Professional Documents
Culture Documents
Falls Risk Asssessmnet (FRAT)
Uploaded by
Livgian Kaur0 ratings0% found this document useful (0 votes)
224 views3 pagesFalls risk assessment for the falls prevention in the elderly
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentFalls risk assessment for the falls prevention in the elderly
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
224 views3 pagesFalls Risk Asssessmnet (FRAT)
Uploaded by
Livgian KaurFalls risk assessment for the falls prevention in the elderly
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
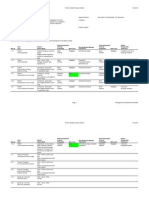
Department of Health
Falls Risk Assessment Tool (FRAT)
Developed by: Peninsula Health
Format: Assessment tool and Instructions for use
Availability: Download FRAT <PDF version> <Word version>
Download Instructions for use <PDF version> <Word version>
The Falls Risk Assessment Tool (FRAT) was developed by the Peninsula Health Falls Prevention
Service for a DH funded project in 1999, and is part of the FRAT Pack. A study evaluating the
reliability and validity of the FRAT has been published (Stapleton C, Hough P, Bull K, Hill K,
Greenwood K, Oldmeadow L (2009). A 4-item falls-risk screening tool for sub-acute and
residential care: The first step in falls prevention. Australasian Journal on Ageing 28(3): 139-143).
The FRAT has been distributed to approximately 400 agencies world wide.
The FRAT has three sections: Part 1 - falls risk status; Part 2 risk factor checklist; and Part 3
action plan. The complete tool (including instructions for use) is a complete falls risk assessment
tool. However, Part 1 can be used as a falls risk screen. An abbreviated version of the instructions
for use has been included on this website. For a complete copy of the instructions for use please
refer to the FRAT Pack or contact the Peninsula Health Falls Prevention Service, telephone (61 3)
9788 1260.
The FRAT is a validated tool, therefore changes to Part 1 of the tool are not recommended.
Please note: The cognitive status question in Part 1 on the FRAT refers to the Abbreviated Mental
Test Score (AMTS). This resource is available at
http://anzsgm.org/vgmtp/Dementia/cognitive_screening_tests.htm (please note: this will take
you out of the Department of Health website).
In 2009 the Department of Health funded Northern Health, in conjunction with National Ageing Research
Institute, to review falls prevention resources for the Department of Healths website. The materials used as
the basis of this generic resource were developed by Peninsula Health under a Service Agreement with the
Department of Human Services, now the Department of Health. Other resources to maintain health and
wellbeing of older people are available from www.health.vic.gov.au/agedcare
Working together to prevent falls
FALLS RISK
ASSESSMENT TOOL
(FRAT)
UR NUMBER .
SURNAME
GIVEN NAMES.
DATE OF BIRTH .
Please fill in if no patient/resident label available
(see instructions for completion of FRAT in the FRAT PACK-Falls Resource Manual)
PART 1: FALL RISK STATUS
RISK FACTOR LEVEL RISK SCORE
RECENT FALLS none in last 12 months 2
one or more between 3 and 12 months ago. 4
one or more in last 3 months. 6
(To score this, complete history of
falls, overleaf)
one or more in last 3 months whilst inpatient / resident. 8
MEDICATIONS not taking any of these 1
(Sedatives, Anti-Depressants
taking one . 2
Anti-Parkinsons, Diuretics
taking two . 3
Anti-hypertensives, hypnotics)
taking more than two.. 4
PSYCHOLOGICAL does not appear to have any of these.. 1
(Anxiety, Depression
appears mildly affected by one or more... 2
Cooperation, Insight or
appears moderately affected by one or more. 3
Judgement esp. re mobility )
appears severely affected by one or more.. 4
COGNITIVE STATUS AMTS 9 or 10 / 10 OR intact.. 1
AMTS 7-8 mildly impaired.. 2
(AMTS: Hodkinson Abbreviated AMTS 5-6 mod impaired... 3
Mental Test Score) AMTS 4 or less severely impaired ... 4
(Low Risk: 5-11 Medium: Risk: 12-15 High Risk: 16-20) RISK SCORE
/20
Automatic High Risk Status: (if ticked then circle HIGH risk below)
Recent change in functional status and / or medications affecting safe mobility (or anticipated)
Dizziness / postural hypotension
FALL RISK STATUS: (Circle ): LOW / MEDIUM / HIGH
List Fall Status on Care
Plan/ Flow Chart
IMPORTANT: IF HIGH, COMMENCE FALL ALERT
PART 2: RISK FACTOR CHECKLIST
Y/N
Vision Reports / observed difficulty seeing - objects / signs / finding way around
Mobility Mobility status unknown or appears unsafe / impulsive / forgets gait aid
Transfers Transfer status unknown or appears unsafe ie. over-reaches, impulsive
Behaviours Observed or reported agitation, confusion, disorientation
Difficulty following instructions or non-compliant (observed or known)
Observed risk-taking behaviours, or reported from referrer / previous facility
Observed unsafe use of equipment
Activities of
Daily Living
(A.D.Ls)
Unsafe footwear / inappropriate clothing
Environment Difficulties with orientation to environment i.e. areas between bed / bathroom / dining
room
Nutrition Underweight / low appetite
Continence Reported or known urgency / nocturia / accidents
Other
Part 2 Continued
HISTORY OF FALLS Note: For an accurate history, consult patient/resident / family / medical records.
Falls prior to this admission (home or referring facility) and/or during current stay
If ticked, detail most recent below)
CIRCUMSTANCES OF RECENT FALLS: Information obtained from____________________________
(Circle below) ( Where? / Comments)
Last fall: Time ago _____ Trip Slip Lost balance Collapse Leg/s gave way Dizziness ______________________
Previous: Time ago _____ Trip Slip Lost balance Collapse Leg/s gave way Dizziness ______________________
Previous: Time ago _____ Trip Slip Lost balance Collapse Leg/s gave way Dizziness ______________________
List History of Falls on Alert Sheet in Patient/Resident Record
PART 3: ACTION PLAN
(for Risk factors identified in Part 1 & 2, list strategies below to manage falls risk. See tips in FRAT PACK)
PROBLEM LIST INTERVENTION STRATEGIES / REFERRALS
Transfer care strategies to Care Plan / Flow Chart
PLANNED REVIEW ________________________________ Date of Assessment:__________________________
INITIAL ASSESSMENT COMPLETED BY:
PRINT NAME __________________________________________ Signed: ______________________________
REVIEW
(Falls Review should occur at scheduled Patient/Resident Review meetings or at intervals set by the Initial assessor)
Review
Date
Risk
Status
Revised Care plan
(Y or N)
Signed Review
Date
Risk
Status
Revised Care plan
(Y or N)
Signed
You might also like
- FRATDocument3 pagesFRATNigel LimNo ratings yet
- Treatment Protocols 2016Document209 pagesTreatment Protocols 2016NanaNo ratings yet
- Emergency Medical Services Pre Hospital Treatment Protocols Version 2019 2 Effective 100119Document231 pagesEmergency Medical Services Pre Hospital Treatment Protocols Version 2019 2 Effective 100119Kyle ChenNo ratings yet
- Hazard_Near_Miss_ReportDocument1 pageHazard_Near_Miss_ReportvNo ratings yet
- Standardised Categories and Indicators For Better Cmam Reporting Final Apr 2015Document44 pagesStandardised Categories and Indicators For Better Cmam Reporting Final Apr 2015Md. Rafiqul IslamNo ratings yet
- Capacity Development Needs Assessment QuestionnaireDocument12 pagesCapacity Development Needs Assessment QuestionnaireAndres OrtizNo ratings yet
- 2015 Trauma ManualDocument165 pages2015 Trauma ManualLunaPerfectNo ratings yet
- Hira 2014 08 20 PDFDocument24 pagesHira 2014 08 20 PDFSADHEDNo ratings yet
- Perfilestoxicologicos PDFDocument666 pagesPerfilestoxicologicos PDFHector GonzalezNo ratings yet
- Statistical Analysis On Risk Factors of Prevalence of Malaria in Z/ Dugda Woreda, Oromia, East ArsiDocument31 pagesStatistical Analysis On Risk Factors of Prevalence of Malaria in Z/ Dugda Woreda, Oromia, East Arsitewodrosmolalign19No ratings yet
- First Aid CPR AedDocument196 pagesFirst Aid CPR AedMW100% (1)
- Practical Guide to School Crisis PlanningDocument132 pagesPractical Guide to School Crisis PlanningAnemoessaNo ratings yet
- Iraqi Injury Surveillance System Annual Report 2013Document46 pagesIraqi Injury Surveillance System Annual Report 2013bejarhasanNo ratings yet
- EFR Participant Manual Mobile PDFDocument118 pagesEFR Participant Manual Mobile PDFAnonymous xpo7HAI100% (4)
- Medical Support Manual For UN Field Missions PDFDocument264 pagesMedical Support Manual For UN Field Missions PDFNadia100% (2)
- Missing Persons Policy SummaryDocument16 pagesMissing Persons Policy SummaryAgnieszka WaligóraNo ratings yet
- Public Health Assessment Guidance Manual UpdateDocument357 pagesPublic Health Assessment Guidance Manual UpdateAbhishek SahuNo ratings yet
- Slip, Trip, and Fall PreventionDocument56 pagesSlip, Trip, and Fall PreventionSagar TannaNo ratings yet
- Chemical Risk AssessmentDocument105 pagesChemical Risk AssessmentRaquel LopesNo ratings yet
- Reporting TemplateDocument10 pagesReporting TemplateVety OctavianyNo ratings yet
- Reporting Template: Introduction and ObjectivesDocument10 pagesReporting Template: Introduction and ObjectivesAJ SaNo ratings yet
- Health and Health Related Indicators 2013 EFYDocument61 pagesHealth and Health Related Indicators 2013 EFYRedietNo ratings yet
- 2BmfnjfGbam9JF6f-EFS20Kit 1.7Document15 pages2BmfnjfGbam9JF6f-EFS20Kit 1.7Ismail ZeroualNo ratings yet
- Camera BookingDocument7 pagesCamera Bookingapi-279869444No ratings yet
- Encyclopedia BD Income-Associated BDDocument15 pagesEncyclopedia BD Income-Associated BDPeter MuennigNo ratings yet
- Agenda CHMP Agenda 8 11 November 2021 Meeting - enDocument107 pagesAgenda CHMP Agenda 8 11 November 2021 Meeting - enntktkinqNo ratings yet
- Health Sector Emergency Preparedness Guide: Making A Difference To VulnerabilityDocument77 pagesHealth Sector Emergency Preparedness Guide: Making A Difference To Vulnerabilitymanique_abeyrat2469No ratings yet
- Merlin WASH GuideDocument24 pagesMerlin WASH Guideash amenNo ratings yet
- 02 DisasterDocument32 pages02 DisasterRezzaCaturKurniawanNo ratings yet
- Guidance Off-The-Shelf Software UseDocument29 pagesGuidance Off-The-Shelf Software UseNeil RaNo ratings yet
- Hospital Safety Index Forms PDFDocument46 pagesHospital Safety Index Forms PDFAnnisa Aisyha MalikNo ratings yet
- Evaluation Forms EngDocument46 pagesEvaluation Forms EngVera RodessaNo ratings yet
- Psad Design Safe ReportDocument2 pagesPsad Design Safe Reportapi-237578058No ratings yet
- Working Group Report On Sea LiceDocument117 pagesWorking Group Report On Sea LiceJon Arne GrøttumNo ratings yet
- Admissions Medical ApplicationDocument2 pagesAdmissions Medical ApplicationkesnaNo ratings yet
- Admissions Medical ApplicationDocument2 pagesAdmissions Medical ApplicationDajueNo ratings yet
- Risk Register Guidance Feb 2013 2Document40 pagesRisk Register Guidance Feb 2013 2SOPHIA-VNo ratings yet
- PAHO - Medium and Small Hospitals - Safety IndexDocument153 pagesPAHO - Medium and Small Hospitals - Safety IndexMiguelNo ratings yet
- Health, Education, Social Protection News & Notes 24/2009Document33 pagesHealth, Education, Social Protection News & Notes 24/2009Dieter NeuviansNo ratings yet
- Risk Prevention and Management Plan Emergency Response ROCK CLIMBINGDocument10 pagesRisk Prevention and Management Plan Emergency Response ROCK CLIMBINGFarooq AzizNo ratings yet
- First Aid CPR AED PDFDocument196 pagesFirst Aid CPR AED PDFwienslaw5804100% (1)
- Epilepsy in African-RegionDocument56 pagesEpilepsy in African-RegionJaiye WeissNo ratings yet
- ARC CPR/AED Health Emergencies and First Aid HandbookDocument196 pagesARC CPR/AED Health Emergencies and First Aid HandbookRaabia Ansari100% (2)
- Health SystemsDocument167 pagesHealth SystemsSimran AroraNo ratings yet
- Apple: Uc Ipm Pest Management GuidelinesDocument74 pagesApple: Uc Ipm Pest Management Guidelinesusama_yasinNo ratings yet
- 6 Tratamiento Del RiesgoDocument15 pages6 Tratamiento Del RiesgoIVAN OVIEDONo ratings yet
- Camera BookingDocument8 pagesCamera Bookingapi-279869444No ratings yet
- Risk Assessment For DummiesDocument26 pagesRisk Assessment For Dummiessorayatamara100% (1)
- Communicable Disease SudanDocument130 pagesCommunicable Disease Sudansida200100% (1)
- PTSD On MilitaryDocument19 pagesPTSD On Militaryayu yuliantiNo ratings yet
- Pok Ped ChildrenDocument34 pagesPok Ped Childrensarfu_sk2005No ratings yet
- Cost Benefits PreventionDocument60 pagesCost Benefits PreventionRaluka KalinovićNo ratings yet
- Statewide Treatment Protocols V 2023-2-5!4!2023Document175 pagesStatewide Treatment Protocols V 2023-2-5!4!2023Robert MccallumNo ratings yet
- Family Support Planning Guide 2011Document29 pagesFamily Support Planning Guide 2011amcpherson9226No ratings yet
- Indonesia HRNA Main Text 28oct09Document52 pagesIndonesia HRNA Main Text 28oct09AnamtaNo ratings yet
- Health, Education, Social Protection News & Notes 12/2010Document30 pagesHealth, Education, Social Protection News & Notes 12/2010Dieter NeuviansNo ratings yet
- Technical Guidelines on Rapid Risk Assessment for Animal Health ThreatsFrom EverandTechnical Guidelines on Rapid Risk Assessment for Animal Health ThreatsNo ratings yet
- Fisheries Emergency Rapid Assessment Tool (FERAT)From EverandFisheries Emergency Rapid Assessment Tool (FERAT)No ratings yet
- Manual for the Management of Operations during an Animal Health EmergencyFrom EverandManual for the Management of Operations during an Animal Health EmergencyNo ratings yet
- Act in a Split Second - First Aid Manual of the US Army: Learn the Crucial First Aid Procedures With Clear Explanations & Instructive Images: How to Stop the Bleeding & Protect the Wound, Perform Mouth-to-Mouth, Immobilize Fractures, Treat Bites and Stings…From EverandAct in a Split Second - First Aid Manual of the US Army: Learn the Crucial First Aid Procedures With Clear Explanations & Instructive Images: How to Stop the Bleeding & Protect the Wound, Perform Mouth-to-Mouth, Immobilize Fractures, Treat Bites and Stings…No ratings yet
- PATOFLOWSTROKEDocument2 pagesPATOFLOWSTROKEBabyna Mozez Iiaa ReztieNo ratings yet
- Tabel Silang Hubungan Karakteristik Pasien Dengan Tingkat Kepuasan Pelayanan KeperawatanDocument3 pagesTabel Silang Hubungan Karakteristik Pasien Dengan Tingkat Kepuasan Pelayanan KeperawatanBabyna Mozez Iiaa ReztieNo ratings yet
- Abdominal TraumaDocument6 pagesAbdominal TraumaBabyna Mozez Iiaa ReztieNo ratings yet
- Effect of Low Impact Aerobic Exercise Therapy on Aggression Self-Control ScoresDocument11 pagesEffect of Low Impact Aerobic Exercise Therapy on Aggression Self-Control ScoresBabyna Mozez Iiaa ReztieNo ratings yet
- Effect of Low Impact Aerobic Exercise Therapy on Aggression Self-Control ScoresDocument11 pagesEffect of Low Impact Aerobic Exercise Therapy on Aggression Self-Control ScoresBabyna Mozez Iiaa ReztieNo ratings yet