Professional Documents
Culture Documents
Lung Carcinoma
Uploaded by
Anna KareninaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lung Carcinoma
Uploaded by
Anna KareninaCopyright:
Available Formats
LUNG CARCINOMA
Lung carcinoma is the most common fatal malignancy in both men and women. In the United
States, it accounts for 14% to 15% of all new cancers and 26% to 30% of all cancer deaths.
Lung cancer is more common in men than women, but at present its incidence is decreasing
in men and increasing in women.
RISK FACTORS FOR LUNG CANCER
Tobacco smoking accounts for 80% to 90% oflung cancers. In smokers, the risk of lung
cancer correlates with younger age at the onset of smoking, the duration and cumulative
amount of exposure, and the depth of inhalation. Heavy smoking is associated with a 20- to
30-fold increase in lung cancer risk compared to nonsmokers. A decrease in risk following
smoking cessation has been demonstrated. Well differentiated squamous cell carcinoma,
small cell carcinoma, large cell carcinoma, and to a lesser extent adenocarcinoma all
demonstrate an increased incidence with increasing cigarette consumption. About 25% of
lung cancers in nonsmokers have been attributed to second-hand smoke. Increasing age is
associated with an increased risk of lung cancer. Lung cancers are rare in patients under age
30. Occupational exposures to various substances have been linked to lung cancer; as many
as 10% of lung cancer cases may be due to occupational exposure. Agents associated with
occupational lung cancer include arsenic, nickel, cluomium, asbestos, beryllium, cadmium,
chromium, mustard gas, pesticides, and radon or uranium. Asbestos exposure is the best-
recognized occupational risk for lung cancer and is the most frequent exposure in the general
population (Fig. 3-1). A dose-response relationship between the severity and duration of
asbestos exposure and the likelihood of developing lung cancer is well established, although
the risk of exposure depends not only on the amount of asbestos to which one is exposed but
also the fiber type (increased risk with amphibole fibers), the industrial use of asbestos, the
conditions of exposure, and the presence of asbestosis. The risk of lung cancer in a heavily
exposed asbestos worker is about five times that of a nonexposed subject Also, smoking is a
synergistic risk in asbestos-exposed subjects: the risk of lung cancer in an asbestos worker
who is a heavy smoker is about 20 times that of a nonsmoking asbestos worker and 100 times
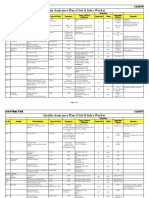
that of a nonexposed nonsmoker (Table 3-1).
Diffuse pulmonary fibrosis has been associated with a 10-fold increase in the risk of lung
cancer. In addition, patients with focal lung scarring. particularly as a result of tuberculosis,
can develop a carcinoma in association with areas of fibrosis or scarring. Although this is
infrequent, cases of carcinoma arising in areas of focal scarring, so-called scar carcinoma, are
encountered in clinical practice. Chronik obstructive lung disease (chronic bronckitis and
emphysema) is a risk factor for developing lung cancer, independent of cigarette smoking. In
both chronic obstructive pulmonary disease (COPD) and diffuse pulmonary fibrosis,
proposed mec:b.anisms of increased cancer risk include decreased clearance of inhaled
carcinogens and epithelial metaplasia.
Genetic: predisposition plays a role in the development of lung cancer. In general, relatives of
subjects with lung cancer have a higher risk of developing lung cancer (about twofold) than
the general population. An increased risk of lung cancer has been associated with specific
oncogenes, chromosome defects, specific HLA antigens, enzyme defects, and defects in
proteins normally produced by tumor suppressor genes.
CELL TYPES OF LUNG CANCER
Lung carcinomas have been classified by the World Health Organization (WHO) based on
their light-microscopic appearances (Table 3-2). The large majority of lung cancers are
classified by WHO criteria as one of four major histologic types: squamous cell carcinoma,
adenocarcinoma, small cell carcinoma, and large cell carcinoma. Numerous subtypes of these
four major twnors have also been defined, but most of these are unimportant from a
radiologic or clinical standpoint. These cell types are not absolutely distinct. As many as 50%
of lung twnors have mixed appearances. and the most differentiated feature of the carcinoma
is used to define its cell type. Many tumors classified as one histologic type (e.g., large cell
carcinoma) using light microscopy and the WHO system would be reclassified if electron
microscopy were used. Cytologic examination uncommonly allows a specific cell type to be
determined; cytologic diagnosis of lung cancer is usually limited to the designation nonsma!l
ceU lung carcinoma (NSCLC) or smaH cell carcinoma.
Preinvasive Lesions
These lesions are dysplastic or localized and include atypical adenomatous hyperplasia
(AAH), squamous dysplasia and carcinoma in situ, and diffuse idiopathic pulmonary
neuroendocrine cell hyperplasia (described below along with carcinoid tumors). AAH
represents a bronchioloalveolar proliferation that resembles but does not meet the criteria for
bronchioloalveolar carcinoma (BAC). Its incidence ranges from 5% to 20%. Most lesions are
5 mm or less in diameter, and lesions are often multiple. AAH is most often found
incidentally in pathologic specimens but may mimic lung carcinoma radiographically
(particularly on cr), leading to resection. On CT, AAH typically appears as a small nodule of
ground-glass opacity.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- TSR 9440 - Ruined KingdomsDocument128 pagesTSR 9440 - Ruined KingdomsJulien Noblet100% (15)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Quality Assurance Plan - CivilDocument11 pagesQuality Assurance Plan - CivilDeviPrasadNathNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Libel Arraignment Pre Trial TranscriptDocument13 pagesLibel Arraignment Pre Trial TranscriptAnne Laraga LuansingNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- COACHING TOOLS Mod4 TGOROWDocument6 pagesCOACHING TOOLS Mod4 TGOROWZoltan GZoltanNo ratings yet
- How Should We Allocate Scarce Resources Over Our Business Portfolio?Document20 pagesHow Should We Allocate Scarce Resources Over Our Business Portfolio?Vivek AryaNo ratings yet
- MGT403 Slide All ChaptersDocument511 pagesMGT403 Slide All Chaptersfarah aqeelNo ratings yet
- (LaSalle Initiative) 0Document4 pages(LaSalle Initiative) 0Ann DwyerNo ratings yet
- 7 Ways To Support Your Babys Learning Today Monti KidsDocument19 pages7 Ways To Support Your Babys Learning Today Monti KidsMareim A HachiNo ratings yet
- Invenio Flyer enDocument2 pagesInvenio Flyer enErcx Hijo de AlgoNo ratings yet
- A List of 142 Adjectives To Learn For Success in The TOEFLDocument4 pagesA List of 142 Adjectives To Learn For Success in The TOEFLchintyaNo ratings yet
- Jurnal Direct and Indirect Pulp CappingDocument9 pagesJurnal Direct and Indirect Pulp Cappingninis anisaNo ratings yet
- Installation, Operation & Maintenance Manual - Original VersionDocument11 pagesInstallation, Operation & Maintenance Manual - Original VersionAli AafaaqNo ratings yet
- Passive Income System 2Document2 pagesPassive Income System 2Antonio SyamsuriNo ratings yet
- BSBSTR602 Project PortfolioDocument16 pagesBSBSTR602 Project Portfoliocruzfabricio0No ratings yet
- DSS 2 (7th&8th) May2018Document2 pagesDSS 2 (7th&8th) May2018Piara SinghNo ratings yet
- INDUSTRIAL PHD POSITION - Sensor Fusion Enabled Indoor PositioningDocument8 pagesINDUSTRIAL PHD POSITION - Sensor Fusion Enabled Indoor Positioningzeeshan ahmedNo ratings yet
- GSP AllDocument8 pagesGSP AllAleksandar DjordjevicNo ratings yet
- Simple Past and Past Perfect TensesDocument13 pagesSimple Past and Past Perfect TensesSincerly RevellameNo ratings yet
- Appsc Aee Mains 2019 Electrical Engineering Paper III 1fcbb2c9Document12 pagesAppsc Aee Mains 2019 Electrical Engineering Paper III 1fcbb2c9SURYA PRAKASHNo ratings yet
- 20 Ijrerd-C153Document9 pages20 Ijrerd-C153Akmaruddin Bin JofriNo ratings yet
- Sample Paper Book StandardDocument24 pagesSample Paper Book StandardArpana GuptaNo ratings yet
- 2015 Grade 4 English HL Test MemoDocument5 pages2015 Grade 4 English HL Test MemorosinaNo ratings yet
- Northern Lights - 7 Best Places To See The Aurora Borealis in 2022Document15 pagesNorthern Lights - 7 Best Places To See The Aurora Borealis in 2022labendetNo ratings yet
- Quality Assurance Plan-75FDocument3 pagesQuality Assurance Plan-75Fmohamad chaudhariNo ratings yet
- Matrix CPP CombineDocument14 pagesMatrix CPP CombineAbhinav PipalNo ratings yet
- HW Chapter 25 Giancoli Physics - SolutionsDocument8 pagesHW Chapter 25 Giancoli Physics - SolutionsBecky DominguezNo ratings yet
- Madam Shazia PaperDocument14 pagesMadam Shazia PaperpervaizhejNo ratings yet
- Chapter 8 - Current Electricity - Selina Solutions Concise Physics Class 10 ICSE - KnowledgeBoatDocument123 pagesChapter 8 - Current Electricity - Selina Solutions Concise Physics Class 10 ICSE - KnowledgeBoatskjNo ratings yet
- Math - Snowflake With ProtractorsDocument4 pagesMath - Snowflake With Protractorsapi-347625375No ratings yet
- Theory of Construction of The Giza Plateau Pyramids (Original Title Hypothesis of Construction of The Pyramids of The Valley of Gizeh (Giza)Document15 pagesTheory of Construction of The Giza Plateau Pyramids (Original Title Hypothesis of Construction of The Pyramids of The Valley of Gizeh (Giza)International Journal of Innovative Science and Research TechnologyNo ratings yet