Professional Documents
Culture Documents
Acupuncture Application For Neurological Disorders PDF
Uploaded by
gonfinhoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acupuncture Application For Neurological Disorders PDF
Uploaded by
gonfinhoCopyright:
Available Formats
P
u
b
l
i
s
h
e
d
b
y
M
a
n
e
y
P
u
b
l
i
s
h
i
n
g
(
c
)
W
.
S
.
M
a
n
e
y
&
S
o
n
L
i
m
i
t
e
d
Acupuncture application for neurological
disorders
Hyangsook Lee*
{
, Hi-Joon Park*
1{
, Jongbae Park*
"
, Mi-Ja Kim
1
,
MeeSuk Hong
1
, JongSoo Yang
&
, SunMi Choi
#
and Hyejung Lee*
1{
*Acupuncture and Meridian Science Research Center,
{
Department of Meridian and Acupuncture, College
of Korean Medicine, and
1
TKM Research Group, Kyung Hee University, Seoul 130-701, Korea
{
Department of Meridian and Acupoint, College of Korean Medicine, Sang Ji University, Wonju 220-702,
Korea
"
Division for Research and Education in Complementary and Integrative Medical Therapies, Harvard
Medical School, Osher Institute, Landmark Center, 401 Park Drive, Suite 22A-West, Boston, MA 02215,
USA
#
Department of Medical Research, Korea Institute of Oriental Medicine, Daejeon 305-811, Korea
&
Department of Small and Medium Business Innovation Center, ITEP, Seoul 135-080, Korea
Background: Acupuncture has been widely used for a range of neurological disorders. Despite its
popularity, the evidence to support the use of acupuncture is contradictory.
Methods: This review was designed to summarize and to evaluate the available evidence of
acupuncture for neurological disorders.
Results: Most of the reviewed studies suffer from lack of methodological rigor. Owing to paucity
and poor quality of the primary studies, no firm conclusion could be drawn on the use of
acupuncture for epilepsy, Alzheimers disease, Parkinsons disease, ataxic disorders, multiple
sclerosis, amyotrophic lateral sclerosis and spinal cord injury. For stroke rehabilitation, the
evidence from recent high-quality trials and previous systematic reviews is not convincing.
Conclusion: More rigorous trials are warranted to establish acupunctures role in neurological
disorders. [Neurol Res 2007; 29: S49S54]
Keywords: Acupuncture; electroacupuncture; randomized clinical trial; neurological disorders
INTRODUCTION
Acupuncture has long been widely practised in China,
Japan, Korea and other Asian countries. Although
acupuncture has been used for years within immigrant
communities in the West, it was not least due to
television reporting in the 1970s of patients undergoing
surgery without conventional analgesia that acupunc-
ture received much attention and generated intensive
research. Over the past two decades, acupuncture has
enjoyed its growing popularity in the United States and
Europe, and a recent survey demonstrated that
Americans pay more than ve million visits a year to
acupuncture practitioners
1
.
Acupuncture involves inserting ne needles into
specic locations in the body called acupuncture
points. The needles are usually manipulated to elicit a
characteristic needle sensation (Deqi) which is believed
to be essential to obtain better therapeutic effects. In
addition to manual needling, a variety of methods are
used to stimulate acupuncture points, e.g. electricity,
laser, ultrasound and moxibustion (burning the powder
of dried leaves of Artemisia vulgaris or mugwort).
Despite the historical usage and present popularity of
acupuncture, the current evidence supporting its use is
largely inconclusive. Systematic reviews have shown
that acupuncture is more effective than placebo for
chemotherapy-induced nausea and vomiting
2
, early
post-operative nausea in adults
3
and for acute dental
pain
4
. Evidence is inconclusive for a range of condi-
tions: low back pain
5,6
, neck pain
7
, headache
8
,
bromyalgia
9
, osteoarthritis
10,11
, stroke
12
, labor pain
13
,
tinnitus
14
and asthma
15
. For smoking cessation
16
and
weight loss
17
, present evidence suggests that acupunc-
ture is no better than placebo.
For neurological disorders, there have not been many
high-quality studies of acupuncture from which rm
conclusions can be drawn. In this review, we aimed at
summarizing the current evidence available for/against
acupuncture for neurological disorders and suggesting
research strategies for further investigation in this eld.
SCIENTIFIC EVIDENCE OF ACUPUNCTURE
It has not been fully explained how acupuncture works
within the framework of Western Medicine. Since gate-
control theory by Wall and Melzack in 1965
18
, basic
scientic research has focused on acupunctures mode
of action from a neurobiologic perspective. One of the
most intensely researched areas is the involvement of
endogenous opioid peptides in acupuncture-induced
Correspondence and reprint requests to: Hyejung Lee, KMD, PhD,
Department of Meridian and Acupuncture, College of Korean
Medicine, Kyung Hee University, 1 Hoegi-dong, Dongdaemoon-gu,
Seoul 130-701, Korea. [hjlee@khu.ac.kr]
#
2007 W. S. Maney & Son Ltd Neurological Research, 2007, Volume 29, Supplement 1 S49
10.1179/016164107X172211
P
u
b
l
i
s
h
e
d
b
y
M
a
n
e
y
P
u
b
l
i
s
h
i
n
g
(
c
)
W
.
S
.
M
a
n
e
y
&
S
o
n
L
i
m
i
t
e
d
analgesia. Researches have revealed that endogenous
opioids in the central nervous system (CNS) play an
essential role in mediating the analgesic effect of
electroacupuncture. Further studies have shown that
different kinds of neuropeptides are released by
electroacupuncture with different frequencies: 2 Hz
electroacupuncture selectively induces the release of
enkephalin, b-endorphin and endomorphin, while
100 Hz electroacupuncture increases the release of
dynorphin
19
. More recent study demonstrated that
alternative 2 and 100 Hz (2/100) electroacupuncture
increased the release of both dynorphin and endomor-
phin, whilst 2 z 100 Hz electroacupuncture increased
only the release of dynorphin, not endomorphin. The
results suggest that a proper combination of different
frequencies of electroacupuncture may produce a maxi-
mal release of various opioids possibly for better
therapeutic effects
20
. This nding from laboratory
animals was studied in post-operative patients and the
data revealed that the alternative mode stimulation (2/
100 Hz) reduced the morphine requirement by 53%,
while a constant 2 or 100 Hz produced only 32 or 35%
decrease, respectively
21
.
Functional magnetic resonance imaging technique
has also been used to investigate the neural mechanism
of acupuncture in healthy volunteers: correlations
between acupuncture stimulation on the vision-related
acupuncture point (BL67) and activation of the visual
cortex were investigated
22
and acupuncture stimulation
on LI4 point might modulate the activity of limbic
system and subcortical structures
23
.
CLINICAL EVIDENCE OF ACUPUNCTURE FOR CNS
DISEASES
The basic idea of acupuncture treatment is that disorders
result from inadequate ow of Qi through the meridian
and can be prevented or corrected by stimulating the
relevant acupuncture points. While time has witnessed
benecial effects of acupuncture, systematic reviews
from rigorous randomized clinical trials (RCTs) do not
seem to make rm conclusions whether acupuncture is
effective or not for neurological disorders.
Seizure and epilepsy
Endogenous opioids, serotonin and c-butyric acid
have been implicated in the mechanism of acupuncture
in suppressing epileptic seizures in animal models
24
.
Kloster et al.
25
compared 8 week acupuncture treatment
with sham acupuncture in 29 patients with chronic
intractable epilepsy. Fifteen patients in the acupuncture
group received real acupuncture consisting of manual
acupuncture and electroacupuncture three times a week
for 8 weeks with a week rest in the middle. For the
control group (n514), acupuncture on non-acupuncture
points without electric stimulation was given. No inter-
group difference was reported in seizure frequency, and
the number of seizure-free weeks increased signicantly
in the control group, not in the acupuncture group
(p50.006). The same team reported no benecial effect
of acupuncture in health-related quality of life from the
same trial
26
(Table 1).
Cerebrovascular disorders
In 1997, the National Institute of Health Consensus
Development Panel on Acupuncture suggested that
acupuncture might be a useful adjunct for stroke
rehabilitation
27
. However, high-quality RCTs and sys-
tematic reviews on the effectiveness of acupuncture for
stroke rehabilitation do not support this claim
12,28,29
. A
recently published meta-analysis also reports no addi-
tional effect of acupuncture on motor recovery when
given with rehabilitation therapy
30
.
Several high-quality RCTs have been published since
Park et al.
12
systematically reviewed the literature
Table 1: Characteristics and results of randomized clinical trials of acupuncture for seizure and epilepsy
Author (year) Study design and quality*
Sample size
(acupuncture) Intervention Outcome measures Results
Kloster (1999)
25
Sham-controlled
(1 z 1 z 1 z 1 z 155)
29 (15) AP: MA z EA three times/week
for 7 weeks with 1 week rest in
the middle; LR3, LI4, GV20 z 1
2 individualized points; 3 Hz,
320 mA
Seizure frequency
8 weeks post-AP
Seizure-free weeks
during treatment
and follow-up
NS
significant benefit
for CON group
(p50.006)
CON: sham AP; non-AP points;
minimal manipulation and no
electrical stimulation
Stavem (2000)
26
Sham-controlled
(1 z 1 z 1 z 0 z 154)
34 (18) AP: MA z EA three times/week
for 7 weeks with 1 week rest in
the middle; LR3, LI4, GV20 z 1
2 individualized points; 3 Hz,
320 mA
QOLIE-89 scores
8 weeks post-AP
NS
CON: sham AP; non-AP points;
minimal manipulation and no
electrical stimulation
*Study quality was assessed using the modified Jadad score
7,53
; randomization 1 point z appropriate randomization method 1 point (z
inappropriate randomization method 21 point) z patient-blinding 1 point z evaluator-blinding 1 point z describing withdrawals and dropouts 1
point5maximum 5 points. AP, acupuncture; EA, electroacupuncture; MA, manual acupuncture; NS, not significantly different between groups;
QOLIE-89, 89-item quality of life in epilepsy questionnaire.
Acupuncture and neurological disorders: H. Lee et al.
S50 Neurological Research, 2007, Volume 29, Supplement 1
P
u
b
l
i
s
h
e
d
b
y
M
a
n
e
y
P
u
b
l
i
s
h
i
n
g
(
c
)
W
.
S
.
M
a
n
e
y
&
S
o
n
L
i
m
i
t
e
d
(Table 2). Johansson et al.
31
conducted a multi-center,
evaluator-blinded RCT involving 150 patients within 5
10 days of stroke onset. Only patients with moderate or
severe functional impairment at randomization were
included: Barthel index (70 points in combination
with inability to walk 10 m without mechanical or
personal support. Patients were allocated by stratied
randomization to receive (1) a combination of manual
acupuncture and low-frequency electroacupuncture
(n548), (2) high-intensity, low-frequency, transcuta-
neous electric nerve stimulation (TENS) (n551); (3)
low-intensity, high-frequency TENS (control group,
n551). Twice-a-week treatment for 10 weeks was given
and if necessary, patients received conventional phy-
siotherapy, occupational therapy and speech therapy
irrespective of group allocation. Walking (time needed
to walk 10 m), motor function (Rivermead mobility
index), activities of daily living (Barthel index) and
quality of life (Nottingham health prole) were mea-
sured at randomization, three months and 12 months
follow-ups after the onset of stroke. The results
demonstrated no signicant differences between groups
in any of outcome measures, and authors concluded
that acupuncture combined with electroacupuncture or
TENS-induced muscle contraction could not be recom-
mended as a standard treatment for patients with
moderate or severe stroke in the subacute stage.
In another evaluator-blinded RCT with 106 stroke
patients within 315 days of the onset of stroke,
additional manual acupuncture to standard treatment
was compared with standard treatment only
32
. Patients
were stratied into Group I (admission Barthel
index,11) and Group II (admission Barthel index>11)
to avoid chance imbalance of severity of disability
between the acupuncture arm and the control arm, and
also because the severe group required longer inpatient
rehabilitation than the moderate group: Group I patients
received 5 weeks (1 week) of inpatient rehabilitation,
followed by 5 weeks (1 week) of day hospital
rehabilitation, while Group II patients received
three weeks (1 week) of inpatient rehabilitation,
followed by 7 weeks (1 week) of day hospital
rehabilitation. Patients in Groups I and II were then
separately randomized to either acupuncture group or
control group (n553). Acupuncture treatment was
carried out 5 times per week for inpatients, three times
per week to the end of the eighth week, and then twice
per week for the remaining two weeks for day hospital
patients. Therefore, the total intervention lasted for
10 weeks. The primary end points were the Fugl-Meyer
assessment of physical performance-motor subsection
(FMAM) median score at week 10 and FMAM median
score change over time. Median scores of Barthel index
and functional independence measure were also
assessed. Acupuncture intervention failed to show
signicant benet in any of the outcome measures at
week 10 or outcome changes over time.
A most recent, placebo-controlled trial
28
tested the
effect of 4 week manual acupuncture treatment for
reduction of leg spasticity in chronic post-stroke patients
(mean time from ischemic stroke: 65.4 48.3 months).
Participants were randomized to receive either 8
sessions of manual acupuncture (n513) or placebo
acupuncture where sham acupuncture needles were
used (n512). Modied Ashworth scale score was
measured as the primary end point. There was no
signicant difference between acupuncture group and
placebo acupuncture group.
The message from the current evidence is clear. There
is a paucity of RCTs and the most recent high-quality
studies
28,30,31
conrm the nding of the systematic
review by Park et al.
12
that methodologically weaker
studies were likely to generate positive outcomes. As
with acupuncture studies in other areas, most studies on
acupuncture for stroke rehabilitation suffer from meth-
odological aws. Control groups are heterogeneous and
few studies adopt placebo control to investigate possible
specic effects of acupuncture. As practitioner-blinding
is virtually impossible in acupuncture trials, at least
evaluator of outcome measures should be blinded to
minimize measurement bias. However, most studies
were found to fail to blind outcome assessor
31,33,37
.
Acupuncture interventions vary across studies in terms
of stimulation method, choice of acupuncture points,
number of treatment sessions and treatment period.
Heterogeneous inclusion criteria across trials and small
sample sizes also preclude estimation of acupuncture
effect for any subgroup of stroke patients. Rigorous
research is warranted to establish acupunctures role in
stroke rehabilitation.
Alzheimers disease
There are only a few uncontrolled studies of
acupuncture for Alzheimers disease. In a pilot study
involving 11 patients, 10 with Alzheimers disease and
one with vascular dementia, twice-a-week acupuncture
treatment for three months was tested whether it had
any effects on depression and anxiety
38
. The researchers
found signicant improvements in the depression and
anxiety scores measured by the Cornell scale for
depression and the Speilberger state anxiety inventory.
Cognitive functioning (mini-mental status examination,
MMSE) remained stable over months of the study.
Another pilot study where eight patients with mild to
moderate Alzheimers disease were given acupuncture
treatment for a month reported that patients signicantly
improved on measures of verbal orientation and motor
coordination, and had higher overall MMSE scores
39
.
The ndings call for rigorous clinical trials in this area.
Parkinsons disease
Several uncontrolled pilot studies were conducted on
the patients with Parkinsons disease. In the study by Ha
et al.
40
, 7 patients with antiparkinsonian drugs and 12
patients without antiparkinsonian drugs, completed
twice-a-week acupuncture treatments for eight weeks.
In the former group, total scores of unied Parkinsons
disease rating scale (UPDRS), UPDRS II for daily activity
and UPDRS IV for side effects improved compared to the
baseline. In the latter group, total scores for UPDRS and
UPDRS III for motor function improved signicantly.
Acupuncture and neurological disorders: H. Lee et al.
Neurological Research, 2007, Volume 29, Supplement 1 S51
P
u
b
l
i
s
h
e
d
b
y
M
a
n
e
y
P
u
b
l
i
s
h
i
n
g
(
c
)
W
.
S
.
M
a
n
e
y
&
S
o
n
L
i
m
i
t
e
d
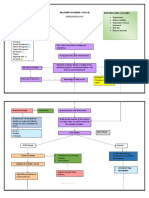
Table 2: Characteristics and results of randomized clinical trials of acupuncture for stroke
Author (year) Study design and quality*
Sample size
(acupuncture)
Days after
onset Intervention
Outcome
measures
Results compared
with control
Zou (1990)
37
Open
(1 z 0 z 0 z 0 z 051)
63 (32) .7 AP: MA everyday
for 6 weeks
CSRM Significant benefit
(p,0.001)
CON: standard
medication
Naeser (1992)
35
Patient-blinded
(1 z 0 z 1 z 0 z 052)
16 (10) 3090 AP: EA, 12 Hz,
five times/week for
4 weeks
ROM NS
CON: sham AP; no
electrical stimulation;
non-paralyzed arms
and leg
Johansson (1993)
31
and Magnusson
(1994)
54
Open
(1 z 0 z 0 z 0 z 152)
78 (38) ,10 AP: EA, 25 Hz, twice/
week for 10 weeks
Walking, Motor
function, balance
and Barthel ADL
Significant benefit
(p,0.05) except
motor function
Significant benefit
for energy, mobility,
emotion and
social isolation
(p,0.05)
CON: rehabilitation NHP
Days spent at
hospital/nursing
home
Significant benefit
(p,0.05)
Hu (1993)
34
Open
(1 z 0 z 0 z 0 z 152)
30 (15) ,1.5 AP: EA, 9.4 Hz, three
times/week for 4 weeks
CON: Rehabilitation
SSS
Barthel ADL
Significant benefit
(p50.02)
NS
Sallstro m (1996)
55
and Kjendahl
(1997)
56
Evaluator-blinded
(1 2 1 z 0 z 1 z 152)
49 (24) ,median
40
AP: MAzEA or Moxa
everyday for 6 weeks,
24 Hz
CON: rehabilitation
Motor function
Sunnaas ADL
NHP
Significant benefit
(p50.002)
NS
Significant benefit
(p50.009)
Zhang (1996)
36
Open
(1 z 0 z 0 z 0 z 051)
64 (31) ,8 AP: EA, 2 Hz, 67 times/
week for 2 weeks
CSRM NS
CON: rehabilitation
Gosman-Hedstro m
(1998)
29
Patient-blinded, Evaluator-
blinded (1 z 1 z 1 z 1 z
155)
104 (37, 34) ,7
AP: deep EAzMA, 2 Hz,
twice/week for 10 weeks
AP2: superficial AP, no
manipulation and no
electrical stimulation
CON: Rehabilitation
SSS, Barthel ADL
and Sunnaas ADL
NHP
NS
Significant benefit
for CON2 (p,0.05)
Si (1998)
57
Evaluator-blinded
(1 z 0 z 0 z 1 z 052) 42 (20) ,7
AP: EA, 5/45 Hz, five
times/week for 37 weeks CSS
Significant benefit
(p,0.01)
CON: standard medication
Duan (1998)
33
Open
(1 z 0 z 0 z 0 z 051)
92 (47) Acute AP: MA everyday for
4 weeks
CSRM Significant benefit
(p,0.001)
CON: standard medication
Johansson (2001)
58
Evaluator-blinded
(1 z 1 z 0 z 1 z 154)
150 (48) 510 AP: MAzEA, 2 Hz,
twice/week for 10 weeks
CON1: TENS, high-
intensity and low-
frequency
CON2: subliminal TENS,
low-intensity and
high-frequency
Barthel ADL,
motor function,
walking and NHP
NS
Sze (2002)
32
Evaluator-blinded
(1 z 1 z 0 z 1 z 154)
106 (53) 315 AP: MA, 25 times/week
for 10 weeks
FMAM, Barthel
ADL and FIM
NS
CON: standard treatment
Fink (2004)
28
Patient-blinded, Evaluator-
blinded (1 z 0 z 1 z 1 z
154)
25 (13) 5 years AP: MA twice /week for
4 weeks
CON: sham AP
MAS NS
*Study quality was assessed using the modified Jadad score
7,53
; randomization 1 point z appropriate randomisation method 1 point (z inappropriate
randomization method 1 point) z patient-blinding 1 point z evaluator-blinding 1 point z describing withdrawals and dropouts 1 point5maximum 5
points. ADL, activities of daily living; AP, acupuncture; CSRM, Chinese stroke recovery measure; CSS, Chinese stroke scale; EA, electroacupuncture; FIM,
functional independence measure; FMAM, Fugl-Meyer assessment of physical performance-motor subsection; MA, manual acupuncture; MAS, modified
Ashworth scale; NHP, Nottinghamhealth profile; NS, not significantly different between groups; ROM, range of movement; SSS, Scandinavian stroke scale.
Acupuncture and neurological disorders: H. Lee et al.
S52 Neurological Research, 2007, Volume 29, Supplement 1
P
u
b
l
i
s
h
e
d
b
y
M
a
n
e
y
P
u
b
l
i
s
h
i
n
g
(
c
)
W
.
S
.
M
a
n
e
y
&
S
o
n
L
i
m
i
t
e
d
Shulman et al.
41
conducted a pilot study in 20
patients with Parkinsons disease. All patients were
given two acupuncture treatment sessions per week for
58 weeks and evaluated before and after acupuncture
treatment with a range of Parkinsons disease and
behavioral scales. Although 85% of patients reported
subjective improvement of symptoms such as tremor,
walking, handwriting, slowness, pain, sleep, depression
and anxiety, the data showed no signicant benet from
acupuncture treatment except improvement in the sleep
and rest categories in sickness impact prole. As
acupuncture was reported to be one of the most
frequently used complementary and alternative medi-
cine modalities
42
, further rigorous research is required
for this indication.
Other diseases of the CNS
There are few RCTs of acupuncture for other impor-
tant disorders of the CNS such as ataxic disorders
43
,
multiple sclerosis
44,45
, amyotrophic lateral sclerosis
46
and traumatic injuries of the spinal cord
47
. The effect of
acupuncture for these indications is largely dependent
upon anecdotal evidence. Considering the prevalence
of acupuncture use
46,48
, well-designed high-quality
RCTs in these populations are needed.
FUTURE DIRECTIONS
Owing to the dearth of high-quality studies, a rm
conclusion on the effectiveness of acupuncture for
neurological disorders cannot be drawn. A careful
analysis of the negative results, however, is required to
dispute acupunctures effect on neurological disorders
as most previous studies have been unable to fully
evaluate therapeutic modality of acupuncture. Based on
the summarized evidence, a few suggestions for future
clinical trials of acupuncture in this eld can be made.
Patient population
The patient populations in the previous studies are
heterogeneous. The effect of acupuncture can be
different in a certain patient group
3
. Future research
should clearly dene patient inclusion criteria to
investigate whether acupuncture works for a certain
subgroup of patients under the same condition.
Control procedures
A variety of control procedures have been used in
acupuncture research from waiting list to sham needle
device
49
. First, comparison should be made between
standard treatment and acupuncture as an adjunct. If an
add-on acupuncture treatment is found to be of any
help, specic effect of acupuncture should be sought in
a placebo-controlled trial. For the ideal placebo-
controlled study of acupuncture, placebo should mimic
acupuncture treatment without physiologic effect.
Recently developed sham needle devices are expected
to play an important role in placebo-controlled
study
50,51
.
Acupuncture technique
Efforts should be made regarding the acupuncture
technique in terms of stimulation method, selection of
acupuncture points, duration of treatment and appro-
priate number of sessions. Acupuncturists prociency
and clinical experience are also important. Rationale
for the acupuncture intervention should be reported
clearly.
Outcome measures
Well-validated, clinically relevant scales should be
used and adequate follow-up is necessary. Reports
should pre-dene the primary and secondary end points
to avoid data dredging.
Methodological rigor
Low-quality trials are more likely to overestimate
efcacy
52
. Previous acupuncture trials have been open
to criticism due to poor quality. Sample size calculation,
description of adequate randomization method, alloca-
tion concealment, appropriate blinding of patient and/or
outcome assessor, intention-to-treat analysis and ade-
quate statistical analysis should be provided in the
report.
CONCLUSION
The current evidence is not conclusive to support the
use of acupuncture for a range of neurological disorders.
The paucity and poor quality of the existing studies
preclude from drawing a rm conclusion whether
acupuncture has any benecial effect on neurological
disorders and stroke rehabilitation. More rigorous
studies are needed to dene acupunctures role in this
area.
ACKNOWLEDGEMENT
This study was supported by the SRC program of KOSEF (R11-2005-014),
Korea.
REFERENCES
1 Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative
medicine use in the United States, 19901997: Results of a follow-
up national survey. JAMA 1998; 280: 15691575
2 Vickers AJ. Can acupuncture have specific effects on health? a
systematic review of acupuncture antiemesis trials. J R Soc Med
1996; 89: 303311
3 Lee A, Done ML. The use of nonpharmacologic techniques to
prevent postoperative nausea and vomiting: A meta-analysis.
Anesth Analg 1999; 88: 13621369
4 Ernst E, Pittler MH. The effectiveness of acupuncture in treating
acute dental pain: A systematic review. Br Dent J 1998; 184: 443
447
5 Ernst E, White AR. Acupuncture for back pain: A meta-analysis of
randomized controlled trials. Arch Intern Med 1998; 158: 2235
2341
6 van Tulder M, Cherkin DC, Berman B, et al. The effectiveness of
acupuncture in the management of acute and chronic low back
pain. A systematic review within the framework of the Cochrane
Collaboration Back Review Group. Spine 1999; 24: 11131123
7 White AR, Ernst E. A systematic review of randomized controlled
trials of acupuncture for neck pain. Rheumatology 1999; 38: 143
147
Acupuncture and neurological disorders: H. Lee et al.
Neurological Research, 2007, Volume 29, Supplement 1 S53
P
u
b
l
i
s
h
e
d
b
y
M
a
n
e
y
P
u
b
l
i
s
h
i
n
g
(
c
)
W
.
S
.
M
a
n
e
y
&
S
o
n
L
i
m
i
t
e
d
8 Melchart D, Linde K, Fischer P, et al. Acupuncture for recurrent
headaches: A systematic review of randomized controlled trials.
Cephalalgia 1999; 19: 779786
9 Berman BM, Ezzo J, Hadhazy V, et al. Is acupuncture effective in
the treatment of fibromyalgia? J Fam Pract 1999; 48: 213218
10 Ernst E. Acupuncture as a symptomatic treatment of osteoarthritis.
Scand J Rheumatol 1997; 26: 444447
11 Ezzo J, Hadhazy V, Birch S, et al. Acupuncture for osteoarthritis of
the knee: A systematic review. Arthritis Rheum 2001; 44: 819825
12 Park J, Hopwood V, White AR, et al. Effectiveness of acupuncture
for stroke: A systematic review. J Neurol 2001; 248: 558563
13 Lee H, Ernst E. Acupuncture for labor pain management: A
systematic review. Am J Obstet Gynecol 2004; 191: 15731579
14 Park J, White AR, Ernst E. Efficacy of acupuncture as a treatment for
tinnitus: A systematic review. Arch Otolaryngol Head Neck Surg
2000; 126: 489492
15 McCarney R, Brinkhaus B, Lasserson T, et al. Acupuncture for
chronic asthma. Cochrane Database Syst Rev 2004; 1: CD000008
16 White AR, Resch KL, Ernst E. A meta-analysis of acupuncture
technique for smoking cessation. Tob Control 1999; 8: 393397
17 Ernst E. Acupuncture/acupressure for weight reduction? A
systematic review. Wien Klin Wochenschr 1997; 109: 6062
18 Melzack R, Wall PD. Pain mechanism: A new theory. Science
1965; 150: 971979
19 Han JS. Acupuncture and endorphins. Neurosci Lett 2004; 361:
258261
20 Wang Y, Zhang Y, Wang W, et al. New evidence for synergistic
analgesia produced by endomorphin and dynorphin. Chin J Pain
Med 2002; 8: 118119
21 Hamza MA, White PF, Ahmed HE, et al. Effect of the frequency of
transcutaneous electrical nerve stimulation on the postoperative
opioid analgesic requirement and recovery profile. Anesthesiology
1999; 91: 12321238
22 Cho ZH, Chung SC, Jones JP, et al. New findings of the correlation
between acupoints and corresponding brain cortices using
functional MRI. Proc Natl Acad Sci USA 1998; 95: 26702673
23 Hui KK, Liu J, Makris N, et al. Acupuncture modulates the limbic
system and subcortical gray structures of the human brain:
Evidence from fMRI studies in normal subjects. Hum Brain Mapp
2000; 9: 1325
24 Wu D. Mechanism of acupuncture in suppressing epileptic
seizures. J Trad Chin Med 1992; 12: 187192
25 Kloster R, Larsson PG, Lossius R, et al. The effect of acupuncture in
chronic intractable epilepsy. Seizure 1999; 8: 170174
26 Stavem K, Kloster R, Rossberg E, et al. Acupuncture in intractable
epilepsy: Lack of effect on health-related quality of life. Seizure
2000; 9: 422426
27 NIH Consensus Development Panel. Acupuncture. JAMA 1998;
280: 15181524
28 Fink M, Rollnik JD, Bijak M, et al. Needle acupuncture in chronic
poststroke leg spasticity. Arch Phys Med Rehabil 2004; 85: 667
672
29 Gosman-Hedstro m G, Claesson L, Klingenstierna U, et al. Effects
of acupuncture treatment on daily life activities and quality of life:
A controlled, prospective, and randomized study of acute stroke
patients. Stroke 1998; 29: 21002108
30 Sze FK, Wong E, Or KK, et al. Does acupuncture improve motor
recovery after stroke? A meta-analysis of randomized controlled
trials. Stroke 2002; 33: 26042619
31 Johansson K, Lindgren I, Widner H, et al. Can sensory stimulation
improve the functional outcome in stroke patients? Neurology
1993; 43: 21892192
32 Sze FK, Wong E, Yi X, et al. Does acupuncture have additional
value to standard poststroke motor rehabilitation? Stroke 2002; 33:
186194
33 Duan G, He J, Zeng Z, et al. Comparison of effects of acupuncture
on cerebral infarction in different parts. World J Acup-Mox 1998;
8: 37
34 Hu HH, Chung C, Liu TJ, et al. A randomized controlled trial on
the treatment for acute partial ischemic stroke with acupuncture.
Neuroepidemiology 1993; 12: 106113
35 Naeser MA, Alexander MP, Stiassny-Eder D, et al. Real versus
sham acupuncture in the treatment of paralysis in acute stroke
patients: A CT scan lesion site study. J Neurol Rehab 1992; 6: 163
173
36 Zhang X, Yuan Y, Kuang P, et al. The changes of vasoactive
intestinal peptide somatostatin and pancreatic polypeptide in
blood and CSF of acute cerebral infarction patients and the effect
of acupuncture on them. Zhen Ci Yan Jiu 1996; 21: 1016
37 Zou X, Wang D. Comparative study of cerebral infarction treated
with acupuncture at 6 acupoints of yang meridian and calan.
Zhong Xi Yi Jie He Za Zhi 1990; 10: 199202
38 Lombardo NE, Vehvilainen L, Ooi WL, et al. Acupuncture to
treat anxiety and depression in Alzheimers disease and
vascular dementia: A pilot feasibility and effectiveness trial.
Present at World Alzheimers Conference, 2000, Washington,
DC, USA
39 Kao H. Acupuncture enhancement in clinical symptoms and
cognitive-motor abilities of the Alzheimers disease patients.
Present at World Alzheimers Conference, 2000, Washington,
DC, USA
40 Ha J, Lee S, Yin C, et al. The effect of manual acupuncture therapy
on symptoms of the patients with idiopathic Parkinsons disease.
J Korean Oriental Med 2003; 24: 172183
41 Shulman LM, Wen X, Weiner WJ, et al. Acupuncture therapy for
the symptoms of Parkinsons disease. Mov Disord 2002; 17: 799
802
42 Rajendran PR, Thompson RE, Reich SG. The use of alternative
therapies by patients with Parkinsons disease. Neurology 2001;
57: 790794
43 Luo JH, Guo JM. 30 cases of cerebellar ataxia treated by skin
acupuncture. Shanghai J Acupunct Mox 1996; 15: 2526
44 Gibson RG, Gibson SLM. Neural therapy in the treatment of
multiple sclerosis. J Altern Complement Med 1999; 5: 543552
45 Miller RE. An investigation into the management of the spasticity
experienced by some patients with multiple sclerosis using
acupuncture based on traditional Chinese medicine.
Complement Ther Med 1996; 4: 5862
46 Wasner M, Klier H, Borasio GD. The use of alternative medicine
by patients with amyotrophic lateral sclerosis. J Neurol Sci 2001;
191: 151154
47 Wong AMK, Leong CP, Su TY, et al. Clinical trial of acupuncture
for patients with spinal cord injuries. Am J Phys Med Rehabil 2003;
82: 2127
48 Nayak S, Matheis RJ, Agostinelli S, et al. The use of complementary
and alternative therapies for chronic pain following spinal cord
injury: A pilot survey. J Spinal Cord Med 2001; 24: 5462
49 Vickers AJ. Placebo controls in randomized trials of acupuncture.
Eval Health Prof 2002; 25: 421435
50 Park J, White AR, Stevinson C, et al. Validating a new non-
penetrating sham acupuncture device: Two randomised controlled
trials. Acupunct Med 2002; 20: 168174
51 Streitberger K, Kleinhenz J. Introducing a placebo needle into
acupuncture research. Lancet 1998; 352: 364365
52 Smith LA, Oldman AD, McQuay HJ, et al. Teasing apart quality
and validity in systematic reviews: An example from acupuncture
trials in chronic neck and back pain. Pain 2000; 86: 119132
53 Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of
reports of randomized clinical trials: Is blinding necessary? Control
Clin Trials 1996; 17: 112
54 Magnusson M, Johansson K, Johansson BB. Sensory stimulation
promotes normalization of postural control after stroke. Stroke
1994; 25: 11761180
55 Sallstro m S, Kjendahl A, Sten PE, et al. Acupuncture in the
treatment of stroke patients in the subacute stage: A randomized,
controlled study. Complement Ther Med 1996; 4: 193197
56 Kjendahl A, Sallstro m S, sten PE, et al. A one year follow-up
study on the effects of acupuncture in the treatment of stroke
patients in the subacute stage: A randomized, controlled study.
Clin Rehabil 1997; 11: 192200
57 Si Q, Wi G, Cao X. Effects of electroacupuncture on acute cerebral
infarction. Acupunct Electrother Res 1998; 23: 117124
58 Johansson BB, Haker E, von Arbin M, et al. Acupuncture and
transcutaneous nerve stimulation in stroke rehabilitation: A
randomized, controlled trial. Stroke 2001; 32: 707713
Acupuncture and neurological disorders: H. Lee et al.
S54 Neurological Research, 2007, Volume 29, Supplement 1
You might also like
- Revolution SliderDocument1 pageRevolution SlidergonfinhoNo ratings yet
- Pain - Physiological PerspectiveDocument391 pagesPain - Physiological Perspectivemummy987100% (2)
- Learning Through Physical PlayDocument4 pagesLearning Through Physical PlaygonfinhoNo ratings yet
- Increase of Lower Esophageal Sphincter Pressure After Osteopathic Intervention On The Diaphragm in Patients With Gastroesophageal RefluxDocument6 pagesIncrease of Lower Esophageal Sphincter Pressure After Osteopathic Intervention On The Diaphragm in Patients With Gastroesophageal RefluxgonfinhoNo ratings yet
- Positional Release TherapyDocument269 pagesPositional Release Therapygonfinho95% (37)
- Trabalho Parto AcupunturaDocument14 pagesTrabalho Parto AcupunturagonfinhoNo ratings yet
- Involvement of Taurine in Penicillin-Induced Epilepsy and Anti-Convulsion of Acupuncture - A Preliminary Report PDFDocument15 pagesInvolvement of Taurine in Penicillin-Induced Epilepsy and Anti-Convulsion of Acupuncture - A Preliminary Report PDFgonfinhoNo ratings yet
- Osteopathy For ChildrenDocument2 pagesOsteopathy For ChildrengonfinhoNo ratings yet
- Revolution SliderDocument1 pageRevolution SlidergonfinhoNo ratings yet
- Effects of Acupuncture On Rates of Pregnancy and Live BirthDocument5 pagesEffects of Acupuncture On Rates of Pregnancy and Live BirthgonfinhoNo ratings yet
- 5 Seasons Formulário AntigoDocument144 pages5 Seasons Formulário AntigogonfinhoNo ratings yet
- Auriculotherapy Manual Chinese and Western Systems of Ear Acupuncture, Third EditionDocument322 pagesAuriculotherapy Manual Chinese and Western Systems of Ear Acupuncture, Third EditionFilip Nikoloski98% (41)
- Sleep Apneia and Acupuncture PDFDocument8 pagesSleep Apneia and Acupuncture PDFgonfinhoNo ratings yet
- Acupunctura e AmamentaçãoDocument76 pagesAcupunctura e AmamentaçãogonfinhoNo ratings yet
- Acupuncture in Polycystic Ovary Syndrome Current Experimental and Clinical EvidenceDocument9 pagesAcupuncture in Polycystic Ovary Syndrome Current Experimental and Clinical EvidencegonfinhoNo ratings yet
- Estudo Randomizado Sobre Acupuntura em IVFDocument8 pagesEstudo Randomizado Sobre Acupuntura em IVFgonfinhoNo ratings yet
- Acupuncture and Anaesthesia PDFDocument12 pagesAcupuncture and Anaesthesia PDFAriel Llamas GarciaNo ratings yet
- Combat-Related Posttraumatic Headache - Diagnosis, Mechanisms of Injury, and Challenges To TreatmentDocument10 pagesCombat-Related Posttraumatic Headache - Diagnosis, Mechanisms of Injury, and Challenges To TreatmentgonfinhoNo ratings yet
- Dor Miofascial Regional PDFDocument21 pagesDor Miofascial Regional PDFgonfinhoNo ratings yet
- Tension HeadacheDocument14 pagesTension HeadacheSamuel Idrogo AlfaroNo ratings yet
- Hewitt Handouts 2009 April 6 PerDocument16 pagesHewitt Handouts 2009 April 6 PergonfinhoNo ratings yet
- Short Right Leg 1Document4 pagesShort Right Leg 1Simo AsterNo ratings yet
- Dor Miofascial Regional PDFDocument21 pagesDor Miofascial Regional PDFgonfinhoNo ratings yet
- Cefaleia e Acupunctura PDFDocument5 pagesCefaleia e Acupunctura PDFgonfinhoNo ratings yet
- Acupuncture and Anaesthesia PDFDocument12 pagesAcupuncture and Anaesthesia PDFAriel Llamas GarciaNo ratings yet
- Cranial Osteopathic Manipulative Medicine's Growing Evidence BaseDocument1 pageCranial Osteopathic Manipulative Medicine's Growing Evidence BasegonfinhoNo ratings yet
- Combat-Related Posttraumatic Headache - Diagnosis, Mechanisms of Injury, and Challenges To TreatmentDocument10 pagesCombat-Related Posttraumatic Headache - Diagnosis, Mechanisms of Injury, and Challenges To TreatmentgonfinhoNo ratings yet
- Combat-Related Posttraumatic Headache - Diagnosis, Mechanisms of Injury, and Challenges To TreatmentDocument10 pagesCombat-Related Posttraumatic Headache - Diagnosis, Mechanisms of Injury, and Challenges To TreatmentgonfinhoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- NCP Ineffective Cerebral Tissue Perfusion STROKEDocument3 pagesNCP Ineffective Cerebral Tissue Perfusion STROKEMa. Elaine Carla TatingNo ratings yet
- High Intensity Exercise For Walking Competency in Individuals With Stroke - A Systematic Review and Meta-AnalysisDocument16 pagesHigh Intensity Exercise For Walking Competency in Individuals With Stroke - A Systematic Review and Meta-AnalysisSusana RodriguezNo ratings yet
- Fundamentals of Nursing Exam 16 (85 Items)Document13 pagesFundamentals of Nursing Exam 16 (85 Items)Mimi VeeNo ratings yet
- Carotid Artery Disease FlyerDocument2 pagesCarotid Artery Disease Flyerdinh son myNo ratings yet
- Npte Practice Paper No # 04Document47 pagesNpte Practice Paper No # 04Ismail JamilNo ratings yet
- Diffuse Optics: Fundamentals & Tissue ApplicationsDocument115 pagesDiffuse Optics: Fundamentals & Tissue ApplicationsGuy CohenNo ratings yet
- PY106Document8 pagesPY106thorarjun4No ratings yet
- Vascular Cognitive Impairment - Advances and TrendsDocument8 pagesVascular Cognitive Impairment - Advances and TrendsLaureanoNo ratings yet
- Navarro-Orozco & Sánchez-Manso, 2019) .: Gordin, Lee, Ducic, & Arnaoutakis, 2015) - Jha, Kochanek, & Simard, 2019)Document7 pagesNavarro-Orozco & Sánchez-Manso, 2019) .: Gordin, Lee, Ducic, & Arnaoutakis, 2015) - Jha, Kochanek, & Simard, 2019)anju dhakalNo ratings yet
- Cva CPDocument53 pagesCva CPApol Pen100% (2)
- Cerebrovascular Accident ReportDocument16 pagesCerebrovascular Accident ReportAngelu Gabrielle CastroNo ratings yet
- DynaMed Plus - Stroke (Acute Management)Document126 pagesDynaMed Plus - Stroke (Acute Management)Sarah Shafa MarwadhaniNo ratings yet
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaNo ratings yet
- Intracerebeller HemorrhageDocument9 pagesIntracerebeller HemorrhageWenny KalamiNo ratings yet
- Management of The Dental Patient With Neurological Disease - Overview, Epilepsy, StrokeDocument5 pagesManagement of The Dental Patient With Neurological Disease - Overview, Epilepsy, StrokearindraNo ratings yet
- Nursing Interventions for Unilateral Neglect PatientDocument6 pagesNursing Interventions for Unilateral Neglect PatientNicole Palarca92% (12)
- Sem 4 Lectura 2 Inhibidores de Recaptación de SerotoninaDocument18 pagesSem 4 Lectura 2 Inhibidores de Recaptación de SerotoninaJesús MoraNo ratings yet
- Neurorehabilitation 1: Stroke, TBI, MS, PD, GBS, and ALS ExaminationDocument439 pagesNeurorehabilitation 1: Stroke, TBI, MS, PD, GBS, and ALS ExaminationDuncan D'AmicoNo ratings yet
- Full Download Ebook PDF Prehospital Emergency Care 11th Edition PDFDocument41 pagesFull Download Ebook PDF Prehospital Emergency Care 11th Edition PDFrodney.pace130100% (25)
- Bayer plc Patient Information Leaflet for oral contraceptive YasminDocument12 pagesBayer plc Patient Information Leaflet for oral contraceptive YasminAditya Syah PutraNo ratings yet
- 40 - Advances in Motion and Electromyography Based Wearabletechnology For Upper Extremity Function Rehabilitation A ReviewDocument7 pages40 - Advances in Motion and Electromyography Based Wearabletechnology For Upper Extremity Function Rehabilitation A Reviewmihaela_986230018No ratings yet
- Are We Prepared To Detect Subtle and Nonconvulsive Status Epilepticus in Critically Ill Patients?Document7 pagesAre We Prepared To Detect Subtle and Nonconvulsive Status Epilepticus in Critically Ill Patients?succa07No ratings yet
- How Your Mind Can Heal Your BodyDocument16 pagesHow Your Mind Can Heal Your BodyAnusha PuttaNo ratings yet
- Physiotherapy Practice Guidelines For Stroke RehabilitationDocument50 pagesPhysiotherapy Practice Guidelines For Stroke Rehabilitation健康生活園Healthy Life Garden90% (10)
- StrokeDocument50 pagesStrokeABREHAM BUKULONo ratings yet
- CVA Case ReportDocument76 pagesCVA Case ReportpaulaNo ratings yet
- Transient Ischemic Attack Precipitating Factors Predisposing FactorsDocument6 pagesTransient Ischemic Attack Precipitating Factors Predisposing FactorsYosef OxinioNo ratings yet
- Acute Vestibular Syndrome: Kevin A. Kerber, MD, MSDocument8 pagesAcute Vestibular Syndrome: Kevin A. Kerber, MD, MSBagus Pithu Ha SpingNo ratings yet
- NCPDocument6 pagesNCPBelle OyosNo ratings yet
- Transforming Community Services 2011: Challenges and WinnersDocument11 pagesTransforming Community Services 2011: Challenges and WinnersDepartmentofHealthNo ratings yet