Professional Documents
Culture Documents
D Insipida
Uploaded by
Andrea Valenzuela AedoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
D Insipida
Uploaded by
Andrea Valenzuela AedoCopyright:
Available Formats
Diabetes insipidus
Stephen Ball
Abstract
Diabetes insipidus (DI) describes the excess production of dilute urine. It is
caused by the lack of production or action of the hormone vasopressin
(AVP). Diagnosis requires a targeted history and examination. Conrmation
requires referral to specialist services with expertise in diagnosis and man-
agement. Lack of AVP can be treated with synthetic vasopressin analogues.
Additional approaches may be needed for specic forms of DI. Combined
defects in AVP production and thirst perception require a structured pro-
gramme of uid intake and antidiuresis. Clinicians need to be aware of
both systemic and locally progressive pathologies that can present with DI.
Keywords adipsia; diabetes insipidus; hypernatraemia; hyponatraemia;
polydipsia; polyuria; vasopressin
Diabetes insipidus (DI) is characterized by excess production of
dilute urine e more than 40 ml/kg/24 hours in adults and more
than 100 ml/kg/24 hours in children.
Urine concentration is regulated by vasopressin (AVP), a nine-
amino-acid peptide produced by magnocellular neurones within
the supra-optic nucleus (SON) and para-ventricular nucleus
(PVN) of the hypothalamus. AVP is released into the circulation
from nerve terminals in the posterior pituitary gland. Production
is directly related to plasma osmolality and inversely related to
plasma volume. The principal site of action of AVP is the kidney,
where it increases the synthesis and assembly of water channels
(aquaporin 2, AQP2), leading to increased free water reabsorp-
tion. These effects are mediated through interaction with a G-
protein coupled cell surface receptor (AVP-R2), found on target
cells lining the luminal surface of the distal nephron.
1
Classication and aetiology
There are three sub-types of DI, each reecting a specic element
of the physiology and/or pathophysiology of the AVP axis.
2
Cranial or hypothalamic diabetes insipidus (HDI): relative
or absolute lack of AVP.
Nephrogenic diabetes insipidus (NDI): partial or total
resistance to the renal antidiuretic effects of AVP.
Dipsogenic diabetes insipidus (DDI, primary polydipsia):
inappropriate, high uid intake in excess of ability to
excrete free water.
Hypothalamic diabetes insipidus
Presentation with HDI occurs when 80% of hypothalamic mag-
nocellular neurone AVP production has been lost. Several path-
ological processes can be involved. All lead to either the
destruction of AVP neurones, or the interruption of the transport
or processing of AVP as it moves along the axons of these neu-
rones for release at nerve terminals in the posterior pituitary
(Table 1). The condition can appear for the rst time or become
worse in pregnancy as residual AVP is degraded by increased
placental (vasopressinase) enzyme activity. Up to 50% of chil-
dren and young adults with HDI have an underlying tumour or
CNS malformation.
3
Familial HDI comprises 5% of cases.
4
Nephrogenic diabetes insipidus
Renal resistance to AVP can be the result of the adverse effects of
specic drugs (e.g. lithium toxicity). These effects may be tem-
porary, but sometimes persist. NDI may also occur following
obstructive nephropathy, acute kidney injury and electrolyte
disturbances (e.g. hypokalaemia, hypercalcaemia). Prolonged
polyuria of any cause can result in partial NDI through disruption
of the intra-renal solute gradient that is an obligatory require-
ment for production of concentrated urine. X-linked familial NDI
results from loss-of-function mutations in the renal AVP-R2 re-
ceptor. Autosomal recessive NDI is caused by loss-of-function
mutations in the AVP-dependent water channel, AQP2.
5
Dipsogenic diabetes insipidus
Persistent inappropriate uid intake leads to appropriate poly-
uria. If it exceeds the limit of renal free water excretion it may
result in hyponatraemia. DDI can be associated with the
following abnormalities in thirst perception:
low threshold for thirst
exaggerated thirst response to osmotic challenge
inability to suppress thirst at low plasma osmolalities.
Structural lesions may be present, but neuroimaging is normal in
most cases. DDI is associated with affective disorders.
Epidemiology
DI is rare. Prevalence of HDI is estimated at 1/25,000 with equal
gender distribution. The prevalence of the other forms is unclear.
While most cases present in adults, familial HDI and NDI char-
acteristically present in childhood.
Whats new?
C
Better understanding of the regulation of vasopressin secretion
and its mechanism of action
C
New insights into the molecular genetics of inherited diabetes
insipidus
C
Evolving approaches and novel tools to aid differential
diagnosis
Stephen Ball BSc PhD FRCP is Senior Lecturer and Honorary Consultant,
Newcastle University and Newcastle Hospitals NHS Trust, UK. SB
studied Basic Science at Birmingham University before pursuing
undergraduate and postgraduate Medical Studies in London. Middle
grade training in Diabetes and Endocrinology included a period in the
USA as a Medical Research Council (UK) and Howard Hughes Fellow. He
combines clinical medicine, research and teaching. He is a member of
Council of the Society for Endocrinology and a Senior Editor of Clinical
Endocrinology. He is also a European Endocrine Society representative
within European Guideline groups. Conicts of interest: none declared.
PITUITARY DISORDERS
MEDICINE 41:9 519 2013 Elsevier Ltd. All rights reserved.
Diagnosis and investigations
DI presents with polyuria and polydipsia. History and examina-
tion may reveal important features suggestive of:
systemic disease
associated endocrinopathy
an associated neurological problem suggestive of struc-
tural disease
drug toxicity.
Polyuria must be distinguished from simple frequency without
excess urine volume.
The initial approach should be to conrm excess urine volume
and exclude simple metabolic causes such as hyperglycaemia
and hypercalcaemia. Denitive diagnosis requires referral to an
endocrine service for testing of AVP production and action in
response to osmolar stress. The water deprivation test measures
renal concentrating capacity in response to dehydration, and is
an indirect assessment of the AVP axis. It is usually followed by
assessment of renal response to the synthetic AVP analogue
DDAVP. Characteristic ndings are as follows.
In DDI, urine concentration is normal in response to
dehydration.
In HDI, urine concentration fails in response to dehydra-
tion, but not to DDAVP.
In NDI, urine concentration fails in response to both
manoeuvres.
In practice, many results are indeterminate.
6
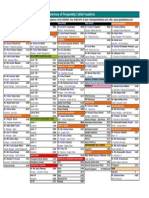
Direct measurement of AVP production during graded hyper-
osmolar stimulation is the gold-standard method for diagnosing
and classifying DI (Figure 1). Recent data suggest that measure-
ment of co-peptin, an inactive fragment of the AVP precursor that
is released in proportion to AVP, may prove to be an alternative.
7
Conrmation of HDI should lead to further pituitary function
testing and cranial MRI. NDI requires renal tract imaging and
additional renal function studies.
Diabetes insipidus and hypernatraemia
There is a close neuroanatomical relationship between the hy-
pothalamic structures responsible for osmoregulation of thirst
and AVP production. Certain structural, neurovascular and
neuro-developmental lesions are thus associated with combined
defects in both processes. Absent or reduced thirst (adipsia) in
association with HDI predisposes to hypernatraemic dehydra-
tion. Diagnosis follows the protocol for HDI, but benets from
the parallel assessment of thirst perception.
8
Management
Mild forms of HDI may not require treatment. Signicant polyuria
and polydipsia are treated effectively with oral or intranasal
DDAVP. In NDI, causal drugs should be withdrawn where possible
and precipitating electrolyte disturbances corrected. NDI may
respond partly to high-dose DDAVP. Thiazide diuretics and non-
steroidal anti-inammatory drugs can be of additional benet,
but may not normalize urine production. The only rational
approach to DDI is reduction in uid intake. DDAVP treatment
must be avoided in DDI, because of the risk of hyponatraemia.
Follow-up
Following initiation of DDAVP, patients may require frequent
review by an endocrine service for dose titration. Thereafter,
they can be seen annually to assess symptom control and check
serum sodium to avoid over-treatment. The combination of HDI
with adipsia requires meticulous follow-up in a specialist service,
with a structured approach to uid intake and antidiuresis.
Prognosis
Isolated HDI has an excellent prognosis and patients should
anticipate a normal quality of life. When HDI is associated with
pituitary hormone deciency, structural or systemic disease,
prognosis is determined by the natural history of the underlying
pathology and co-morbidities. HDI following trauma may
resolve.
9
NDI is difcult to treat, and the symptoms seldom
Aetiology of hypothalamic diabetes insipidus
Primary Genetic Wolframs syndrome, autosomal
dominant, autosomal recessive
Developmental
syndromes
Septo-optic dysplasia
Idiopathic
Secondary Trauma Head injury, post-surgery
(transcranial, trans-sphenoidal)
Tumour Craniopharyngioma, germinoma,
metastases, pituitary
macroadenoma
Inammatory Sarcoidosis, histiocytosis,
meningitis, encephalitis,
infundibuloneurohypophysitis,
GuillaineBarre syndrome,
autoimmune
Vascular Aneurysm, infarction
Classication describes primary and secondary (acquired) causes. All result in
decreased production of vasopressin (AVP) through direct or indirect damage
to hypothalamic AVP magnocellular neurones.
Table 1
Diagnosis and classification of diabetes insipidus by
measurement of plasma vasopressin in response to
graded hyperosmolar stimulation
The shaded area depicts the normal-range response of plasma vasopressin
as plasma osmolality is raised. Patients with hypothalamic diabetes insipidus
have a response below the normal range. Those with dipsogenic diabetes
insipidus have a normal response. Patients with nephrogenic diabetes
insipidus have a response at the top of the reference range but coincident
urine osmolalities that are dilute, consistent with vasopressin resistance.
P
l
a
s
m
a
v
a
s
o
p
r
e
s
s
i
n
(
p
m
o
l
/
l
i
t
r
e
)
20
15
10
0
Plasma osmolality (mOsmol/kg)
310 300 290 280 320
5
Nephrogenic
Dipsogenic
Hypothalamic
Figure 1
PITUITARY DISORDERS
MEDICINE 41:9 520 2013 Elsevier Ltd. All rights reserved.
respond completely. Future developments may further help early
diagnosis and guide appropriate intervention.
10
A
REFERENCES
1 Ball SG. Vasopressin and disorders of water balance: the physiology
and pathophysiology of vasopressin. Ann Clin Biochem 2007; 44:
417e31.
2 Ball SG, Baylis PH. The neurohypophysis. In: Wass JAH, Shalet SM,
eds. Oxford textbook of endocrinology and diabetes. Oxford: Oxford
University Press, 2002; 87e99.
3 Maghnie M, Cosi G, Genovese E, et al. Central diabetes insipidus in
children and young adults. N Engl J Med 2000; 343: 998e1007.
4 Babey M, Kopp P, Robertson GA. Familial forms of diabetes insipidus:
clinical and molecular characteristics. Nat Rev Endocrinol 2011; 7:
701e14.
5 Moeller HB, Rittig S, Fenton RA. Nephrogenic diabetes insipidus:
essential insights into the molecular background and potential
therapies for treatment. Endocr Rev 2013; 34: 278e301.
6 Ball SG, Barber T, Baylis PH. Tests of posterior pituitary function.
J Endocrinol Invest 2003; 26(suppl): 15e24.
7 Fenske W, Quinkler M, Lorenz D, et al. Copeptin in the differential
diagnosis of the polydipsia-polyuria syndromedrevisiting the direct
and indirect water deprivation tests. J Clin Endocrinol Metab 2011;
96: 1506e15.
8 Ball SG, Vaidja B, Baylis PH. Hypothalamic adipsic syndrome: diag-
nosis and management. Clin Endocrinol 1997; 47: 405e9.
9 Behan LA, Thompson CJ, Agha A. Neuroendocrine disorders
after traumatic brain injury. J Neurol Neurosurg Psychiatr 2008; 79:
753e9.
10 Fenske W, Allolio B. Current state and future perspectives in the
diagnosis of diabetes insipidus: a clinical review. J Clin Endocrinol
Metab 2012; 97: 3426e37.
PITUITARY DISORDERS
MEDICINE 41:9 521 2013 Elsevier Ltd. All rights reserved.
You might also like
- The Secret of The House WTDocument22 pagesThe Secret of The House WTPetr -50% (2)
- Life Sciences Part 1 CSIR JRF NET GATE DBT PDFDocument132 pagesLife Sciences Part 1 CSIR JRF NET GATE DBT PDFPavani Reddy68% (22)
- Diabetes InsipidusDocument21 pagesDiabetes InsipidusMoni RethNo ratings yet
- ME JBP 70A Pen Dissolved Oxygen Meter PDFDocument1 pageME JBP 70A Pen Dissolved Oxygen Meter PDFpiknikmonsterNo ratings yet
- Module A Specimen Questions January2020 PDFDocument5 pagesModule A Specimen Questions January2020 PDFShashi Bhusan SinghNo ratings yet
- Case Studies On Industrial Accidents - 2Document84 pagesCase Studies On Industrial Accidents - 2Parth N Bhatt100% (2)
- Case Report_ Diabetes InsipidusDocument4 pagesCase Report_ Diabetes InsipidusSACHI DANIELLA TATOYNo ratings yet
- Diagnosis of Polyuria and Diabetes Insipidus - UP To DATEDocument15 pagesDiagnosis of Polyuria and Diabetes Insipidus - UP To DATELuis Fernando Arias VillalobosNo ratings yet
- Diagnosis and Management of Central Diabetes Insipidus in AdultsDocument8 pagesDiagnosis and Management of Central Diabetes Insipidus in AdultsPenta AssiddiqiNo ratings yet
- NCBI Bookshelf-Diabetes InsipidusDocument44 pagesNCBI Bookshelf-Diabetes InsipidusDiah Pradnya ParamitaNo ratings yet
- Diabetes InsipidusDocument18 pagesDiabetes InsipidusElena Patricia GonzálezNo ratings yet
- Diabetes InsipidusDocument7 pagesDiabetes Insipiduspaul_stefenson10No ratings yet
- Diabetes InsipidusDocument14 pagesDiabetes InsipidusTom BiusoNo ratings yet
- Diabetes InsipidusDocument5 pagesDiabetes InsipidusFazalJaturieNo ratings yet
- 58 DI diagnosis and treatmentDocument11 pages58 DI diagnosis and treatmentBogdan SoltuzuNo ratings yet
- Diabetes InsipidusDocument4 pagesDiabetes Insipidusshelly_shellyNo ratings yet
- Pediatric Diabetes InsipidusDocument11 pagesPediatric Diabetes InsipidusVictor Matias BarriosNo ratings yet
- Deficiencies of Vasopressin Secretion and ActionDocument71 pagesDeficiencies of Vasopressin Secretion and Actionbiniam MesfinNo ratings yet
- Research Paper On Diabetes InsipidusDocument5 pagesResearch Paper On Diabetes Insipidusfypikovekef2100% (1)
- Diabetes InsipidaDocument15 pagesDiabetes Insipidapaulito_delgadoNo ratings yet
- Nephrogenic Diabetes InsipidusDocument10 pagesNephrogenic Diabetes InsipidusJapheth SalvanNo ratings yet
- Diabetes Insipidus: Pathogenesis, Diagnosis, and Clinical ManagementDocument13 pagesDiabetes Insipidus: Pathogenesis, Diagnosis, and Clinical Managementputrirahayu srikandiNo ratings yet
- Sonia Nabila (P17220194050) Artikel B.InggrisDocument10 pagesSonia Nabila (P17220194050) Artikel B.InggrisSonia NabilaNo ratings yet
- Syndromeofinappropriate Antidiuresis: Michael L. MoritzDocument18 pagesSyndromeofinappropriate Antidiuresis: Michael L. MoritznelidayslasNo ratings yet
- Diabete InsipidaDocument20 pagesDiabete InsipidaLuciana RafaelNo ratings yet
- Diabetes Insipidus HandoutDocument4 pagesDiabetes Insipidus HandoutllianNo ratings yet
- Sands PDFDocument10 pagesSands PDFAsmaulKhusnaNo ratings yet
- Diabetes INSIPIDUSDocument6 pagesDiabetes INSIPIDUSavinash dhameriya100% (1)
- Posterior Pituitary Gland Disorders ExplainedDocument29 pagesPosterior Pituitary Gland Disorders ExplainedZanida ZainonNo ratings yet
- Lab 5 Diabetes InsipidusDocument6 pagesLab 5 Diabetes InsipidusLisa EkapratiwiNo ratings yet
- Clinical Manifestations and Causes of Central Diabetes InsipidusDocument12 pagesClinical Manifestations and Causes of Central Diabetes InsipidusTessa AcostaNo ratings yet
- Guidelines For The Inpatient Management of Cranial Diabetes InsipidusDocument4 pagesGuidelines For The Inpatient Management of Cranial Diabetes InsipidusAndrei MarianNo ratings yet
- Nephrogenic Diabetes Insipidus (Includes: Nephrogenic Diabetes Insipidus, Autosomal Nephrogenic Diabetes Insipidus, X-Linked)Document18 pagesNephrogenic Diabetes Insipidus (Includes: Nephrogenic Diabetes Insipidus, Autosomal Nephrogenic Diabetes Insipidus, X-Linked)ironNo ratings yet
- Pediatrics in Review 2013 HiponatremiaDocument5 pagesPediatrics in Review 2013 HiponatremiaCarlos Elio Polo Vargas100% (1)
- Managing Diabetes Insipidus after Pituitary Tumor SurgeryDocument11 pagesManaging Diabetes Insipidus after Pituitary Tumor SurgeryAnggun RosalinaNo ratings yet
- A Clinical Overview of Non-Alcoholic Fatty Liver Disease A GuideDocument12 pagesA Clinical Overview of Non-Alcoholic Fatty Liver Disease A GuideAnindya RosmaNo ratings yet
- Hypernatremia: Hypernatremia Is Defined As A Plasma Na+ Concentration 145 Mmol/lDocument13 pagesHypernatremia: Hypernatremia Is Defined As A Plasma Na+ Concentration 145 Mmol/ltamir14No ratings yet
- ACP Board Review Nephrology 20052ndDocument35 pagesACP Board Review Nephrology 20052nddoctormido2010100% (1)
- Refardt 2020Document14 pagesRefardt 2020ushNo ratings yet
- Diabetes Insipidus: Basic Information DiagnosisDocument4 pagesDiabetes Insipidus: Basic Information DiagnosisHarmando Frankho Hacoltsi HernanndesNo ratings yet
- Diabetes Insipidus.Document10 pagesDiabetes Insipidus.Nithya ManiNo ratings yet
- Cen 91 22Document11 pagesCen 91 22Elena MandrescuNo ratings yet
- D-Lactic AcidosisDocument8 pagesD-Lactic AcidosisJoe DoeNo ratings yet
- Garrahy 2020Document13 pagesGarrahy 2020Ana Elizabeth Gangotena CoralNo ratings yet
- A Rare Case of Familial Neurogenic Diabetes Insipidu - 2021 - AACE Clinical CaseDocument4 pagesA Rare Case of Familial Neurogenic Diabetes Insipidu - 2021 - AACE Clinical CaseShuaib AhmedNo ratings yet
- Diabetes Insipidus: Presented By-Akansha Student, B.sc. Nursing 3rd Semester Con, DR - RmlimsDocument12 pagesDiabetes Insipidus: Presented By-Akansha Student, B.sc. Nursing 3rd Semester Con, DR - Rmlimsakanshaa32000No ratings yet
- Diabetes Insipidus: Done By: Farah Suhimat Sereen MajaliDocument23 pagesDiabetes Insipidus: Done By: Farah Suhimat Sereen Majaliraed faisalNo ratings yet
- Diabetes InsipidusDocument3 pagesDiabetes InsipidusfynneroNo ratings yet
- PamphletDocument1 pagePamphletAldenn MinotaurNo ratings yet
- Maintenance Intravenous Fluids in Acutely Ill Patients: Review ArticleDocument11 pagesMaintenance Intravenous Fluids in Acutely Ill Patients: Review ArticleyoiiiNo ratings yet
- Diabetes InsipidusDocument10 pagesDiabetes InsipidussoniaNo ratings yet
- Acute Decompensated HeartDocument7 pagesAcute Decompensated HeartRay MartínezNo ratings yet
- Endocrine Emergencies: James A. Kruse, MDDocument10 pagesEndocrine Emergencies: James A. Kruse, MDNataRamos57No ratings yet
- Diabetes InsidipusDocument2 pagesDiabetes InsidipusLena RoweNo ratings yet
- Clinical Manifestations and Causes of Central Diabetes Insipidus - UpToDateDocument15 pagesClinical Manifestations and Causes of Central Diabetes Insipidus - UpToDateMihaela Alexandra RepeziNo ratings yet
- Osmotic Diuretic Nursing CareDocument2 pagesOsmotic Diuretic Nursing CareBrandy RectoNo ratings yet
- Management of Fluid Status in Haemodialysis Patients: The Roles of Technology and Dietary AdviceDocument15 pagesManagement of Fluid Status in Haemodialysis Patients: The Roles of Technology and Dietary AdviceRuwaedaNasruddinNo ratings yet
- Jurnal Geriatri Dr. BrinnaDocument12 pagesJurnal Geriatri Dr. Brinnabrinna aninditaNo ratings yet
- Diabetes Insipidus: Causes, Symptoms & TestsDocument11 pagesDiabetes Insipidus: Causes, Symptoms & TestsHam SotheaNo ratings yet
- A Copeptin-Based Classification of The Osmoregulatory DefectDocument15 pagesA Copeptin-Based Classification of The Osmoregulatory DefectDEWINo ratings yet
- Diabetic Ketoacidosis 1Document10 pagesDiabetic Ketoacidosis 1Victor Manuel Gonzalez GalindoNo ratings yet
- DI Diagnosis and TreatmentDocument2 pagesDI Diagnosis and TreatmentLuiciaNo ratings yet
- Fluid and ElectrolytesDocument135 pagesFluid and ElectrolytesLindsay PinedaNo ratings yet
- Diabetes Insipidus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandDiabetes Insipidus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- BOF, LF & CasterDocument14 pagesBOF, LF & CastermaklesurrahmanNo ratings yet
- Female Reproductive System Histology IDocument5 pagesFemale Reproductive System Histology ISolomon Seth SallforsNo ratings yet
- Solcon Catalog WebDocument12 pagesSolcon Catalog Webquocviet612No ratings yet
- How To Become A Coffee Aficionado: Tips & Tricks: Kate Macdonnell Brewing Updated: Feb 06 2023Document17 pagesHow To Become A Coffee Aficionado: Tips & Tricks: Kate Macdonnell Brewing Updated: Feb 06 2023sadenaikeNo ratings yet
- Subaru Forester ManualsDocument636 pagesSubaru Forester ManualsMarko JakobovicNo ratings yet
- Kertas Trial English Smka & Sabk K1 Set 2 2021Document17 pagesKertas Trial English Smka & Sabk K1 Set 2 2021Genius UnikNo ratings yet
- Hypertension Protocol Mukta VatiDocument18 pagesHypertension Protocol Mukta VatiDr. Avnish UpadhyayNo ratings yet
- Request For Review FormDocument11 pagesRequest For Review FormJoel MillerNo ratings yet
- English Financial Assistance ApplicationDocument4 pagesEnglish Financial Assistance ApplicationAlyssa JenningsNo ratings yet
- Life Overseas 7 ThesisDocument20 pagesLife Overseas 7 ThesisRene Jr MalangNo ratings yet
- SM RSJ 420 800Document77 pagesSM RSJ 420 800elshan_asgarovNo ratings yet
- EcoLettsandSOM, Dulvy Et Al 2004Document25 pagesEcoLettsandSOM, Dulvy Et Al 2004Nestor TorresNo ratings yet
- Daudo PH-396PVP PDFDocument54 pagesDaudo PH-396PVP PDFVanBang TNNo ratings yet
- XDocument266 pagesXTrần Thanh PhongNo ratings yet
- Jairo Garzon 1016001932 G900003 1580 Task4Document12 pagesJairo Garzon 1016001932 G900003 1580 Task4Jairo Garzon santanaNo ratings yet
- Ic Audio Mantao TEA2261Document34 pagesIc Audio Mantao TEA2261EarnestNo ratings yet
- Growth Developt Pearl MilletDocument17 pagesGrowth Developt Pearl MilletdarmaNo ratings yet
- Role of Family and Society in The Rehabiloitation of Offenders PDFDocument4 pagesRole of Family and Society in The Rehabiloitation of Offenders PDFDevlika DasNo ratings yet
- Hydrogeological Characterization of Karst Areas in NW VietnamDocument152 pagesHydrogeological Characterization of Karst Areas in NW VietnamCae Martins100% (1)
- TA-Ingles IX - UAPDocument10 pagesTA-Ingles IX - UAPmanuel brennerNo ratings yet
- Perforamance Based AssessmentDocument2 pagesPerforamance Based AssessmentJocelyn Acog Bisas MestizoNo ratings yet
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- Fluid Mechanics Sessional: Dhaka University of Engineering & Technology, GazipurDocument17 pagesFluid Mechanics Sessional: Dhaka University of Engineering & Technology, GazipurMd saydul islamNo ratings yet
- FinalsDocument8 pagesFinalsDumpNo ratings yet
- Merit of RatingDocument1 pageMerit of RatingRaidasNo ratings yet