Professional Documents
Culture Documents
Upper Respiratory Tract Infections
Uploaded by
sierranevada123100%(1)100% found this document useful (1 vote)
76 views1 pagehopkins module
medical
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenthopkins module
medical
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
76 views1 pageUpper Respiratory Tract Infections
Uploaded by
sierranevada123hopkins module
medical
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Upper Respiratory Tract Infection Summary Page 2015
Christopher Hoffmann MD, Stephen D. Sisson MD/Ambulatory Curriculum
Section 1: Upper respiratory tract infection
Causes: rhinovirus (30-50%); coronavirus (7-18%); influenza (5-7%); RSV (5%); parainfluenza, adenovirus and
enterovirus each <5%
Symptoms: sore throat, sneezing, cough, nasal congestion, headache, sinus pressure, malaise
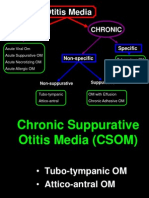
Complications: rare (<2%), include bacterial sinusitis or otitis media
Treatment: symptomatic; antibiotics are not indicated
Section 2: Influenza
Causes: influenza A; influenza B
o Antigenic drift: small changes in HA and NA antigens
o Antigenic shift: major change in HA or NA antigen; results in pandemic. Swine-origin H1N1 in 2009
represented antigenic shift.
Symptoms: fever, myalgias, malaise/lethargy, non-productive cough, sore throat, delirium
Diagnosis: consider EBV, acute HIV in differential, as clinical overlap significant
Treatment: treatment must begin within 48H of onset of symptoms; vaccination always preferable
o Amantadine/rimantadine: treats only influenza A; resistance widespread
Amantadine: 100mg bid (100mg qd if age>65 or renal insuff)
Rimantadine: 100mg bid (100mg qd if age >65 or renal insuff
o Oseltamivir/zanamivir: treats influenza A and B. Zanamivir is by inhalation; use with caution if h/o reactive
airways.
Oseltamivir: 75mg bid x 5d; Widespread Influenza A H1N1 resistance to this drug seen in 2008-09
season.
Zanamivir: 100mg bid inhalation. Influenza A resistance not seen but use limited by
contraindications (e.g., lung disease, elderly)
Section 3: Pharyngitis
Causes: Same as URTI, but add EBV, HIV, HSV, gonorrhea to differential.
o Major clinical concern is etiology of Streptococcus pyogenes (GABHS)
Complications: major concerns are rheumatic fever and post-streptococcal glomerulonephritis
o Treatment must begin within 9 days of onset of symptoms to prevent these complications
Diagnosis
o Centor criteria
T>38C
Tonsillar exudates
Tender cervical adenopathy
No cough or rhinitis
Treatment (penicillin is antibiotic of choice, with erythromycin used if allergic)
o 0-1 Centor criteria: symptomatic treatment
o 2 or 3 Centor criteria: rapid strep antigen test; antibiotics only if positive
o 4 Centor criteria: empiric antibiotics or rapid strep test and antibiotics if positive
Section 4: Sinusitis
Causes: Same as URTI; major clinical concern is presence of bacterial infection (S. pneumoniae most common; H.
influenzae second most common)
Diagnosis: Features suggestive of acute bacterial sinusitis include fever or any of the following:
o Presence of symptoms>7d or symptoms worsening after initial improvement
o Maxillary tooth pain
o Unilateral facial pain or unilateral sinus tenderness
o Purulent nasal discharge
Treatment: amoxicillin, doxycycline, trimethoprim/sulfamethoxazole are best options; use amoxicillin/clavulanate or
moxi/levofloxacin if recent antibiotic exposure
Section 5: Acute bronchitis
Definition: a respiratory illness of <3wks duration in which cough is primary complaint
Causes: same as URTI, but may include Mycoplasma pneumoniae, Chlamydophila pneumoniae
Diagnosis: differential includes pneumonia or pertussis. American College of Physicians states evaluation should focus
on clinically ruling out pneumonia
Treatment: antibiotics are not indicated for treatment of bronchitis. Beta-agonist inhalers, NSAIDs, first-generation
antihistamines may improve cough
You might also like
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesFrom EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNo ratings yet
- Dhanusthamba/Dhanurvata/Tetanus: Dr. Mahesh C KundagolDocument19 pagesDhanusthamba/Dhanurvata/Tetanus: Dr. Mahesh C KundagolkundagolNo ratings yet
- Upper Respiratory Tract InfectionDocument10 pagesUpper Respiratory Tract InfectionBrandon McgeeNo ratings yet
- Drug Resistant TuberculosisDocument58 pagesDrug Resistant TuberculosisbharatnarayananNo ratings yet
- Epid COPDDocument9 pagesEpid COPDAgung WistaraNo ratings yet
- Small Pox (CHN)Document13 pagesSmall Pox (CHN)Getom NgukirNo ratings yet
- Hypertension: Mayur BV BPH 3 Semester PSPHDocument29 pagesHypertension: Mayur BV BPH 3 Semester PSPHBijay Kumar MahatoNo ratings yet
- Hypertension SPMDocument25 pagesHypertension SPMSai tejendraNo ratings yet
- Pediatric Upper Respiratory InfectionsDocument74 pagesPediatric Upper Respiratory Infectionslordoftheweb100% (5)
- Alzeimer's DiseaseDocument11 pagesAlzeimer's DiseaseDale GoNo ratings yet
- A Study to Assess the Effectiveness of Video Assisted Teaching Module on Knowledge Regarding Myocardial Infarction and its Prevention among the Patients Attending Diabetic Clinic at BVV Sangha’s HSK Hospital and Research Centre, BagalkotDocument3 pagesA Study to Assess the Effectiveness of Video Assisted Teaching Module on Knowledge Regarding Myocardial Infarction and its Prevention among the Patients Attending Diabetic Clinic at BVV Sangha’s HSK Hospital and Research Centre, BagalkotInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Prognosis MGDocument7 pagesPrognosis MGPutri Cindy Claudia PandoyoNo ratings yet
- Zollinger Ellis Wps OfficeDocument15 pagesZollinger Ellis Wps OfficeAbhash MishraNo ratings yet
- TB MeningitisDocument17 pagesTB MeningitisSylvan LaminaNo ratings yet
- Manual 24 Hour RecallDocument160 pagesManual 24 Hour RecallMadalina CervidNo ratings yet
- What Is NeuropathyDocument4 pagesWhat Is NeuropathyLord Pozak MillerNo ratings yet
- ACUTE KIDNEY INJURY (AutoRecovered)Document21 pagesACUTE KIDNEY INJURY (AutoRecovered)Axsa Alex100% (1)
- Warning Signs of Various DiseasesDocument44 pagesWarning Signs of Various DiseasesamsabavanNo ratings yet
- Management of Asthma ExacerbationDocument13 pagesManagement of Asthma ExacerbationAini Shofa HaniahNo ratings yet
- A Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalDocument6 pagesA Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Malabsorption Diseases (My Seminar)Document75 pagesMalabsorption Diseases (My Seminar)Laith Al TamimiNo ratings yet
- Bronchial AsthmaDocument45 pagesBronchial Asthmamuluken mulatieNo ratings yet
- Case Study About: Cardiac Failure and Pulmonary EdemaDocument32 pagesCase Study About: Cardiac Failure and Pulmonary EdemaIan Simon DorojaNo ratings yet
- Health Assessment ON Genito Urinary System: Submitted To: Submitted byDocument16 pagesHealth Assessment ON Genito Urinary System: Submitted To: Submitted byAnanthibalaNo ratings yet
- Definition of HypertentionDocument10 pagesDefinition of HypertentionTSetiawan TSetiawanNo ratings yet
- Introduction To HematologyDocument61 pagesIntroduction To HematologyThis is PonyNo ratings yet
- Adult Chemotherapy Induced Anaphylaxis PolicyDocument12 pagesAdult Chemotherapy Induced Anaphylaxis PolicyMohammed Gazo100% (1)
- Pre Anaesthetic Check-UpDocument4 pagesPre Anaesthetic Check-UpUdoy PaulNo ratings yet
- GerdDocument19 pagesGerdMuhammad HafizdNo ratings yet
- Persuasive Communication in NursingDocument4 pagesPersuasive Communication in NursingNicole Audrey JoaquinNo ratings yet
- Brain Tumor PDFDocument11 pagesBrain Tumor PDFSujith KuttanNo ratings yet
- Riaz Gul AHN Unit 1Document106 pagesRiaz Gul AHN Unit 1Riaz Gul RindNo ratings yet
- Asthma Management and Prevention in ChildrenDocument57 pagesAsthma Management and Prevention in ChildrenSundararajaperumal AnandhakrishnanNo ratings yet
- Acute Bronchiolitis EditedDocument19 pagesAcute Bronchiolitis EditedSurgicalgownNo ratings yet
- Pneumonia: DefinitionDocument5 pagesPneumonia: DefinitionhemaanandhyNo ratings yet
- CSOM TreatmentDocument21 pagesCSOM TreatmentSarwinder SinghNo ratings yet
- Osce EarexamDocument2 pagesOsce EarexamminhaapNo ratings yet
- Seminar ON HepatitisDocument41 pagesSeminar ON HepatitissomivipinNo ratings yet
- After The Class Students Will Be Able To Gain Knowledge About TriageDocument3 pagesAfter The Class Students Will Be Able To Gain Knowledge About TriageRahul DamorNo ratings yet
- HIV:AIDS Determinants and Control of The EpidemicDocument4 pagesHIV:AIDS Determinants and Control of The EpidemicahiNo ratings yet
- Coronavirus Disease 2019 (COVID-19) - Nurseslabs PDFDocument21 pagesCoronavirus Disease 2019 (COVID-19) - Nurseslabs PDFSanket TelangNo ratings yet
- Colostomy CareDocument4 pagesColostomy CareRhenzes HaraNo ratings yet
- OxygenationDocument50 pagesOxygenationLulu MushiNo ratings yet
- Mounika G1Document8 pagesMounika G1pandem soniyaNo ratings yet
- Mood Stabilizers BookletDocument20 pagesMood Stabilizers Bookletrabiaa_48No ratings yet
- Case Presentation - GASTRODocument46 pagesCase Presentation - GASTROalidudeNo ratings yet
- Cardiopulmonary ResuscitationDocument22 pagesCardiopulmonary ResuscitationSundaraBharathiNo ratings yet
- Analgesics Content (AutoRecovered)Document11 pagesAnalgesics Content (AutoRecovered)ELISION OFFICIAL100% (1)
- Psychiatric EmergenciesDocument25 pagesPsychiatric EmergenciesAnnapurna DangetiNo ratings yet
- Ethical Issues of HIV and AIDS in HealthDocument25 pagesEthical Issues of HIV and AIDS in HealthSCRIBDISTHEBEASTNo ratings yet
- AppendicitisDocument36 pagesAppendicitisPetro MyronovNo ratings yet
- International Journal of Trend in Scientific Research and Development (IJTSRD)Document4 pagesInternational Journal of Trend in Scientific Research and Development (IJTSRD)Editor IJTSRDNo ratings yet
- World Patient Safety DayDocument17 pagesWorld Patient Safety DayNam PHẠM THÀNHNo ratings yet
- Acute Liver FailureDocument78 pagesAcute Liver FailurePankaj IngleNo ratings yet
- Heart Failure CaseDocument2 pagesHeart Failure CasePaulo Arwin BaduriaNo ratings yet
- What Is Epilepsy?Document10 pagesWhat Is Epilepsy?RegineCuasSulibNo ratings yet
- Medication ErrorDocument22 pagesMedication ErrorUzamaNo ratings yet
- The Perfect Neutropenic Diet Cookbook; The Complete Nutrition Guide To Reinstating Overall Health For General Wellness With Delectable And Nourishing RecipesFrom EverandThe Perfect Neutropenic Diet Cookbook; The Complete Nutrition Guide To Reinstating Overall Health For General Wellness With Delectable And Nourishing RecipesNo ratings yet
- Swine FluDocument22 pagesSwine FluNurhidayahNo ratings yet
- Human Immunodeficiency Virus Type 1: Sedayao, Mariano Jose Mls 3ADocument2 pagesHuman Immunodeficiency Virus Type 1: Sedayao, Mariano Jose Mls 3ABONNA FAYE CHRISZEL HUI YING TANNo ratings yet
- Respirador 3M N95Document18 pagesRespirador 3M N95Mirko Vela ReaNo ratings yet
- Infection & Specific Wound InfectionsDocument39 pagesInfection & Specific Wound InfectionsAhmed ShorshNo ratings yet
- Make A Tabulated Summary For Nematodes (Round Worms) : HabitatDocument4 pagesMake A Tabulated Summary For Nematodes (Round Worms) : HabitatJoshua TrinidadNo ratings yet
- Peace Corps MTG 200 Attach A DRUG FORMULARYDocument7 pagesPeace Corps MTG 200 Attach A DRUG FORMULARYAccessible Journal Media: Peace Corps DocumentsNo ratings yet
- Implementing AORN Recommended Practices For Surgical AttireDocument19 pagesImplementing AORN Recommended Practices For Surgical AttireKimberly Bundley-JohnsonNo ratings yet
- ImpetigoDocument31 pagesImpetigoUmmu Insyirah100% (1)
- Sand Fly PDFDocument4 pagesSand Fly PDFSneha SahaNo ratings yet
- PARASITOLOGYDocument35 pagesPARASITOLOGYMcarl Matel100% (8)
- Medical Microbiology 2 Presentation VisaDocument53 pagesMedical Microbiology 2 Presentation VisavisaNo ratings yet
- 160 Nursing Bullets - Medical Surgical NursingDocument7 pages160 Nursing Bullets - Medical Surgical Nursingdecsag06No ratings yet
- Urinary Tract Infections During PregnancyDocument8 pagesUrinary Tract Infections During PregnancyGloria SaldivarNo ratings yet
- 1 s2.0 S0167701218306821 Main PDFDocument5 pages1 s2.0 S0167701218306821 Main PDFDiego TulcanNo ratings yet
- Acute Viral Encephalitis in Children Clinical Manifestations and DiagnosisDocument41 pagesAcute Viral Encephalitis in Children Clinical Manifestations and DiagnosisCRISTOPHER CHAVAR GARCIANo ratings yet
- Freedom ConferenceDocument1 pageFreedom ConferencePeer Coach Academy Colorado100% (2)
- Sexually Transmitted Diseases PDFDocument31 pagesSexually Transmitted Diseases PDFMedicoz HeroNo ratings yet
- Al Borg Laboratories PriceDocument23 pagesAl Borg Laboratories PriceCheche Bureche0% (2)
- Subject PredicateDocument69 pagesSubject PredicateyuldaNo ratings yet
- Case Study On Otitis Media. Group 2 BSN2A MCNP, Penablanca, CagayanDocument27 pagesCase Study On Otitis Media. Group 2 BSN2A MCNP, Penablanca, CagayanJean nicole GaribayNo ratings yet
- MCQs of Pharmacology Unit-2 (D) Anti-Viral DrugsDocument4 pagesMCQs of Pharmacology Unit-2 (D) Anti-Viral DrugsShayan ShayanNo ratings yet
- Uti NCPDocument3 pagesUti NCPHamdy Pagilit Dimaporo0% (1)
- Nano Based Approach To Combat Emerging Viral NIPAH Virus InfectionDocument26 pagesNano Based Approach To Combat Emerging Viral NIPAH Virus InfectionYolanda Charlota ThenuNo ratings yet
- Communicable Disease Basics WordDocument7 pagesCommunicable Disease Basics WordGena SabellanoNo ratings yet
- Icd 10 Kasus Bedah SarafDocument8 pagesIcd 10 Kasus Bedah SarafHanda YaniNo ratings yet
- The Physical and Sexual SelfDocument49 pagesThe Physical and Sexual SelfFuransuhito100% (1)
- Rekaptulasi Pasien Berisi Atau Perbulan (Autorecovered)Document384 pagesRekaptulasi Pasien Berisi Atau Perbulan (Autorecovered)Namichan17No ratings yet
- CoronaDocument7 pagesCoronaAlicia ParadiseNo ratings yet
- HIV Topic Discussion HandoutDocument4 pagesHIV Topic Discussion HandoutMatthew LeiNo ratings yet
- Communicable Diseases Lecture 32 Pages Pg. 567 597Document32 pagesCommunicable Diseases Lecture 32 Pages Pg. 567 597ShiraishiNo ratings yet