Professional Documents
Culture Documents
Infectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 93 Ocular Infections
Uploaded by
soledadDC3290 ratings0% found this document useful (0 votes)
64 views36 pagesPositive isolation rates of between 46% and 91% in clinically healthy dogs have been reported. Control of the normal ocular flora is maintained by rinsing of the ocular surface with tears. Conditions debilitating to the eye, such as reduced tear secretions, ultraviolet (UV) radiation should be corrected.
Original Description:
Original Title
93 Ocular Infections
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPositive isolation rates of between 46% and 91% in clinically healthy dogs have been reported. Control of the normal ocular flora is maintained by rinsing of the ocular surface with tears. Conditions debilitating to the eye, such as reduced tear secretions, ultraviolet (UV) radiation should be corrected.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
64 views36 pagesInfectious Diseases of The Dog and Cat, 3rd Edition: CHAPTER 93 Ocular Infections
Uploaded by
soledadDC329Positive isolation rates of between 46% and 91% in clinically healthy dogs have been reported. Control of the normal ocular flora is maintained by rinsing of the ocular surface with tears. Conditions debilitating to the eye, such as reduced tear secretions, ultraviolet (UV) radiation should be corrected.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
CHAPTER 93 Ocular Infections
Jean Stiles
EXTRAOCULAR INFECTIONS
Normal Flora
Despite the fact that all dogs probably have indigenous bacteria in their conjunctival cul-de-sac, positive
isolation rates of between 46% and 91% in clinically healthy dogs have been reported (Table 93-1). Variables
in the type of and frequency of isolate may be a result of geography, culturing technique, breed, and season.
Fungi are isolated from 10% to 22% of dogs.
42,100
In contrast to dogs, cats have a relatively lower rate of cultivable bacteria in their conjunctival sac.
33
Bacteria or
mycoplasmas have been isolated from 34% of the conjunctival samples and from 25% of the samples from the
lid margins. In one study of 50 cats, no organisms were isolated from 42% of the cats, bacteria were isolated
from the conjunctiva of 34% of the cats or 47% of the eyes, and 26% of the cats or 14% of the eyes had fungal
isolates from the conjunctiva (Table 93-2). No anaerobes were isolated.
40
Ocular Surface and Adnexa
Most surface bacterial infections are not strictly primary; other debilitating conditions often potentiate the
pathogenicity of organisms that are indigenous to the ocular surface. Other local nidi of infection, such as in the
lacrimal sac and meibomian glands or structures adjacent to the eye (ears, lip-folds), should be sought and
corrected to overcome persistent or recurring infection. Control of the normal ocular flora is maintained by
rinsing of the ocular surface with tears and blinking, which pushes the tears into the nasolacrimal (NL) system.
Tears also contain IgA and other antibacterial substances such as lactoferrin. Competitive interactions among
the indigenous flora keeps the numbers of organisms lower, whereas disrupting this balance may cause an
overgrowth of one species. Conditions debilitating to the ocular surface, such as reduced tear secretions,
ultraviolet (UV) radiation, immune suppression (e.g., with diabetes mellitus or Cushing's disease), and trauma
creating breaks in the epithelial barrier, may allow indigenous bacteria to adhere and possibly overgrow to
produce disease. To become established, bacteria must adhere, replicate, and then invade the tissue. Invasion
subsequently incites inflammation. Tissue damage with infection produces a combination of toxins from the
organism and enzymes such as collagenase, elastase, and cathepsins liberated by the neutrophilic response.
102
Bacteria, such as Pseudomonas aeruginosa, that have various proteolytic enzymes typically produce rapidly
progressive corneal ulcers.
Blepharitis in Dogs
Blepharitis, or inflammation of the eyelids, may develop secondary to bacterial, fungal, or parasitic agents.
Blepharitis can develop with other dermatologic diseases, with other ocular diseases such as conjunctivitis,
or as a sole clinical presentation. Clinical features of blepharitis include eyelid swelling, erythema, skin
ulceration, chalazia (granulomatous foci of inflammation along meibomian glands), and pruritis.
93
93.1
93.1.1
93.1.2
93.1.2.1
CHAPTER 93 Ocular Infections Page 1 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
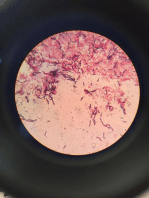
Staphylococcus species can cause a primary blepharitis and may also generate a hypersensitivity reaction.
Pruritis may lead to self-trauma, exacerbating the blepharitis. Bacterial infection of the eyelids may also
occur with keratoconjunctivitis sicca (KCS) or atopy.
Treatment of bacterial blepharitis should include cleansing the skin with dilute povidone iodine solution and
rubbing a broad-spectrum ophthalmic antibiotic into ulcerated skin as well as placing it in the eye 3 to 4
times daily. If skin is very inflamed, an antibiotic with dexamethasone is indicated. Severe cases may require
systemic antibiotic therapy such as cephalosporins and possibly antiinflammatory doses of oral
glucocorticoids. Any underlying condition that can be identified should also be addressed.
Canine juvenile pyoderma develops occasionally in puppies ages 3 to 16 weeks. Early reports suggested a
hypersensitivity reaction to Staphylococcus species, although the cause is considered unknown. Pustules and
granulomatous inflammation are present in the eyelids and face. In some cases the pinna and regional lymph
nodes are also affected. Rarely, joints may also be involved.
The condition responds quickly to administration of systemic glucocorticoids, suggesting an autoimmune
disease. Diagnosis is based on age, history, and clinical presentation. Prednisolone (2 mg/kg/day) should be
administered for 2 to 3 weeks. Lesions typically improve within a few days of beginning therapy. A systemic
antibiotic such as a cephalosporin is indicated if skin has become secondarily infected with bacteria.
Table 93-1 Frequency of Bacterial Isolation from the Conjunctival Sacs of
Clinically Healthy Dogs
7, 41, 51, 118
ORGANISM
ISOLATION (PERCENTAGE)
a
Staphylococcus (Total) 5770
Coagulase-positive 2445
Coagulase-negative 4655
Streptococcus (Total) 643
Nonhemolytic 1251
-Hemolytic 434
-Hemolytic 27
Corynebacterium (Total) 3075
Undifferentiated 11
C. pseudodiphtheriticum 9
C. xerosis 13
Neisseria (Total) 26
Undifferentiated 4
N. catarrhalis 9
N. pharyngis 4
N. sicca 3
N. caviae 3
N. lactamicus 3
N. flavescens 3
Pseudomonas (Total) 14
Moraxella (Total) 7
Bacillus (Total) 618
a Percentages are based on the numbers of animals from which organisms were isolated.
975
CHAPTER 93 Ocular Infections Page 2 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Table 93-2 Bacterial and Fungal Isolates from Clinically Healthy Cats
33,40
LOCATION ORGANISM
PERCENTAGE
a
Conjunctiva Staphylococcus spp. 27
Corynebacterium spp. 1.35
Bacillus spp. 35
Streptococcus spp. 22.5
Mycoplasma 05
Fungal isolates 13
Lids Staphylococcus spp. 2328
Streptococcus spp. 02
Bacillus spp. 25
Corynebacterium spp. 1.6
a Percentages are based on the numbers of animals from which organisms were isolated.
Blepharitis in Cats
Blepharitis in the cat is less common than in the dog. Cats appear relatively resistant to bacterial blepharitis,
except when they have a traumatic injury and resulting bacterial invasion. This type of injury most
commonly occurs in cat fights and may involve the head and eyelids. Abscesses near the eyelids should be
opened as they would be elsewhere and appropriate systemic antibiotics administered.
Conjunctivitis in Dogs
Bacterial conjunctivitis may be a primary condition or secondary to another ocular condition such as KCS,
distemper virus, a parasitic invasion, or the presence of a foreign body. Primary bacterial conjunctivitis
typically occurs for unknown reasons and in some cases is secondary to an insult that is no longer apparent
or is merely an overgrowth of normal conjunctival flora. The symptoms are purulent discharge with mild to
moderate discomfort. Diagnosis should be based on cytologic examination of the exudate and identification
of bacteria and neutrophilic inflammation. KCS should be ruled out based on a normal Schirmer tear test.
Bacterial overgrowth is common when tear production is low, and the underlying problem of KCS must be
addressed. Culture is typically not warranted for bacterial conjunctivitis unless response to therapy is poor. A
complete ocular exam, including a Schirmer tear test, fluorescein staining of the cornea, fluorescein
evaluation of NL duct patency, and a search for a foreign body in the conjunctival sac and behind the third
eyelid, should be performed. Therapy should include a broad-spectrum topical antibiotic such as
bacitracin-neomycin-polymixin B every 6 hours until resolution.
Viral conjunctivitis in dogs has been associated most often with distemper virus. The first signs of distemper
are bilateral conjunctivitis with a discharge that progresses from serous to mucopurulent. The virus may also
invade lacrimal tissue, causing an adenitis that results in KCS. In this situation the cornea may become
ulcerated and possibly even become perforated. KCS typically resolves over several weeks in dogs that
recover from distemper. Early diagnosis of dogs with distemper may be possible by fluorescent antibody
stains of conjunctival epithelial cells obtained from a scraping.
Therapy should include cleansing of eyes, application of a broad-spectrum topical antibiotic to help prevent
secondary bacterial infection, and if KCS is present, topical cyclosporine and artificial tears.
93.1.2.2
93.1.2.3
CHAPTER 93 Ocular Infections Page 3 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Conjunctivitis in Cats
Bacterial conjunctivitis in cats is unusual, with the exception of infection with Chlamydophila felis, which is
a common cause of conjunctivitis in cats (see Chapter 31). The typical clinical picture is unilateral
conjunctivitis with involvement of the second eye a few days later. The clinical presentation is
indistinguishable from conjunctivitis caused by feline herpesvirus-1 (FHV-1), and the two organisms may be
present simultaneously. Diagnosis is based on seeing the typical elementary body in the cytoplasm of
conjunctival epithelial cells (Fig. 93-1) or obtaining a positive fluorescent antibody (FA) test result on a
conjunctival scraping. C. felis can also be cultured but requires special transport media. Elementary bodies
are often few in number and the numbers diminish with chronicity, making them easy to miss. In an
experimental study of chlamydial conjunctivitis, infection with feline immunodeficiency virus (FIV)
prolonged the duration of clinical signs and led to chronic conjunctivitis.
86
Conjunctivitis caused by
Chlamydophila should be treated with topical tetracycline applied to both eyes 4 times daily until resolution
and then an additional 1 week. Oral doxycycline at 10 mg/kg/day was found to be superior to twice-daily
topical fusidic acid or chlortetracycline in one experimental study.
103
Treatment with oral doxycycline may
also be advisable to clear the GI tract of infection.
86
The potential of this organism to infect people is
uncertain; however, washing hands after treating an affected cat is advised.
Mycoplasma felis has been variably implicated as a cause of conjunctivitis in cats (Fig. 93-2). Some studies
have recovered Mycoplasma species as normal flora from feline conjunctiva, whereas others have not.
Similarly, experimental infections of healthy, young cats have produced conjunctivitis in some studies
50
and
not in others. Mycoplasma organisms may require a stressor such as FHV to cause disease. Mycoplasma
species are sensitive to many topical antibiotics, including tetracycline.
Fig 93-1 Intracytoplasmic C. felis inclusions in conjunctival epithelial cells of a
cat with conjunctivitis (Giemsa stain, 330).
975
976
93.1.2.4
CHAPTER 93 Ocular Infections Page 4 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-2 Mycoplasma organisms within conjunctival epithelial cells in a cat
with conjunctivitis (Wright stain, 330).
FHV-1 is a frequent cause of ocular disease in cats.
2,106,107,120
Young cats with respiratory tract disease
generally have conjunctivitis with marked conjunctival hyperemia, chemosis, and serous to purulent ocular
discharge (Fig. 93-3). The condition is usually self-limiting and resolves in 1 to 2 weeks. In severe cases of
herpesvirus conjunctivitis, the risk of symblepharon is high. Symblepharon, or adhesions of the conjunctiva
to itself or the cornea, may lead to permanent visual impairment, and an attempt to break these adhesions
early should be made. After application of topical anesthesia, a cotton-tip swab can be used to break
adhesions and strip off cellular debris and fibrin. This process may need to be repeated frequently until the
conjunctivitis has resolved. In severe conjunctivitis a topical antiviral such as trifluridine should also be used
at least 4 times daily. In addition to general supportive care, the eyes should be cleansed frequently and a
broad-spectrum topical antibiotic applied to minimize secondary bacterial infection as the conjunctival
surface sloughs. Once infected, cats become latent carriers of FHV-1 and may have recurrences of ocular
disease, including conjunctivitis and corneal ulcers. Many cats have transient episodes of conjunctivitis, with
conjunctival hyperemia, serous or purulent ocular discharge, and blepharospasm. Most cases are self-limiting
and do not require treatment. If a topical antibiotic is used, tetracycline is the most appropriate choice
because of its efficacy in treating C. felis and M. felis, which are common feline conjunctival pathogens that
may contribute to conjunctivitis in addition to FHV-1. Hartmannella vermiformis, an amebic endosymbiont
that contains the Chlamydia-like agent Neorickettsia hartmannellae, has been isolated in greater prevalence
from cats with keratitis or conjunctivitis than from clinically healthy cats.
121
CHAPTER 93 Ocular Infections Page 5 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-3 Acute conjunctivitis secondary to feline herpesvirus. Note severe
chemosis and conjunctival hyperemia.
Cats may develop chronic conjunctivitis or proliferative keratitis associated with FHV-1.
17,104
Laboratory
diagnostic tests, such as virus isolation from the conjunctiva and conjunctival scrapings for fluorescent
antibody testing, to prove FHV-1 as a cause of conjunctivitis in cats are frequently negative, making the
diagnosis uncertain.
85
Identification of FHV-1 DNA in conjunctiva or the cornea by the polymerase chain
reaction (PCR) is a more sensitive test than virus isolation or FA testing, although a high percentage of
clinically normal cats have positive tests for viral DNA by PCR.
108,116
Treatment with an ophthalmic
antiviral medication such as trifluridine can be used in cats with chronic conjunctivitis, although results vary.
Treatment for KCS in cats with FHV-1 conjunctivitis can include topical 0.2% cyclosporine ointment in
addition to antiviral therapy. Recombinant interferon (IFN) has also been administered to cats with chronic
FHV-1related ocular disease, although no studies have documented its effectiveness. Oral (see Chapter 2)
and topical administration of IFN have been used.
76,111,112
Topical administration is discussed in the later
Keratitis in Cats section.
Treatment with oral lysine has been shown to be efficacious in reducing the severity of FHV-1induced
conjunctivitis in an experimental setting.
47,110
Cats receiving 500 mg of oral L-lysine twice daily had less
severe conjunctivitis than cats receiving placebo, although the length of disease and isolation of virus did not
differ between the groups. Kittens with FHV-1related disease may benefit from administration of 250 mg
oral lysine twice daily. Adult cats with frequent recurrences of FHV-1related disease can be treated long
term with 500 mg of oral lysine twice daily. Lysine should be given with food to avoid gastric upset.
976
977
CHAPTER 93 Ocular Infections Page 6 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Keratitis in Dogs
Infectious keratitis in dogs develops after a corneal ulceration or traumatic wounding. Bacterial flora
inhabiting the ocular surface are those most likely to invade a corneal wound. Ulcerative keratitis and
corneal abscesses are the two bacterial corneal diseases of concern. Staphylococcus and Streptococcus
species are especially common, although infections with gram-negative bacteria may also develop.
Bacterial keratitis usually incites a visible neutrophilic response, characterized by a yellow to white cellular
infiltrate within the cornea. Vascular growth into the cornea also occurs but usually does not begin for
several days after injury and infection. Vessels originate from the limbus and grow at a rate of approximately
1 mm/day toward the site of infection. Rapid corneal destruction may occur with infectious keratitis.
Invading bacteria and neutrophils may release proteases and collagenases, which contribute to corneal
melting. Increased cyclooxygenase-2 expression has been documented in all corneal layers of dogs with
keratitis, indicating that antiprostaglandin therapy may be a potential treatment for inflammatory keratitis.
101
Fungal keratitis, which can be indistinguishable from bacterial keratitis, is less common but can be caused by
penetrating injuries with plant material or prolonged topical treatment with antibacterial or glucocorticoid
therapy. White or brown infiltrates in the cornea are more likely to be caused by fungal growth. Fungal
keratitis manifests as ulcerative keratitis, interstitial inflammation, or eventually iris prolapse because of
damage to Descemet's membrane and corneal perforation.
Diagnosis of infectious keratitis is based on clinical findings, cytology, and culture. Fluorescein staining is
used to detect epithelial ulceration. All corneal ulcers that are progressive or involve the stroma should be
cultured. A mini-tip culturette with a moistened tip should be gently swabbed over the ulcer bed. After
application of topical proparacaine, a flattened spatula or the blunt end of a scalpel blade should be used to
gently scrape the ulcer edge for a cytology sample. Healthy corneas have noncornified epithelial cells.
Keratin debris, an occasional bacterium, and mucus may also be observed. With bacterial keratitis,
neutrophils are the predominant cell type, and bacteria may be either numerous or few or not visualized on
cytology. Antibacterial treatment should be instituted to prevent the colonizing bacteria from causing more
damage to the cornea. The initial decision about therapy should be based on whether cocci or rods have been
identified. Culture is more sensitive than cytology for detecting bacteria and is the only way to confirm the
species type and its antibacterial susceptibility. Until culture results are known, the broadest spectrum of
antibacterial drugs possible should be used. Often, this means combination therapy, such as a topical
fluoroquinolone and cefazolin. To achieve broad-spectrum bactericidal activity, commercial antibiotics can
be fortified, and injectable antibiotics can be used with artificial tears or saline to create topical formulations
(Tables 93-3 and 93-4). Frequency of application is critical. In a rapidly progressive corneal ulcer, topical
antibiotics should be applied every 1 to 2 hours.
Systemic antibiotics are usually not indicated unless the cornea has a penetrating wound. Fungal keratitis is
also treated with topical medication because systemic drug penetration of ocular tissues is poor (Table 93-5).
Topical atropine can be used 2 to 4 times daily if miosis is present, although it should not be used in dogs
with KCS or glaucoma. The use of topical agents to halt the proteolytic destruction of the cornea may be
beneficial. Autogenous serum, acetylcysteine, or sodium ethylenediaminetetraacetic acid applied topically
several times daily have all been advocated. The author favors autogenous serum because it is readily
available and not irritating, although it must be handled and maintained using a sterile technique. Serum
should be refrigerated and replenished every 48 hours.
93.1.2.5
CHAPTER 93 Ocular Infections Page 7 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
If fungal keratitis is documented or suspected, it should be treated with a topical antifungal agent every 2 to 3
hours (see Table 93-5). Although natamycin is the only approved ophthalmic antifungal agent, other agents
such as silver sulfadiazine have proven effective and safe for topical ocular use.
81
Deep corneal ulcers in danger of perforating respond best to surgical therapy, such as placement of a
conjunctival flap.
Ocular discharge should be cleansed frequently to remove neutrophils and their proteolytic enzymes. If tear
production is inadequate, topical cyclosporine every 12 hours and artificial tears several times daily should
be administered to supplement and stimulate lacrimation. Closing the lids or placing a third eyelid flap
should be avoided. These procedures limit drug contact with the cornea, impair discharge drainage, increase
the temperature of the environmentthus promoting bacterial growth, fungal growth, or bothand prevent
visualization of the ulcer's progress.
Systemic antiinflammatory agents can be beneficial as analgesics and to aid in the treatment of uveitis
associated with deep corneal ulcers. Oral carprofen at 2 mg/kg every 12 hours is well tolerated by most dogs
but is not recommended for cats.
Keratitis in Cats
Bacterial keratitis in cats may occur secondary to corneal ulcers (including those initiated by FHV-1) or
traumatic wounding. Appearance, diagnosis, and treatment are the same as for the dog.
Corneal ulceration and keratitis from FHV is very common and begins with invasion of the corneal
epithelium by the virus.
106
The most common corneal abnormality is punctate or linear epithelial erosions
(Fig. 93-4), which may enlarge to form geographic ulcers. Conjunctivitis usually accompanies corneal
ulcers.
104
Mechanical debridement of loose epithelium to remove virus and treatment with a topical antiviral
agent have been the most successful therapies, although many of the ulcers heal without antiviral agents.
Grid keratotomies should not be performed in cats because this treatment modality appears to increase the
risk of corneal sequestration.
60
Antiviral agents such as trifluridine are virostatic and should be given at least
4 times daily until the ulcer heals and for approximately 1 week afterward.
Stromal keratitis is one of the most serious manifestations of FHV-1 corneal infection and is thought to
primarily be a result of an immune reaction to the virus. Clinically healthy cats without apparent infection
may harbor the virus in a latent or an active form in their corneas or trigeminal ganglia.
116
Experimentally,
subconjunctival dexamethasone caused cats infected with FHV-1 to develop stromal keratitis.
82
Stromal
keratitis may develop with or without a corneal ulcer. Vascularization and cellular infiltrate of the deeper
layers of the cornea, often accompanied by chronic discomfort, are typical symptoms (Fig. 93-5). Antiviral
agents alone usually do not improve the keratitis. Topical antiinflammatory agents, such as glucocorticoids,
nonsteroidal topical agents, or cyclosporine, may help the inflammatory response but could exacerbate the
viral infection. Antiinflammatory agents should be used only in conjunction with an antiviral agent. Topical
glucocorticoids may predispose cats to the development of corneal sequestration. Topical IFN has been used
in humans with herpetic keratitis and may be beneficial in cats,
76,111,112
although controlled studies are
lacking. Lyophilized recombinant -IFN can be reconstituted in saline and used as a topical drop. The dosage
for cats is typically one drop every 6 hours of a solution ranging from 100 to 2500 U/ml, whereas in humans
977
980
93.1.2.6
CHAPTER 93 Ocular Infections Page 8 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
up to 10
6
U/ml have been used. Oral IFN can also be used and is discussed in Chapter 2. Lysine for ocular
herpetic disease is discussed under feline conjunctivitis.
Table 93-3 Commercially Available Ophthalmic Antibacterial Agents
GENERIC NAME TRADE NAME CONCENTRATION
SOLUTION (PERCENTAGE)
OINTMENT
Individual Agents
Bacitracin AK-Tracin NA 500 U/g
Available generically
Chloramphenicol AK-Chlor 0.5% NA
Chloromycetin 0.16% 10%
Chloroptic 0.5% 10%
Available generically 0.5% NA
Ciprofloxacin hydrochloride Ciloxan 0.3% 0.3%
Erythromycin Available generically NA 0.5%
Gentamicin sulfate Gentamicin 0.3% 0.3%
Genoptic 0.3% 0.3%
Gentacidin 0.3% 0.3%
Gentak 0.3% 0.3%
Available generically 0.3% 0.3%
Norfloxacin Chibroxin 0.3% NA
Ofloxacin Ocuflox 0.3% NA
Sulfacetamide sodium AK-Sulf 10% 10%
Bleph-10 10% 10%
Sulf-10 10% NA
Available generically 10% 10%
Tobramycin sulfate Tobrex 0.3% 0.3%
Aktob 0.3% 0.3%
Tomycin 0.3% NA
Available generically 0.3% NA
Mixtures
Polymyxin B-bacitracinZinc AK-Poly-Bac NA 10,000 U
Polysporin 500 U/g
Available generically
Polymyxin B-neomycin
bacitracin
AK-Spore NA 10,000 U
Neosporin 3.5 mg
Available generically 400 U/g
Polymyxin
B-neomycin-gramicidin
AK-Spore 10,000 U 10,000 U
Neosporin 1.75 mg 3.5 mg
Available generically 0.025 mg/ml NA
Polymyxin B-oxytetracycline Terramycin NA 10,000 U
Terak 5 mg/g
Polymyxin B-trimethoprim Polytrim 10,000 U NA
Available generically 0.1% NA
Modified from Whitley RD. 2000. Canine and feline primary ocular bacterial infections. Vet Clin North Am
30(5):11511167.122
NA, Not available.
CHAPTER 93 Ocular Infections Page 9 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Table 93-4 Fortified and Noncommercial Topical Antibiotic Solution
Preparation
Gentamicin (fortified)
Gentamicin injectable (50 mg/ml) 6 ml
Artificial tears 24 ml
TOTAL 30 ml
Final concentration = 10 mg/ml (1% solution)
or
Add 2 ml of injectable gentamicin (50 mg/ml)to the 5-ml bottle of commercial ophthalmic gentamicin solution
(0.3%)
Final concentration: 14 mg/ml (1.4% solution). Shelf-life: 30 days
Amikacin
Amikacin injectable (250 mg/ml) 4 ml
Artificial tears 26 ml
TOTAL 30 ml
Final concentration = 33 mg/ml (3.3% solution)
or
Remove 2 ml from a 15-ml squeeze bottle of artifical tears and discard
Add 2 ml of injectable amikacin (50 mg/ml)
Final concentration: 6.7 mg/ml (0.67% solution). Shelf-life: 30 days
Ampicillin
Mix 125-mg vial ampicillin with sterile saline or artificial tears to a concentration of 20 mg/ml
Cefazolin
Remove 2 ml from a 15-ml squeeze bottle of artificial tears and discard
Reconstitute a 500 or 1000 mg vial of cefazolin with sterile saline to a concentration of 250 mg/ml
Add 500 mg of the reconstituted cefazolin (2 ml) to the bottle of artificial tears
Final concentration: 33 mg /ml (3.3% solution). Shelf-life: 14 days. Keep refrigerated
Cephalothin
Remove 6 ml from a 15-ml squeeze bottle of artificial tears and save
Add the 6 ml of tear solution to a 1000 mg vial of cephalothin
Add the entire 1000 mg of the reconstituted cephalothin (6 ml) to the bottle of artificial tears.
Final concentration: 67 mg/ml (6.7% solution). Keep refrigerated
Ticarcillin
Reconstitute a 1-g vial of ticarcillin with 10 ml of sterile saline
Add 1.0 ml (100 mg) of this solution to a 15-ml squeeze bottle of artificial tears.
Final concentration: 6.7 mg/ml (0.67% solution). Shelf-life: 4 days. Keep refrigerated
Tobramycin (fortified)
Add 1.0 ml of injectable tobramycin (40 mg/ml)to a 5-ml bottle of commercial ophthalmic tobramycin solution
(0.3%)
Final concentration: 9.2 mg /ml (0.92% solution). Shelf-life: 30 days.
Vancomycin
Remove 9 ml from a 15-ml squeeze bottle of artificial tears and discard
Reconstitute a 500-mg vial of vancomycin with 10 ml of sterile saline
Add the entire 500 mg of reconstituted vancomycin (10 ml)to the bottle of artificial tears
Final concentration: 31 mg/ml (3.1% solution). Shelf-life: 4 days. Keep refrigerated
Adapted from Whitley RD. Canine and feline primary ocular bacterial infections. Vet Clin North Am 30(5):11511167,
2000, with premission.
122
CHAPTER 93 Ocular Infections Page 10 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Table 93-5 Commercially Available Ophthalmic Antifungal Agents
GENERIC NAME CONCENTRATION AND
FORMULATION
MYCELIAL YEASTS
Polyenes
Natamycin 5% suspension Aspergillus, Fusarium
Amphotericin B
0.15% suspension
a
Aspergillus variable efficacy Numerous, Candida
Azoles
Miconazole Vaginal cream or
compounded
a
Aspergillus, Fusarium, Candida
Alternaria, Penicillium
Ketoconazole
2% solution
a
Aspergillus, Fusarium, Candida
Candida, Curvularia
Itraconazole 1% in 30% DMSO
compounded
a
Aspergillus, Pseudallescheria Candida
Fluconazole
0.2% solution
a
Aspergillus Candida
Voriconazole
1% solution
a
Aspergillus, Fusarium,
Penicillium, Scedosporium
Other
Silver sulfadiazine 1% cream Aspergillus, Fusarium Candida
Disinfectants
N-acetylcysteine 10% solution Aspergillus, Fusarium
Chlorhexidine 0.2% solution Various species Variety
Povidone iodine 1:10 to 1:50 solution Various species Variety
Modified from Whitley RD. 2000. Canine and feline primary ocular bacterial infections. Vet Clin North Am
30(5):11511167.
122
DMSO, Dimethylsulfoxide.
a Not available commercially for ophthalmic use. Must use existing parenteral or topical solutions
or make by compounding pharmacy.
Fig 93-4 Linear epithelial ulcer caused by feline herpesvirus. Note chemosis
from dorsal conjunctiva.
CHAPTER 93 Ocular Infections Page 11 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-5 Corneal stromal keratitis in cat. Note corneal vascularization, edema,
and conjunctivitis.
Corneal sequestration is a common disorder in cats, particularly Persians and Himalayans, and may follow
chronic corneal ulcers or keratitis caused by FHV-1 (Fig. 93-6). It has been noted to occur after topical
glucocorticoid treatment in FHV-1 experimentally infected cats, and in cats receiving grid keratotomies.
60,83
The condition is characterized by an area of corneal degeneration with a brown to black discoloration. The
lesions vary from pinpoint sequestra to those that occupy more than half the cornea; vascularization may be
intense or absent; and ocular pain ranges from none to marked. Like stromal keratitis, sequestra can be one
of the most serious and potentially blinding sequela of FHV-1. Most ophthalmologists recommend
keratectomy followed by a graft (corneal or conjunctival) as the therapy for sequestra.
Fig 93-6 Corneal sequestrum in a cat. Note corneal blood vessels.
980
981
CHAPTER 93 Ocular Infections Page 12 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Dacryocystitis in Dogs and Cats
Dacryocystitis, or inflammation of the NL system, is usually associated with a bacterial infection. NL foreign
bodies such as plant material are frequently the inciting cause. Dacryocystitis is more uncommon in cats than
dogs. Clinical manifestations of dacryocystitis include conjunctival hyperemia, especially of the ventral
conjunctival sac, purulent ocular discharge, and epiphora. Blepharospasm may or may not be present. Pain,
purulent exudate, or both from the lacrimal puncta occasionally can be elicited by pressing on the skin near
the medial canthus. Swelling or draining tracks in the skin near the medial canthus may also occur.
The diagnosis is confirmed by NL flushing with culture of any purulent debris recovered.
Dacryocystorhinography may be necessary to identify foreign bodies or cystic structures within the NL
system. If foreign bodies cannot be flushed from the system, surgical removal via a dacryocystotomy may be
required.
After NL flushing, a broad-spectrum antibiotic solution such as polymixin-B-neomycin-gramicidin should be
used 4 to 6 times daily. Systemic antibiotics are not indicated if the infection is confined to the NL system.
Repeated flushings may be needed to maintain patency. The NL duct can also be cannulated with Silastic
tubing to establish and maintain patency. Stricture of the NL duct may occur with dacryocystitis leading to
chronic epiphora.
Orbital Infections in Dogs and Cats
Orbital disease caused by bacterial infection generally has a fairly rapid onset compared with the slow
progression of clinical signs seen with orbital neoplasia. Typical clinical signs of orbital abscess and
cellulitis include periorbital swelling, exophthalmos, elevation of the nictitating membrane, conjunctival
hyperemia, and pain on palpation of periorbita or when opening the mouth (Fig. 93-7). Swelling of the oral
mucosa behind the last molar is evident in some animals.
Bacterial infection of the orbit is common, especially in dogs, although fungal infections have also been
reported in both dogs and cats.
52,126
Infectious agents may gain access to the orbit by several routes,
including through the oral mucosa behind the last molar, from the frontal sinus through breakdown of medial
orbital bone, from tooth root abscesses in which bacteria dissect through soft tissue planes, from penetrating
wounds or foreign bodies of the skin or oral cavity, and through hematogenous spread from distant sites of
infection.
Fig 93-7 Orbital abscess in dog. Note severe periorbital swelling. (Courtesy
Kirk Gelatt, Gainesville, Fla.)
93.1.2.7
93.1.2.8
CHAPTER 93 Ocular Infections Page 13 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Orbital bacterial abscesses are best diagnosed with ultrasonography, in which the abscess appears as a
hypoechoic area posterior to the globe (Fig. 93-8). A fungal granuloma would appear hyperechoic and could
not be readily differentiated from neoplasia. Computed tomography or magnetic resonance imaging are more
helpful for delineating infections that involve the respiratory system and orbit simultaneously, which is more
likely in fungal infections.
Drainage of orbital abscesses should be established when possible. Because only soft tissue separates the oral
cavity from the ventral orbit in the dog and cat, an incision through the tissue behind the last molar can be
used to access the orbit. A small mosquito forceps should be advanced into the orbit, using blunt probing
not graspingto attempt to hit the abscess. Any purulent material should be cultured for aerobic and
anaerobic bacteria and submitted for cytologic evaluation. Pending culture results, broad-spectrum systemic
antibiotic therapy such as clindamycin and a penicillin or cephalosporin should be instituted.
The prognosis for bacterial orbital abscesses is generally good, whereas the prognosis for orbital fungal
infections is more guarded.
Diagnosis
The decision to perform cultures from the ocular surface should be made early in the examination before
various eye drops have been administered and manipulations performed. The use of a moist or calcium alginate
swab improves the recovery rate.
51,118
Because the volume of material collected is usually small and subject to
drying, swabs should be inoculated quickly onto appropriate media or placed in transport media.
Cytologic examination of conjunctival and corneal scrapings is an important and rapid diagnostic aid. Topical
proparacaine should be applied and the appropriate surface scraped with a small, flat spatula or the blunt end of
a scalpel blade. Excessive ocular discharges should be removed before scraping. Collected material should be
gently spread onto glass slides and air dried. Multiple slides should be prepared, because some slides may not
have adequate numbers of cells. The slides can be stained with a modified Giemsa or Wright's stain for
cytologic evaluation and a Gram stain to evaluate the type of bacteria that might be present. Slides can also be
made for examination by indirect FA for distemper virus, FHV, and C. felis.
981
93.1.3
CHAPTER 93 Ocular Infections Page 14 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-8 Ultrasound image of retrobulbar abscess in a cat. Markers delineate a
hypoechoic structure posterior to globe.
981
982
CHAPTER 93 Ocular Infections Page 15 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-9 Nylon bristle brush used to obtain conjunctival cytology specimen.
An alternate technique is to roll a small, nylon bristle-brush applicator (Microbrush, Grafton, Wisc.) over the
appropriate surface and then roll it onto a slide (Fig. 93-9). Preparations made with this method have fewer cells
that are dispersed better on the slide and have less crushing artifact.
117,127
This method is less traumatic and
easier to perform on cats and small dogs with tight lid-globe conformations.
Small snip biopsy specimens of the conjunctiva can be readily obtained using topical anesthesia for the animal.
These small pieces of tissue should be spread out on a piece of paper before they are placed in fixative.
INTRAOCULAR INFECTIONS
Intraocular bacterial infections may be exogenous or endogenous in origin. The source of an exogenous infection
from a penetrating ocular injury may be obvious from the history and appearance of the eye, but it may be an
inapparent injury, such as a self-sealing cat claw injury through the conjunctiva and sclera. Exogenously induced
infections are usually unilateral, whereas endogenous infections are often bilateral.
Local Injury
All recent perforating ocular injuries should be considered septic and treated intensively with bactericidal
broad-spectrum antibiotics, topically and systemically, until susceptibility data are obtained. Topical
fluoroquinolones, especially ofloxacin, have excellent corneal penetration and achieve therapeutic levels in the
anterior segment against a wide variety of bacteria.
128
In suspected or confirmed bacterial endophthalmitis, a
topical fluoroquinolone should be used every 1 to 2 hours. Topical antiinflammatory therapy is also indicated
and may include frequent prednisolone acetate or a nonsteroidal agent such as flurbiprofen. Systemic
broad-spectrum antibiotic therapy as well as systemic antiinflammatory therapy should also be administered.
Most active intraocular inflammations associated with perforating injuries should have centesis performed.
Anterior chamber centesis for cultures and cytology is safe and may yield specific information to guide future
93.2
93.2.1
CHAPTER 93 Ocular Infections Page 16 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
therapy. Aqueous centesis is not as reliable as vitreous centesis in demonstrating bacterial growth in
endophthalmitis; consequently, negative culture results from an aqueous sample are not definitive evidence of
sterile inflammation.
37
Sepsis is indicated on oculocentesis by degenerate neutrophils and bacteria.
Nondegenerate neutrophils may indicate a sterile purulent inflammation such as phacoclastic uveitis
(phacoanaphylaxis, lens-induced inflammation) caused by lens capsule rupture.
Systemic Disease
The eye is often a target organ for systemic infectious agents. The ocular disease may be the primary complaint,
with the systemic disease being unidentified or overlooked. It is important to recognize the systemic
involvement to give an accurate prognosis and provide adequate therapy. Conversely, animals with systemic
disease should have ocular examinations, which may provide rapid diagnostic clues and prognostic information.
Most infectious agents access the eye via the uveal or vascular tunic. Typically, infectious agents or immune
complexes become established in the uvea, producing a posterior uveitis or chorioretinitis, an anterior uveitis,
or if overwhelming, endophthalmitis or panophthalmitis.
Canine Distemper
Ocular signs of distemper (see Chapter 3) usually include bilateral conjunctivitis with a discharge that
progresses from serous to mucopurulent. The palpebral conjunctiva is primarily involved. Lacrimal adenitis
may result in reduced tear production, which in turn results in more profound signs of conjunctivitis, corneal
ulceration, and pain. The dry eye usually resolves if the animal recovers from systemic infection.
Occasionally, conjunctival or lacrimal involvement has such mild systemic signs that distemper is not
suspected.
Distemper virus often produces a multifocal, nongranulomatous chorioretinitis that does not usually cause
blindness. The prevalence of chorioretinitis is unknown but probably varies, as do the neurologic signs, with
strain of virus and immune competency of the host. Dogs with neurologic forms of distemper had an overall
prevalence of chorioretinal lesions of 41%, but 83% of the dogs with chronic leukoencephalopathy
syndromes had chorioretinal lesions.
115
Occasionally, chorioretinitis is diffuse and blinding and may mimic
the genetic syndrome of progressive retinal atrophy. Acute focal lesions in the tapetum or nontapetum have
gray to white, hazy or ill-defined borders (Fig. 93-10).
36
Chorioretinal scars resulting from distemper virus
have sharply demarcated borders, are hyperreflective in the tapetum, and are depigmented in the nontapetum.
Histologically, retinal changes are characterized by degeneration of the retina with perivascular cuffing in
some instances. Lesions may be focal or diffuse degeneration of ganglion cells, proliferation of retinal
pigment epithelium, atrophy of photoreceptors, disorganization of retinal layers, focal gliosis, and distemper
inclusion bodies in glial cells.
982
983
93.2.2
93.2.2.1
CHAPTER 93 Ocular Infections Page 17 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-10 Multifocal acute distemper lesions in nontapetum of dog. Active
lesions are recognized by their white cellular infiltrates with hazy
borders.
The most serious clinical ocular problem associated with distemper is optic neuritis.
35
Optic neuritis is
characterized by an acute onset of bilateral blindness and mydriasis. If inflammation extends rostrally to the
optic papilla, ophthalmoscopic signs of peripapillary hemorrhages and edema, retinal vascular congestion,
and elevation of the papilla are observed (Fig. 93-11).
35
If the neuritis remains retrobulbar, the diagnosis is
made by exclusion (e.g., blind eyes with mydriasis and normal retinal function as tested by
electroretinography). The optic neuritis may be isolated, prodromal, or concurrent with other neurologic
distemper signs. Distemper-associated blindness also may occur with inflammation of the occipital cortex or
optic radiations, but pupillary reflexes are usually normal under such circumstances. Optic neuritis may
occur with other central nervous system (CNS) inflammatory conditions such as granulomatous
meningoencephalitis (see Chapter 84).
Ocular signs are suggestive but not definitive for distemper. Acute lesions of chorioretinitis usually correlate
well with concurrent systemic disease, but chorioretinal scars do not. Finding distemper inclusions or
positive immunofluorescence on a conjunctival scraping may be of diagnostic help early in the course of
systemic disease (5 to 21 days after inoculation), but a negative finding is inconclusive. Distemper should be
considered in any animal with acute optic neuropathy or an acute onset of KCS.
CHAPTER 93 Ocular Infections Page 18 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-11 Acute optic neuritis characterized by elevated disc, peripapillary
hemorrhages, and loss of vision. Distemper is one cause for this
syndrome.
Because no specific antiviral therapy is available, treatment is primarily symptomatic. Acute optic neuritis or
severe chorioretinitis should be treated with systemic antiinflammatory dosages of glucocorticoids. Dry eye
should be treated with topical cyclosporine twice daily and artificial tears. Corneal ulcers should also be
treated with a topical broad-spectrum antibiotic several times daily.
Infectious Canine Hepatitis
Canine adenovirus-1 (CAV-1) infection has been estimated to produce ocular lesions in approximately 20%
of dogs recovering from natural infections, whereas a 0.4% or less prevalence has been noted in
CAV-1-vaccinated dogs (see Chapter 4). The universal use of CAV-2 for immunization has made the
postvaccinal reaction of corneal edema and uveitis much less common. The lesion, considered to be an
immune complex Arthus reaction, occurs 10 to 21 days after vaccination and requires about an equal time to
resolve. The condition is bilateral in 12% to 28% of the cases. The Afghan hound has been reported to have
an increased prevalence,
19
and other sight hounds and Siberian huskies may have similarly high frequencies
of ocular reactions to CAV-l.
The most visible ocular lesion is stromal corneal edema resulting from inflammatory damage to the corneal
endothelium (Fig. 93-12). Occasionally, a dog has signs of uveitis (blepharospasm, miosis, hypotony, and
93.2.2.2
CHAPTER 93 Ocular Infections Page 19 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
aqueous flare) 1 to 2 days before the corneal edema is evident. Corneal edema may be focal or generalized
and is usually transient. In some instances, the edema is permanent or may require several months to clear. A
marked hypotony combined with altered corneal rigidity may result in a keratoconus. Glaucoma, the most
significant sequela of uveitis, may be missed in the early stages because of the preexisting corneal edema and
conjunctival hyperemia. Uveitis associated with vaccination is usually diagnosed by the typical ocular
lesions combined with the history of recent vaccination in a puppy or young (younger than 2 years of age)
dog. Other causes of corneal edema, such as congenital pupillary membranes, glaucoma, or corneal
ulceration, should be ruled out. Therapy is similar to that for other forms of nonseptic anterior uveitis
specifically, topical prednisolone acetate 4 to 6 times daily and atropine to achieve mydriasis. Oral carprofen
may also be helpful.
Fig 93-12 Diffuse corneal edema induced by vaccination with canine
adenovirus-1 live vaccine.
Canine Herpesvirus Infection
Canine herpesvirus (CHV) infection (see Chapter 5) in the adult dog has produced only a transient
conjunctivitis and vaginitis of 4 to 5 days duration. Occasional dendritic corneal ulceration patterns are seen
in the dog, but their cause has not been determined. Neonatal CHV infection produces a bilateral panuveitis
with keratitis, synechiae, cataracts, retinal necrosis and disorganization, retinal atrophy and dysplasia, and
optic neuritis and atrophy.
1
983
984
93.2.2.3
CHAPTER 93 Ocular Infections Page 20 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Rickettsial Agents of Dogs
Ehrlichiosis
Ocular lesions occur frequently in dogs with ehrlichiosis caused by Ehrlichia canis, although the ocular
abnormalities may vary in severity and do not develop in every patient (see Chapter 28). The most typical
lesions include unilateral or bilateral anterior uveitis characterized by one or more of the following:
conjunctival and episcleral hyperemia, miosis, aqueous flare, hypopyon, keratic precipitates, hyphema,
synechiae, and hypotony. Glaucoma may occur secondary to chronic anterior uveitis (Fig. 93-13). Signs of
posterior segment inflammation may include chorioretinitis as evidenced by inflammatory cell infiltrate
under and within the retina, serous retinal detachment, retinal hemorrhage, and optic neuritis. Optic
neuritis may be evidenced by a swollen optic disk and peripapillary hemorrhages. Anterior uveitis has also
been seen in dogs naturally infected by Ehrlichia chaffeensis.
8
In an experimental study of dogs infected
with E. canis, E. chaffeensis, or Ehrlichia ewingii, histologic examination of eyes showed uveitis only in
dogs infected with E. canis.
91
The lymphocytic inflammatory infiltrate was most intense in the ciliary
body, becoming less intense in the choroid, iris, and retina, respectively.
The granulocytic ehrlichial agents E. ewingii and Anaplasma phagocytophilum have not been as
extensively studied as E. canis. However, it appears that they may also be capable of inciting ocular
inflammatory disease in dogs.
105
They cause polyarthritis and meningitis in dogs and would be expected
to cause uveitis. Inflammation at these sites is characteristic of depositing immune complexes or
bloodborne agents such as rickettsiae (see Chapter 28). More information is needed to define the
pathogenesis of these agents, but serum antibody titers that include these agents should be measured in
dogs being evaluated for tickborne disease.
Fig 93-13 E. canisinduced anterior uveitis with hyphema. Iris bombe is
present.
93.2.2.4
93.2.2.4.1
CHAPTER 93 Ocular Infections Page 21 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Thrombocytic Ehrlichiosis
Anaplasma platys (Ehrlichia platys), the agent of canine infectious cyclic thrombocytopenia, is common,
particularly in the southern states. Based on serologic evidence, dogs in Florida and Louisiana have a high
rate of infection.
Uveitis with A. platys infection has been only infrequently reported.
8,44
It is possible that uveitis occurs
more commonly than the literature suggests and is missed. If the organism is not detected within platelets
on a blood smear, an antibody test for A. platys may not be requested for a dog with uveitis. Likewise, if
platelet numbers are not dramatically low, infection with A. platys may not be suspected.
Rocky Mountain Spotted Fever
Ocular lesions are frequently associated with Rocky Mountain spotted fever (RMSF) caused by Rickettsia
rickettsii and primarily arise as a consequence of vasculitis (see Chapter 29). Lesions include conjunctival
hyperemia, subconjunctival hemorrhage, hyphema, anterior uveitis, iris hemorrhage, retinal hemorrhage,
retinal edema, and retinal perivascular inflammatory cell infiltrate (Fig. 93-14). Fluorescein angiography
in experimentally infected dogs demonstrated increased retinal vascular permeability beginning on day 6
after infection and 2 days after the onset of pyrexia.
22
Venules were found to be affected twice as
frequently as arterioles, and smaller vessels were affected more frequently than larger primary vessels.
Retinal vascular lesions in this study paralleled the progression of fever, leukopenia, thrombocytopenia,
and prolongation of activated partial thromboplastin time during the second week after infection.
It is critical to examine the fundus of dogs confirmed or suspected to have RMSF, because the anterior
segment may be normal, although iris hemorrhage and hyphema develop as well. Lesions tend to be
bilateral in affected dogs but may not be symmetrical. Nystagmus may occur in dogs that have vestibular
disease associated with RMSF.
Fig 93-14 Multifocal retinal hemorrhages in a dog with Rocky Mountain
spotted fever.
984
985
93.2.2.4.2
93.2.2.4.3
CHAPTER 93 Ocular Infections Page 22 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
The ocular signs of RMSF may overlap with those of canine ehrlichiosis. Although ocular hemorrhages
are the most common ophthalmic sign of RMSF, hemorrhage may also occur with ehrlichiosis. Although
exceptions occur, intraocular hemorrhages and inflammatory cell infiltrates tend to be less dramatic in
RMSF than ehrlichiosis.
45
Therapy for Rickettsial Disease
Treatment of ocular signs of canine ehrlichiosis must include antiinflammatory therapy in addition to
appropriate systemic antimicrobial therapy (see Chapter 28). Appropriate topical glucocorticoid
preparations for treating anterior uveitis include 1% prednisolone acetate and 0.1% dexamethasone.
Frequency is dictated by the severity of the uveitis, but administration every 6 hours is typically the
minimum desirable frequency. Choroiditis or other posterior segment disease must be treated by the
systemic route and should include an antiinflammatory dose of oral prednisolone. In addition to treating
posterior segment ocular disease, oral glucocorticoids are helpful in reducing other immune-mediated
consequences of ehrlichiosis, such as vasculitis and the production of antiplatelet antibodies that result in
worsening thrombocytopenia.
Ocular lesions in dogs infected with RMSF may resolve quickly with appropriate systemic antibiotic
therapy if they include only small retinal hemorrhages. If more severe uveitis occurs, systemic and topical
glucocorticoid therapy as described for ehrlichiosis should be instituted.
Canine Brucellosis
Brucella canis has been documented as a cause of unilateral or bilateral anterior uveitis and endophthalmitis
and is often accompanied by intraocular hemorrhage. Ocular involvement is often severe and blinding (see
Chapter 40).
48
A retrospective study of the prevalence of ocular lesions among dogs examined for
brucellosis at veterinary schools in the United States and Canada found that 38 of 313 (14.2%) dogs had
ocular involvement.
119
Testing for B. canis should be performed in dogs with unexplained uveitis or ocular
hemorrhage. Therapy consists of systemic antibiotics as well as topical prednisolone acetate for anterior
uveitis. The prognosis for uveitis associated with brucellosis is guarded.
Lyme Borreliosis in Dogs
Lyme disease, or borreliosis, produced by the spirochete Borrelia burgdorferi may cause ocular lesions in
humans, horses, and dogs (see Chapter 45). An increasing number of humans is being diagnosed with ocular
Lyme disease.
79,95
The most common ocular manifestation appears to be uveitis, but neuroophthalmic
disorders and surface inflammations such as episcleritis and keratitis have also been reported. Ocular
manifestations are more likely to be seen in late-stage disease.
A single case report describes isolation of B. burgdorferi, which was isolated from the eye of a pony with
uveitis.
10
However, such documentation is lacking in dogs. In a retrospective review of 132 dogs
seropositive by indirect FA, five had the primary symptom of ocular lesions. Ocular lesions reported were
conjunctivitis, anterior uveitis, corneal edema, retinal petechia, chorioretinitis, and retinal detachment.
16
Follow-up with Western blot was not performed. In this study 24 dogs, were also seropositive for E. canis,
although information was not provided as to whether dogs with ocular disease were positive for ehrlichiosis,
thus it is impossible to ascribe the ocular lesions to borreliosis. Although it is highly likely that Lyme disease
93.2.2.4.4
93.2.2.5
93.2.2.6
CHAPTER 93 Ocular Infections Page 23 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
can cause ocular disease in infected dogs, more definitive information is needed to document the condition.
Diagnosis and treatment of systemic borreliosis are discussed in Chapter 45. Ocular disease should also be
treated with topical prednisolone acetate 4 to 6 times daily for anterior segment inflammation and oral
prednisolone at a dose of 1 to 2 mg/kg/day for posterior segment inflammation.
Leptospirosis in Dogs
Leptospirosis, a spirochete bacterial infection, can affect any organ but has been primarily associated with
renal disease in the dog (see Chapter 44). Leptospires incite vasculitis and endotheliitis, making the eyes a
potential target organ. Although leptospires have been found in the eyes of infected dogs, the paucity of
reports of uveitis associated with canine leptospirosis in the literature probably does not reflect the true
incidence of disease.
30
Leptospirosis is considered a major cause of uveitis in horses and has also been
reported in humans. In these species the development of uveitis often occurs months after acute infection.
This likely represents a delayed hypersensitivity reaction between cell-bound antibodies and persistent
leptospiral antigens in the eye. This delayed response has not been reported in the dog. The author has seen
dogs with anterior uveitis, as well as chorioretinitis with retinal detachment, and high serum titers against
serovars canicola, grippotyphosa, pomona, and bratislava.
Treatment should consist of appropriate systemic antibiotic therapy. Anterior uveitis should be treated with
frequent topical prednisolone acetate, whereas chorioretinitis with or without retinal detachment should be
treated with oral prednisolone at a dose of 1 to 2 mg/kg/day.
Neosporosis in Dogs
Neospora caninum is a protozoal parasite that is morphologically similar to Toxoplasma gondii (see Chapter
80). Transplacental transmission has been documented, and reports in the dog have primarily involved
infections in neonates and puppies younger than 6 months of age. Although puppies die or are euthanized
because of neuromuscular signs, ocular lesions are present in many cases. The ocular lesions are primarily a
retinitis with extension into the choroid (retinochoroiditis). A mild anterior uveitis was also reported.
28
Leishmaniasis in Dogs
The dog is a reservoir host for the protozoal organism Leishmania donovani in endemic areas of the
Mediterranean, Africa, and Asia (see Chapter 73). Most documented cases in North America have been in
dogs imported from endemic areas, but reports involving a closed research colony of English foxhounds in
Ohio and Oklahoma indicated that once introduced, the agent can be transmitted in the United States.
113
Leishmaniasis was diagnosed in a Maryland poodle that had not traveled outside the United States.
31
Ocular and periocular lesions associated with leishmaniasis developed in 25% of 105 dogs in a study.
94
In
15% of the dogs in the study, ocular lesions were the only clinical sign. Clinical ocular disease, in decreasing
order of frequency, included anterior uveitis, conjunctivitis, keratoconjunctivitis, periocular alopecia, diffuse
blepharitis, posterior uveitis, orbital cellulitis, and a solitary eyelid nodule.
The diagnosis is made by histopathologic identification of the organism, serologic testing, PCR testing, or all
of these. In dogs with conjunctivitis, scraping and cytologic examination have revealed the organism in some
cases. The inflammation is mononuclear, and the organism is found within histiocytes.
985
986
93.2.2.7
93.2.2.8
93.2.2.9
CHAPTER 93 Ocular Infections Page 24 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Therapy is discussed in Chapter 73. In addition to systemic antiprotozoal therapy, keratoconjunctivitis or
uveitis should be treated with topical prednisolone acetate several times daily. Blepharitis can be treated with
a topical ophthalmic antibiotic-dexamethasone ointment that is rubbed into the skin several times daily,
whereas posterior uveitis should be treated with oral prednisolone at a dose of 1 to 2 mg/kg/day.
Other Bacterial Infections of Dogs
Septicemias caused by various bacteria may affect the eyes. Infections such as bacterial endocarditis, urinary
tract infection, pyometra, and dental infection may cause uveitis through hematogenous spread of bacteria to
the eye. Simultaneously cleaning teeth and performing intraocular surgery should be avoided to minimize the
risk of bacteria localizing in injured ocular tissue. Contagious bacterial infections such as tuberculosis and
salmonellosis may also manifest with ocular lesions.
Mycoses of Dogs and Cats
The systemic mycoses in North America are frequently associated with a granulomatous posterior uveitis.
Anterior uveitis accompanies chorioretinitis in a large number of cases. With the exception of
cryptococcosis, systemic fungal infections are less common in the cat than the dog; however, when they
develop, ocular lesions are often present. In many animals, the ocular signs are the primary symptom.
In indigenous regions of the Mississippi and Ohio Rivers and the central Atlantic states, Blastomyces
dermatitidis is common in dogs (see Chapter 59). Ocular involvement occurs in up to 52% of the cases.
6
Ocular lesions are from chorioretinitis, which may vary from a focal granuloma in the fundus to widespread
subretinal infiltrates of organisms and granulomatous inflammation (Fig. 93-15).
11
Anterior uveitis is
common with extensive posterior segment disease, although the organism is not usually found in these
tissues or in aqueous humor aspirates; however, in cases with endophthalmitis and granulomas in the anterior
segment, the organism is widespread within the eye (Fig. 93-16). Secondary glaucoma is a frequent
complication.
Histoplasma capsulatum infection develops most commonly in the Ohio, Missouri, and Mississippi River
valleys but has been reported in many states in North America (see Chapter 60). As evidenced by published
reports, ocular involvement with histoplasmosis is relatively rare in dogs.
48
In the cat, systemic
histoplasmosis causes nonspecific clinical signs such as weight loss, anorexia, fever, and anemia. Ocular
lesions occur in a fairly high percentage of affected cats and include granulomatous chorioretinitis, retinal
detachment, anterior uveitis, and secondary glaucoma.
43
93.2.2.10
93.2.2.11
CHAPTER 93 Ocular Infections Page 25 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-15 Large subretinal granuloma and retinal hemorrhage in a dog with
blastomycosis.
Fig 93-16 Endophthalmitis caused by blastomycosis in a cat. Note granuloma
in anterior chamber. (Courtesy Sheryl Krohne, West Lafayette, Ind.)
CHAPTER 93 Ocular Infections Page 26 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Coccidioides immitis is endemic in the southwestern United States, Mexico, and Central and South America
(see Chapter 62). Ocular lesions are similar to those of blastomycosis, namely granulomatous chorioretinitis,
retinal detachment, anterior uveitis, and secondary glaucoma. Organisms are found predominantly in the
choroid. Limited data exist regarding the prevalence of ocular lesions in dogs and cats with
coccidioidomycosis. Ocular lesions may be the presenting sign in up to 42% of dogs, and in 80% of dogs the
lesions are unilateral.
4
One study found that 13% of 48 cats had ocular lesions.
46
Cryptococcus neoformans is the most commonly reported feline mycotic infection and enters the body
through the respiratory tract (see Chapter 61). This mycotic infection is common in dogs as well.
Chorioretinitis with granulomatous inflammation and retinal detachment is the most common manifestation;
anterior uveitis is less common. The appearance of chorioretinal lesions is often somewhat different than the
other mycotic infections. Tapetal lesions are usually dark gray in color, in contrast to the whitish appearance
of most fungal granulomas (Fig. 93-17). Optic neuritis may also develop, particularly if the CNS is involved.
A feline case of adnexal cryptococcus without intraocular or systemic lesions has been described.
73
Fig 93-17 Multifocal subretinal granulomas in a dog with cryptocococcis.
Larger lesions are producing small bullous detachments.
Bilateral granulomatous chorioretinitis or endophthalmitis should suggest the possibility of systemic
mycoses. Associated systemic signs of fever and respiratory, skeletal, dermatologic, or CNS involvement are
often present. The specific diagnosis is often made by finding the organism in tissue aspirates. Vitreal
centesis in an eye with endophthalmitis may be the best method of diagnosis if other sites are unyielding.
Therapy for ocular involvement with the systemic mycoses includes appropriate systemic antifungal therapy
as discussed in Chapter 57. In many instances the ocular inflammatory reaction continues to worsen with
systemic therapy because of the immune reaction to the dying organisms. The use of oral prednisolone at a
dose of 1 to 2 mg/kg/day has been extremely valuable in halting this vision-threatening inflammatory
response. Oral prednisolone should be continued until fundic lesions completely resolve, which may take
986
987
CHAPTER 93 Ocular Infections Page 27 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
several weeks to months.
59
If anterior uveitis is present, topical prednisolone acetate should be used several
times daily, tapering once the overall disease is in remission.
Enucleation of blind eyes has been proposed as a means of eliminating a nidus of infection that may cause
relapses. Although it is justifiable to remove a blind, painful eye (such as one with glaucoma), no
rationalization can be made for removing an eye that has been affected by blastomycosis but is comfortable.
Protothecosis in Dogs and Cats
Prototheca species are ubiquitous algae in soil and water and occasionally pathogenic in dogs and cats (see
Chapter 69). More than 50% of affected dogs have ocular involvement,
78
whereas ocular lesions have not
been reported in cats. Most dogs with ocular lesions also have systemic signs such as diarrhea, but in some
instances the systemic signs are inapparent or missed. Lesions include a granulomatous posterior uveitis,
often with retinal detachment, that is similar in appearance to those associated with fungal infections like
blastomycosis. Anterior uveitis is often present as well. Definitive diagnosis is usually made by finding the
organism in aspirates, urine sediment, or biopsy samples. Vitreous centesis often yields the organism in dogs
with ocular protothecosis. No efficacious therapy has been reported.
Toxoplasmosis in Cats and Dogs
Generalized toxoplasmosis has been associated with ocular inflammation in cats and dogs (see Chapter 80).
The most prominent lesion is choroiditis with extension into the retina.
20
These lesions typically appear as
multifocal dark gray infiltrates in the tapetal fundus and fluffy white infiltrates in the nontapetal fundus.
Anterior uveitis also occurs, and T. gondii bradyzoites and tachyzoites have been identified
histopathologically in the iris and ciliary body of systemically affected cats.
28
The ability of T. gondii to cause ocular disease without systemic disease is poorly understood. The fact that
many cats have positive serum antibody titers to T. gondii, particularly IgG, makes it difficult to correlate
uveitis alone with toxoplasmosis. It is possible that T. gondii may incite an im-mune-mediated uveitis
without systemic disease. Several mechanisms have been proposed, including homing of activated immune
cells to ocular tissues, molecular mimicry, circulating antigens or immune complexes from nonocular sites of
parasite replication, and a nonspecific increase in immune response.
20,23
In kittens experimentally infected in
utero or in the early neonatal period, chorioretinitis and anterior uveitis developed without other evidence of
clinical illness.
97
Serologic testing for T. gondii should include IgM and IgG. IgM increases and decreases for 3 months after
infection, whereas IgG stays elevated for years. Cats coinfected with FIV and T. gondii may develop a
positive IgM titer, whereas the IgG titer remains negative.
65
T. gondii-specific antibodies can be measured in aqueous humor. Antibody levels can be compared with
serum levels through use of the Witmer-Goldman coefficient, or C-value. C-values of greater than 8 suggest
intraocular antibody production and may be more helpful than serum titers alone in diagnosing ocular
toxoplasmosis. Aqueous humor can also be evaluated by PCR for the presence of T. gondii DNA.
74
Treatment of ocular toxoplasmosis in cats and dogs should include clindamycin at a dose of 12.5 mg/kg
every 12 hours for 21 to 30 days.
64
The uveitis should also be treated with antiinflammatory agents such as
93.2.2.12
93.2.2.13
CHAPTER 93 Ocular Infections Page 28 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
topical prednisolone acetate or a nonsteroidal ophthalmic preparation several times daily for anterior uveitis.
Chorioretinitis should be treated with oral prednisolone at a dose of 1 to 2 mg/kg/day until resolution.
Feline Immunodeficiency Virus
Ocular inflammation has been associated with FIV in experimentally and naturally infected cats (see Chapter
14). Anterior uveitis is the most commonly reported ocular abnormality. Conjunctivitis, pars planitis, and
chorioretinitis have also been reported. Ocular inflammation may be caused by direct viral damage to tissue,
initiating immune-mediated disease, or allowing opportunistic infections to develop.
125
Other common feline
pathogens, such as herpesvirus, C. felis, and T. gondii, that can cause ocular disease should be considered in
FIV-positive cats. In an experimental study of chlamydial conjunctivitis, coinfection with FIV markedly
prolonged the duration of clinical signs and led to chronic conjunctivitis.
Serologic evidence of coinfection with T. gondii was present in 28 (57%) of 49 FIV-positive cats in one
study.
90
Approximately 43% of cats coinfected with FIV and T. gondii had positive T. gondiispecific IgM
serum antibody titers without a positive T. gondiispecific IgG titer.
If another infectious disease can be identified in an FIV-positive cat, it should be treated as specifically as
possible. Uveitis caused by FIV can be expected to be a chronic problem. Treatment should be symptomatic
and include topical antiinflammatory agents such as prednisolone acetate or a nonsteroidal agent such as
flurbiprofen. For long-term use, a topical nonsteroidal drug is preferred because of the risk of exacerbating
ocular herpesvirus with glucocorticoids. Oral prednisolone may be required for chorioretinitis. The author's
experience in treating pars planitis has been poor.
Feline Infectious Peritonitis Virus
The most common ocular manifestation of infection with feline infectious peritonitis virus (FIPV) is bilateral
granulomatous anterior uveitis, often accompanied by chorioretinitis (see Chapter 11). Frequently, large
keratic precipitates and a fibrinous exudate are found in the anterior chamber (Fig. 93-18). The nature of the
disease is a vasculitis, and it is common to see a pyogranulomatous exudate sheathing the retinal vessels
(Fig. 93-19). Retinal hemorrhages and detachments may also develop.
Ocular disease is more common with the noneffusive, or dry, form of FIPV infection and may be the initial
presenting sign. Diagnosis of FIPV-associated ocular disease is difficult because of the nonspecific nature of
available coronavirus serum antibody tests. Rising serum antibody titers in the presence of characteristic
ocular lesions is suggestive.
Because no effective treatment exists for FIPV infection, treatment of ocular disease is symptomatic. Topical
glucocorticoids such as prednisolone acetate should be used several times daily for anterior uveitis. Systemic
prednisolone should be used for chorioretinitis. Ocular disease may be temporarily ameliorated, but it usually
recurs if the systemic disease worsens.
Feline Leukemia Virus
The predominant ocular manifestation of feline leukemia virus infection is lymphosarcoma (see Chapter
13).
9
The uveal tract is a common site for metastasis of neoplastic lymphocytes via hematogenous spread.
Cats with ocular lymphosarcoma may initially show signs of mild uveitis, including miosis, aqueous flare,
987
988
93.2.2.14
93.2.2.15
93.2.2.16
CHAPTER 93 Ocular Infections Page 29 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
and keratic precipitates. As the disease progresses, the iris becomes greatly thickened and distorted with the
infiltration of tumor cells. Glaucoma is a common sequela because tumor cells infiltrate the iridocorneal
angle. Aqueous centesis may be helpful in making the diagnosis, because neoplastic lymphocytes readily
exfoliate into the aqueous humor. In addition to intraocular involvement, invasion of the orbit by
lymphosarcoma may occur. Aggressive treatment of cats with ocular lymphosarcoma with topical
glucocorticoids, such as prednisolone acetate, as well as systemic therapy with glucocorticoids and other
chemotherapeutic protocols can result in improvement.
Fig 93-18 Anterior uveitis with large keratic precipitates in a cat with feline
infectious peritonitis.
Diagnosis
Aqueous Centesis
Aqueous centesis can be performed using heavy sedation or general anesthesia. A 27- to 30-gauge needle on
a tuberculin syringe should be used with the seal broken so that movement of the plunger is smooth. The
site of centesis is usually at the dorsal or lateral limbus because it is the most accessible. Topical
proparacaine should be used even with sedation. A cotton-tip swab soaked in proparacaine and held at the
site of centesis for 60 seconds before insertion of the needle facilitates the procedure. Forceps applied to the
conjunctiva close to the limbus should be used to fixate the globe and apply counter pressure to the needle.
The needle enters the cornea just rostral to the limbus and parallel to the plane of the iris (Fig. 93-20). The
operator must be careful to avoid the iris, lens, and corneal endothelium. The procedure may be more
hazardous in the diseased cornea because the needle point is obscured, and the increased corneal thickness
results in a longer, beveled tract before the needle enters the anterior chamber. Unless the anterior chamber is
collapsed, the volume that can be removed from the dog is about 0.3 ml and from the cat is about 0.5 ml. A
culture swab is saturated with a portion of the aspirated aqueous, and the remaining aliquot is prepared for
93.2.3
93.2.3.1
CHAPTER 93 Ocular Infections Page 30 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
cytology by centrifugation. If fibrin is present or iris adhesions of less than a few days duration are present,
25 g of tissue plasminogen activator (tPA) may be injected to dissolve clots and break synechiae.
72
Vitreous Centesis
Centesis of the vitreous cavity has more potential complications than aqueous centesis and is usually
reserved for eyes that have lost considerable visual function. Choroidal hemorrhage and retinal tears are the
two most likely complications. A 25- to 22-gauge needle with a 3-ml syringe should be used. The site of
entry is 6 mm caudal to the limbus in the dorsolateral quadrant. Forceps are used to apply counter pressure,
and the needle point is aimed posteriorly away from the lens and toward the center of the vitreous cavity
(Fig. 93-21). The needle should be short (0.5 inch) so that it does not inadvertently pass completely across
the vitreous humor and tear the opposite retina. Approximately 0.5 ml of vitreous humor can be removed for
culture and cytology. If fluid cannot be obtained, minor positioning changes of the needle point should be
attempted.
Fig 93-19 Chorioretinitis and retinal perivascular sheathing in a cat with feline
infectious peritonitis.
988
989
93.2.3.2
CHAPTER 93 Ocular Infections Page 31 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Fig 93-20 Aqueous centesis in a dog. A 27- to 30-gauge needle enters at
limbus, avoiding iris and corneal endothelium.
Fig 93-21 Vitreous centesis in a dog. Needle enters 6 mm posterior to limbus
and is directed slightly posterior and toward center of globe.
Therapy
The therapeutic routes available for treating ocular infections and inflammations are topical, subconjunctival,
intraocular, and systemic. The routes selected depend on the location, severity of the infection, and the drug
being administered. The eye has three barriers to drug penetration: the intact cornea for topical penetration and
the blood-aqueous and blood-retinal barriers for systemic drug penetration. In general, drugs with a differential
solubility in water and lipids and small molecular size are better able to penetrate these barriers. Inflammation
or ulceration weaken these barriers to variable degrees and allow better penetration. The ability of antibiotics to
penetrate into the normal eye varies by drug and route (Table 93-6).
53
The vitreous humor is a large, rather inert
93.2.4
CHAPTER 93 Ocular Infections Page 32 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
structure, resulting in low drug levels by any route of drug administration except direct intravitreal injection, in
which the vitreous humor acts as a depot for the relatively slow release of the drug.
Topical
Depending on the drug and whether the cornea is intact, topical therapy may provide adequate drug levels
only on the surface or as deep as the iris and ciliary body. Epithelial defects of 25% to 50% increase drug
penetration into the corneal stroma and aqueous by nine times, but larger defects do not produce an
additional increase.
56
Other variables influencing drug concentrations via topical administration are the
frequency of application, drug contact time, and drug concentration. Solutions are generally easier to apply
to a painful eye and therefore are preferred in terms of compliance. To a point, a higher drug concentration
increases the absorption. However, concentrated drugs may increase reflex lacrimation and become diluted
by osmotically drawing fluid from the tissues.
When solutions are used, one drop (about 30 to 50 l) of a preparation is adequate. Multiple or rapidly
repeated instillations of the same or different preparations simply increase the rate of loss via the NL duct or
mutually dilute each preparation, thereby reducing the availability of each drug. Waiting an interval of at
least 5 minutes between instillation of multiple drugs is preferred to allow reflex tearing to subside and
prevent dilution of the previous drop.
Treatment of routine surface infections of the conjunctiva or prophylactic antibacterial therapy of corneal
ulcers should include topical broad-spectrum antibiotics such as neomycin-polymyxin-bacitracin that are not
applied systemically. This rationale is based on minimizing bacterial resistance to antibiotics that are
beneficial in systemic therapy and avoiding sensitization of a patient by a topical antibiotic that might have
potential in systemic therapy.
Reports have begun to emerge of anaphylactic reactions in cats after administration of topical
bacitracin-neomycin-polymixin B preparations.
96
Most cases have been fatal, thus it would be best not to use
this formula in cats.
Subconjunctival
Subconjunctival administration of antibiotics or antiinflammatories is used primarily for anterior segment
disease and can achieve therapeutic intraocular levels of medication. The major limitations of
subconjunctival injections are drug irritation and ocular manipulation. The means by which a
subconjunctivally injected drug reaches the interior of the eye are controversial, but direct diffusion through
the sclera, which has no epithelial barrier as the cornea does, and leakage through the needle hole with
topical absorption have been demonstrated. Except for long-acting drugs, most others must be readministered
at 12- to 24-hour intervals to maintain therapeutic levels. Typically a single injection of a subconjunctival
drug is administered, followed by topical agents, systemic agents, or both.
Drugs should be injected under the bulbar conjunctiva, not the palpebral conjunctiva. The dorsal 12 oclock
position is easiest to access. Adequate topical anesthesia is required. A proparacaine soaked cotton-tip swab
should be held at the injection site for at least 60 seconds, followed by slow injection of drug with a
25-gauge needle. In many animals, this can be accomplished without sedation, although sedation may be
required in some. In dogs and cats a volume of 0.2 to 0.5 ml can be administered, creating a bleb that
resolves in a few hours.
93.2.4.1
93.2.4.2
CHAPTER 93 Ocular Infections Page 33 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
Whereas significant posterior segment levels of drugs can be obtained when injecting near the equator of the
globe, the subconjunctival route is not adequate for bacterial infections of the vitreous or optic nerve.
Subconjunctival dosages vary by antibiotic (see Appendix 9).
Table 93-6 Intraocular Penetration of Antibacterial Agents in the Uninflamed
Eye
PENETRATION BY ROUTE
AGENT SYSTEMIC TOPICAL SUBCONJUNCTIVAL
Penicillin Poor Poor Good
Ampicillin Poor Poor Good
Methicillin Good (multiple dose) NA Good
Erythromycin Poor Good Good
Cephalosporins Poor Poor Good
Enrofloxacin Good NA NR
Gentamicin Poor Poor Good
Tobramycin Poor Poor Good
Lincomycin Good NA NA
Neomycin NA Poor NA
Choramphenicol Fair Good Good
Tetracycline Poor Good NA
Doxycycline Good NA NA
Bacitracin NA Poor Poor
Polymyxin B NA Poor NA
Trimethoprim-sulfadiazineGood Good Good
Sulfonamides (in general) Good Good Good
Ciprofloxacin Good Good NR
Ofloxacin NA Good Good
NA, Not available in a form for route of administration; NR, not recommended due to retinal toxicity.
Intraocular
Intracameral or intraocular injection of antibiotics is a heroic and an extremely effective means of obtaining
high levels of intraocular antibiotics for the treatment of bacterial endophthalmitis. If vision is to be
preserved, the decision to use the intracameral route must be made early to avoid rapidly devastating
inflammation to delicate intraocular structures. Because culture and susceptibility testing results are not
available for a few days, a broad-spectrum bactericidal antibiotic is usually administered.
The use of intravitreal vancomycin is common in human medicine for the treatment of bacterial
endophthalmitis following injury or intraocular surgery. Dosages of 1 mg (0.1 ml) of vancomycin have been
injected into the vitreous, along with 2.25 mg (0.1 ml) ceftazidime or 0.4 mg (0.1 ml) amikacin.
34,38,99
Typically, vancomycin is also administered intravenously. The intracameral injection of the drug
combination can be repeated 3 to 4 days later.
Systemic
The systemic route of therapy is indicated in cases of chorioretinitis and optic neuritis, because topical or
subconjunctival application does not result in therapeutic levels of drug in these tissues. Many drugs are
989
990
93.2.4.3
93.2.4.4
CHAPTER 93 Ocular Infections Page 34 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
unable to cross the blood-retinal or blood-aqueous barrier, although some agents have good ocular
penetration (see Table 93-6). However, in animals with inflammation, most drugs administered systemically
do penetrate the eye. Antiinflammatory agents such as prednisolone, carprofen, and aspirin reach therapeutic
levels in inflamed ocular tissue. Likewise, most antibiotics reach therapeutic intraocular levels when the
blood-aqueous and blood-retinal barriers are disrupted by inflammation. Of the systemically administered
antifungal azole compounds, fluconazole penetrates the eye and CNS best. Itraconazole has also been
effective in many animals for treating systemic mycoses such as blastomycosis with ocular involvement.
In some cases, administration of a systemic medication may have an adverse effect on the eye. Systemic
fluoroquinolones penetrate normal ocular tissue and have the potential to damage the retina. Some cats
receiving systemic enrofloxacin (oral or injectable) have developed acute retinal degeneration and permanent
blindness.
39,123
This has been most notable in cats receiving greater than the recommended dose of 5
mg/kg/day. However, even lower doses may cause retinal degeneration in some cats, particularly older or
debilitated animals, and all systemically administered fluoroquinolones should be viewed as potentially
retinotoxic.
Adjunctive
In addition to specific antimicrobial therapy, standard nursing care involves cleansing of the ocular surface
and lids with warm, moist swabs or using hot packing if lid and orbital swelling is evident. Systemic
nonsteroidal agents such as carprofen or aspirin (for dogs only) are analgesic and lessen the inflammatory
reaction. Topical atropine minimizes ocular pain from ciliary muscle spasms and helps prevent synechia;
however, atropine should not be used if KCS, glaucoma, or iridocorneal angle compromise are present.
Injection of 25 g of tPA into the anterior chamber is an effective and dramatic means of breaking down
adhesions and dissolving fibrin clots if given within 3 to 7 days of formation. Once the clot is organized, the
efficacy is lost. If active or recent bleeding has occurred in the eye, intraocular rebleeding may occur after
injection of tPA. Injections may be repeated if necessary. Injection of tPA into the vitreous humor is not as
safe because of retinal toxicity.
Suggested Readings
*
* See the CD-ROM for a complete list of references.
91. Panciera, RJ, Ewing, SA, Confer, AW: Ocular histopathology of ehrlichial infections in the dog. Vet
Pathol. 38, 2001, 4346.
94. Pena, MT, Roura, X, Davidson, MG: Ocular and periocular manifestations of leishmaniasis in dogs: 105
cases (1993-1998). Vet Ophthalmol. 3, 2000, 3541.
97. Powell, CC, Lapin, MR: Clinical ocular toxoplasmosis in neonatal kittens. Vet Ophthalmol. 4, 2001,
8792.
103. Sparkes, AH, Caney, SM, Sturgess, CP, et al.: The clinical efficacy of topical and systemic therapy for
the treatment of feline ocular chlamydiosis. J Feline Med Surg. 1, 1999, 3135.
110. Stiles, J, Townsend, WM, Rogers, QR, et al.: Effect of oral administration of L-lysine on conjunctivitis
caused by feline herpesvirus in cats. Am J Vet Res. 63, 2002, 99103.
116. Townsend, WM, Stiles, J, Guptill-Yoran, L, et al.: Development of a reverse transcriptase-polymerase
chain reaction assay to detect feline herpesvirus-1 latency-associated transcripts in the trigeminal ganglia
and corneas of cats that did not have clinical signs of ocular disease. Am J Vet Res. 65, 2004, 314319.
93.2.4.5
93.3
CHAPTER 93 Ocular Infections Page 35 of 36
Infectious Diseases of the Dog and Cat, 3rd Edition
119. Vinayak, A, Greene, CE, Moore, PA, et al.: Clinical resolution of Brucella canis-induced ocular
inflammation in a dog. J Am Vet Med Assoc. 224, 2004, 18041807.
Uncited references
54. Helps, C, Reeves, N, Egan, K, et al.: Detection of Chlamydophila felis and feline herpesvirus by
multiplex real-time PCR analysis. J Clin Microbiol. 41, 2003, 27342736.
69. Maggs, DJ, Nasisse, MP, Kass, PH: Efficacy of oral supplementation with L-lysine in cats latently
infected with feline herpesvirus. Am J Vet Res. 64, 2003, 3742.
990
991
93.4
CHAPTER 93 Ocular Infections Page 36 of 36
You might also like
- Cryptococcosis ManualDocument3 pagesCryptococcosis Manualnassem54No ratings yet
- Papular Urticaria FIXDocument13 pagesPapular Urticaria FIXbungagladysNo ratings yet
- Insects and Allergic Reactions: ) Department of Parasitology Faculty of Medicine, Trisakti UniversityDocument7 pagesInsects and Allergic Reactions: ) Department of Parasitology Faculty of Medicine, Trisakti UniversityFenty SuwidakNo ratings yet
- Insects and Allergic Reactions FixDocument10 pagesInsects and Allergic Reactions FixFenty SuwidakNo ratings yet
- Proceeding of The SEVC Southern European Veterinary ConferenceDocument4 pagesProceeding of The SEVC Southern European Veterinary ConferenceHartina SamosirNo ratings yet
- Clostridial infections-LR3Document8 pagesClostridial infections-LR3yomifNo ratings yet
- Bheesam KumarDocument4 pagesBheesam KumardileepNo ratings yet
- Papular UrticariaDocument10 pagesPapular UrticariaNuri Sakina SuhartoNo ratings yet
- Prepared By: Ken Robin A. Canada, RMT, Mls AscpiDocument35 pagesPrepared By: Ken Robin A. Canada, RMT, Mls AscpiKen Robin CanadaNo ratings yet
- ConjunctivitisDocument113 pagesConjunctivitisHussam AliNo ratings yet
- KeratitisDocument26 pagesKeratitisHIDAYATUL RAHMINo ratings yet
- Canine DistemperDocument18 pagesCanine DistemperJ Elver SilvaNo ratings yet
- ConjunctivitisDocument27 pagesConjunctivitisElukoti BhosleNo ratings yet
- CakirDocument7 pagesCakircherruskaNo ratings yet
- Chapter 5 Bacterial Diseases of Ruminants 2020Document30 pagesChapter 5 Bacterial Diseases of Ruminants 2020JAD IMADNo ratings yet
- Bheesam KumarDocument4 pagesBheesam KumardileepNo ratings yet
- MICROBIOLOGY Pathogenic Gram-Positive Bacilli (Corynebacterium)Document7 pagesMICROBIOLOGY Pathogenic Gram-Positive Bacilli (Corynebacterium)Ravindra SinghNo ratings yet
- Gram Positive Cocci StaphylococciDocument41 pagesGram Positive Cocci StaphylococciZainab ElgehaniNo ratings yet
- Gram Positive BacilliDocument6 pagesGram Positive BacilliSteve ShirmpNo ratings yet
- Practical 4 Staphylococci PresentationDocument24 pagesPractical 4 Staphylococci PresentationPatrisha BuanNo ratings yet
- Taenia SoliumDocument2 pagesTaenia SoliumGlazy Kim SecoNo ratings yet
- Clinical Avian Nutrition Excerpt PDFDocument22 pagesClinical Avian Nutrition Excerpt PDFAlejandraNo ratings yet
- Echinococcosis AsiyaDocument20 pagesEchinococcosis AsiyaBiswadeepan AcharyaNo ratings yet
- Viro Final 6Document10 pagesViro Final 6Muhammad Arslan UsmanNo ratings yet
- NocardiaDocument3 pagesNocardiasujithas0% (1)
- PneumococcusDocument29 pagesPneumococcusThe tooth fairyNo ratings yet
- Bacterial Keratitis: Signs and SymptomsDocument4 pagesBacterial Keratitis: Signs and Symptoms]]]100% (1)
- Canine Viral InfectionDocument15 pagesCanine Viral InfectionNathalia gallegoNo ratings yet
- 792 Viral Protozoal Corneal UlcerDocument33 pages792 Viral Protozoal Corneal UlcerMounika PapireddyNo ratings yet
- GinecologíaDocument5 pagesGinecologíaLeonela SánchezNo ratings yet
- Neoformans. Cryptococcosis Caused by C. Neoformans Is Commonly Seen inDocument9 pagesNeoformans. Cryptococcosis Caused by C. Neoformans Is Commonly Seen inLeah CamangonNo ratings yet
- Topic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"Document26 pagesTopic: "Picoronoviruses. Coxsackie. ECHO. Laboratory Diagnostics"deekshit dcNo ratings yet
- Contagious Bovine PleuropneumoniaDocument16 pagesContagious Bovine PleuropneumoniaMuhammad Saif KhanNo ratings yet
- Fowl PoxDocument3 pagesFowl PoxakhmadfuadiNo ratings yet
- Impetigo - Review : Luciana Baptista Pereira1Document7 pagesImpetigo - Review : Luciana Baptista Pereira1Edwar RevnoNo ratings yet
- HGJK J LHB, JKDocument4 pagesHGJK J LHB, JKChandra Noor RachmanNo ratings yet
- DiphtheriaDocument10 pagesDiphtheriakudzaimuregidubeNo ratings yet
- Contagious Ecthyma: Orf, Contagious Pustular Dermatitis, Sore Mouth, Scabby MouthDocument27 pagesContagious Ecthyma: Orf, Contagious Pustular Dermatitis, Sore Mouth, Scabby MouthMohammedNo ratings yet
- Lecture7 Medical Mycology - YeastsDocument32 pagesLecture7 Medical Mycology - YeastsKarthick AnbuNo ratings yet
- JEADV Clinical Practice - 2022 - Absil - Scabies and Therapeutic Resistance Current Knowledge and Future PerspectivesDocument8 pagesJEADV Clinical Practice - 2022 - Absil - Scabies and Therapeutic Resistance Current Knowledge and Future Perspectivestravel doctorNo ratings yet
- Neisseriaceae FamilyDocument15 pagesNeisseriaceae FamilyHamidreza RahmaniNo ratings yet
- Review Article Systemic Treatment of Bacterial Skin Infections of Dogs and CatsDocument11 pagesReview Article Systemic Treatment of Bacterial Skin Infections of Dogs and CatsAma&ran& MizNo ratings yet
- Diphtheria Pertussis TetanusDocument43 pagesDiphtheria Pertussis Tetanuspnalinl108No ratings yet
- Ecthyma Contagiosum (Human Orf)Document2 pagesEcthyma Contagiosum (Human Orf)Deba P SarmaNo ratings yet
- Lauren R. Pinchbeck, DVM, MS, DACVD South Texas Veterinary Allergy & Dermatology, San Antonio, TX, USADocument4 pagesLauren R. Pinchbeck, DVM, MS, DACVD South Texas Veterinary Allergy & Dermatology, San Antonio, TX, USADonny ArtikaNo ratings yet
- AdenovirusDocument14 pagesAdenoviruszoomar muzammilNo ratings yet
- Ocular and Periocular Manifestations of Leishmaniasis in Dogs: 105 Cases (1993 1998)Document7 pagesOcular and Periocular Manifestations of Leishmaniasis in Dogs: 105 Cases (1993 1998)soledadDC329No ratings yet
- Toxoplasmosis AaoDocument28 pagesToxoplasmosis AaoUNHAS OphthalmologyNo ratings yet
- Immunoproteomic Approach To Elucidating The Pathogenesis of Cryptococcosis Caused by Cryptococcus GattiiDocument10 pagesImmunoproteomic Approach To Elucidating The Pathogenesis of Cryptococcosis Caused by Cryptococcus GattiiGabriella FreitasNo ratings yet
- Pyrexia of Unknown OriginDocument55 pagesPyrexia of Unknown OriginsanjeevNo ratings yet
- Overview of Infectious Laryngotracheitis in Poultry: Veterinary ManualDocument2 pagesOverview of Infectious Laryngotracheitis in Poultry: Veterinary ManualSamapanNo ratings yet
- IMPETIGODocument10 pagesIMPETIGOafifulichwan18No ratings yet
- ch28Document63 pagesch28Renata CezarNo ratings yet
- Glanders: C H A P T E R 2 - 5 - 1 1Document10 pagesGlanders: C H A P T E R 2 - 5 - 1 1Ryan ChenNo ratings yet
- Staphylococci: R.Varidianto Yudo T., DRDocument36 pagesStaphylococci: R.Varidianto Yudo T., DRIndra MahaputraNo ratings yet
- 2.03.10 FowlpoxDocument7 pages2.03.10 FowlpoxJulius MwanandotaNo ratings yet
- Brucella BaronDocument12 pagesBrucella BaronMeghana SharmaNo ratings yet
- Infectious DiseaseDocument33 pagesInfectious DiseaseebraheemelmandouhNo ratings yet
- 911 Pigeon Disease & Treatment Protocols!From Everand911 Pigeon Disease & Treatment Protocols!Rating: 4 out of 5 stars4/5 (1)
- Veterinaria HomeopáticaDocument424 pagesVeterinaria HomeopáticaAegtvvra Ervrvtwrv100% (2)
- 10Document6 pages10soledadDC329No ratings yet
- 5Document9 pages5soledadDC329No ratings yet
- Use of Thromboelastography in Dogs With Immune-Mediated Hemolytic Anemia: 39 Cases (2000 2008)Document5 pagesUse of Thromboelastography in Dogs With Immune-Mediated Hemolytic Anemia: 39 Cases (2000 2008)soledadDC329No ratings yet
- 6Document8 pages6soledadDC329No ratings yet
- 11Document6 pages11soledadDC329No ratings yet
- EsterilizacionDocument2 pagesEsterilizacionsoledadDC329No ratings yet
- The Effect of Hetastarch (670/0.75) in Vivo On Platelet Closure Time in The DogDocument6 pagesThe Effect of Hetastarch (670/0.75) in Vivo On Platelet Closure Time in The DogsoledadDC329No ratings yet
- 1Document15 pages1soledadDC329No ratings yet
- 11Document6 pages11soledadDC329No ratings yet
- 3Document12 pages3soledadDC329No ratings yet
- 13Document5 pages13soledadDC329No ratings yet
- Noninvasive Ventilation in Cats: Original StudyDocument10 pagesNoninvasive Ventilation in Cats: Original StudysoledadDC329No ratings yet
- 9Document6 pages9soledadDC329No ratings yet
- A Comparison of Total Calcium, Corrected Calcium, and Ionized Calcium Concentrations As Indicators of Calcium Homeostasis Among Hypoalbuminemic Dogs Requiring Intensive CareDocument8 pagesA Comparison of Total Calcium, Corrected Calcium, and Ionized Calcium Concentrations As Indicators of Calcium Homeostasis Among Hypoalbuminemic Dogs Requiring Intensive CaresoledadDC329No ratings yet
- Evaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)Document6 pagesEvaluation of Fresh Frozen Plasma Administration in Dogs With Pancreatitis: 77 Cases (1995 2005)soledadDC329No ratings yet
- Effect of Antivenin Dose On Outcome From Crotalid Envenomation: 218 Dogs (1988 2006)Document8 pagesEffect of Antivenin Dose On Outcome From Crotalid Envenomation: 218 Dogs (1988 2006)soledadDC329No ratings yet
- 6Document15 pages6soledadDC329No ratings yet
- 1Document9 pages1soledadDC329No ratings yet
- Effect of Antivenin Dose On Outcome From Crotalid Envenomation: 218 Dogs (1988 2006)Document8 pagesEffect of Antivenin Dose On Outcome From Crotalid Envenomation: 218 Dogs (1988 2006)soledadDC329No ratings yet
- 5Document9 pages5soledadDC329No ratings yet
- 3Document7 pages3soledadDC329No ratings yet
- A Comparison of Total Calcium, Corrected Calcium, and Ionized Calcium Concentrations As Indicators of Calcium Homeostasis Among Hypoalbuminemic Dogs Requiring Intensive CareDocument8 pagesA Comparison of Total Calcium, Corrected Calcium, and Ionized Calcium Concentrations As Indicators of Calcium Homeostasis Among Hypoalbuminemic Dogs Requiring Intensive CaresoledadDC329No ratings yet
- Endoscopically Guided Nasojejunal Tube Placement in Dogs For Short-Term Postduodenal FeedingDocument10 pagesEndoscopically Guided Nasojejunal Tube Placement in Dogs For Short-Term Postduodenal FeedingsoledadDC329No ratings yet
- 7Document6 pages7soledadDC329No ratings yet
- 6Document6 pages6soledadDC329No ratings yet
- 8Document6 pages8soledadDC329No ratings yet
- Factor VIII Inhibitors Complicating Treatment of Postoperative Bleeding in A Dog With Hemophilia ADocument5 pagesFactor VIII Inhibitors Complicating Treatment of Postoperative Bleeding in A Dog With Hemophilia AsoledadDC329No ratings yet
- 7Document6 pages7soledadDC329No ratings yet
- 5Document5 pages5soledadDC329No ratings yet
- The Side Effects of Corticosteroids: Bernard BeckerDocument6 pagesThe Side Effects of Corticosteroids: Bernard BeckerShayyy JacksonNo ratings yet
- Acanthamoeba KeratitisDocument2 pagesAcanthamoeba KeratitisHitesh SharmaNo ratings yet
- Diagnosis and Management of Microbial Keratitis: AIOS Guidelines ForDocument24 pagesDiagnosis and Management of Microbial Keratitis: AIOS Guidelines ForKukuh Rizwido PrasetyoNo ratings yet
- Interesting Case - Yohanes Firmansyah - Epithelial KeratitisDocument51 pagesInteresting Case - Yohanes Firmansyah - Epithelial Keratitis-Yohanes Firmansyah-No ratings yet
- Acyclovir - Iarc Monographs 76-6Document25 pagesAcyclovir - Iarc Monographs 76-6NitinPrachiJainNo ratings yet
- Clinical Pearls Herpes Eye InfectionDocument20 pagesClinical Pearls Herpes Eye InfectionmudymaxNo ratings yet
- EVER2012Abstractbook PDFDocument330 pagesEVER2012Abstractbook PDFfarinazNo ratings yet
- Review On Ophthalmic InsertsDocument9 pagesReview On Ophthalmic InsertsIoana Bojescu RoșuNo ratings yet
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 22Document16 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 22sarasjunkNo ratings yet
- Red Eye, Conjuctivitis, Vision LossDocument213 pagesRed Eye, Conjuctivitis, Vision LossShashi Royal TNNo ratings yet
- Corne A: Dr. Yulia Fitriani, SPMDocument47 pagesCorne A: Dr. Yulia Fitriani, SPMEdsel QasswaraNo ratings yet
- Corneal UlcerDocument35 pagesCorneal UlcerMary Mae Bercacio BuellaNo ratings yet
- Eye (4th Year) MCQs - Rana Haseeb 2020Document59 pagesEye (4th Year) MCQs - Rana Haseeb 2020boyziddi32No ratings yet
- Konjungtivitis Dan KeratitisDocument117 pagesKonjungtivitis Dan KeratitisResti Puteri ApriyuslimNo ratings yet
- Herpetic Keratitis: Jenan GhaithDocument8 pagesHerpetic Keratitis: Jenan GhaithJenan GhaithNo ratings yet
- 06 Cornea PDFDocument74 pages06 Cornea PDFLeo TedjaNo ratings yet
- Medadteam 2010 - 4th Year ExamsDocument80 pagesMedadteam 2010 - 4th Year ExamsAmerdad DzulkifliNo ratings yet
- Persistent Corneal Epithelial Defects A Review ArticleDocument14 pagesPersistent Corneal Epithelial Defects A Review ArticleDr. Abhishek OnkarNo ratings yet
- Emailing Ophthalmology - Past Papers SEQS - KMUDocument70 pagesEmailing Ophthalmology - Past Papers SEQS - KMUem khan100% (2)
- Ophthalmology - Diseases of CorneaDocument18 pagesOphthalmology - Diseases of CorneajbtcmdtjjvNo ratings yet
- Color Atlas & Synopsis of Clinical Ophthalmology - Wills Eye Institute CorneaDocument384 pagesColor Atlas & Synopsis of Clinical Ophthalmology - Wills Eye Institute Corneam.No ratings yet
- Ophthalmology MCQsDocument532 pagesOphthalmology MCQsSaiSri LalamNo ratings yet
- Eyelids, Conjunctiva, Cornea and Sclera: McquestionsDocument52 pagesEyelids, Conjunctiva, Cornea and Sclera: McquestionsHawwi Ismail100% (1)
- Therapy LV CNS 4th Year KirubelDocument156 pagesTherapy LV CNS 4th Year Kirubelpblinder1319No ratings yet
- BCQs POOLDocument39 pagesBCQs POOLabusaudinternationalNo ratings yet
- عملي السليداتDocument92 pagesعملي السليداتSandyDavidNo ratings yet
- Viral ConjunctivitisDocument30 pagesViral ConjunctivitisJoane Chan LimNo ratings yet
- HSV Keratitis Treatment Guideline HarvardDocument69 pagesHSV Keratitis Treatment Guideline HarvardabciximabNo ratings yet
- Common Eye Problems and DiagnosisDocument84 pagesCommon Eye Problems and Diagnosisvivekrajbhilai5850No ratings yet
- The CorneaDocument60 pagesThe CorneaSarahNo ratings yet