Professional Documents
Culture Documents
NCP For Pneumonia
Uploaded by
KahMallariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP For Pneumonia
Uploaded by
KahMallariCopyright:
Available Formats
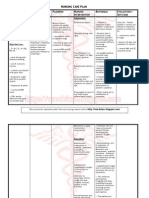
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective:
Ilang araw na syang
inuubo at nahihirapang
huminga, as verbalized
by the relative of the
patient.
Objective:
O2 sat: 80%
With O2 at
2LPM via nasal
cannula
Respirations:
24breaths/min
Chronically bed
ridden
81 y/o
Skin is pale and
cool to touch
Use of accessory
muscles when
breathing
Inspiratory
crackles with
diminished
breath sounds
when
auscultated
Thick yellow
sputum is
present during
suctioning
Ineffective airway
clearance related to thick
sputum secondary to
pneumonia as evidenced
by adventitious
breath sounds and thick
yellow sputum.
Pneumonia is an
inflammation of the lung
parenchyma, associated
with alveolar edema and
congestion that impair
gas exchange.
Short Term:
After 8 hours of nursing
interventions, the patient
will be able to
expectorate/clear
secretions readily.
Long Term:
After 1 week of nursing
interventions, the patient
will be able to maintain
airway patency by
showing:
a. Normal breath
sounds when
auscultated
b. Respiratory rate
of 16-20
breaths/min
c. Not using
accessory
muscles when
breathing
Monitor rate, rhythm,
depth, and effort of
respirations.
Note chest movements,
watch for symmetry, use
of accessory
muscles, and
supraclavicular and
intercostal muscle
retractions.
Elevate head of the
bed/change position
every 2hours and prn
Promote systemic fluid
hydration, as
appropriate.
Oral suction prn.
Auscultate lung sounds
after treatments to note
results.
Institute respiratory
therapy treatments (e.g.,
nebulizer, expectorant,
bronchodilators) as
needed.
Provides a basis for
evaluating adequacy of
ventilation.
Presence of nasal flaring
and use of accessory
muscles of respirations
may occur in response to
ineffective ventilation.
To take advantage of
gravity decreasing
pressure on the
diaphragm and
enhancing drainage
of/ventilation to different
lung segments.
Adequate fluid intake
enhances liquefaction of
pulmonary secretions
and facilitates
expectoration of mucus.
To clear out secretions
when it blocks the
airway.
Assists in evaluating
prescribed treatments
and client outcomes.
A variety of respiratory
therapy treatments may
be used to open
constricted airways and
liquefy secretions.
Short Term:
After 8 hours of nursing
interventions, the patient
was able to
expectorate/clear
secretions readily.
Long Term:
After 1 week of nursing
interventions, the patient
was able to maintain
airway patency by
showing:
a. Normal breath
sounds when
auscultated
b. Respiratory rate
of 16-20
breaths/min
c. Not using
accessory
muscles when
breathing
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective:
Patients relative stated,
lalo syang nanghina
nung magkaubo.
Objective:
O2 sat: 80%
With O2 at
2LPM via nasal
cannula
Respirations:
24breaths/min
Chronically bed
ridden
81 y/o
Skin is pale and
cool to touch
PEG
Iron supplement
medication
Activity intolerance
related to exhaustion
associated with
interruption in usual
sleep pattern because of
discomfort, excessive
coughing, and dyspnea as
evidenced by verbal
reports.
Definition: Insufficient
physiological or
psychological energy to
endure or complete
required or desired daily
activities
Short Term:
After 8 hours of nursing
interventions, the patient
will be able to report a
measurable increase in
tolerance to activity with
absence of dyspnea and
excessive fatigue, and
vital signs within
patients acceptable
range.
Long Term:
After 1 week of nursing
interventions, the patient
will be able demonstrate
a measurable increase in
tolerance to activity with
absence of dyspnea and
excessive fatigue, and
vital signs within
patients acceptable
range.
Evaluate patients
response to activity. Note
reports of dyspnea,
increased weakness/
fatigue, and changes in
vital signs during and
after activities.
Provide a quiet
environment and limit
visitors.
Explain importance of
rest in treatment plan
and necessity for
balancing activities with
rest.
Assist patient to assume
comfortable position for
rest/ sleep.
Assist with self-care
activities as necessary.
Provide for progressive
increase in activities
during recovery phase
and demand.
Establishes patients
capabilities/needs and
facilitates choice of
interventions.
Reduces stress and
excess stimulation,
promoting rest.
Bed rest is maintained
during acute phase to
decrease metabolic
demands, thus
conserving energy for
healing. Activity
restrictions thereafter
are determined by
individual patient
response to activity and
resolution of respiratory
insufficiency.
Patient may be
comfortable with head of
bed elevated, sleeping in
a chair, or leaning
forward on over bed
table with pillow support.
Minimizes exhaustion
and helps balance oxygen
supply and demand.
Short Term:
After 8 hours of nursing
interventions, the patient
was able to report a
measurable increase in
tolerance to activity with
absence of dyspnea and
excessive fatigue, and
vital signs within
patients acceptable
range.
Long Term:
After 1 week of nursing
interventions, the patient
was able demonstrate a
measurable increase in
tolerance to activity with
absence of dyspnea and
excessive fatigue, and
vital signs within
patients acceptable
range.
You might also like
- Improve Activity Tolerance Through Rest and RelaxationDocument7 pagesImprove Activity Tolerance Through Rest and RelaxationKrisJane Ratilla Abiva100% (2)
- NCPDocument9 pagesNCPEjie Boy Isaga67% (3)
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway ClearanceImation DataNo ratings yet
- PTB NCPDocument12 pagesPTB NCPNiel LeeNo ratings yet
- Causes and Nursing Care of Pleural EffusionDocument4 pagesCauses and Nursing Care of Pleural EffusionHania Polangi100% (1)
- Pleural Effusion NCPsDocument7 pagesPleural Effusion NCPsJaja Nagallo100% (2)
- NCP PneumoniaDocument2 pagesNCP PneumoniaSteffanie Serrano100% (1)
- Nursing Care Plan For Pneumonia NCPDocument3 pagesNursing Care Plan For Pneumonia NCPderic79% (133)
- NCP PneumoniaDocument3 pagesNCP Pneumoniakaiserdominick100% (2)
- SAMPLE NCP For PneumoniaDocument3 pagesSAMPLE NCP For Pneumoniakana_mercado100% (6)
- Asthma Impaired Gas ExchangeDocument2 pagesAsthma Impaired Gas ExchangeNedeve Ozned100% (5)
- Pneumonia NCPDocument5 pagesPneumonia NCPElbert Aquitania Mutuc RN100% (2)
- NCP Ineffective Airway Clearance For PneumoniaDocument5 pagesNCP Ineffective Airway Clearance For PneumoniaKullin Rain100% (1)
- Pneumonia-Ineffective Airway ClearanceDocument2 pagesPneumonia-Ineffective Airway ClearanceNursesLabs.com86% (7)
- Ineffective Breathing PatternDocument5 pagesIneffective Breathing PatternruguNo ratings yet
- NCP For Community Acquired PnuemoniaDocument7 pagesNCP For Community Acquired PnuemoniaAshley Gaton Alindogan100% (1)
- NCP PneumoniaDocument28 pagesNCP PneumoniaW'ton Borbe83% (6)
- Nursing Care Plan For Ineffective Airway ClearanceDocument7 pagesNursing Care Plan For Ineffective Airway Clearancearlee marquez96% (117)
- NCP - CapDocument4 pagesNCP - CapSherryNo ratings yet
- Nursing Care Plan for PneumoniaDocument4 pagesNursing Care Plan for PneumoniaJazzmin Angel ComalingNo ratings yet
- Cap NCPDocument2 pagesCap NCPkyshb100% (2)
- NCP For AsthmaDocument1 pageNCP For AsthmaMelvin Martinez100% (1)
- Lopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaDocument9 pagesLopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaSofia Lopez100% (2)
- Nursing Interventions for PneumoniaDocument2 pagesNursing Interventions for PneumoniaGabriel Tolentino70% (10)
- NCP Ineffective Breathing Pattern TalaDocument1 pageNCP Ineffective Breathing Pattern TalaJhen Bitco Fidel70% (10)
- NCP PneumoniaDocument2 pagesNCP Pneumonia_garonNo ratings yet
- Pneumonia NCPDocument7 pagesPneumonia NCPitsmeaya100% (3)
- Ineffective Breathing PatternDocument8 pagesIneffective Breathing PatternJansen Arquilita Rivera100% (2)
- NCP For Aspiration PnuemoniaDocument11 pagesNCP For Aspiration PnuemoniaChristy Rose AgrisNo ratings yet
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- NCP 1 Ineffective Airway ClearanceDocument2 pagesNCP 1 Ineffective Airway ClearanceDivine Jane PurciaNo ratings yet
- NCP Ineffective Breathing ActualDocument3 pagesNCP Ineffective Breathing ActualArian May Marcos100% (1)
- NCP AsthmaDocument3 pagesNCP AsthmaGellie Santos68% (19)
- Ineffective Airway ClearanceDocument1 pageIneffective Airway Clearancerozj0750% (2)
- NCP - Ineffective Airway ClearanceDocument2 pagesNCP - Ineffective Airway Clearancelarapatricia1215No ratings yet
- NANDA Page 658Document5 pagesNANDA Page 658Ashley Gaton Alindogan100% (1)
- Ineffective Breathing Pattern - NCPDocument2 pagesIneffective Breathing Pattern - NCPHsintan HsuNo ratings yet
- Nursing Care Plan Impaired Gas ExchangeDocument1 pageNursing Care Plan Impaired Gas Exchangecuicuita100% (3)
- NCP Ineffective Airway ClearanceDocument5 pagesNCP Ineffective Airway ClearanceEmm Estipona HaoNo ratings yet
- ANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationDocument2 pagesANOLIN, Marc Edriann T. Nursing Care Plan Assessmen T Diagnosis Rationale Planning Interventio N Rationale EvaluationEdrianne Tui100% (2)
- NCP For FeverDocument2 pagesNCP For FeverDominises Jade Corpuz82% (17)
- Improving airway clearance and managing activity intoleranceDocument2 pagesImproving airway clearance and managing activity intoleranceAva VierNo ratings yet
- Nursing Care Plan Problem: Difficulty of BreathingDocument5 pagesNursing Care Plan Problem: Difficulty of BreathingIvan Louise Fajardo ManiquizNo ratings yet
- 4 NCP's FinalDocument9 pages4 NCP's FinalZenel Yap100% (1)
- NCPDocument4 pagesNCPAbegail Abaygar100% (1)
- Revised NCP (Baiae)Document9 pagesRevised NCP (Baiae)Jennifer BactatNo ratings yet
- NCPDocument4 pagesNCPEugine Elizabeth Pilarca PerezNo ratings yet
- Nursing Care PlanDocument10 pagesNursing Care PlanmariasomorayNo ratings yet
- Ineffective Breathing Pattern Nursing DiagnosisDocument2 pagesIneffective Breathing Pattern Nursing DiagnosisChristianmel JavierNo ratings yet
- Nursing Careplan #1Document15 pagesNursing Careplan #1aninNo ratings yet
- CVA NCP Ineffective Airway ClearanceDocument2 pagesCVA NCP Ineffective Airway ClearanceJoanne Kaye Taylor100% (1)
- NCP JulieDocument14 pagesNCP JulieJulie Mae RubioNo ratings yet
- Nursing Care Plan for Ineffective Airway ClearanceDocument9 pagesNursing Care Plan for Ineffective Airway ClearanceAngelokeizer GavinoNo ratings yet
- Wk2 NCP Edited2012Document6 pagesWk2 NCP Edited2012Jessely Caling SalasNo ratings yet
- 1 Ineffective Airway ClearanceDocument8 pages1 Ineffective Airway ClearanceEsel Mae DinamlingNo ratings yet
- Nursing Care Plan for Respiratory ConditionsDocument7 pagesNursing Care Plan for Respiratory ConditionsJonathan Delos ReyesNo ratings yet
- Activity Intolerance NCPDocument6 pagesActivity Intolerance NCPDoo NahNo ratings yet
- Postural DrainageDocument6 pagesPostural DrainageKit Alizon Barredo0% (1)
- Nursing Diagnosis and Interventions for Pneumonia, Aspiration Risk, Breathing IssuesDocument9 pagesNursing Diagnosis and Interventions for Pneumonia, Aspiration Risk, Breathing IssuesmizrypNo ratings yet
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- What Is Macular Pucker, Epiretinal Membrane and Macular Pucker Surgery, Treatment, Recovery?Document2 pagesWhat Is Macular Pucker, Epiretinal Membrane and Macular Pucker Surgery, Treatment, Recovery?http://feelgoodtime.netNo ratings yet
- CLACIDODocument22 pagesCLACIDOSergel CapsuleNo ratings yet
- BullyingDocument8 pagesBullyingJennifer OestarNo ratings yet
- Dr. Joseph Mercola - Total Health ProgramDocument296 pagesDr. Joseph Mercola - Total Health ProgramCatalin BaicanNo ratings yet
- CGH202012022479 Lab-2020-0411918 Laboratory Covid-Pcr-TestDocument2 pagesCGH202012022479 Lab-2020-0411918 Laboratory Covid-Pcr-TestJosa Camille BungayNo ratings yet
- Contact Dermatitis Skin Blisters Hives Dermatitis: Treating A Rash at HomeDocument3 pagesContact Dermatitis Skin Blisters Hives Dermatitis: Treating A Rash at HomeDesty ArianiNo ratings yet
- Getting The Most Out of The Clinical Encounter: The Four Habits ModelDocument11 pagesGetting The Most Out of The Clinical Encounter: The Four Habits ModelFacu YaneNo ratings yet
- Newstart: Nutrition Exercise Water Sunlight Temperance Air Rest TrustDocument77 pagesNewstart: Nutrition Exercise Water Sunlight Temperance Air Rest TrustFaline Lumindas BalansagNo ratings yet
- Americanas Neumo PDFDocument291 pagesAmericanas Neumo PDFUri MoraNo ratings yet
- Environmental Impact AssessmentDocument24 pagesEnvironmental Impact AssessmentSeann Marquez100% (1)
- FactSheetAD 101 Adults FINAL EditedDocument1 pageFactSheetAD 101 Adults FINAL EditedAidana AidarbekNo ratings yet
- Jennifer Coates CVDocument19 pagesJennifer Coates CVMuhammadTanvirNo ratings yet
- MSDS Carbon Fiber Sheet PDFDocument6 pagesMSDS Carbon Fiber Sheet PDFiran1362No ratings yet
- Recognition of Psychotherapy EffectivenessDocument6 pagesRecognition of Psychotherapy EffectivenessPablo Cesar Chavez VeraNo ratings yet
- Green 1974Document31 pagesGreen 1974uciiiiii908No ratings yet
- Rajiv Gandhi National Quality Award Eligibility and Assessment CriteriaDocument2 pagesRajiv Gandhi National Quality Award Eligibility and Assessment Criteriasidharth100% (1)
- Module 5 Lesson 2 - DiscoveriesDocument2 pagesModule 5 Lesson 2 - Discoveriesdeez nutsNo ratings yet
- Airborne Microbes of Medical and Agricultural Importance MCB 403Document5 pagesAirborne Microbes of Medical and Agricultural Importance MCB 403abu firdawsNo ratings yet
- Ward Round Participation - Introduction - : Prepared By: Dr. C. Suhas ReddyDocument25 pagesWard Round Participation - Introduction - : Prepared By: Dr. C. Suhas Reddysuhas reddyNo ratings yet
- Diagnostic Exam AnsDocument14 pagesDiagnostic Exam AnsDarren Mae MosadaNo ratings yet
- Curriculum Map: Davao Wisdom AcademyDocument10 pagesCurriculum Map: Davao Wisdom Academycindy juntongNo ratings yet
- 6.3 Ergonomics For General Industry & OshaDocument33 pages6.3 Ergonomics For General Industry & Osharazlan ghazaliNo ratings yet
- Intravenous Injection: Presented by Mrs. Silpa Jose T Assistant Professor STCON, KattanamDocument33 pagesIntravenous Injection: Presented by Mrs. Silpa Jose T Assistant Professor STCON, KattanamSilpa Jose TNo ratings yet
- Competente Engleza 2019 PDFDocument11 pagesCompetente Engleza 2019 PDFAna Panait100% (1)
- ResumeDocument3 pagesResumeapi-311643710No ratings yet
- 2022 POP FINAL EXAM TIMETABLEDocument11 pages2022 POP FINAL EXAM TIMETABLEokoro collinsNo ratings yet
- CT Somatom ForceDocument8 pagesCT Somatom ForcerchidNo ratings yet
- dm2020 0123Document47 pagesdm2020 0123Franchise AlienNo ratings yet
- GERD Nursing CareDocument9 pagesGERD Nursing CareTrisha ArizalaNo ratings yet
- Georgia Dept. of Public Health HFR COVID-19 Report Posted 5.7.2020Document12 pagesGeorgia Dept. of Public Health HFR COVID-19 Report Posted 5.7.2020NewsChannel 9 StaffNo ratings yet