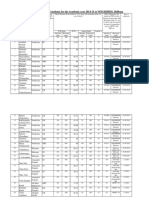
Table 1 Patient data, peroperative blood loss, and fluid and
blood replacement (mean (SD or range) or number). No
significant differences between groups
Table 2 Cumulated doses of midazolam and fentanyl (mean
(SD) [range]). Median = 0 for fentanyl in both groups, and
1.25 mg for midazolam in both groups. No significant
differences between groups
Sex (M: F)
Age (yr)
ASA I: II: III:IV
p and/or Ca blockers ()
Height (cm)
Weight (kg)
Haemoglobin (g dl"
1
)
SAP (mm Hg) (upper arm,
lateral pos.)
HR (beat min-
1
)
Duration of surgery (min)
Time anaesthesia to surgery
(min)
Peroperative blood loss (litre)
3 % Dextran (litre)
Crystalloid (litre)
Packed red cells (litre)
Placebo
group
48
20:28
69 (43-86)
18:24:6:0
12
168 (8)
73(15)
13.7(1.5)
143(26)
74(12)
118(34)
48(11)
1.1(0.7)
1.2 (0.3)
1.3 (0.4)
0.26 (0.47)
Ephedrine
group
50
20:30
70 (37-89)
21:20:8:1
7
168 (9)
76 (16)
13.7(1.8)
148(31)
75(12)
114(33)
51 (10)
1.0(0.6)
1.1(0.3)
1.2(0.4)
0.32 (0.49)
Midazolam (mg)
Fentanyl (|ig)
160 T
150
- 1 4 0 -
I
130-
E
o. 120-
w
no
100-
90-
<
1
) T
Ephedrine group
1.3 (1.3) [0-5]
6.0 (22.0) [0-100]
Placebo group
1.2 (1.2) [0-3.75]
1.0 (8.0) [0-50]
10 20 30 40
Time (min)
50 60
Figure 1 Systolic arterial pressure (mean, SEM) during the first
60 min after anaesthesia in the placebo (O) and ephedrine ( #)
groups. Except at time = 0, all differences were significant
(P < 0.05).
were no significant differences in the amount of
midazolam or fentanyl given within 5, 10, 30 and
60 min after anaesthesia or in the total cumulated
doses throughout the whole procedure (table 2).
Spinal anaesthesia was successful in all patients.
The median values of the upper segmental sensory
level of the spinal anaesthesia (determined by the
cold discrimination test) were T4 (range T3-10) and
T5 (T2-10) for the ephedrine-treated and placebo
groups, respectively. Regression analysis did not
reveal any significant relation between the level of
sensory analgesia and SAP every 5 min during the
first 60 min after the block. The incidence of nausea
and vomiting and the amounts of antiemetics
administered during operation and within 12 h after
operation did not differ significantly between the
groups. SAP in the placebo group was significantly
lower compared with the ephedrine group when
assessed every 5 min after anaesthesia, and the
reduction in SAP compared with the corresponding
baseline value was significantly more pronounced in
the placebo group 10 min after anaesthesia (P <
0.008) and throughout the first hour after anaesthesia
(fig. 1). There were also statistically significant
differences between the groups in the percentage of
patients given rescue i.v. ephedrine aimed at main-
taining SAP above the threshold level (fig. 2). These
differences were apparent when the groups were
compared during the first 60 min after anaesthesia,
and also throughout the whole procedure.
The number of patients with reductions in SAP of
more than 30% from the baseline level was signifi-
cantly lower in the ephedrine group at 10, 25, 45, 50
and 55 min after anaesthesia (table 3). No patient in
b
y
g
u
e
s
t
o
n
A
u
g
u
s
t
6
,
2
0
1
2
h
t
t
p
:
/
/
b
j
a
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
Prophylactic ephedrine 519
80
60
s .
4 0
-^ 20
< 30 min 30-60 min > 60 min i Total
Figure 2 Percentage of patients given i.v. rescue ephedrine
according to study criteria with regard to time after anaesthesia
in the ephedrine ( ) and placebo ( ) groups. The difference
obtained within 30 min was significant at P < 0.01 and the
other comparisons at P < 0.001.
Table 3 Number of patients with a reduction in systolic
arterial pressure > 30 % of that before anaesthesia within the
first hour after anaesthesia (mean reduction (Reduction %)).
Group P = placebo, group E = ephedrine. * P < 0.05
Time after block
(min) Group n
Reduction
o/
/o
5
10
15
20
25
30
35
40
45
50
55
60
P
E
P
E
P
E
P
E
P
E
P
E
P
E
P
E
P
E
P
E
P
E
P
E
3
0
10*
0
6
2
6
2
6*
1
7
3
12
9
16
9
16*
6
20*
7
24*
7
20
11
44
34
38
33
36
37
37
33
34
37
39
33
39
36
35
39
38
36
37
39
38
36
the placebo group received midazolam or fentanyl
within 10 min after anaesthesia and after sedatives or
analgesics were administered, no correlations be-
tween SAP and administration of these drugs were
found.
Seven patients in the ephedrine group and 12 in
the placebo group were receiving medication with
beta adrenergic, calcium channel blockers, or both.
In these patients the value of SAP was higher at all
times after anaesthesia if prophylactic ephedrine had
been given and this difference was statistically
significant at 10 min, and between 35 and 60 min of
anaesthesia. The need for rescue i.v. ephedrine in
patients treated with beta adrenergic, calcium chan-
nel blockers, or both, was significantly less if
prophylactic ephedrine had been given (table 4). In
the corresponding subgroup of patients not treated
with beta adrenergic or calcium channel blockers,
the significant differences in SAP between the two
groups were consistent with the data for all of the
patients studied, as indicated in figure 1. The need
for rescue ephedrine in patients not treated with beta
adrenergic or calcium channel blockers is shown in
table 4.
An increase of more than 20% in SAP (from 160
to 210mmHg) was observed in one patient in the
ephedrine-treated group. HR was unchanged at 120
beat min"
1
. One patient in each group had an increase
in HR of more than 20%, the one in the untreated
group from 95 to 125 beat min"
1
and in the ephedrine
group from 80 to 107 beat min"
1
.
Discussion
Hypotension after spinal or extradural block may be
hazardous in patients with a compromised arterial
supply to vital organs (i.e. coronary and cerebral
circulations), but may also reflect a reduction in
afterload, which in most cases is beneficial [3]. As
there is no method to assess with accuracy the lowest
acceptable arterial pressure in the individual patient,
the decision to administer drugs to increase arterial
pressure is dependent on the anaesthetist's judge-
ment. Thus our decision to give i.v. ephedrine if
SAP decreased by more than 30% to less than
100 mm Hg was partly empirical.
It has been observed that volume expansion alone
with colloid or crystalloid solutions has not been
consistently effective in attenuating hypotension
induced by spinal or extradural anaesthesia and it
may even by harmful in the elderly patient with
incipient heart failure [2, 3]. Of the vasoactive drugs
suitable for prophylaxis, ephedrine is generally
agreed as the most appropriate. I.v. infusions of
ephedrine or intermittent i.v. doses titrated to
response are the techniques most often recom-
mended. However, as hypotension may develop
rapidly after spinal anaesthesia, optimal SAP control
with these techniques calls for very close monitoring
by invasive or automated techniques, and these are
not always feasible. On the other hand, i.m. prophy-
lactic administration of ephedrine is generally not
recommended because of the alleged unpredictable
absorption from the injection site and the belief that
a relative overdose may result in hypertension,
Table 4 Number of administered rescue doses of ephedrine (5 mg i.v.) within 1 h after anaesthesia (< 1 h) and
during the entire procedure (Total) in patients with (cardiovascular medication) and without (no cardiovascular
medication) treatment with beta-adrenergic, calcium channel blockers, or both. Data are mean (SD) [median]
Cardiovascular medication No cardiovascular medication All patients
Placebo
(n = 12)
Ephedrine
( = 7) P
Placebo
(n = 36)
Ephedrine
(n = 43) P
Placebo
( = 48)
Ephedrine
(n = 50) P
< l h 1.8 (1.2) [2] 0.3 (0.5) [0] 0.01
Total 3.8 (2.0) [4] 1.0 (1.9) [0] 0.01
0.8 (1.2) [0] 0.2 (0.5) [0] 0.01
2.1 (1.8) [2] 0.9 (1.5) [0] 0.01
1.0 (1.3) [1] 0.2 (0.5) [0] 0.0001
2.5 (2.0) [2] 1.0 (1.5) [0] 0.0001
b
y
g
u
e
s
t
o
n
A
u
g
u
s
t
6
,
2
0
1
2
h
t
t
p
:
/
/
b
j
a
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
520 British Journal of Anaesthesia
tachycardia, or both, which may be detrimental [2,
3]. Indeed, use of the i.m. route in obstetric spinal or
extradural anaesthesia has been condemned. In a
study by Rolbin and colleagues in which ephedrine
was given i.m. 15-30 min before extradural an-
aesthesia for elective Caesarean section, ephedrine
25 mg was ineffective in reducing the incidence
of maternal hypotension, while a dose of 50 mg
produced unacceptable hypertension which was
associated with derangement in fetal acid-base status
[4]. Rout and co-workers also recommended that
prophylactic i.m. ephedrine not be used before
obstetric spinal or extradural anaesthesia in case the
block should fail and it became necessary to resort to
general anaesthesia [5].
However, in non-obstetric cases, Hemmingsen,
Poulsen and Risbo administered i.m. ephedrine
37.5 mg after an initial i.v. bolus of 12.5 mg. This
was compared with placebo in 48 patients under-
going surgery of the lower abdomen or lower
extremities during bupivacaine spinal anaesthesia.
Greater stability of arterial pressure occurred in
ephedrine-treated patients, especially in a subgroup
of ASA III patients, where all eight patients in the
placebo group had a decrease in mean arterial
pressure exceeding 33 % compared with none in the
ephedrine-treated group. Tachycardia or hyperten-
sion was not observed [6].
It seems that the problem associated with i.m.
ephedrine is that of a reliable regimen which is both
effective and also avoids overdosage. Surprisingly,
matching the dose to body mass has not been
undertaken in the earlier studies. From our previous
clinical experience it seemed that an i.m. dose of
0.6 mg kg"
1
was appropriate and that reliable ab-
sorption could be expected if ephedrine was injected
deep into the paravertebral muscles. In our study we
found that this regimen provided a significant
stabilizing effect on SAP throughout the study
period of 1 h and that this effect was evident both in
the presence and absence of beta adrenergic or
calcium channel blockers, or both.
The detailed part of this study was terminated
60 min after anaesthesia, as we expected that the
effects of i.m. ephedrine would have terminated
within this period and also we expected that any
difference in haemodynamic state would be in-
fluenced or obscured by surgical blood loss and
cementing. Nevertheless, the percentage of patients
treated with i.v. ephedrine after the first 60 min was
also significantly higher (70 % vs 31 %; P < 0.001) in
the placebo group.
The price paid for SAP stability in the ephedrine
group may have been a 31 % increase in SAP in a
patient suffering from heart failure, atrial fibrillation
and diabetes who was haemodynamically unstable
both before and during anaesthesia. Increases in HR
occurred in one patient in each group. These results
must be weighed against the significantly inferior
haemodynamic stability in a substantial number of
patients in the placebo group. The incidence of
nausea and vomiting during and after operation was
not affected by the use of ephedrine [9] and there was
no effect on blood loss and need for intraoperative
transfusion [10]. Finally, it should be emphasized
that we used plain bupivacaine, which has a rather
slow onset of action compared with other local
anaesthetics [11]. Our results can not be indis-
criminately applied therefore to all situations where
spinal anaesthesia is used.
References
1. Ockerblad NF, Dillon TG. The use of ephedrine in spinal
anesthesia. Journal of the American Medical Association 1927;
88: 1135-1136.
2. Morgan P. The role of vasopressors in the management of
hypotension induced by spinal and epidural anaesthesia.
Canadian Journal of Anaesthesia 1994; 41: 404-413.
3. McCrae AF, Wildsmith JAW. Prevention and treatment of
hypotension during central neural block. British Journal of
Anaesthesia 1993; 70: 672-680.
4. Rolbin SH, Cole AFD, Hew EM, Pollard A, Virgint S.
Prophylactic intramuscular ephedrine before epidural an-
aesthesia for caesarean section: Efficacy and actions on the
foetus and newborn. Canadian Anaesthetists Society Journal
1982; 29: 148-153.
5. Rout CC, Rocke DA, Brijball R, Kovarjee RV. Prophylactic
intramuscular ephedrine prior to caesarean section. An-
aesthesia and Intensive Care 1992; 20: 448-452.
6. Hemmingsen C, Poulsen JA, Risbo A. Prophylactic ephedrine
during spinal anaesthesia: double-blind study in patients in
ASA groups IIII. British Journal of Anaesthesia 1989; 63:
340-342.
7. Ohqvist G, Hallin R, Gelinder S. A comparison between
morphine, meperidine and ketobemidone in continuous
intravenous infusion for postoperative pain relief. Acta
Anaeslhesiologica Scandinavica 1991; 35: 4448.
8. Larsson S, Hagerdal M, Lundberg D. Premedication with
intramuscular dixyrazine. A controlled double-blind com-
parison with morphine-scopolamine and placebo. Ada
Anaesthesiologica Scandinavica 1988; 32: 131-134.
9. Rothenberg DM, Parnass SM, Litwack K, McCarthy RJ,
Newman ML. Efficacy of ephedrine in the prevention of
postoperative nausea and vomiting. Anesthesia and Analgesia
1991; 72: 58-61.
10. Thorburn J. Subarachnoid blockade and total hip replace-
ment. Effect of ephedrine on intraoperative blood loss. British
Journal of Anaesthesia 1985; 57: 290-293.
11. Tuominen M. Bupivacaine spinal anaesthesia. Acta Anaes-
thesiologica Scandinavica 1991; 35: 110.
b
y
g
u
e
s
t
o
n
A
u
g
u
s
t
6
,
2
0
1
2
h
t
t
p
:
/
/
b
j
a
.
o
x
f
o
r
d
j
o
u
r
n
a
l
s
.
o
r
g
/
D
o
w
n
l
o
a
d
e
d
f
r
o
m
You might also like
- KomDocument8 pagesKomGeorge Herland PradiktaNo ratings yet
- KomDocument8 pagesKomGeorge Herland PradiktaNo ratings yet
- YrtyrtDocument1 pageYrtyrtGeorge Herland PradiktaNo ratings yet
- WWWDocument1 pageWWWGeorge Herland PradiktaNo ratings yet
- Opioid Pharmacology: Pain Physician 2008: Opioid Special Issue: 11: S133-S153 - ISSN 1533-3159Document22 pagesOpioid Pharmacology: Pain Physician 2008: Opioid Special Issue: 11: S133-S153 - ISSN 1533-3159Suresh KumarNo ratings yet
- EeeDocument1 pageEeeGeorge Herland PradiktaNo ratings yet
- RRRHJKKHDocument1 pageRRRHJKKHGeorge Herland PradiktaNo ratings yet
- ZXCDocument1 pageZXCGeorge Herland PradiktaNo ratings yet
- Jbsi 18 NXJPW 0 U 1Document1 pageJbsi 18 NXJPW 0 U 1George Herland PradiktaNo ratings yet
- BBBDocument1 pageBBBGeorge Herland PradiktaNo ratings yet
- JNC 7 (Klasifikasi Hipertensi) PDFDocument2 pagesJNC 7 (Klasifikasi Hipertensi) PDFAbdur RahmanNo ratings yet
- Googles BookDocument1 pageGoogles BookGeorge Herland PradiktaNo ratings yet
- Popo PopDocument1 pagePopo PopGeorge Herland PradiktaNo ratings yet
- Serial NoDocument1 pageSerial NoGeorge Herland PradiktaNo ratings yet
- Read Me 1Document10 pagesRead Me 1pmk888No ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- EulaDocument63 pagesEulatechkasambaNo ratings yet
- List FileDocument73 pagesList FileGeorge Herland PradiktaNo ratings yet
- Accidental Radioactive ContaminationDocument1 pageAccidental Radioactive ContaminationGeorge Herland PradiktaNo ratings yet
- List FileDocument73 pagesList FileGeorge Herland PradiktaNo ratings yet
- Jurnal VertebraDocument10 pagesJurnal VertebraGeorge Herland PradiktaNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Syllabus ECDO 4225 - Professional Aspects of Nutrition and DieteticsDocument6 pagesSyllabus ECDO 4225 - Professional Aspects of Nutrition and DieteticsOEAENo ratings yet
- Acute Tracheobronchitis Causes, Symptoms, TreatmentDocument2 pagesAcute Tracheobronchitis Causes, Symptoms, TreatmentNicole Shannon CariñoNo ratings yet
- JUSTINE Medical-for-Athletes-2-1Document2 pagesJUSTINE Medical-for-Athletes-2-1joselito papa100% (1)
- As 2550.5-2002 Cranes Hoists and Winches - Safe Use Mobile CranesDocument8 pagesAs 2550.5-2002 Cranes Hoists and Winches - Safe Use Mobile CranesSAI Global - APACNo ratings yet
- Admission For 1st Year MBBS Students For The Academic Year 2014-2015Document10 pagesAdmission For 1st Year MBBS Students For The Academic Year 2014-2015Guma KipaNo ratings yet
- Appendix - 6 - Site Logistics PlanDocument16 pagesAppendix - 6 - Site Logistics PlanRamesh BabuNo ratings yet
- Anarchy RPG 0.2 Cover 1 PDFDocument14 pagesAnarchy RPG 0.2 Cover 1 PDFanon_865633295No ratings yet
- Weeblylp MedicinaDocument18 pagesWeeblylp Medicinaapi-538325537No ratings yet
- The Process of Grief PDFDocument6 pagesThe Process of Grief PDFnicoletagr2744100% (1)
- Handbook of Laboratory Animal Science - Vol IIIDocument319 pagesHandbook of Laboratory Animal Science - Vol IIICarlos AlmeidaNo ratings yet
- Chapter 22 The First Heart SoundDocument5 pagesChapter 22 The First Heart SoundAbhilash ReddyNo ratings yet
- Facts of MaintenanceDocument9 pagesFacts of Maintenancegeorge youssefNo ratings yet
- OCPD: Symptoms, Diagnosis and TreatmentDocument4 pagesOCPD: Symptoms, Diagnosis and TreatmentRana Muhammad Ahmad Khan ManjNo ratings yet
- Introduction 1 Esoteric HealingDocument20 pagesIntroduction 1 Esoteric HealingChicowski Caires100% (1)
- Swan-Ganz Catheter Insertion GuideDocument3 pagesSwan-Ganz Catheter Insertion GuideJoshNo ratings yet
- LabTec Product SpecificationsDocument292 pagesLabTec Product SpecificationsDiego TobrNo ratings yet
- Nursing Interventions for Ineffective Airway ClearanceDocument3 pagesNursing Interventions for Ineffective Airway Clearanceaurezea100% (3)
- EN Sample Paper 12 UnsolvedDocument9 pagesEN Sample Paper 12 Unsolvedguptasubhanjali21No ratings yet
- Injeksi Mecobalamin Vas ScoreDocument5 pagesInjeksi Mecobalamin Vas ScoreHerdy ArshavinNo ratings yet
- College Women's Experiences With Physically Forced, Alcohol - or Other Drug-Enabled, and Drug-Facilitated Sexual Assault Before and Since Entering CollegeDocument12 pagesCollege Women's Experiences With Physically Forced, Alcohol - or Other Drug-Enabled, and Drug-Facilitated Sexual Assault Before and Since Entering CollegeGlennKesslerWP100% (1)
- (260821) PPT Analsis Evaluasi Penggunaan Obat Di FKTPDocument43 pages(260821) PPT Analsis Evaluasi Penggunaan Obat Di FKTPreginaNo ratings yet
- Detailed Advertisement of Various GR B & C 2023 - 0 PDFDocument47 pagesDetailed Advertisement of Various GR B & C 2023 - 0 PDFMukul KostaNo ratings yet
- Occlusion For Implant Suppported CDDocument4 pagesOcclusion For Implant Suppported CDpopat78No ratings yet
- Cough and ColdsDocument3 pagesCough and ColdsKarl-Ren Lacanilao100% (1)
- Labcorp: Patient ReportDocument4 pagesLabcorp: Patient ReportAsad PrinceNo ratings yet
- Leaving Disasters Behind: A Guide To Disaster Risk Reduction in EthiopiaDocument12 pagesLeaving Disasters Behind: A Guide To Disaster Risk Reduction in EthiopiaOxfamNo ratings yet
- Dr. Abazar Habibinia's Guide to Overweight, Obesity, and Weight ManagementDocument41 pagesDr. Abazar Habibinia's Guide to Overweight, Obesity, and Weight ManagementTasniiem KhmbataNo ratings yet
- 798 3072 1 PBDocument12 pages798 3072 1 PBMariana RitaNo ratings yet
- Environmental Hazards For The Nurse As A Worker - Nursing Health, & Environment - NCBI Bookshelf PDFDocument6 pagesEnvironmental Hazards For The Nurse As A Worker - Nursing Health, & Environment - NCBI Bookshelf PDFAgung Wicaksana100% (1)
- Updates On Upper Eyelid Blepharoplasty.4Document8 pagesUpdates On Upper Eyelid Blepharoplasty.4Dimitris RodriguezNo ratings yet