Professional Documents
Culture Documents
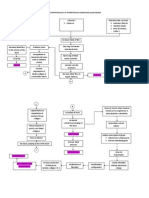
Pathophysiology of Hypertension
Uploaded by
Kaloy KamaoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathophysiology of Hypertension
Uploaded by
Kaloy KamaoCopyright:
Available Formats
Pathophysiology of Hypertension
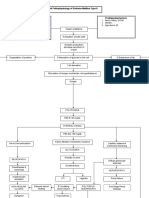
Pathophysiology of Cancer
Pathophysiology of Dementia
Pathophysiology of Stroke
Pathophysiology of Diabetes
Liceo de Cagayan University
College of Nursing
ASSIGNMENT IN
ELECTIVE 2
Submitted to:
Mrs. Emmie G. Basas
Submitted by:
Rose May O. Co Paler
April 24, 2013
Diabetes management
Food
Healthy eating is a cornerstone of any diabetes management plan. But it's not
just what you eat that affects your blood sugar level. How much you eat and
when you eat matters, too.
What to do:
Keep to a schedule. Your blood sugar level is highest an hour or two after you
eat, and then begins to fall. But this predictable pattern can work to your
advantage. You can help lessen the amount of change in your blood sugar levels
if you eat at the same time every day, eat several small meals a day or eat
healthy snacks at regular times between meals.
Make every meal well-balanced. As much as possible, plan for every meal to
have the right mix of starches, fruits and vegetables, proteins, and fats. It's
especially important to eat about the same amount of carbohydrates at each
meal and snack because they have a big effect on blood sugar levels. Talk to
your doctor, nurse or dietitian about the best food choices and appropriate
balance.
Eat the right amount of foods. Learn what portion size is appropriate for each
type of food. Simplify your meal planning by writing down portions for the foods
you eat often. Use measuring cups or a scale to ensure proper portion size.
Coordinate your meals and medication. Too little food in comparison to your
diabetes medications especially insulin may result in dangerously low blood
sugar (hypoglycemia). Too much food may cause your blood sugar level to climb
too high (hyperglycemia). Talk to your diabetes health care team about how to
best coordinate meal and medication schedules.
Exercise
Physical activity is another important part of your diabetes management plan.
When you exercise, your muscles use sugar (glucose) for energy. Regular
physical activity also improves your body's response to insulin. These factors
work together to lower your blood sugar level. The more strenuous your workout,
the longer the effect lasts. But even light activities such as housework,
gardening or being on your feet for extended periods can lower your blood
sugar level.
What to do:
Talk to your doctor about an exercise plan. Ask your doctor about what type
of exercise is appropriate for you. If you've been inactive for a long time, your
doctor may want to check the condition of your heart and feet before advising
you. He or she can recommend the right balance of aerobic and muscle-
strengthening exercise.
Keep an exercise schedule. Talk to your doctor about the best time of day for
you to exercise so that your workout routine is coordinated with your meal and
medication schedules.
Know your numbers. Talk to your doctor about what blood sugar levels are
appropriate for you before you begin exercise.
Check your blood sugar level. Check your blood sugar level before, during and
after exercise, especially if you take insulin or medications that lower blood
sugar. Be aware of warning signs of low blood sugar, such as feeling shaky,
weak, confused, lightheaded, irritable, anxious, tired or hungry.
Stay hydrated. Drink plenty of water while exercising because dehydration can
affect blood sugar levels.
Be prepared. Always have a small snack or glucose pill with you during exercise
in case your blood sugar drops too low. Wear a medical identification bracelet
when you're exercising.
Adjust your diabetes treatment plan as needed. If you take insulin, you may
need to adjust your insulin dose before exercising or wait a few hours to exercise
after injecting insulin. Your doctor can advise you on appropriate changes in your
medication. You may need to adjust treatment if you've increased your exercise
routine.
Medication
Insulin and other diabetes medications are designed to lower your blood sugar
level when diet and exercise alone aren't sufficient for managing diabetes. But
the effectiveness of these medications depends on the timing and size of the
dose. And any medications you take for conditions other than diabetes can affect
your blood sugar level, too.
What to do:
Store insulin properly. Insulin that's improperly stored or past its expiration date
may not be effective.
Report problems to your doctor. If your diabetes medications cause your blood
sugar level to drop too low, the dosage or timing may need to be adjusted.
Be cautious with new medications. If you're considering an over-the-counter
medication or your doctor prescribes a new drug to treat another condition
such as high blood pressure or high cholesterol ask your doctor or pharmacist
if the medication may affect your blood sugar level. Sometimes an alternate
medication may be recommended.
Coping Mechanism and Support System of Diabetes
THE STRESS RESPONSE
The body responds to stress by producing certain hormones that cause a rapid
heartbeat, faster breathing and a rise in blood pressureotherwise known as the
fight or flight response. Even when you do not experience these kinds of
symptoms, stressespecially chronic stresscan affect your health. Common
symptoms of chronic stress are fatigue, anxiety, headaches and stomach
cramps.
DIABETES AND STRESS
Having diabetes and adjusting your lifestyle to care for it can be stressful. Stress
can also affect your diabetes. The hormones your body produces when you are
stressed can raise blood glucose levels. Some people find that stress causes
their blood glucose levels to drop, but this is less common. Either way, stress can
make your diabetes harder to predict and harder to control.
IDENTIFYING STRESS
Before you can cope with stress, you need to be able to identify when you are
under stress. Signs that tell you your mind and body are under stress can include
headaches, tight muscles in your neck or shoulders, changes in eating or
sleeping patterns, moodiness, loss of interest in fun activities, and feelings of
confusion or uncertainty. You may find it helpful to keep track of certain
information, such as how you feel when you are under stress, what causes you
stress and how you handle stress. You can use this information much the same
way you use your diabetes data: to evaluate your personal stressors and the
most effective ways for you to deal with stressful events.
DEALING WITH STRESS
We all have our preferred ways of dealing with stress. Some coping methods,
such as eating too much, drinking alcohol or smoking, may help ease tension
initially, but have hazardous effects in the long runespecially if you have
diabetes. Finding effective coping mechanisms to deal with both the positive and
negative stresses in your life can help you feel in control, informed and supported
by other people.
STRESS BEATERS
Get some exercise. Exercise is a proven stress beater.
Take a break and get some rest.
Find some support. Talk with a friend, family or a professional. Look for a
support group.
Find someone to express your feelings to. If you dont have a person you
can talk to, try writing your feelings down.
Actively take care of your body: meditate, get a massage or take a
relaxing bath.
Set manageable goals.
Take time to do the things you love, not just the things you have to do.
Learn to say no, or set limits on those things that dont fit with your goals.
Move forward. Take positive actions to change what you can about the
situation.
Change your outlook. Learn to look at the issue differently, reassess its
importance or let it go.
It is important to learn how to cope with stress. Manage it well in order to
enjoy your life and deal more effectively with your diabetes.
Stroke management
Scope of the guidelines
These National Clinical Guidelines for stroke cover the management of patients
with acute stroke and the secondary prevention of stroke. Primary prevention of
stroke, rehabilitation and subarachnoid hemorrhage are excluded from the scope
of these guidelines. These guidelines cover the management of stroke in adults
(over 18 years) from onset to chronic care and focus on patients with a new
clinical event (first stroke or recurrent stroke).
Goal and objectives of the guidelines
The primary goal of the guidelines is to continuously improve the quality of care
in patients with stroke nationally. Our intention is closing the gap between best
practice and actual practice.
The objective of the guidelines is to provide clinicians and administrators with
explicit statements, where evidence is available, on the best way to manage
specific problems. Local health service facilities (e.g. hospitals, nursing homes,
etc.) will need to add detail.
The guidelines are directed primarily at practising clinicians involved in
management of patients with stroke. Their aim is to help clinicians, at any level
primary, secondary or tertiary - to make the best decisions for each patient, using
the evidence currently available. The focus is on the more common clinical
questions faced in day-to-day practice. The guidelines may be used by all health
professionals or health care planners involved in the management of the patients
with stroke.
The secondary objectives of the guidelines are to identify areas where gaps in
knowledge or lack of evidence exist and to stimulate research in each area.
The guidelines are concerned with the management of patients who present with
a new clinical event that might be stroke. Stroke in this context is defined as a
clinical syndrome characterized by rapidly developing signs and symptoms of
focal or at times global loss (as in subarachnoid hemorrhage or brain stem
involvement) of cerebral brain functions, lasting more than 24 hours or leading to
death, with no apparent cause other than of vascular origin.
While appraisal of evidence forms the basis of the development of these
guidelines, we wish to clarify some points:
Evidence related to drugs is generally stronger, because it is
methodologically easier to study each intervention in contrast to studying
complex intervention like occupational therapy, health education or
nursing care. These do not necessarily mean that interventions with so
called strong evidence are more important than those where the evidence
is weak.
We believe that highest level of evidence is not always required to make
strong recommendation. If the intervention is safe, logic is strong and
effect is obvious, the level of evidence desirable to make strong
recommendation may be lower than the highest.
We recognize that many areas of clinical importance may not have
evidence available to construct guidelines, and the recommendations
represent a consensus from the working group on such areas.
The working group is aware of recent developments in evaluating levels of
evidence and strength of recommendations, and also that the GRADE
methodology has been adopted by more than 25 organizations around the world
including the WHO. The group endorses the use of GRADE methodology (Guyatt
and Oxman)[1] for this purpose and will incorporate this in the next version of the
guidelines.
Context and use
These guidelines should be taken as statements to inform the clinician, not as
rigid rules. Practitioners may need to deviate from the guidelines in individual
cases but such deviations should be justifiable and justified.
The guidelines may be used to inform decisions on standards of good practice
and are likely to be used for audit of stroke services. Before the guidelines are
used as standards, it is important to ensure that the relevance and
appropriateness of the guidelines are discussed in the context proposed.
These guidelines do not cover specific management of associated illnesses like
diabetes mellitus, cardiac problems and others as these may addressed by
guidelines from related organizations or are generally expected from a physician.
:
Guidelines for Organization of Services for Stroke Care
Stroke care may be organized at three levels - a basic stroke care facility, a
primary stroke care facility and a comprehensive stroke care facility. The basic
stroke care facility should be the minimum setup at district hospitals; primary
stroke care facility should be mandatory for all medical colleges and
multispeciality hospitals; and well-equipped hospitals including some medical
colleges should develop comprehensive stroke care facilities. The basic stroke
facility may not have artificial ventilators, echocardiography and carotid Doppler
facility, primary stroke care facilities may have these facilities but not
neurosurgery, MRI or angiography. Comprehensive stroke care facilities should
have all these facilities.
Coping Mechanism of Stroke Patients
Physical Strength and Conditioning
Patients need to keep their movements strong and lively. You also need to keep
blood pressure and cholesterol under control to prevent complications or another
stroke. Both practices help a patient cope with the condition of restricted blood
flow and circulation, and the weakening of muscles from inactivity. Regular
walking strengthens muscles and the cardiovascular system. Weight lifting or tai
chi can make you stronger and raise your conditioning so you can have a more
active life.
Diet
Liveliness in daily activities depends upon a controlled weight and low blood
pressure and cholesterol. Eat a healthful diet low in salt, fat and sugars.
Vegetables, fiber-rich whole grain breads and chicken or fish are good for
controlling your weight and cardiovascular system. Nutritional charts and healthy
recipes can be a part of typical eating.
Daily Living
Daily living can be difficult after a stroke if you do not make changes to your
home. With less control, balance and vision on one side of your body, walking
through the home can be obstructed by a narrow doorway or end in slips or falls.
A patient needs clear access to each part of the house. If necessary, paths are
wide enough for walking with a walker or cane, or moving in a wheelchair.
Reorganizing the furniture so all pathways are clear is a wise choice. Danger can
be avoided by removing throw rugs. Modifications also might be a good choice.
Instead of leaning on furniture or fixtures, you can install grab bars for walking
stairs or entering the bathtub or ramps to enter heightened areas.
Communications
When a patient has had a stroke in the left side of the brain, a disruption of
communications occurs due to loss of blood flow to the language center in the
brain. This condition is called aphasia. A patient with aphasia has difficulty
forming words to speak or write, or can not understand when others talk to them.
Telling family and friends about the condition that is in the way of communicating
helps you cope with the difficulties in relating. Regular speech practice can
improve language ability.
Engagement and Activity
Patients can be depressed or upset by living with the effects of a stroke. Life is
made more vital by staying engaged with family and friends, and staying active,
to keep the emotions stable. Encourage friends and family to check in with you
and do social activities with you. Join a support group with stroke patients who
understand your condition. For vitality and pleasant satisfaction, live a physically
active life and do the things you enjoy.
Management of dementia
Education
The importance of education for the carer must not be underestimated
(Pollitt, 1994). This includes information about the disease, its prognosis
and likely consequences. It may include training in carrying out a
programme of behaviour modification and information about giving
medication. It can include information about the various means of
obtaining practical support.
Emotional support
It is important that the carer is also cared for. Opportunities are needed for
carers to talk about the problems they are having, and about their feelings,
including the negative feelings about the person with dementia. Carers
support groups as well as experienced counsellors (such as community
psychiatric nurses) can be of great benefit.
One carer, whose wife had Alzheimers disease, writing about his own
experience (Reveley, 1988) offered these pieces of advice: do not hide the
disease from those around you; take care of yourself; enlist help in all
areas; and take calculated risks.
Professional carers such as nurses, residential home staff, doctors and
social workers, also need support and care. A professional team needs to
build into it a mechanism to enable such support to be given. Hospital-
based professionals can help the staff of residential homes to think about
and to achieve their goals (see Garland, 1991).
Coping mechanism and support system in Dementia
It is important to remember that correcting your loved one will not rehabilitate the
brain damage caused by his disease. One of your most difficult challenges lies in
accepting his new communication pattern.
week to your offer to help her with something, that resentment can stay around
long after she remembers why she was displeased with you in the first place.
Keep in mind that this is not an attempt to mistreat you.
Second, its vital to realize that emotional memory may or may not be affected
along the course of dementia.
What you might find as a result
Dementia produces inconsistent behaviors within the same week or even the
same day. Similar to a fading fire sparking and flickering unpredictably, the
brains neurons can fire and achieve connections erratically and randomly. Brain
tissue damage to the emotional memory can cause your loved one to feel
embarrassed when he cant communicate a pressing need to his closest family
and friends.
The person with dementia cant prevent or control any of this, of course. But
family and friends instantaneously try to place comments and behavior in the
context of their longtime relationships. Its human nature.
empathy tip
imagine yourself in the dentists chair, mouth numbed and filled with cotton rolls.
Suddenly, you experience a sharp pain, or perhaps you need to use the
restroom. You try to speak, but even you cant understand your words. if you
point to your mouth, the dentist will probably guess pain rather quickly. But
how will you let him know you desperately need the restroom? and how long will
it take him to guess? thats exactly the frightening, embarrassing, panic-inducing
situation your loved one may experience.
empathy tip
Respect comprises a fundamental part of our shared humanity. People
diagnosed with dementia-from the very early stages, to those too ill to read this
guide-all recognize when theyre being treated with respect and when theyre not.
It becomes easy to associate any communication shortcomings with those of a
temperamental toddler learning to speak. This might cause you to behave in a
way that condescends or demeans your loved one. Remember, he is still an
adult with a lifetime of knowledge and experience, and he deserves your respect.
Management of cancer
Cancer can be treated by surgery, chemotherapy, radiation
therapy, immunotherapy, and monoclonal antibody therapy. The choice of
therapy depends upon the location and grade of the tumor and the stage of the
disease, as well as the general state of the patient (performance status). A
number of experimental cancer treatments are also under development.
Complete removal of the cancer without damage to the rest of the body is the
goal of treatment. Sometimes this can be accomplished by surgery, but the
propensity of cancers to invade adjacent tissue or to spread to distant sites by
microscopic metastasis often limits its effectiveness; chemotherapy and
radiotherapy can unfortunately have a negative effect on normal cells.
[1]
Because "cancer" refers to a class of diseases,
[2][3]
it is unlikely that there will
ever be a single "cure for cancer" any more than there will be a single treatment
for all infectious diseases.
[4]
Angiogenesis inhibitors were once thought to have
potential as a "silver bullet" treatment applicable to many types of cancer, but this
has not been the case in practice.
[5]
Coping Mechanisms and Support system for Cancer
Denial, anger, fear and depression are very common when coming to terms with
the disease, its prognosis and treatment. It is easy to feel scared and alone in
the face of breast cancer, and through this article we hope to provide information
on coping mechanisms, their importance, and where to turn to for social support
and help.
Every person reacts differently, and that's fine! Crying, shock, feelings of
numbness and being overwhelmed are all normal reactions. Just as people react
in different ways, there are many different ways to cope with a diagnosis of
breast cancer. There is a difference, however, between reacting and
coping. While people react in a multitude of ways, there are some coping
mechanisms that are considered healthier and more effective than others. Below
we will outline some of the more constructive ways to cope with a diagnosis of
breast cancer.
According to research, one of the most important aspects of a good coping
mechanism is social support. Confide in someone, whether it is family, friends or
a social support group. At the end of this article, you will find a link that provides
tips on how to break the news of your diagnosis to different family
members. Based on research found in medical literature, support from any
source can help reduce depression, emotional distress and anxiety. It can
decrease feelings of social isolation, and help improve your mood and
outlook. Support has not been shown to decrease the rate of recurrence of
survival, with the notable exception of one study conducted in 1989 whose
results have never been reproduced. Social support will undeniably improve
your quality of life.
While your family and friends can be an important and powerful source of
support, you might find it necessary to seek help and support from others. These
people include other survivors, support groups, physicians, nurses and social
workers. It is important to have an outside social support network as well as
family and friends as your diagnosis can often cause emotional strain on those
closest to you and it is very beneficial to have a support network at all times.
Many different kinds of support groups exist including those in your community,
online, religious and spiritual and those affiliated with the American Cancer
Society. The purpose and type of support offered can vary from group to group
and it is important to find the one that best suits your needs. According to the
Susan G. Komen website, support groups are classified as emotion-focused or
information-based. Emotion-focused groups emphasize sharing feelings, and
are best for people who are open to communicating their fears and hopes with
people outside of the family and friend circle. Others prefer to only share these
feelings with their close family and friends and information-based groups that
focus on patient education are more beneficial. Support groups also vary based
on the stage of your breast cancer. Some groups are geared toward those
recently diagnosed, some provide support during treatment, and others give
support to women and men who have achieved remission. Many online
discussion boards and support websites also exist, and links can be found
through the American Cancer Society website.
Often physicians and other health care workers are overlooked as sources of
support. This can be due to multiple factors, both from the patient and health
care provider. The Susan G. Komen website offers a brochure entitled Talking
with your doctor. The link can be found below. Some key points include doing a
little bit of research about your diagnosis ahead of time, asking open-ended
questions, taking notes, and giving your health care provider feedback on what
was or was not useful.
Another important and beneficial coping mechanism is staying active and eating
healthy. It is important to keep your immune system boosted and maintain a
healthy lifestyle in the face of a diagnosis of breast cancer. According to the
American Cancer Society, recommendations include eating a diet high in fruits,
vegetables, grains and fiber, and low in fat. Drinking plenty of fluids, getting a
good nights sleep and exercise are also important. One study showed that yoga
and meditation exercises improved emotional well-being, mood and general
quality of life in a diverse population of breast cancer survivors.Simply choosing
an activity you enjoy, such as walking, biking or swimming, can improve your
health in many ways.
COPD management
An effective COPD management plan includes four components: (1) assess and
monitor disease; (2) reduce risk factors; (3) manage stable COPD; (4) manage
exacerbations.
The goals of effective COPD management are to:
Prevent disease progression
Relieve symptoms
Improve exercise tolerance
Improve health status
Prevent and treat complications
Prevent and treat exacerbations
Reduce mortality
These goals should be reached with a minimum of side effects from treatment, a
particular challenge in patients with COPD where comorbidities are common.
The extent to which these goals can be realized varies with each individual, and
some treatments will produce benefits in more than one area. In selecting a
treatment plan, the benefits and risks to the individual and the costs, direct and
indirect, to the community must be considered. Patients should be identified
before the end stage of the illness, when disability is substantial. However, the
benefits of spirometric screening, of either the general population or smokers, are
still unclear. Educating patients and physicians to recognize that cough, sputum
production, and especially breathlessness are not trivial symptoms is an
essential aspect of the public health care of this disease.
Reduction of therapy once symptom control has been achieved is not normally
possible in COPD. Further deterioration of lung function usually requires the
progressive introduction of more treatments, both pharmacologic and
nonpharmacologic, to attempt to limit the impact of these changes. Acute
exacerbations of signs and symptoms, a hallmark of COPD, impair patients'
quality of life and decrease their health status. Appropriate treatment and
measures to prevent further exacerbations should be implemented as quickly as
possible.
Component 1: Assess and monitor disease
Diagnosis of COPD is based on a history of exposure to risk factors and the
presence of airflow limitation that is not fully reversible, with or without the
presence of symptoms.
Patients who have chronic cough and sputum production with a history of
exposure to risk factors should be tested for airflow limitation, even if they do not
have dyspnea.
For the diagnosis and assessment of COPD, spirometry is the gold standard as it
is the most reproducible, standardized, and objective way of measuring airflow
limitation. FEV1/FVC < 70% and a postbronchodilator FEV1 < 80% predicted
confirms the presence of airflow limitation that is not fully reversible.
Health care workers involved in the diagnosis and management of patients with
COPD should have access to spirometry.
Measurement of arterial blood gas tensions should be considered in all patients
with FEV1 < 40% predicted or clinical signs suggestive of respiratory failure or
right heart failure.
Component 2: Reduce risk ractors
Reduction of total personal exposure to tobacco smoke, occupational dusts and
chemicals, and indoor and outdoor air pollutants are important goals to prevent
the onset and progression of COPD.
Smoking cessation is the single most effective and cost-effective way to reduce
the risk of developing COPD and stop its progression. Brief tobacco dependence
treatment is effective and every tobacco user should be offered at least this
treatment at every visit to a health care provider.
Three types of counseling are especially effective: practical counseling, social
support as part of treatment, and social support arranged outside of treatment.
Several effective pharmacotherapies for tobacco dependence are available, and
at least one of these medications should be added to counseling if necessary
and in the absence of contraindications.
Progression of many occupationally induced respiratory disorders can be
reduced or controlled through a variety of strategies aimed at reducing the
burden of inhaled particles and gases.
Component 3: Manage stable COPD
The overall approach to managing stable COPD should be characterized by a
stepwise increase in treatment, depending on the severity of the disease.
For patients with COPD, health education can play a role in improving skills,
ability to cope with illness, and health status. It is effective in accomplishing
certain goals, including smoking cessation.
None of the existing medications for COPD has been shown to modify the long-
term decline in lung function that is the hallmark of this disease. Therefore,
pharmacotherapy for COPD is used to decrease symptoms and complications.
Bronchodilator medications are central to the symptomatic management of
COPD. They are given on an as-needed basis or on a regular basis to prevent or
reduce symptoms.
The principal bronchodilator treatments are 2-agonists, anticholinergics,
theophylline, and a combination of one or more of these drugs.
Regular treatment with inhaled glucocorticosteroids should only be prescribed for
symptomatic patients with COPD with a documented spirometric response to
glucocorticosteroids or for those with an FEV1 < 50% predicted and repeated
exacerbations requiring treatment with antibiotics or oral glucocorticosteroids.
Chronic treatment with systemic glucocorticosteroids should be avoided because
of an unfavorable benefit-to-risk ratio.
All patients with COPD benefit from exercise training programs, improving with
respect to both exercise tolerance and symptoms of dyspnea and fatigue.
The long-term administration of oxygen (> 15 h per day) to patients with chronic
respiratory failure has been shown to increase survival.
Component 4: Manage exacerbations
Exacerbations of respiratory symptoms requiring medical intervention are
important clinical events in COPD.
The most common causes of an exacerbation are infection of the
tracheobronchial tree and air pollution, but the cause of approximately one-third
of severe exacerbations cannot be identified.
Inhaled bronchodilators (particularly inhaled 2-agonists or anticholinergics),
theophylline, and systemic, preferably oral, glucocorticosteroids are effective for
treatments for acute exacerbations of COPD.
Patients experiencing COPD exacerbations with clinical signs of airway infection
(e.g., increased volume and change of color of sputum, or fever) may benefit
from antibiotic treatment.
Noninvasive positive pressure ventilation (NIPPV) in acute exacerbations
improves blood gases and pH, reduces in-hospital mortality, decreases the need
for invasive mechanical ventilation and intubation, and decreases the length of
hospital stay.
Coping mechanism and support system in COPD
Help for Physical COPD Symptoms
COPD requires lifestyle changes and ongoing care to cope with physical
symptoms like coughing, shortness of breath, and sputum. Your friends and
family can help, but you need to let them know what you need. Here are ways in
which they might help:
Daily chores. Ask your friends and family to help with daily chores, such as
getting your house organized, so that you don't have to move around as much
or go up and down stairs.
Transportation to rehab. Ask for help getting to your pulmonary
rehabilitation appointments. This is an important part of your treatment.
Attending doctors appointments. Ask a loved one to go with you to doctors
appointments. They can help you make a list of all your medications, write
down questions to ask your care team, and create a diary of your daily
symptoms.
Avoiding allergens and irritants. Ask the people who live with you to help
keep your home free of dust, fumes, and secondhand smoke.
Other resources. For more help and support, you can call the COPD
Information Line at 1-866-316-COPD and the Family Caregiver Alliance at 1-
800-445-8106.
Help for Quitting Smoking
If you have COPD and you are still smoking, you need to quit to
successfully manage your condition. "The fact that it takes the average person
about seven attempts to quit shows that most people need help with quitting
smoking," notes Wu.
Here are some ways you can get support for quitting smoking:
Encouragement from loved ones. Ask friends and family to encourage you
to quit and to help you by not smoking around you.
Quit-smoking programs. Join a smoking cessation program. "Behavior
modification learned in a smoking cessation program is key to quitting long-
term," says Wu. You can ask your doctor about finding a smoking program in
your area, such as at your local hospital.
Smoking cessation aids. Ask your doctor about using quit-smoking aids,
such as gum, a patch, or prescription pills.
Other resources. Take advantage of resources like www.smokefree.gov,
which provides tools and expert advice to help people quit smoking.
Although COPD symptoms can take an emotional and physical toll on you, there
is help available. The key is to not feel guilty about having COPD and to not be
ashamed to ask for help.
Learn as much as you can about COPD and encourage your family to get
educated too. Managing COPD well takes teamwork and support that you can
find through family, friends, support groups, COPD organizations, and your
health care team.
Management of Hypertension
Lifestyle interventions
Advise lifestyle measures in patients with hypertension and high normal blood
pressure (BP), ie clinic BP 130-139/85-89 mm Hg. Inform about any local
initiatives, and supplement advice with leaflets or audiovisual information.
Preventing or treating obesity
[
3
]
Weight reduction should be suggested if necessary, to maintain ideal body mass
index (BMI) of 20-25 kg/m
2
. Offer a diet sheet and/or dietetic appointment.
Dietary self-help, eg dieting clubs, may be appropriate.
The National Institute for Health and Clinical Excellence (NICE)
recommends basing meals on starchy foods (potatoes, bread, rice and
pasta) - using wholegrain bread, and brown rice if possible, but watch the
portion size of meals and cut down on snacks.
Eat foods rich in fibre, ie cereals, pulses (beans, peas, lentils, grains, seeds),
fruit and vegetables.
Have at least five portions of fruit and vegetables a day.
Select low-fat foods - avoid foods containing a lot of fat and sugar (eg fried
food, sweetened drinks, crisps, confectionery).
Reduce any excessive caffeine consumption and have a low dietary sodium
intake (reduce or substitute any sodium salt). Calcium, magnesium or
potassium supplements are not recommended.
Ensure you eat breakfast.
Cut alcohol intake to no more than 21 units (male) or 14 units (female) of
alcohol per week. Be careful not to take too many calories in the form of
alcohol.
See the Dietary Approaches to Stop Hypertension (DASH) eating plan.
[
4
]
Stopping smoking
Patients should stop smoking (offer help nicotine replacement therapy) - see
separate article Smoking Cessation.
Encouraging exercise
Make physical activities part of everyday life (eg walk or cycle to work, use
stairs instead of lift, walk at lunchtime), and build in enjoyable activities to
leisure time every week (e.g walking, cycling, gardening, swimming,
aerobics, etc.) .
Minimise sedentary activities, e.g limit television watching or sitting at a
computer or playing video games.
Once more, look for local activities, join a sporting group, take advantage of
taster sessions and get used to exercising regularly, ideally several times a
week.
Starting treatment
[
1
]
Consider treating immediately if BP in clinic is 180/110 mm Hg; otherwise,
consider after results of ambulatory blood pressure monitoring (ABPM) or home
blood pressure monitoring (HBPM), blood tests and cardiovascular risk
assessment are available.
Diagnose hypertension if average of ABPM or HBPM readings is 135/85 mm
Hg, (ignore first day readings and average the rest - see Hypertension article).
Stage 1 hypertension - clinic readings 140/90 mm Hg and ABPM/HBPM
135/85 mm Hg.
Stage 2 hypertension - clinic readings 160/100 mm Hg and ABPM/HBPM
150/95 mm Hg.
Drug treatment should be commenced in patients aged under 80 years with
stage 1 hypertension plus signs of end organ damage (known cardiovascular or
renal disease), or with diabetes mellitus or a 10-year cardiovascular disease
(CVD) risk 20%.
Treatment should be started in all patients (any age) with stage 2 hypertension.
Treat isolated systolic hypertension in the same way.
Coping mechanism and support system for hypertension
Want to remain adept at reasoning and continue recalling people, places, and
events in your life well into your golden years? Better exercise your body as well
as your mind while youre younger, say NC State researchers. Studies by
psychology professors in the College of Humanities and Social Sciences have
found links between various health factors and the cognitive performance of older
adults. The brain doesnt operate in a vacuum, Dr. Jason Allaire says. Factors
that adversely affect other systems in the body often diminish cognitive
functioning as well.
High blood pressure and lack of sleep are two such factors, according to Dr.
Alyssa Gamaldo, a former student of Allaires who earned her Ph.D. from NC
State in May and now works at the National Institute on Aging (NIA). Because
her sister is a sleep researcher, Gamaldo was curious to find if there was any
connection between sleep and memory. She tapped into data collected for the
Baltimore Study of Black Aging, a longitudinal study led by Allaire and a Duke
University professor, and found that seniors who reported having trouble falling
asleep performed worse on cognitive tests than those who slept soundly. Sleep
re-energizes the body and helps the mind consolidate memory, she says. So a
lack of sleep or disrupted sleep can easily affect your ability to function the next
day.
In a separate study, Gamaldo examined data from a group of older adults who,
for two months, took daily short-term memory and problem-solving tests and
measured their blood pressure every morning and afternoon. People who already
exhibited high blood pressure performed poorly on the tests when their pressure
spiked. Elevated blood pressure didnt adversely affect the mental agility of those
who werent hypertensive, however. Stressful situations make it more difficult for
some people to think clearly, Gamaldo says. Its not clear why people with
hypertension have a harder time than others processing information under
stress.
Dr. Shevaun Neupert, who studies older adults responses to stress, says they
routinely forget more when under stress. This is especially true if one has had an
argument or experienced some other setback to an interpersonal relationship.
Neupert, an assistant professor of psychology, is comparing her findings with
studies on younger adults to determine if the stress-memory relationship is true
for all ages or is more pronounced among seniors. We can avoid some stress in
our daily lives, but not all, she says. Recognizing that it could cause problems
for older adults will help us develop coping mechanisms and support systems for
them.
The NIA wants to find ways to maximize older adults ability to live independently,
so Dr. Tom Hess has been examining seniors judgment and decision-making
skills. The psychology professor has found that, while seniors cognitive abilities
decline, their base of knowledge remains intact. So they usually choose to focus
their mental energies on tasks and information that they deem most important.
Older adults tune out irrelevant information, he says, while younger people try
to integrate every detail.
Issues and Trends in COPD
You might also like
- Pathophysiology HypertensionDocument1 pagePathophysiology HypertensionAlinor Abubacar100% (3)
- Pathophysiology of Hypertensive Cardiovascular DiseaseDocument3 pagesPathophysiology of Hypertensive Cardiovascular Diseasekhrizaleeh100% (9)
- Pathophysiology HypertensionDocument2 pagesPathophysiology HypertensionCyrus De Asis50% (2)
- Pathophysilogy of Primary HypertensionDocument1 pagePathophysilogy of Primary Hypertensionromeo rivera75% (4)
- Hypertension PathophysiologyDocument1 pageHypertension PathophysiologyZaida Eunice EstabayaNo ratings yet
- Pathophysiology of Congestive Heart Failure: Predisposing Factors Precipitating/Aggravating FactorsDocument1 pagePathophysiology of Congestive Heart Failure: Predisposing Factors Precipitating/Aggravating Factorsguillermojerry100% (2)
- Pathophysiology of Congestive Heart Failure III With Pleural EffusionDocument3 pagesPathophysiology of Congestive Heart Failure III With Pleural EffusionKen100% (1)
- Pathophysiology of Congestive Heart Failure ExplainedDocument4 pagesPathophysiology of Congestive Heart Failure ExplainedMar Ble50% (2)
- Pathophysiology of CHFDocument1 pagePathophysiology of CHFImae Mayo60% (5)
- Pathophysiology of Congestive Heart FailureDocument2 pagesPathophysiology of Congestive Heart FailurePerry Oliver AlvarezNo ratings yet
- Pathophysiology of Diabetes Mellitus Type 2Document4 pagesPathophysiology of Diabetes Mellitus Type 2jo_annamae4413100% (3)
- Hypertension PathophysiologyDocument2 pagesHypertension PathophysiologyJems60% (5)
- Pathophysiology of HCVD DM2 CVD Left Basal GangliaDocument1 pagePathophysiology of HCVD DM2 CVD Left Basal GangliaJake Caballo100% (1)
- Pathophysiology of HCVD, DM2, CVD (Left Basal Ganglia)Document1 pagePathophysiology of HCVD, DM2, CVD (Left Basal Ganglia)rexale ria100% (1)
- Pathophysiology of Chronic Kidney DiseaseDocument2 pagesPathophysiology of Chronic Kidney DiseaseKeij AranetaNo ratings yet
- Pathophysiology of Congestive Heart FailureDocument2 pagesPathophysiology of Congestive Heart FailureAnonymous XvwKtnSrMR100% (10)
- Pathophysiology DMDocument1 pagePathophysiology DMMJ AmarilloNo ratings yet
- Pathophysiology of Congestive Heart FailureDocument2 pagesPathophysiology of Congestive Heart FailureTrixia Almendral100% (2)
- Anemia PathophysiologyDocument2 pagesAnemia PathophysiologyHoney Lorie D. Simbajon67% (6)
- Pathophysiology of Diabetes Mellitus Type 1Document3 pagesPathophysiology of Diabetes Mellitus Type 1CajRofuli100% (2)
- Pathophysiology of DMDocument5 pagesPathophysiology of DMRgn Mckl100% (3)
- Modifiable Risk Factors for Atherothrombotic and Embolic DiseasesDocument2 pagesModifiable Risk Factors for Atherothrombotic and Embolic DiseasesJoy Rachelle Fermin100% (2)
- Pathophysiology - Diabetes Mellitus Type 2Document3 pagesPathophysiology - Diabetes Mellitus Type 2Francis Kevin Sagudo100% (10)
- Pathophysiology of Hypertensive Cardiovascular Disease (HCVDDocument5 pagesPathophysiology of Hypertensive Cardiovascular Disease (HCVDNicolne Lorraine100% (1)
- Chronic Kidney Disease Pathophysiology - Schematic DiagramDocument3 pagesChronic Kidney Disease Pathophysiology - Schematic DiagramMeine MheineNo ratings yet
- Chronic Kidney Disease Pathophysiology Schematic DiagramDocument3 pagesChronic Kidney Disease Pathophysiology Schematic Diagramnursing concept maps100% (5)
- Acute Renal Failure PathoDocument4 pagesAcute Renal Failure PathoGlenn Asuncion Pagaduan100% (1)
- Pathophysiology of StrokeDocument2 pagesPathophysiology of StrokeACe JAy100% (2)
- Pathophysiology of Kidney DiseaseDocument3 pagesPathophysiology of Kidney DiseaseSTEPHANIE JOSUE100% (1)
- Pathophysiology Diagram of Congestive Heart FailureDocument3 pagesPathophysiology Diagram of Congestive Heart Failurea_samiane64% (11)
- CKDDocument3 pagesCKDMarc Lawrence Balderas CAra100% (1)
- CKD PathophysiologyDocument1 pageCKD Pathophysiologynursing concept mapsNo ratings yet
- Pathophysiology of Acute Renal FailureDocument2 pagesPathophysiology of Acute Renal Failurekristel_nicole18yaho100% (3)
- Pathophysiology of Diabetes Mellitus Type 2Document1 pagePathophysiology of Diabetes Mellitus Type 2faula rocamora100% (3)
- Pathophysiology of Diabetes Mellitus Type 2Document7 pagesPathophysiology of Diabetes Mellitus Type 2jnrue_aerith96% (28)
- Pathophysiology - ESRDDocument5 pagesPathophysiology - ESRDheiyu100% (3)
- CVA PathophysiologyDocument3 pagesCVA Pathophysiologyshmily_0810No ratings yet
- COPD PathophysiologyDocument1 pageCOPD Pathophysiologyaj ajNo ratings yet
- Pathophysiology CVDDocument1 pagePathophysiology CVDPamela Shiermaine FilomenoNo ratings yet
- Stroke PathophysiologyDocument2 pagesStroke PathophysiologyJaessa Feliciano100% (2)
- Pathophysiology CKDDocument1 pagePathophysiology CKDReymon Mary JanineNo ratings yet
- Pathophysiology ESRDDocument9 pagesPathophysiology ESRDJaye DangoNo ratings yet
- Pathophysiology of Cerebrovascular AccidentDocument2 pagesPathophysiology of Cerebrovascular AccidentJohn Michael FernandezNo ratings yet
- Angina Pectoris PathophysiologyDocument2 pagesAngina Pectoris Pathophysiologydana86% (7)
- Risk Factors and Pathophysiology of StrokeDocument4 pagesRisk Factors and Pathophysiology of StrokeSherlyn KirisakiNo ratings yet
- Congestive Heart Failure Schematic DiagramDocument1 pageCongestive Heart Failure Schematic DiagramCyrus De Asis100% (1)
- Hypertension Concept MapDocument1 pageHypertension Concept Mapnursing concept maps100% (1)
- Hypertension PathophysiologyDocument1 pageHypertension PathophysiologyLuis LedesmaNo ratings yet
- Chronic Kidney Disease Pathophysiology - Schematic DiagramDocument3 pagesChronic Kidney Disease Pathophysiology - Schematic DiagramJake CaballoNo ratings yet
- Pathophysiology of different Chronic Heart DiseasesDocument54 pagesPathophysiology of different Chronic Heart DiseasesMarissa AsimNo ratings yet
- Understanding Type 2 Diabetes: Fewer Highs, Fewer Lows, Better HealthFrom EverandUnderstanding Type 2 Diabetes: Fewer Highs, Fewer Lows, Better HealthNo ratings yet
- Diabetes: Glucose Monitoring and Insulin Treatment: The most important information you need to improve your healthFrom EverandDiabetes: Glucose Monitoring and Insulin Treatment: The most important information you need to improve your healthNo ratings yet
- The Best Life Guide to Managing Diabetes and Pre-DiabetesFrom EverandThe Best Life Guide to Managing Diabetes and Pre-DiabetesRating: 4 out of 5 stars4/5 (8)
- DASH Diet Weight Loss Motivation: A Foolproof Healthy Eating Solution To Easing The Symptoms of Hypertension And High Blood PressureFrom EverandDASH Diet Weight Loss Motivation: A Foolproof Healthy Eating Solution To Easing The Symptoms of Hypertension And High Blood PressureNo ratings yet
- The End of Diabetes: The Eat to Live Plan to Prevent and Reverse DiabetesFrom EverandThe End of Diabetes: The Eat to Live Plan to Prevent and Reverse DiabetesRating: 3.5 out of 5 stars3.5/5 (12)
- How Is Type 2 Diabetes Treated - What To Know If You Are Newly DiagnosedDocument2 pagesHow Is Type 2 Diabetes Treated - What To Know If You Are Newly DiagnosedRatnaPrasadNalamNo ratings yet
- Reverse Diabetes Forever Newly Updated: How to Shop, Cook, Eat and Live Well with DiabetesFrom EverandReverse Diabetes Forever Newly Updated: How to Shop, Cook, Eat and Live Well with DiabetesNo ratings yet
- Insulin Resistance Recipes: Simple and Delicious Recipes to Lower Your Blood Sugar and Reverse Insulin Resistance Naturally: Healthy CookingFrom EverandInsulin Resistance Recipes: Simple and Delicious Recipes to Lower Your Blood Sugar and Reverse Insulin Resistance Naturally: Healthy CookingNo ratings yet
- Ladies Weight Loss Programme: Are you fat and fed up of dieting?From EverandLadies Weight Loss Programme: Are you fat and fed up of dieting?No ratings yet
- Laboratory ResultsDocument1 pageLaboratory ResultsKaloy KamaoNo ratings yet
- Nursing Care PlansDocument2 pagesNursing Care PlansKaloy KamaoNo ratings yet
- ProQuestDocuments 2016-01-08Document7 pagesProQuestDocuments 2016-01-08Kaloy KamaoNo ratings yet
- Health TeachingsDocument1 pageHealth TeachingsKaloy KamaoNo ratings yet
- Penetrating Injuries To The Liver or Spleen - Care GuideDocument4 pagesPenetrating Injuries To The Liver or Spleen - Care GuideKaloy KamaoNo ratings yet
- Injury Severity ScoringDocument12 pagesInjury Severity ScoringJavier del MattoNo ratings yet
- Motorcycle Rider Risk ManagementDocument3 pagesMotorcycle Rider Risk ManagementKaloy KamaoNo ratings yet
- Location and Pictures of Different Organs in The AbdomenDocument13 pagesLocation and Pictures of Different Organs in The AbdomenKaloy KamaoNo ratings yet
- Paramedic Care: Principles & Practice Trauma EmergenciesDocument61 pagesParamedic Care: Principles & Practice Trauma EmergenciesKaloy KamaoNo ratings yet
- Motorcycle Rider Risk ManagementDocument3 pagesMotorcycle Rider Risk ManagementKaloy KamaoNo ratings yet
- Penetrating Injuries To The Liver or Spleen - Care GuideDocument4 pagesPenetrating Injuries To The Liver or Spleen - Care GuideKaloy KamaoNo ratings yet
- Pathophysiology 3Document10 pagesPathophysiology 3Kaloy KamaoNo ratings yet
- Location and Pictures of Different Organs in The AbdomenDocument13 pagesLocation and Pictures of Different Organs in The AbdomenKaloy KamaoNo ratings yet
- Doctor's Order SheetDocument2 pagesDoctor's Order SheetKaloy KamaoNo ratings yet
- Nursing Care PlansDocument2 pagesNursing Care PlansKaloy KamaoNo ratings yet
- IvtttDocument1 pageIvtttBobot Julius OropezaNo ratings yet
- Transverse Myelitis and Vaccines - A Multi-AnalysisDocument8 pagesTransverse Myelitis and Vaccines - A Multi-AnalysisKaloy KamaoNo ratings yet
- Health TeachingsDocument1 pageHealth TeachingsKaloy KamaoNo ratings yet
- Pain ManagementDocument19 pagesPain ManagementKaloy KamaoNo ratings yet
- Nutrition: Your Role in Promoting ProperDocument11 pagesNutrition: Your Role in Promoting ProperKaloy KamaoNo ratings yet
- Management of Hydrocephalus in Patients With Tuberculous MeningitisDocument11 pagesManagement of Hydrocephalus in Patients With Tuberculous MeningitisKaloy KamaoNo ratings yet
- Mapping The Literature of Public Health and Community NursingDocument4 pagesMapping The Literature of Public Health and Community NursingKaloy KamaoNo ratings yet
- Prevention CHN Ward ClassDocument2 pagesPrevention CHN Ward ClassKaloy KamaoNo ratings yet
- Group 2 Lesson Plan HandwashingDocument8 pagesGroup 2 Lesson Plan HandwashingKaloy KamaoNo ratings yet
- Management of Pain - Non-Pharmacological Management - Nursing Best Practice GuidelinesDocument2 pagesManagement of Pain - Non-Pharmacological Management - Nursing Best Practice GuidelinesKaloy KamaoNo ratings yet
- Nursing Management in The Local Public Health SystemDocument33 pagesNursing Management in The Local Public Health SystemKaloy KamaoNo ratings yet
- Management of Pain - Non-Pharmacological Management - Nursing Best Practice GuidelinesDocument2 pagesManagement of Pain - Non-Pharmacological Management - Nursing Best Practice GuidelinesKaloy KamaoNo ratings yet
- Occupational Nursing CHN Ward ClassDocument2 pagesOccupational Nursing CHN Ward ClassKaloy KamaoNo ratings yet
- Transverse MyelitisDocument7 pagesTransverse MyelitisKaloy KamaoNo ratings yet
- CHN Ward ClassDocument1 pageCHN Ward ClassKaloy KamaoNo ratings yet
- Improving Criminology Board PerformanceDocument14 pagesImproving Criminology Board PerformanceSharry CastilloNo ratings yet
- Q1-M1 Ans (Eapp)Document9 pagesQ1-M1 Ans (Eapp)JD MartinNo ratings yet
- 1 Hills Beyond A River James Cahill PDFDocument222 pages1 Hills Beyond A River James Cahill PDFLuis Lopez Sanchez100% (1)
- Good Psychiatric PracticeDocument42 pagesGood Psychiatric Practicecalvojm6786100% (1)
- SSC NR MTS, Havaldar Exam Admit Card 2022Document4 pagesSSC NR MTS, Havaldar Exam Admit Card 2022Ashish sangwanNo ratings yet
- Original Marks ListDocument291 pagesOriginal Marks ListFurqan WarisNo ratings yet
- Outside State Colleges Email DetailsDocument84 pagesOutside State Colleges Email Detailsuniquerealestate098No ratings yet
- APC Boosts Polypropylene OperationDocument6 pagesAPC Boosts Polypropylene OperationJuan AlejandroNo ratings yet
- Dr. Atanas Kirjakovski: Social PsychologyDocument33 pagesDr. Atanas Kirjakovski: Social PsychologyAlmirMuratiNo ratings yet
- Student Motivation: Unit - 3Document36 pagesStudent Motivation: Unit - 3RubeenaNo ratings yet
- Tutorial Letter 103/0/2020 Teaching Practice For Intermediate Phase (Grades 4-6) Assignment 50 Year Module Department of Curriculum and Instructional StudiesDocument94 pagesTutorial Letter 103/0/2020 Teaching Practice For Intermediate Phase (Grades 4-6) Assignment 50 Year Module Department of Curriculum and Instructional StudiesMandisaNo ratings yet
- Buwan NG Kasaysayan: Contest Criteria Date & Time Venue Participants Materials JudgeDocument1 pageBuwan NG Kasaysayan: Contest Criteria Date & Time Venue Participants Materials JudgeJireh Alido FlavioNo ratings yet
- Handouts IT of Education CompleteDocument523 pagesHandouts IT of Education CompleteNamtu LewanyNo ratings yet
- Chapter 8 - Nervous SystemDocument12 pagesChapter 8 - Nervous SystemlalaNo ratings yet
- Dr. Sarbari Guha Physics ProfileDocument5 pagesDr. Sarbari Guha Physics Profilevishwas gaurNo ratings yet
- Curriculum Vitae: To: Crewing Manager Subject: Deck Cadet Application Dear Sir or MadamDocument1 pageCurriculum Vitae: To: Crewing Manager Subject: Deck Cadet Application Dear Sir or MadamWiwit PrihatiniNo ratings yet
- Department of Education Region III Division of Pampanga Basa Air Base National High School Floridablanca, Pampanga S.Y. 2019 - 2020Document2 pagesDepartment of Education Region III Division of Pampanga Basa Air Base National High School Floridablanca, Pampanga S.Y. 2019 - 2020Edita AquinoNo ratings yet
- Investigating Elective Courses in Architectural Education: Frontiers of Architectural ResearchDocument22 pagesInvestigating Elective Courses in Architectural Education: Frontiers of Architectural ResearchPuñith SadashivaNo ratings yet
- Cognitve TheoryDocument8 pagesCognitve Theorymanu sethiNo ratings yet
- NSTP-CWTS GraduationDocument4 pagesNSTP-CWTS GraduationAngie Esponilla100% (1)
- Qslides 02 Design ProcessDocument47 pagesQslides 02 Design ProcessNathan HahnNo ratings yet
- PDF 36Document3 pagesPDF 36Armia GaberNo ratings yet
- Howe - Music DisabilityDocument9 pagesHowe - Music DisabilityfdjaklfdjkaNo ratings yet
- Selection 6th 5 in 1 EM Term - 1Document64 pagesSelection 6th 5 in 1 EM Term - 1Jeeva BharathiNo ratings yet
- DNA Molecule & Central DogmaDocument43 pagesDNA Molecule & Central DogmaJoanna Ruth SeproNo ratings yet
- Genalyn Puno Cordez Resume for IT Administration PositionDocument4 pagesGenalyn Puno Cordez Resume for IT Administration PositionJay Mark Albis SantosNo ratings yet
- George ResumeDocument3 pagesGeorge Resumeapi-287298572No ratings yet
- TOEFL STRATEGIES Structure and Written ExpressionDocument6 pagesTOEFL STRATEGIES Structure and Written ExpressionTaufand K. ImamNo ratings yet
- Improve Group Project PerformanceDocument15 pagesImprove Group Project PerformanceВаля БоберськаNo ratings yet
- Using Historical Thinking to Teach GovernmentsDocument2 pagesUsing Historical Thinking to Teach GovernmentsSneha MishraNo ratings yet