Professional Documents
Culture Documents
FLOW
Uploaded by
Jackie Swift Funtanilla0 ratings0% found this document useful (0 votes)
28 views12 pagesbloodflow
Original Title
FLOW.docx
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentbloodflow
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views12 pagesFLOW
Uploaded by
Jackie Swift Funtanillabloodflow
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 12
The Biliary System: Anatomy and Functions
The Biliary System: Anatomy and Functions
Click Image to Enlarge
Anatomy of the biliary system
The biliary system consists of the organs and ducts (bile ducts, gallbladder, and associated structures) that are involved in
the production and transportation of bile. The transportation of bile follows this sequence:
1. When the liver cells secrete bile, it is collected by a system of ducts that flow from the liver through
the right and left hepatic ducts.
2. These ducts ultimately drain into the common hepatic duct.
3. The common hepatic duct then joins with the cystic duct from the gallbladder to form the common
bile duct, which runs from the liver to the duodenum (the first section of the small intestine).
4. However, not all bile runs directly into the duodenum. About 50 percent of the bile produced by the
liver is first stored in the gallbladder, a pear-shaped organ located directly below the liver.
5. Then, when food is eaten, the gallbladder contracts and releases stored bile into the duodenum to
help break down the fats.
Functions of the biliary system
The biliary system's main function includes the following:
To drain waste products from the liver into the duodenum
To help in digestion with the controlled release of bile
Bile is the greenish-yellow fluid (consisting of waste products, cholesterol, and bile salts) that is secreted by the liver cells to
perform two primary functions, including the following:
To carry away waste
To break down fats during digestion
Bile salt is the actual component which helps break down and absorb fats. Bile, which is excreted from the body in the form
of feces, is what gives feces its dark brown color.
Regulation of Bile Release
Bile
Bile is produced in the liver by hepatocytes. Bile
contains phospholipids and bile salts, emulsifying agents that
are necessary for fat absorption and digestion. Importantly, the bile
is also a route for excretion of cholesterol and bile pigments. Bile
pigments are metabolic breakdown products of hemoglobin and
cytochromes that give bile its yellow-green color. Bile pigments are
further metabolized by bacteria in the colon, causing feces to have a
characteristic brown color. Additionally, bile contains water
andbicarbonate ions that are secreted by duct cells that line the
bile ducts within the liver.
Bile storage in the gallbladder
Whether or not bile is released into the small intestine depends
upon the activity of the sphincter of Oddi (also known as the
hepatopancreatic sphincter). During the interdigestive period, the
sphincter of Oddi is contracted, preventing bile from flowing out into
the duodenum. As a consequence, pressure increases in
the common bile duct, and bile flows into the gallbladder. In the
gallbladder, epithelial cells reabsorb water and electrolytes, causing
the bile to become more concentrated.
Bile release into the small intestine
During the digestive period, intestinal phase signals stimulate the
release of bile into the small intestine.
Fatty acids in the lumen of the duodenum stimulate endocrine
cells to release the hormone cholecystokinin (CCK). CCK
stimulates contractions in the smooth muscle of the gallbladder.
As well, CCK causes relaxation of the sphincter of Oddi, allowing
bile release into the duodenum.
Acidic chyme in the lumen of the duodenum stimulates other
endocrine cells to release the hormone secretin. Secretin
stimulates duct cells in the liver to release bicarbonate into the
bile.
Enterohepatic circulation
The bile salts present
in the body are not
sufficient to fully
process the fats in a
typical meal, thus
they need to be
recycled. This is
achieved by
the enterohepatic
circulation. Specific
transporters in
the terminal
ileum move bile salts from the lumen of the digestive tract to the
intestinal capillaries. They are then transported directly to the liver
via the hepatic portal vein. Hepatocytes take up bile salts from
the blood, and increase the secretion of bile salts into the bile
canaliculi, small passageways that convey bile into the larger bile
ducts. 95% of the bile that is released to the small intestine is
recycled via the enterohepatic circulation,while 5% of the bile salts
are lost in the feces.
Gallstones
In the majority of cases, gallstones are precipitates of cholesterol.
Cholesterol is a hydrophobic molecule that is kept in solution in the
bile by bile salts and phospholipids. Gallstones form when the level
of cholesterol in the bile exceeds the capacity of the phospholipids
and bile salts to keep it in solution. This might occur in someone
with hypercholesterolemia (high circulating levels of LDL
cholesterol), or in an older person in whom bile salt synthetic
enzymes have become less active.
Gallstones can be completely asymptomatic. When they become a
problem is when gallbladder contractions cause a stone to move
into one of the bile ducts. The figure summarizes the pathological
consequences of gallstones in different locations. Notably, a
gallstone blocking the common bile duct will prevent the flow of bile
into the small intestine. Without bile, fats cannot be digested and
absorbed, leading to the presence of fat in the feces,
orsteatorrhea. If the gallstone is lodged in the duodenal papilla,
neither bile nor pancreatic secretions will be able to be released to
the small intestine (although some individuals possess an accessory
duct for the release of pancreatic secretions). Inappropriate
activation of pancreatic zymogens within the pancreas leads
to acute pancreatitis (tissue damage and inflammation in the
pancreas).
Gallstones are usually treated by surgical methods. Gallstones
confined to the gallbladder and cystic bile duct can be treated with
removal of the gallbladder (cholecystectomy). Endoscopic surgical
methods can be used to remove gallstones lodged in the common
bile duct or duodenal papilla. In patients that are not good
candidates for surgery, shock waves can be used to break up
stones. Oral bile salts are used to help solubilize cholesterol
gallstones. This therapy works because oral bile salts are delivered
to the bile ducts and gallbladder by the enterohepatic circulation.
Blood Flow
All blood enters the right side of the heart through two veins: Thesuperior vena cava (SVC) and
the inferior vena cava (IVC) (see figure 3).
The SVC collects blood from the upper half of the body. The IVC collects blood from the lower half of the
body. Blood leaves the SVC and the IVC and enters the right atrium (RA) (3).
When the RA contracts, the blood goes through the tricuspid valve (4) and into the right ventricle (RV)
(5). When the RV contracts, blood is pumped through the pulmonary valve (6), into the pulmonary
artery(PA) (7) and into the lungs where it picks up oxygen.
Why does it happen this way? Because blood returning from the body is relatively poor in oxygen. It
needs to be full of oxygen before being returned to the body. So the right side of the heart pumps blood to
the lungs first to pick up oxygen before going to the left side of the heart where it is returned to the body
full of oxygen.
Blood now returns to the heart from the lungs by way of the pulmonary veins (8) and goes into the left
atrium (LA) (9). When the LA contracts, blood travels through the mitral valve(10) and into the left
ventricle (LV) (11). The LV is a very important chamber that pumps blood through the aortic valve (12)
and into the aorta (13). The aorta is the main artery of the body. It receives all the blood that the heart
has pumped out and distributes it to the rest of the body. The LV has a thicker muscle than any other
heart chamber because it must pump blood to the rest of the body against much higher pressure in the
general circulation (blood pressure).
Here is a recap of what we just discussed. Blood from the body flows:
to the superior and inferior vena cava,
then to the right atrium
through the tricuspid valve
to the right ventricle
through the pulmonic valve
to the pulmonary artery
to the lungs
The blood picks up oxygen in the lungs, and then flows from the lungs:
to the pulmonary veins
to the left atrium
through the mitral valve
to the left ventricle
through the aortic valve
to the aorta
to the body
The Path of Blood through the Human Body
When a heart contracts and forces blood into the blood vessels, there is a certain path that the
blood follows through the body. The blood moves through pulmonary circulation and then
continues on through systemic circulation. Pulmonary and systemic are the two circuits in the
two-circuit system of higher animals with closed circulatory systems.
Humans and other mammals have two-circuit circulatory systems: one circuit is for pulmonary
circulation (circulation to the lungs; pulmo = lungs), and the other circuit is for systemic
circulation (the rest of the body). As each atrium and ventricle contract, blood is pumped into
certain major blood vessels, and from there, continues through the circulatory system.
The intertwined circulatory system pathways: Pulmonary circulation and systemic circulation work
together.
Pulmonary circulation
Blood that is lacking oxygen is said to be deoxygenated. This blood has just exchanged oxygen
for carbon dioxide across cell membranes, and now contains mostly carbon dioxide.
Deoxygenated blood enters the right atrium through the superior vena cava and the inferior vena
cava.
Superior means higher, and inferior means lower, so the superior vena cava is at the top of the
right atrium, and the inferior vena cava enters the bottom of the right atrium.
From the right atrium, the deoxygenated blood drains into the right ventriclethrough the
right atrioventricular (AV) valve, which is so named because it is between the atrium and the
ventricle. This valve is also referred to as thetricuspid valve because it has three flaps in its
structure. When the ventricles contract, the AV valve closes off the opening between the ventricle
and the atrium so that blood does not flow back up into the atrium.
As the right ventricle contracts, it forces the deoxygenated blood through thepulmonary semilunar
valve and into the pulmonary artery. Semilunar means half-moon and refers to the shape of the
valve. Note that this is the only artery in the body that contains deoxygenated blood; all other
arteries contain oxygenated blood. The semilunar valve keeps blood from flowing back into the
right ventricle once it is in the pulmonary artery.
The pulmonary artery carries the blood that is very low in oxygen to the lungs, where it becomes
oxygenated.
Systemic circulation
Freshly oxygenated blood returns to the heart via the pulmonary veins. Note that these are the
only veins in the body that contain oxygenated blood; all other veins contain deoxygenated blood.
The pulmonary veins enter the left atrium. When the left atrium relaxes, the oxygenated blood
drains into the left ventricle through the left AV valve. This valve is also called the bicuspid
valve because it has only two flaps in its structure.
Now the heart really squeezes. As the left ventricle contracts, the oxygenated blood is pumped
into the main artery of the body the aorta. To get to the aorta, blood passes through the aortic
semilunar valve, which serves to keep blood flowing from the aorta back into the left ventricle.
The aorta branches into other arteries, which then branch into smaller arterioles. The arterioles
meet up with capillaries, which are the blood vessels where oxygen is exchanged for carbon
dioxide.
Capillary exchange
Capillaries bridge the smallest of the arteries and the smallest of the veins. Near the arterial end,
the capillaries allow materials essential for maintaining the health of cells to diffuse out (water,
glucose, oxygen, and amino acids).
To maintain the health of cells, it is also necessary for the capillaries to transport wastes and
carbon dioxide to places in the body that can dispose of them. The waste products enter near the
venous end of the capillary. Water diffuses in and out of capillaries to maintain blood volume,
which adjusts to achievehomeostasis.
Capillaries are only as thick as one cell, so the contents within the cells of the capillaries can
easily pass out of the capillary by diffusing through the capillary membrane. And, because the
capillary membrane abuts the membrane of other cells all over the body, the capillarys contents
can easily continue through the abutting cells membrane and get inside the adjoining cell.
The process of capillary exchange is how oxygen leaves red blood cells in the bloodstream and
gets into all the other cells of the body. Capillary exchange also allows nutrients to diffuse out of
the bloodstream and into other cells. At the same time, the other cells expel waste products that
then enter the capillaries, and carbon dioxide diffuses out of the bodys cells and into the
capillaries.
How capillary exchange works.
After the capillaries pick up the garbage from other cells, the capillaries carry the wastes and
carbon dioxide through the deoxygenated blood to the smallest of the veins, which are
called venules. The venules branch into bigger vessels called veins. The veins then carry the
deoxygenated blood toward the main vein, which is the vena cava. The two branches of the vena
cava enter the right atrium, which is where pulmonary circulation begins.
What Is Digestion?
Digestion is the complex process of turning the food you eat into the energy you need to survive. The
digestion process also involves creating waste to be eliminated.
The digestive tract (or gut) is a long twisting tube that starts at the mouth and ends at the anus. It is made
up of a series of muscles that coordinate the movement of food and other cells that produce enzymes and
hormones to aid in the breakdown of food. Along the way are three other organs that are needed for
digestion: the liver, gallbladder, and the pancreas.
Food's Journey Through the Digestive System
Stop 1: The Mouth
The mouth is the beginning of the digestive system, and, in fact, digestion starts here before you even
take the first bite of a meal. The smell of food triggers the salivary glands in your mouth to secrete saliva,
causing your mouth to water. When you actually taste the food, saliva increases.
Once you start chewing and breaking the food down into pieces small enough to be digested, other
mechanisms come into play. More saliva is produced to begin the process of breaking down food into a
form your body can absorb and use. In addition, "juices" are produced that will help to further break down
food. Chew your food more -- it helps with your digestion.
Stop 2: The Pharynx and Esophagus
Also called the throat, the pharynx is the portion of the digestive tract that receives the food from your
mouth. Branching off the pharynx is the esophagus, which carries food to the stomach, and the trachea or
windpipe, which carries air to the lungs.
The act of swallowing takes place in the pharynx partly as a reflex and partly under voluntary control. The
tongue and soft palate -- the soft part of the roof of the mouth -- push food into the pharynx, which closes
off the trachea. The food then enters the esophagus.
The esophagus is a muscular tube extending from the pharynx and behind the trachea to the stomach.
Food is pushed through the esophagus and into the stomach by means of a series of contractions called
peristalsis.
Just before the opening to the stomach is an important ring-shaped muscle called the lower esophageal
sphincter (LES). This sphincter opens to let food pass into the stomach and closes to keep it there. If your
LES doesn't work properly, you may suffer from a condition calledGERD, or reflux, which
causes heartburn and regurgitation (the feeling of food coming back up).
Stop 3: The Stomach and Small Intestine
The stomach is a sac-like organ with strong muscular walls. In addition to holding food, it serves as the
mixer and grinder of food. The stomach secretes acid and powerful enzymes that continue the process of
breaking the food down and changing it to a consistency of liquid or paste. From there, food moves to the
small intestine. Between meals, the non-liquefiable remnants are released from the stomach and ushered
through the rest of the intestines to be eliminated.
Made up of three segments -- the duodenum, jejunum, and ileum -- the small intestine also breaks down
food using enzymes released by the pancreas and bile from the liver. The small intestine is the 'work
horse' of digestion, as this is where most nutrients are absorbed. Peristalsis is also at work in this organ,
moving food through and mixing it up with the digestive secretions from the pancreas and liver, including
bile. The duodenum is largely responsible for the continuing breakdown process, with the jejunum and
ileum being mainly responsible for absorption of nutrients into the bloodstream.
A more technical name for this part of the process is "motility," because it involves moving or emptying
food particles from one part to the next. This process is highly dependent on the activity of a large
network of nerves, hormones, and muscles. Problems with any of these components can cause a variety
of conditions.
While food is in the small intestine, nutrients are absorbed through the walls and into the bloodstream.
What's leftover (the waste) moves into the large intestine (large bowel or colon).
Everything above the large intestine is called the upper GI tract. Everything below is the lower GI tract
Stop 4: The Colon, Rectum, and Anus
The colon (large intestine) is a five- to seven -foot -long muscular tube that connects the small intestine to
the rectum. It is made up of the ascending (right) colon, the transverse (across) colon, the descending
(left) colon and the sigmoid colon, which connects to the rectum. The appendix is a small tube attached to
the ascending colon. The large intestine is a highly specialized organ that is responsible for processing
waste so that defecation (excretion of waste) is easy and convenient.
Stool, or waste left over from the digestive process, passes through the colon by means of peristalsis, first
in a liquid state and ultimately in solid form. As stool passes through the colon, any remaining water is
absorbed. Stool is stored in the sigmoid (S-shaped) colon until a "mass movement" empties it into the
rectum, usually once or twice a day.
It normally takes about 36 hours for stool to get through the colon. The stool itself is mostly food debris
and bacteria. These bacteria perform several useful functions, such as synthesizing various vitamins,
processing waste products and food particles, and protecting against harmful bacteria. When the
descending colon becomes full of stool, it empties its contents into the rectum to begin the process of
elimination.
The rectum is an eight-inch chamber that connects the colon to the anus. The rectum:
Receives stool from the colon
Lets the person know there is stool to be evacuated
Holds the stool until evacuation happens
When anything (gas or stool) comes into the rectum, sensors send a message to the brain. The brain
then decides if the rectal contents can be released or not. If they can, the sphincters relax and the rectum
contracts, expelling its contents. If the contents cannot be expelled, the sphincters contract and the
rectum accommodates so that the sensation temporarily goes away.
The anus is the last part of the digestive tract. It consists of the muscles that line the pelvis (pelvic floor
muscles) and two other muscles called anal sphincters (internal and external).
The pelvic floor muscle creates an angle between the rectum and the anus that stops stool from coming
out when it is not supposed to. The anal sphincters provide fine control of stool. The internal sphincter is
always tight, except when stool enters the rectum. It keeps us continent (not releasing stool) when we are
asleep or otherwise unaware of the presence of stool. When we get an urge to defecate (go to the
bathroom), we rely on our external sphincter to keep the stool in until we can get to the toilet.
Accessory Digestive Organs
Pancreas
Among other functions, the pancreas is the chief factory for digestive enzymes that are secreted into the
duodenum, the first segment of the small intestine. These enzymes break down protein, fats, and
carbohydrates.
Continue reading below...
Liver
The liver has multiple functions, but two of its main functions within the digestive system are to make and
secrete an important substance called bile and to process the blood coming from the small intestine
containing the nutrients just absorbed. The liver purifies this blood of many impurities before traveling to
the rest of the body.
Gallbladder
The gallbladder is a storage sac for excess bile. Bile made in the liver travels to the small intestine via the
bile ducts. If the intestine doesn't need it, the bile travels into the gallbladder, where it awaits the signal
from the intestines that food is present. Bile serves two main purposes. First, it helps absorb fats in the
diet, and secondly, it carries waste from the liver that cannot go through the kidneys.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- PTW QuestionareDocument63 pagesPTW QuestionareIshtiaq Ahmad100% (2)
- NVH PDFDocument3 pagesNVH PDFSubhendu BarisalNo ratings yet
- Working Capital Management at Padmavathi Co-operative BankDocument53 pagesWorking Capital Management at Padmavathi Co-operative BankMamidishetty Manasa67% (3)
- Characteristics of Technical WritingDocument3 pagesCharacteristics of Technical Writingakhilesh kumar pandey100% (1)
- Hemorrhage - A Isatypeof - It's Caused by An in The Bursting and Causing Localized Bleeding in The Surrounding Tissues. This Bleeding Kills CellsDocument1 pageHemorrhage - A Isatypeof - It's Caused by An in The Bursting and Causing Localized Bleeding in The Surrounding Tissues. This Bleeding Kills CellsJackie Swift FuntanillaNo ratings yet
- Jfnr07 2 p058 062 MinarovicovaDocument5 pagesJfnr07 2 p058 062 MinarovicovaJackie Swift FuntanillaNo ratings yet
- AppetizersDocument1 pageAppetizersJackie Swift FuntanillaNo ratings yet
- World Facts-1Document4 pagesWorld Facts-1Jack FuntanillaNo ratings yet
- Philippine HistoryDocument11 pagesPhilippine HistoryJackie Swift FuntanillaNo ratings yet
- Asst 16 Projectile Motion AnsDocument10 pagesAsst 16 Projectile Motion AnsJackie Swift FuntanillaNo ratings yet
- Ten Tough Interview Questions and Ten Great AnswersDocument8 pagesTen Tough Interview Questions and Ten Great AnswersJackie Swift FuntanillaNo ratings yet
- Nats Del Castillo Sdasdasd SD AsdewDocument12 pagesNats Del Castillo Sdasdasd SD AsdewJackie Swift FuntanillaNo ratings yet
- Taylor Swift Karaoke 1989 Digital Booklet - ITunesDocument18 pagesTaylor Swift Karaoke 1989 Digital Booklet - ITunesAirene SibleNo ratings yet
- 07 TorqueDocument16 pages07 TorqueJackie Swift FuntanillaNo ratings yet
- CH 9 PPT Cellular RespirationDocument47 pagesCH 9 PPT Cellular RespirationJackie Swift FuntanillaNo ratings yet
- Parthenogenesis - Cellular Mechanisms - Chromosomes, Meiosis, Animals, and Egg - Jrank Articles Mechanisms - Html#Ixzz37MdtlhzrDocument1 pageParthenogenesis - Cellular Mechanisms - Chromosomes, Meiosis, Animals, and Egg - Jrank Articles Mechanisms - Html#Ixzz37MdtlhzrJackie Swift FuntanillaNo ratings yet
- TAN PlanDocument3 pagesTAN PlanJackie Swift FuntanillaNo ratings yet
- EDocument3 pagesEJackie Swift FuntanillaNo ratings yet
- Chapter 2: 1-D Kinematics: Velocity & Acceleration Hints & Answers. - Updated 9/6/11Document8 pagesChapter 2: 1-D Kinematics: Velocity & Acceleration Hints & Answers. - Updated 9/6/11Jackie Swift FuntanillaNo ratings yet
- Basic Flower Parts and StructuresDocument5 pagesBasic Flower Parts and StructuresJackie Swift FuntanillaNo ratings yet
- 03 N-CycleDocument24 pages03 N-CycleJackie Swift FuntanillaNo ratings yet
- HistoryDocument14 pagesHistoryJackie Swift FuntanillaNo ratings yet
- 2012 05 25 112133 - 5226Document5 pages2012 05 25 112133 - 5226Jackie Swift FuntanillaNo ratings yet
- Introduction 20to 20zooplankton 20ecology08Document42 pagesIntroduction 20to 20zooplankton 20ecology08Jackie Swift FuntanillaNo ratings yet
- Nucleic Acids and Cell OrganellesDocument19 pagesNucleic Acids and Cell OrganellesJackie Swift FuntanillaNo ratings yet
- Defisiensi Bhs InggrisDocument3 pagesDefisiensi Bhs InggrisHanna KartikasariNo ratings yet
- Class Agnatha Integulatory SystemDocument5 pagesClass Agnatha Integulatory SystemJackie Swift Funtanilla100% (1)
- Amphi OxusDocument3 pagesAmphi OxusJackie Swift FuntanillaNo ratings yet
- John Lennon BiographyDocument3 pagesJohn Lennon BiographyJackie Swift FuntanillaNo ratings yet
- 07 TorqueDocument16 pages07 TorqueJackie Swift FuntanillaNo ratings yet
- ChondrichthyesDocument4 pagesChondrichthyesJackie Swift FuntanillaNo ratings yet
- Pamantasan NG Lungsod NG Maynila (University of The City of Manila) Intramuros, Manila Preliminary Registration Form First Semester, SY 2011 - 2012Document1 pagePamantasan NG Lungsod NG Maynila (University of The City of Manila) Intramuros, Manila Preliminary Registration Form First Semester, SY 2011 - 2012Jackie Swift FuntanillaNo ratings yet
- Hazop Recommendation Checked by FlowserveDocument2 pagesHazop Recommendation Checked by FlowserveKareem RasmyNo ratings yet
- DX DiagDocument42 pagesDX DiagVinvin PatrimonioNo ratings yet
- Repair Max II Pump 310894lDocument20 pagesRepair Max II Pump 310894lAndreina FajardoNo ratings yet
- Citi Global College Inc 12STEM3G72Document9 pagesCiti Global College Inc 12STEM3G72yanna villarealNo ratings yet
- ScreenwritingDocument432 pagesScreenwritingkunalt09100% (4)
- ARTS 9 Q4 Week 1Document3 pagesARTS 9 Q4 Week 1Elaissa MaglanqueNo ratings yet
- Ti 1000 0200 - enDocument2 pagesTi 1000 0200 - enJamil AhmedNo ratings yet
- Salt Analysis-Ferric ChlorideDocument3 pagesSalt Analysis-Ferric ChlorideVandana0% (1)
- IRC-114-2013 Use of Silica Fume in Rigid PavementDocument14 pagesIRC-114-2013 Use of Silica Fume in Rigid PavementZakee MohamedNo ratings yet
- Plano Electrico 785CDocument2 pagesPlano Electrico 785CLuis MartínezNo ratings yet
- LSAP 423 Tech Data 25kVA-40KVA - 3PH 400VDocument1 pageLSAP 423 Tech Data 25kVA-40KVA - 3PH 400Vrooies13No ratings yet
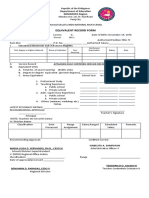
- Equivalent Record Form: Department of Education MIMAROPA RegionDocument1 pageEquivalent Record Form: Department of Education MIMAROPA RegionEnerita AllegoNo ratings yet
- MIL (Second Quarter)Document13 pagesMIL (Second Quarter)Menma ChanNo ratings yet
- ATM ReportDocument16 pagesATM Reportsoftware8832100% (1)
- Openstack Deployment Ops Guide PDFDocument197 pagesOpenstack Deployment Ops Guide PDFBinank PatelNo ratings yet
- Math 7: "The Nearest Approximation To An Understanding of Life Is To Feel It and Realize It To The Fullest."Document16 pagesMath 7: "The Nearest Approximation To An Understanding of Life Is To Feel It and Realize It To The Fullest."benjamin ladesma0% (1)
- Rostam's Seven LaboursDocument3 pagesRostam's Seven LaboursArifin SohagNo ratings yet
- ZO 503 Physiological Chemistry by Dr.S.S.KunjwalDocument22 pagesZO 503 Physiological Chemistry by Dr.S.S.KunjwalAbhishek Singh ChandelNo ratings yet
- Palo Alto Firewall VirtualizationDocument394 pagesPalo Alto Firewall VirtualizationRyanb378No ratings yet
- Case Study No. 11 - Hydroelectric Power Plant in The PhilippinesDocument26 pagesCase Study No. 11 - Hydroelectric Power Plant in The PhilippinespicefeatiNo ratings yet
- Sequence TransformationDocument2 pagesSequence Transformationbrown222No ratings yet
- Learn R For Applied StatisticsDocument457 pagesLearn R For Applied StatisticsyasortyNo ratings yet
- Vijay Solvex PROJECT "Retention Strategy"Document110 pagesVijay Solvex PROJECT "Retention Strategy"Jayesh SinghNo ratings yet
- Aligning With New Digital Strategy A Dynamic CapabilitiesDocument16 pagesAligning With New Digital Strategy A Dynamic Capabilitiesyasit10No ratings yet
- Stress-Busting Plan for Life's ChallengesDocument3 pagesStress-Busting Plan for Life's Challengesliera sicadNo ratings yet
- HDL Coder™ ReferenceDocument487 pagesHDL Coder™ ReferenceVictor Colpo NavarreteNo ratings yet
- Caribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDocument37 pagesCaribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDarrion BruceNo ratings yet