Professional Documents
Culture Documents
Confidence Intervals
Uploaded by
Candice Cheng0 ratings0% found this document useful (0 votes)
88 views9 pagesConfidence Intervals Guide
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentConfidence Intervals Guide
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
88 views9 pagesConfidence Intervals
Uploaded by
Candice ChengConfidence Intervals Guide
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 9
G A confidence interval calculated for a measure of treatment
effect shows a range within which the true treatment effect is
likely to lie.
G Confidence intervals are preferable to p-values, as they tell us the
range of possible effect sizes compatible with the data.
G A confidence interval that embraces the value of no
difference indicates that the treatment under investigation is not
significantly different from the control.
G Confidence intervals aid interpretation of clinical trial
data by putting upper and lower bounds on the likely size of
any true effect.
G Bias must be assessed before confidence intervals can be
interpreted. Even very large samples and very narrow confidence
intervals can mislead if they come from biased studies.
G Non-significance does not mean no effect. Small studies
will often report non-significance even when there are important,
real effects.
G Statistical significance does not necessarily mean that the effect is
real: by chance alone about one in 20 significant findings will
be spurious.
G Statistical significance does not necessarily mean clinically
important. It is the size of the effect that determines the
importance, not the presence of statistical significance.
1
Volume 3, number 1
www.evidence-based-medicine.co.uk
Sponsored by an educational grant from AVENTIS Pharma
What are
confidence
intervals?
Huw T O Davies
MA, MSc, PhD,
HonMFPHM
Reader in Health
Care Policy and
Management,
University of
St Andrews
Prescribing information is on page 8
2
What are
confidence intervals?
Measuring effect size
Clinical trials aim to generate new
knowledge on the effectiveness (or
otherwise) of healthcare
interventions. Like all clinical
research, this involves estimating a
key parameter of interest, in this case
the effect size. The effect size can be
measured in a variety of ways, such as
the relative risk reduction, the
absolute risk reduction or the number
needed to treat (NNT) (Table 1).
Relative measures tend to
emphasise potential benefits, whereas
absolute measures provide an
across-the-board summary.
1
Either
may be appropriate, subject to correct
interpretation.
Whatever the measure used, some
assessment must be made of the
trustworthiness or robustness of the
findings. The findings of the study provide a
point estimate of effect, and this raises a
dilemma: are the findings discovered about
the sample also likely to be true about other
similar groups of patients? Before we can
answer such a question, two issues need to be
addressed. Does any apparent treatment
benefit arise because of the way the study has
been conducted (bias), or could it arise
simply because of chance? The short note
below briefly covers the importance of
assessing bias but focuses more on assessing
the role of chance.
What are confidence intervals?
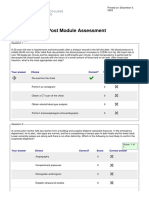
Measure of effect Abbreviation Description No effect Total success
Absolute risk ARR Absolute change in risk: the risk ARR=0% ARR=initial risk
reduction of an event in the control group
minus the risk of an event in the
treated group; usually expressed
as a percentage
Relative risk RRR Proportion of the risk removed RRR=0% RRR=100%
reduction by treatment: the absolute risk
reduction divided by the initial
risk in the control group; usually
expressed as a percentage
Relative risk RR The risk of an event in the treated RR=1 or RR=0
group divided by the risk of an event RR=100%
in the control group; usually expressed
as a decimal proportion, sometimes as
a percentage
Odds ratio OR Odds of an event in the treated group OR=1 OR=0
divided by the odds of an event in the
control group; usually expressed as a
decimal proportion
Number needed NNT Number of patients who need to be NNT= NNT=1/initial risk
to treat treated to prevent one event; this is the
reciprocal of the absolute risk reduction
(when expressed as a decimal fraction);
it is usually rounded to a whole number
Table 1: Summary of effect measures
3
What are
confidence intervals?
Bias
Bias is a term that covers any systematic
errors in the way the study was designed,
executed or interpreted. Common flaws in
treatment trials are: lack of (or failure in)
randomisation, leading to unbalanced
groups; poor blinding, leading to unfair
treatment and biased assessments; and large
numbers of patients lost to follow-up.
Assessment in these areas is crucial before
the results from any trial can be assessed,
and many useful guides exist to assist this
process.
25
Interpretation of the effects of
chance is only meaningful once bias has
been excluded as an explanation for any
observed differences.
6,7
Chance variability
Until comparatively recently, assessments of
the role of chance were routinely made using
hypothesis testing, which produces a p-
value (Box 1). The p-value allows assessment
of whether or not the findings are
significantly different or not significantly
different from some reference value (in trials,
this is usually the value reflecting no effect;
see Table 1). More recently, a different and
more useful approach to assessing the role of
chance has come to the fore: confidence
intervals.
8
Although these might appear
rather dissimilar to p-values, the theory and
calculations underlying these two approaches
are largely the same.
What are confidence
intervals?
Confidence intervals provide different
information from that arising from
hypothesis tests. Hypothesis testing
produces a decision about any observed
difference: either that the difference is
statistically significant or that it is
statistically non-significant. In contrast,
Box 1: Hypothesis testing and the generation of p-values
The logic of hypothesis testing and p-values is convoluted. Suppose a new treatment appears to
outperform the standard therapy in a research study. We are interested in assessing whether this
apparent effect is likely to be real or could just be a chance finding: p-values help us to do this.
In calculating the p-value, we first assume that there really is no true difference between the
two treatments (this is called the null hypothesis). We then calculate how likely we are to see
the difference that we have observed just by chance if our supposition is true (that is, if there is
really no true difference). This is the p-value.
So the p-value is the probability that we would observe effects as big as those seen in the
study if there was really no difference between the treatments. If p is small, the findings are
unlikely to have arisen by chance and we reject the idea that there is no difference between the
two treatments (we reject the null hypothesis). If p is large, the observed difference is plausibly a
chance finding and we do not reject the idea that there is no difference between the treatments.
Note that we do not reject the idea, but we do not accept it either: we are simply unable to say
one way or another until other factors have been considered.
But what do we mean by a small p-value (one small enough to cause us to reject the idea
that there was really no difference)? By convention, p-values of less than 0.05 are considered
small. That is, if p is less than 0.05 there is a less than one in 20 chance that a difference as big
as that seen in the study could have arisen by chance if there was really no true difference. With
p-values this small (or smaller) we say that the results from the trial are statistically significant
(unlikely to have arisen by chance). Smaller p-values (say p<0.01) are sometimes called highly
significant because they indicate that the observed difference would happen less than once in a
hundred times if there was really no true difference.
4
What are
confidence intervals?
confidence intervals provide a range about
the observed effect size. This range is
constructed in such a way that we know how
likely it is to capture the true but unknown
effect size.
Thus the formal definition of a confidence
interval is: a range of values for a variable of
interest [in our case, the measure of treatment
effect] constructed so that this range has a
specified probability of including the true
value of the variable. The specified
probability is called the confidence level, and
the end points of the confidence interval are
called the confidence limits.
9
It is a widespread convention to create
confidence intervals at the 95% level so
this means that 95% of the time properly
constructed confidence intervals should
contain the true value of the variable
of interest.
Hence, more colloquially, the confidence
interval provides a range for our estimate
of the true treatment effect that is
plausible given the size of the difference
actually observed.
Assessing significance
from a confidence interval
One useful feature of confidence intervals is
that one can easily tell whether or not
statistical significance has been reached, just
as in a hypothesis test.
G If the confidence interval captures the
value reflecting no effect, this represents
a difference that is statistically
non-significant (for a 95% confidence
interval, this is non-significance at the
5% level).
G If the confidence interval does not
enclose the value reflecting no effect,
this represents a difference that is
statistically significant (again, for a 95%
confidence interval, this is significance at
the 5% level).
Thus statistical significance can be
inferred from confidence intervals but,
in addition, these intervals show the
largest and smallest effects that are likely
given the observed data. This is useful
extra information.
An example of the use of confidence
intervals is shown in Box 2.
Examining the width of a
confidence interval
One of the advantages of confidence intervals
over traditional hypothesis testing is the
additional information that they convey. The
upper and lower bounds of the interval give
us information on how big or small the true
effect might plausibly be, and the width of
the confidence interval also conveys some
useful information.
If the confidence interval is narrow,
capturing only a small range of effect sizes, we
can be quite confident that any effects far
from this range have been ruled out by the
study. This situation usually arises when the
size of the study is quite large and hence the
estimate of the true effect is quite precise.
Another way of saying this is to note that
the study has reasonable power to detect
an effect.
However, if the confidence interval is
quite wide, capturing a diverse range of
effect sizes, we can infer that the study was
probably quite small. Thus any estimates of
effect size will be quite imprecise. Such a
study is low powered and provides us with
less information.
Errors in interpretation
Confidence intervals, like p-values, provide us
with a guide to help with the interpretation
of research findings in the light of the effects
of chance. There are, however, three
important pitfalls in interpretation.
Getting it wrong: seeing effects that
are not real
First of all, we may examine the confidence
interval and observe that the difference is
statistically significant. From this we will
usually conclude that there is a difference
between the two treatments. However, just
because we are unlikely to observe such a
large difference simply by chance, this does
not mean that it will not happen. By
definition, about one in 20 significant
findings will be spurious arising simply
from chance. Thus we may be misled by
chance into believing in something that
is not real technically, this is called a
type I error.
5
What are
confidence intervals?
Box 2: An example of the use of confidence intervals
Ramipril is an angiotensin-converting enzyme (ACE) inhibitor which has been tested for use
in patients at high risk of cardiovascular events. In one study published in the New England
Journal of Medicine,
10
a total of 9,297 patients were recruited into a randomised,
double-blind, controlled trial. The key findings presented on the primary outcome and deaths
were as follows:
Incidence of primary outcome and deaths from any cause
Outcome Ramipril group Placebo group Relative risk
(n=4,645) (n=4,652) (95% CI)
number (%) number (%)
Cardiovascular event 651 (14.0) 826 (17.8) 0.78
(including death) (0.700.86)
Death from 200 (4.3) 192 (4.1) 1.03
non-cardiovascular cause (0.851.26)
Death from any cause 482 (10.4) 569 (12.2) 0.84
(0.750.95)
These data indicate that fewer people treated with ramipril suffered a cardiovascular
event (14.0%) compared with those in the placebo group (17.8%). This gives a relative
risk of 0.78, or a reduction in (relative) risk of 22%. The 95% confidence interval for this
estimate of the relative risk runs from 0.70 to 0.86. Two observations can then be made from
this confidence interval:
G First, the observed difference is statistically significant at the 5% level, because the interval
does not embrace a relative risk of one.
G Second, the observed data are consistent with as much as a 30% reduction in relative risk or
as little as a 14% reduction in risk.
Similarly, the last row of the table shows that statistically significant reductions in the
overall death rate were recorded: a relative risk of 0.84 with a confidence interval running
from 0.75 to 0.95. Thus the true reduction in deaths may be as much as a quarter or it could
be only as little as 5%; however, we are 95% certain that the overall death rate is reduced in
the ramipril group.
Finally, exploring the data presented in the middle row shows an example of how a
confidence interval can demonstrate non-significance. There were a few more deaths
from non-cardiovascular causes in the ramipril group (200) compared with the placebo group
(192). Because of this, the relative risk is calculated to be 1.03 showing a slight increase in risk
in the ramipril group. However, the confidence interval is seen to capture the value of no effect
(relative risk = 1), running as it does from 0.85 to 1.26. The observed difference is thus non-
significant; the true value could be anything from a 15% reduction in non-cardiovascular deaths
for ramipril to a 26% increase in these deaths. Not only do we know that the result is not
significant, but we can also see how large or small a true difference might plausibly be, given
these data.
6
What are
confidence intervals?
It is a frustrating but unavoidable feature
of statistical significance (whether assessed
using confidence intervals or p-values) that
around one in 20 will mislead. Yet we cannot
know which of any given set of comparisons
is doing the misleading. This observation
cautions against generating too many
statistical comparisons: the more
comparisons made in any given study the
greater the chance that at least some of them
will be spurious findings. Thus clinical trials
which show significance in only one or two
subgroups are unconvincing such
significance may be deceptive. Unless
particular subgroup analyses have been
specified in advance, differences other than
for the primary endpoint for the whole group
should be viewed with suspicion.
Statistical significance and clinical
significance
Statistical significance is also sometimes
misinterpreted as signifying an important
result: this is a second important pitfall in
interpretation. Significance testing simply
asks whether the data produced in a study are
compatible with the notion of no difference
between the new and control interventions.
Rejecting equivalence of the two
interventions does not necessarily mean that
we accept that there is an important
difference between them. A large study
may identify as statistically significant a
fairly small difference. It is then quite a
separate judgement to assess the clinical
significance of this difference. In assessing
the importance of significant results, it is the
size of the effect not just the size of the
significance that matters.
Getting it wrong again: failing to
find real effects
A further error that we may make is to
conclude from a non-significant finding that
there is no effect, when in fact there is this
is called a type II error. Equating non-
significance with no effect is a frequent and
damaging misconception. A non-significant
confidence interval simply tells us that the
observed difference is consistent with there
being no true difference between the two
groups. Thus we are unable to reject this
possibility. This is where confidence intervals
are much more helpful than simple p-values:
the observed difference will also be
compatible with a range of other effect sizes
as described by the confidence interval.
8
We
are unable to reject these possibilities either
and must then assess whether some of these
possibilities might be important. Just because
we have not found a significant treatment
effect does not mean that there is no
treatment effect to be found.
11
The crucial
question is how hard have we looked?.
Extrapolating beyond
the trial
For all the complexity of understanding bias
and chance in the interpretation of the
findings from clinical trials, another
important consideration should not be
forgotten. The findings from any given study
relate to the patients included in that study.
Even if an effect is assessed as probably real
and large enough to be clinically important, a
further question remains: how well are the
findings applicable to other groups of
patients, and do they particularise to a given
individual?
12
Neither confidence intervals nor
p-values are much help with this judgement.
Assessment of this external validity is made
based on the patients characteristics and on
the setting and the conduct of the trial.
Summary
Confidence intervals take as their starting
point the results observed in a study.
Crucially, we must check first that this is an
unbiased study. The question they then
answer is what is the range of real effects that
are compatible with these data?. The
confidence interval is just such a range, which
95% of the time will contain the true value of
the main measure of effect (relative risk
reduction, absolute risk reduction, NNT or
whatever; Table 1).
This allows us to do two things. First, if the
confidence interval embraces the value of no
effect (for example, no difference between
two treatments as shown by a relative risk
equal to one or an absolute difference equal
to zero) then the findings are non-significant.
If the confidence interval does not embrace
the value of no difference then the findings
7
What are
confidence intervals?
are statistically significant. Thus confidence
intervals provide the same information as a
p-value. But more than this: the upper and
lower extremities of the confidence interval
also tell us how large or small the real effect
might be and yet still give us the observed
findings by chance. This additional
information is very helpful in allowing us to
interpret both borderline significance and
non-significance. Confidence intervals from
large studies tend to be quite narrow in width,
showing the precision with which the study is
able to estimate the size of any real effect. In
contrast, confidence intervals from smaller
studies are usually wide, showing that the
findings are compatible with a wide range of
effect sizes.
References
1. Davies HTO. Interpreting measures of treatment effect.
Hosp Med 1998; 59: 499501.
2. Guyatt GH, Sackett DL, Cook DJ. Users guides to the
medical literature. II. How to use an article about therapy
or prevention. A. Are the results of the study valid? JAMA
1993; 270: 25982601.
3. Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical
epidemiology: A basic science for clinical medicine. 2nd edn.
Boston, Massachusetts: Little, Brown and Company, 1991.
4. Sackett DL, Richardson WS, Rosenberg W, Haynes RB.
Evidence based medicine: how to practice and teach EBM.
London: Churchill Livingstone, 1997.
5. Crombie IK. The pocket guide to critical appraisal.
London: BMJ Publishing, 1996.
6. Brennan P, Croft P. Interpreting the results of
observational research: chance is not such a fine thing.
BMJ 1994; 309: 727730.
7. Hill A, Spittlehouse C. What is critical appraisal? London:
Hayward Medical Communications, 2000 (in press).
8. Gardner MJ, Altman DG. Confidence intervals rather
than p values: estimation rather than hypothesis testing.
BMJ 1986; 292: 746750.
9. Last JM. A dictionary of epidemiology. Oxford:
International Journal of Epidemiology, 1988.
10. The Heart Outcomes Prevention Evaluation Study
Investigators. Effects of an angiotensin-converting-
enzyme inhibitor, ramipril, on cardiovascular events in
high-risk patients. N Engl J Med 2000; 342: 145153.
11. Altman DG, Bland JM. Absence of evidence is not
evidence of absence. BMJ 1995; 311: 485.
12. Guyatt GH, Sackett DL, Cook DJ. Users guides to the
medical literature. II. How to use an article about therapy
or prevention. B. What were the results and will they help
me in caring for my patients? JAMA 1994; 271: 5963.
Sponsored by an educational grant from
AVENTIS Pharma
What are
confidence intervals?
Published by Hayward Medical
Communications, a division of
Hayward Group plc.
Copyright 2001 Hayward
Group plc.
All rights reserved.
Volume 3, number 1
8
This publication, along with the others in the
series, is available on the internet at
www.evidence-based-medicine.co.uk
Prescribing information: Tritace
Presentation: Capsules containing 1.25mg, 2.5mg, 5mg or 10mg ramipril.
Indications: Reducing the risk of myocardial infarction, stroke, cardiovascular death or need for revascularisation procedures in
patients of 55 years or more who have clinical evidence of cardiovascular disease (previous MI, unstable angina or multivessel CABG or
multivessel PTCA), stroke or peripheral vascular disease. Reducing the risk of myocardial infarction, stroke, cardiovascular death or need
for revascularisation procedures in diabetic patients of 55 years or more who have one or more of the following clinical findings:
hypertension (systolic blood pressure >160mmHg or diastolic blood pressure >90mmHg); high total cholesterol (>5.2mmol/l); low HDL
(< 0.9mmol/l); current smoker; known microalbuminuria; clinical evidence of previous vascular disease. Mild to moderate
hypertension. Congestive heart failure as adjunctive therapy to diuretics with or without cardiac glycosides. Reduction in mortality in
patients surviving acute MI with clinical evidence of heart failure.
Dosage and administration: Reduction in risk of MI, stroke, cardiovascular death or need for revascularisation procedure:
The initial dose is 2.5mg Tritace o.d.. Depending on tolerability, the dose should be gradually increased. It is recommended that this
dose is doubled after about 1 week of treatment then, after a further 3 weeks, increased to 10mg. The usual maintenance dose is 10mg
Tritace o.d.. Patients stabilised on lower doses of Tritace for other indications where possible should be titrated to 10mg Tritace o.d..
Hypertension: Initial dose 1.25mg titrated up to a maximum of 10mg o.d. according to response. Usual dose 2.5mg or 5mg o.d.. Stop
diuretic therapy 2 - 3 days before starting Tritace and resume later if required. Congestive heart failure: Initial dose 1.25mg o.d.
titrated up to a maximum of 10mg daily according to response. Doses above 2.5mg daily can be given o.d. or b.d.. Post Myocardial
Infarction: Initiate treatment between day 3 and day 10 following AMI. Initially 2.5mg b.d. increasing to 5mg b.d after 2 days.
Assessment of renal function is recommended prior to initiation. Reduced maintenance dose may be required in impaired renal
function. Monitor patients with impaired liver function. In the elderly the dose should be titrated according to need. Not recommended
for children.
Contraindications: Hypersensitivity to ramipril or excipients, history of angioneurotic oedema, haemodynamically relevant renal
artery stenosis, hypotensive or haemodynamically unstable patients, pregnancy, lactation.
Precautions: Do not use in aortic or mitral valve stenosis or outflow obstruction. Assess renal function before and during use, as there
is a risk of impairment of renal function. Use with caution during surgery or anaesthesia. Hyperkalaemia. Do not use in patients using
polyacrylonitrile (AN69) dialysis membranes or during low-density lipoprotein apheresis with dextran sulphate. Agranulocytosis and
bone marrow depression seen rarely with ACE inhibitors as well as a reduction in red cell count, haemoglobin and platelet content.
Symptomatic hypotension may occur after initial dose or increase in dose, especially in salt/volume depleted patients.
Drug interactions: Combination with diuretics, NSAIDs, adrenergic blocking drugs or other antihypertensive agents may potentiate
antihypertensive effect. Risk of hyperkalaemia when used with agents increasing serum potassium. May enhance the effect of
antidiabetic agents. May increase serum lithium concentrations.
Side effects: Dizziness, headache, weakness, disturbed balance, nervousness, restlessness, tremor, sleep disorders, confusion, loss of
appetite, depressed mood, anxiety, paraesthesiae, taste changes, muscle cramps & joint pain, erectile impotence, reduced sexual desire,
fatigue, cough, hypersensitivity reactions; pruritus, rash, shortness of breath, fever, cutaneous and mucosal reactions, Raynauds
phenomenon, gastrointestinal disturbances, jaundice, hepatitis, impaired renal function, angioneurotic oedema, pancreatitis,
eosinophilia and vasculitis. Symptomatic hypotension, myocardial infarction or cerebrovascular accident possibly secondary to severe
hypotension in high-risk patients, chest pain, palpitations, rhythm disturbances, angina pectoris may occur. Use with caution and
closely monitor patients with impaired liver function. Reduced serum sodium levels, elevated blood urea nitrogen and serum creatinine.
Pre-existing proteinuria may deteriorate.
Basic NHS cost: 28 x 1.25mg capsules 5.30; 28 x 2.5mg capsules 7.51; 28 x 5mg capsules 9.55; 28 x 10mg capsules 13.00
Marketing authorisation numbers: 1.25mg 13402/0021, 2.5mg 13402/0022, 5mg 13402/0023, 10mg 13402/0024
Legal category: POM
Marketing authorisation holder: Aventis Pharma, 50 Kings Hill Avenue, Kings Hill, West Malling, Kent, ME19 4AH
Date of preparation: July 2000
TRI1151200
Date of preparation: February 2001
What is ?
Sponsored by an educational grant from Aventis Pharma
What is? bulletins
Name: ____________________________________________________________________________
Position: ____________________________________________________________________________
Address: ____________________________________________________________________________
____________________________________________________________________________
____________________________________________________________________________
Postcode: _______________________________(For mailing purposes a postcode must be supplied)
Tel: _______________________________Fax: ________________________________________
Email: ____________________________________________________________________________
www.evidence-based-medicine.co.uk
faxback form
fax no. 01732 584029
If you would like to receive more information about the
What is ? series simply print out this form, fill in your
details and fax it to: Team Assistant to the Health
Economics Unit, Aventis Pharma.
You might also like
- Varying Definitions of Online Communication ResearchDocument11 pagesVarying Definitions of Online Communication ResearchCalvin WirawanNo ratings yet
- The Role of Adaptive T Cell Immunity in AtherosclerosisDocument6 pagesThe Role of Adaptive T Cell Immunity in AtherosclerosisCandice ChengNo ratings yet
- Planner Flag StickersDocument2 pagesPlanner Flag StickersCandice ChengNo ratings yet
- Academic Integrity Guide Using APA StyleDocument4 pagesAcademic Integrity Guide Using APA StyleSohaila YaftaliNo ratings yet
- Atherosclerosis As InflammationDocument9 pagesAtherosclerosis As InflammationCandice Cheng0% (1)
- Easy Way To Learn ABGsDocument13 pagesEasy Way To Learn ABGsMunaim TahirNo ratings yet
- Clinical Patient WorksheetDocument1 pageClinical Patient WorksheetCandice ChengNo ratings yet
- Hypertrophic Pyloric StenosisDocument3 pagesHypertrophic Pyloric StenosisCandice ChengNo ratings yet
- Fluid Maintenance - PPPDocument17 pagesFluid Maintenance - PPPCandice ChengNo ratings yet
- Human Sexuality Chapter 15 NotesDocument7 pagesHuman Sexuality Chapter 15 NotesCandice ChengNo ratings yet
- Clinical Patient WorksheetDocument1 pageClinical Patient WorksheetCandice ChengNo ratings yet
- Adipocyte Dysfunctions Linking Obesity To Insulin Resistance and Type 2 DiabetesDocument12 pagesAdipocyte Dysfunctions Linking Obesity To Insulin Resistance and Type 2 DiabetesCandice ChengNo ratings yet
- Fluid MaintenanceDocument18 pagesFluid MaintenanceCandice ChengNo ratings yet
- Tables of Normal ValuesDocument6 pagesTables of Normal ValuesEunice BautistaNo ratings yet
- Stats Midterm Review-1Document8 pagesStats Midterm Review-1Candice ChengNo ratings yet
- Diffuse and Active in Ammation Occurs in Both Vulnerable and Stable Plaques of The Entire Coronary TreeDocument9 pagesDiffuse and Active in Ammation Occurs in Both Vulnerable and Stable Plaques of The Entire Coronary TreeCandice ChengNo ratings yet
- The Role of Adaptive T Cell Immunity in AtherosclerosisDocument6 pagesThe Role of Adaptive T Cell Immunity in AtherosclerosisCandice ChengNo ratings yet
- Inflammation Atherosclerosis ObesityDocument11 pagesInflammation Atherosclerosis ObesityCandice ChengNo ratings yet
- Acute Myocardial Infarction LANCETDocument15 pagesAcute Myocardial Infarction LANCETSi vis pacem...No ratings yet
- Oxidized LDL, A Critical Factor in AtherogenesisDocument2 pagesOxidized LDL, A Critical Factor in AtherogenesisCandice ChengNo ratings yet
- Atherosclerosis PathophysiologyDocument11 pagesAtherosclerosis PathophysiologyCandice ChengNo ratings yet
- Cardiomyopathy An OverviewDocument11 pagesCardiomyopathy An OverviewCandice ChengNo ratings yet
- Mechanisms of Disease - Acute Renal Failure and SepsisDocument12 pagesMechanisms of Disease - Acute Renal Failure and SepsisCandice ChengNo ratings yet
- Acute Kidney Injury - New Concepts in Definition, Diagnosis, Pathophysiology, and TreatmentDocument7 pagesAcute Kidney Injury - New Concepts in Definition, Diagnosis, Pathophysiology, and TreatmentCandice ChengNo ratings yet
- Chest Pain NICEDocument52 pagesChest Pain NICEAliya Batrisya AliyaNo ratings yet
- Acute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesDocument17 pagesAcute Exacerbation of COPD Nursing Application of Evidence-Based GuidelinesCandice ChengNo ratings yet
- #32 Anemia ManualDocument24 pages#32 Anemia ManualCandice ChengNo ratings yet
- Muscle Study NotesDocument15 pagesMuscle Study NotesCandice ChengNo ratings yet
- s121 Cpnre Study GuideDocument3 pagess121 Cpnre Study GuideCandice Cheng64% (14)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Templates For Planning and M&E (AIP, WFP, SMEA Templates)Document6 pagesTemplates For Planning and M&E (AIP, WFP, SMEA Templates)Genzo TaniaNo ratings yet
- Brand Name:: VasopressinDocument3 pagesBrand Name:: VasopressinHannah BuquironNo ratings yet
- Cardiovascular System Physical AssessmentDocument6 pagesCardiovascular System Physical Assessmentpulsating humNo ratings yet
- BipMED Price List May 2022Document9 pagesBipMED Price List May 2022erlinNo ratings yet
- Neo JaundiceDocument67 pagesNeo Jaundicemanisha thakur100% (1)
- Basic Construction Risk AssessmentDocument119 pagesBasic Construction Risk Assessmentbabylyn JurillaNo ratings yet
- Managing Hyperglycaemia in People With DKD - Final DraftDocument90 pagesManaging Hyperglycaemia in People With DKD - Final DraftRiched LhyneNo ratings yet
- BASH Headache ManagementDocument75 pagesBASH Headache ManagementsbjavedNo ratings yet
- Poster On 9 StepsDocument1 pagePoster On 9 StepsJOHN TAIPINo ratings yet
- Viii. Nursing Care Plan: Asessment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesViii. Nursing Care Plan: Asessment Diagnosis Planning Intervention Rationale Evaluationhehehe29No ratings yet
- Apollo Munich Optima Restore Premium ReceiptDocument17 pagesApollo Munich Optima Restore Premium ReceiptParag AmbreNo ratings yet
- Differential Diagnosis of Cervicobrachial PainDocument11 pagesDifferential Diagnosis of Cervicobrachial PainpuchioNo ratings yet
- 2019 - Asupan Zat Gizi Makro Dan Mikro Terhadap Kejadian Stunting Pada BalitaDocument6 pages2019 - Asupan Zat Gizi Makro Dan Mikro Terhadap Kejadian Stunting Pada BalitaDemsa SimbolonNo ratings yet
- Melissa Lockhart Resume 2021Document2 pagesMelissa Lockhart Resume 2021api-581746859No ratings yet
- Op-Ed ObesityDocument3 pagesOp-Ed Obesityapi-302568521No ratings yet
- Milrinone As Compared With DobutamineDocument10 pagesMilrinone As Compared With DobutamineArquivos DiversosNo ratings yet
- EVS - CO-5 - PPT - UO 5fDocument22 pagesEVS - CO-5 - PPT - UO 5fGirish KhedikarNo ratings yet
- M102 Notes 3. Presumptive Sign: Extreme Form of Morning Sickness ThatDocument3 pagesM102 Notes 3. Presumptive Sign: Extreme Form of Morning Sickness ThatNano KaNo ratings yet
- Nursing Care Plan: Chronic Pain and COPDDocument11 pagesNursing Care Plan: Chronic Pain and COPDneuronurse100% (1)
- Defining Child Abuse TypesDocument14 pagesDefining Child Abuse TypesAndreas Springfield GleasonNo ratings yet
- Ocean Breeze Air Freshener: Safety Data SheetDocument7 pagesOcean Breeze Air Freshener: Safety Data SheetMark DunhillNo ratings yet
- Curriculum Vitae: Dr. Raghu Ram PillarisettiDocument11 pagesCurriculum Vitae: Dr. Raghu Ram PillarisettiAjay Varun ReddyNo ratings yet
- Laws of Malaysia: Act A1648Document42 pagesLaws of Malaysia: Act A1648ana rizanNo ratings yet
- Psychological Psychoeducational Neuropsychological Assessment Information For Adults Families 1Document3 pagesPsychological Psychoeducational Neuropsychological Assessment Information For Adults Families 1ClaudiaNo ratings yet
- Trichiasis: Prepared By:pooja Adhikari Roll No.: 27 SMTCDocument27 pagesTrichiasis: Prepared By:pooja Adhikari Roll No.: 27 SMTCsushma shresthaNo ratings yet
- Full Download Ebook Ebook PDF Nelson Essentials of Pediatrics 8th Edition PDFDocument41 pagesFull Download Ebook Ebook PDF Nelson Essentials of Pediatrics 8th Edition PDFdavid.anderson198100% (37)
- 1.1. What Is Stress?: Chapter Six-Stress ManagementDocument6 pages1.1. What Is Stress?: Chapter Six-Stress ManagementMikias DegwaleNo ratings yet
- Tumor StagingDocument9 pagesTumor Stagingmalaran.deboraheloisaNo ratings yet
- Atls Pre Test SolvedDocument18 pagesAtls Pre Test SolvedDr.Mukesh KumarNo ratings yet
- Factors Affecting Adherence to Intranasal CorticosteroidsDocument20 pagesFactors Affecting Adherence to Intranasal CorticosteroidsKathrinna Feliz AlertaNo ratings yet