Professional Documents
Culture Documents
A Pain Education Programme
Uploaded by
api-2442306640 ratings0% found this document useful (0 votes)
68 views13 pagesOriginal Title
a pain education programme
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
68 views13 pagesA Pain Education Programme
Uploaded by
api-244230664Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 13
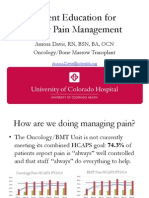
PAI N MANAGEMENT
A pain education programme to improve patient satisfaction with
cancer pain management: a randomised control trial
Pi-Ling Chou and Chia-Chin Lin
Aim. The purpose of this study was (1) to evaluate the effectiveness of a pain education programme to increase the satisfaction
of patients with cancer with regard to pain management and (2) to examine how patient satisfaction with pain management
mediates the barriers to using analgesics and analgesic adherence.
Background. The patients satisfaction with pain management is not merely an indicator, it is actually a contributor to med-
ication adherence. However, very few studies investigate methods for improving patient satisfaction with pain management.
Design. This study used an experimental and longitudinal design.
Methods. A total of 61 patientfamily pairs (n = 122) were randomly assigned to either experimental or control groups. The
instruments included the American Pain Society outcome questionnaire, the Barriers Questionnaire-Taiwan form, self-reporting
evaluations of analgesic adherence and the Pain Education Booklet. The experimental group (n = 31) participated in a pain
education programme, while those in the control group (n = 30) did not. The two groups were compared using generalised
estimation equations after the second and fourth weeks. A Sobel test was used to examine the mediating relationships among
patient satisfaction with pain management, barriers to using analgesics and analgesic adherence.
Results. The experimental group showed a signicant improvement in the level of satisfaction they felt for physicians and nurses
regarding pain management. For those in the experimental group, satisfaction with pain management was a signicant mediator
between barriers to using analgesics and analgesic adherence.
Conclusions. This research provides evidence supporting the effectiveness of a pain education programme for patients and their
family members in increasing patient satisfaction with regard to the management of cancer pain.
Relevance to clinical practice. It is important for health providers to consider patient satisfaction when attempting to improve
adherence to pain management regimes in a clinical setting.
Key words: barriers to pain management, cancer pain, mediator, nurses, nursing, pain education programme, pain management,
patient satisfaction
Accepted for publication: 9 January 2011
Introduction
Cancer pain is a serious clinical problem and improving the
means by which it is treated is an issue of critical importance
(Gordon et al. 2002, Jain et al. 2008). Assuring the quality of
cancer pain management by systematically evaluating the
methods employed in such treatment can enhance the effec-
tiveness of pain control in patients with cancer (Ward et al.
1998). The patients satisfaction with pain control is an
essential indicator in assessing the quality of cancer pain
management (Sterman et al. 2003, Panteli & Patistea 2007);
however, very few researchers have adopted a longitudinal
Authors: Pi-Ling Chou, MS, RN, Doctoral Student, Graduate
Institute of Nursing, College of Nursing, Taipei Medical University;
Chia-Chin Lin, PhD, RN, Professor and Director, School of Nursing,
College of Nursing, Taipei Medical University and Wan-Fang
Hospital, Taipei, Taiwan
Correspondence: Chia-Chin Lin, Professor and Director, School of
Nursing, College of Nursing, Taipei Medical University, No.250,
Wuxing St., Taipei 11031, Taiwan. Telephone: + 886 2 2377 6229.
E-mail: clin@tmu.edu.tw
1858 2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869
doi: 10.1111/j.1365-2702.2011.03740.x
approach to studying pain education as it pertains to this
issue. Patient satisfaction with pain control is not merely an
important indicator. If patients are more satised with their
pain management, they more likely to comply with the advice
of health providers (Hirsh et al. 2005). Previous studies
related to pain intervention have focused on barriers to
changing analgesics and the resulting inuence on patient
adherence to such treatment (Lin et al. 2006, Syrjala et al.
2008). Unfortunately, the means by which these barriers
inuence adherence remains unclear. A deeper under-
standing of the mechanisms involved in patient satisfaction
that dissuade patients from adhering to the prescribed use
of analgesics could prove extremely valuable in clinical
practice.
Background
Patient satisfaction towards their treatment was dened by
Lebow (1982) as the extent to which treatment graties the
wants, wishes and desires of clients. Several studies have
adopted the satisfaction that patients feel towards pain
management as an indicator for assessing the effectiveness of
pain management (de Wit et al. 2001, Jain et al. 2008).
Merkouris et al. (1999) reported that patient satisfaction
might provide the means to evaluate outcomes and act as a
contributor to other outcomes (i.e. adherence), inuencing
the process of recovery. Several researchers have discovered
that patient satisfaction with medical management could be
used to forecast medical outcomes, in addition to acting as an
outcome indicator (Meakin & Weinman 2002). For instance,
studies focusing on older patients suffering from coronary
heart disease discovered that the degree to which patients
adhere to the instructions they received regarding their
medication improves proportionally to the patients satisfac-
tion feel towards an increase in medical management from
their physicians and nurses (Rich et al. 1996, Rybacki 2002,
Simpson et al. 2002). Similarly, if the adherence of patients
increases with medical management, studies could more
accurately predict the outcome of health care services. Most
researchers recognise that patientprovider relationships and
patient satisfaction with those relationships are important
factors in adherence to treatment regimes (Cameron 1996,
Bos et al. 2005). One study indicated that the more satised
patients are with their pain management, the more they
comply with the advice of health care providers (Hirsh et al.
2005). Another study on chronic pain in children revealed
that the satisfaction of parents and children is signicantly
correlated with patient adherence (Simons et al. 2010).
Interventions that improve patient satisfaction could have a
positive inuence on the outcome of treatment for cancer pain.
Adherence to analgesic regimens has become one of the
most signicant clinical problems in the management of
cancer pain (Miaskowski et al. 2001). The lack of adher-
ence to analgesics is a result of myths regarding their use
(Tzeng et al. 2008, Valeberg et al. 2008). In the past few
decades, promoting and maintaining adherence to prescribed
analgesic regimens has become an important intervention in
the treatment of patients with cancer (Agency for Healthcare
Research and Quality 2001). As a result, many studies have
developed strict guidelines to ameliorate misconceptions
regarding pain and analgesics, and several of these interven-
tions have signicantly increased patient adherence to the
prescriptions of medical personnel (Ferrell et al. 1993, Lin
et al. 2006, Syrjala et al. 2008). Patients who had been
educated concerning pain intervention were less likely to self-
terminate their medication when the pain decreased. Pain
education programmes appear to be benecial in reducing
patient misconceptions regarding analgesics and improving
patient adherence to their analgesic regimens.
The cancer patients satisfaction feel towards pain manage-
ment programmes is a relatively new topic of discussion and
many of the implications are scarcely understood (Alalo &
Tselios 1996, Sherwood et al. 2000). Evaluating the level of
patients satisfaction with the management of their cancer
pain can provide a deeper understanding of their general
satisfaction with the treatment they receive from their
physicians and nurses. In a study by Sherwood et al.
(2000), patients with cancer who were dissatised with their
pain management perceived a lack of empathy among health
care professionals, who were slow to respond to their
complaints of pain. In addition, the same patients believed
that health care professionals did not have sufcient knowl-
edge or the skills required to properly manage their pain.
Dissatisfaction with pain management may be a reection of
poor pain management provided by health care professionals
(Sherwood et al. 2000).
Several studies have shown that interventions encourage
patients with cancer to overcome the barriers preventing
them from adhering to analgesics meant to reduce their pain.
However, the mechanisms involved in the reduction of such
barriers have never been explored. This study suggests that
patient satisfaction with pain management regimes is a
signicant factor inuencing medication adherence and fully
exploring these underlying mechanisms is crucial. This study
hypothesises that long-term education programmes address-
ing the issue of cancer pain management for patients and
their families would improve patient satisfaction. Patient
satisfaction with pain management could be a signicant
mediating factor among the various barriers to using anal-
gesics and analgesic adherence.
Pain management Pain education to improve pain management
2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869 1859
Methods
Participants and settings
This study, part of which has been published elsewhere (Lin
et al. 2006), is one component of a large randomised control
study. It was conducted in the oncology outpatient clinics of
two hospitals in Taipei, Taiwan. A purposive sample
consisting of outpatients and their primary caregivers was
recruited. Patientfamily pairs enrolled in the study were
randomly assigned to the experimental group or control
group using a computer-generated randomisation scheme
developed by the researcher. Random allocation sequences
and sealed, opaque envelopes were used to ensure security.
Two participants in the experimental group and two partic-
ipants in the control group discontinued involvement in the
study during the second assessment and three participants
stopped treatment after the third assessment. Sixty-one
patientfamily pairs (n = 122) completed the analysis, of
which 31 pairs were in the experimental group and 30 pairs
were in the control group (Fig. 1). Participants had to meet
the following criteria: (1) diagnosed with cancer; (2) expe-
riencing pain due to cancer and currently taking oral
analgesics; (3) over 18 years of age; and (4) ability to
communicate in Mandarin or Taiwanese. Participants suffer-
ing from cognitive impairment or brain metastasis were
excluded from the study. This study used SSIZE SSIZE software
(Hsieh 1991) to estimate the size of the sample from the pilot
study. Scores regarding patient satisfaction were used as the
primary outcome; with a r value of 005 and a test power of
85%. Satisfaction scores in the pretest were 35 (slightly
dissatised) and after two weeks 45 (somewhat satised).
Each group had to be maintained at 30 samples with a
difference of 1 between the two groups.
Instruments
The American Pain Society (APS) outcome questionnaire
The APS outcome questionnaire was developed from qual-
ity assurance studies, using identical tools for exploring
patient satisfaction with regard to the treatment of cancer-
related pain (Ward & Gordon 1994, Miaskowski et al.
1994). The standards proposed by the Quality Assurance
Committee of the APS were adopted in the development of
the questionnaire used in this study. In addition, the views
of patients regarding the means by which their doctors and
nurses managed their pain were also included (Max et al.
1991, Agency for Health Care Policy and Research 1994).
The questionnaire was translated into Mandarin using a
translation and back-translation method to ensure accuracy.
This questionnaire included three parts: (1) a patient
assessment of their satisfaction with the method of pain
management employed by their physician(s); (2) a patient
assessment of their satisfaction with the method of pain
management employed by their nurse(s); (3) a patient
assessment of their satisfaction with the overall treatment
they received for the management of their pain. This study
was scored on a six-point Likert scale ranging from 6 for
very satised 1 for very dissatised to establish reli-
ability and validity (Lin 2000, Panteli & Patistea 2007).
The Barriers Questionnaire-Taiwan form (BQT)
Ward and Colleagues proposed the Barriers Questionnaire
(BQ), which was specically developed to measure barriers to
the use of analgesics in patients with cancer (Ward et al.
1993). The BQT was translated and modied specically for
Taiwanese participants. It comprises nine subscales with 34
items (Lin & Ward 1995). Based on the results of content
analysis of the Taiwanese population, several items were
added to the BQT. The subscale of fear of injection was
dropped; and a three-item subscale labelled religious fatal-
ism was added. Another three-item subscale labelled P.R.N.
was also added. The nal BQT consisted of nine subscales,
Declined participation
(n = 19)
Not interested (n = 10)
Felt too burdensome (n = 4)
Other reasons (n = 5)
Randomised (n = 68)
Allocated to the
experimental group
(n = 34)
Allocated to the
control group
(n = 34)
Completed
assessment at T1
(n = 34)
Complete follow up at
T2 (n = 32)
Too ill (n = 2)
Completed
assessment at T1
(n = 34)
Complete follow up at
T2 (n = 32)
Transferred to hospice ward (n = 1)
Did not wish to continue (n = 1)
Complete follow up at
T3 (n = 31) Did not
wish to continue (n = 1)
Complete follow up at
T3 (n = 30)
Died (n = 1)
Missed because researcher
was unavailable (n = 1)
Assessed for eligibility
(n = 87)
Figure 1 Flow chart of the trial.
P-L Chou and C-C Lin
1860 2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869
with 34 items (Lin 2001). These subscales included the fol-
lowing: (1) addiction (three items); (2) disease progression
(three items); (3) pain tolerance (three items); (4) fatalism
(three items); (5) religious fatalism (three items); (6) P.R.N. or
as needed (three items); (7) concern about side effects
(10 items); (8) fear of distracting physicians (three items); and
(9) a desire to be good (three items). The BQT asks patients to
rate the extent to which they agree with each item on a scale
from 0 (do not agree at all) 5 (agree very much). This study
used both subscale scores and total score in the analyses. The
reliability and validity of the BQT were previously estab-
lished (Chang et al. 2002, Lin et al. 2006).
The Taiwanese version of the Morisky Medication Adherence
Measure (MMAM-T)
A structured four-item self-reporting measure of analgesic
adherence developed by Morisky et al. (1986) was adminis-
tered to patients to measure their compliance with analgesics.
The theory underlying this measure is that errors of drug
omission can occur for any or all of the following reasons:
forgetfulness, carelessness, cessation of the drug when feeling
better and use of the drug when feeling worse. The sum of the
yes answers provided a composite measure of non-adher-
ence. The total score ranged from 04, with higher scores
indicating a greater degree of adherence. The group showing
a high degree of adherence received a total score of 4; the
group with moderate adherence received a score of 23 and
the group with low adherence received a score of 01. A
Taiwanese sample with cancer pain veried the reliability and
concurrent construct validity of this measure (Tzeng et al.
2008).
Brief Pain Inventory-Chinese version (BPI-C)
This study uses the BPI-C version to measure the intensity of
pain and the degree to which pain interfered with daily
activities (Wang et al. 1996). The rst part of the BPI com-
prised the following four, single-item measures of pain
intensity, with each item rated on a scale of 0 (no pain) 10
(the worst pain I can imagine): (1) worst pain, (2) least pain,
(3) average pain and (4) pain now. A Taiwanese sample with
cancer pain established the reliability and validity of this
measure (Wang et al. 1996, Lin et al. 2006, Tsai et al. 2007).
The Pain Education Booklet
The primary researcher in this study developed the Pain
Education Booklet using concise descriptions and illustra-
tions to provide important information specic to Taiwanese
patients with cancer and their family caregivers, addressing
concerns of reporting pain and using analgesics. This pocket-
sized booklet is 16 pages long and addresses nine common
concerns. A panel of experts validated the content of the Pain
Education Booklet. Further modications to the content of
this booklet were made according to comments from patients
and experts. Cancer outpatients previously used this booklet in a
pain education programme (Chang et al. 2002, Lin et al. 2006).
Karnofsky Performance Status (KPS)
This study used the KPS to assess the performance status of
patients. The KPS is rated on a scale of 1100, in steps of 10.
The KPS has demonstrated a high level of predictive validity
(Buccheri et al. 1996).
Procedure
A research assistant approached patientfamily groups to
describe the study and obtain informed consent. On the day of
the rst interview, the patients in the experimental group lled
out the APS outcome questionnaire, the BQT, the BPI-C and
the self-reported measure of analgesics. They also ll out a
demographic questionnaire. After the patients had completed
the questionnaire, the research assistant provided a pain
education intervention session for patients and family caregiv-
ers, using the Pain Education Booklet. Researchers conducted
the session in a private room at the outpatient unit, to avoid
interruptions. The research assistant discussed all of the
content covered by the booklet and encouraged patients and
family caregivers to ask questions. The pain education session
took approximately 3040 minutes to complete. Patients and
family caregivers were encouraged to call phone numbers
included the booklet, following the education session, if they
required answers to any questions. Each participant received a
copy of the pain education booklet. The second and third
interviews were conducted two and four weeks after the pain
education session, respectively. At each interview, the patients
were asked to complete the questionnaire again. Researchers
took the chance to answer any questions the patients or family
caregivers had and reviewed the information on pain educa-
tion. Patients and their family caregivers in the control group
received conventional care. Patients in the control group
individually and independently completed the questionnaires
on pain and demographic data during the rst interview. They
complete the questionnaires during the two- and four-week
follow-up interviews. The control group did not receive an
education programme. The research assistant only answered
questions asked by patients or family caregivers. If the
interviewer observed that a patient appears to be in pain or
distress, or if a patient verbalised pain or distress, the
assessment or follow-up would cease until the patient was
relieved fromthese symptoms. Noadverse events or side effects
resulted from the intervention.
Pain management Pain education to improve pain management
2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869 1861
Data analysis
This study used complete analysis to interpret the collected
data. The generalised estimating equations (GEE) analyses
the effects of the pain education programme on patient
satisfaction, and the Sobel test under the SAS SAS system (version
8.2; SAS Institute Inc., Cary, NC, USA) assesses the mediating
role on the barriers to using analgesics and analgesic adher-
ence. To account for repeated measurement dependence that
might occur at the two- and four-week intervals (Liang &
Zeger 1986, Zeger & Liang 1992, Lin et al. 2006), GEE were
used to analyse whether the pain education programme
improved patient satisfaction with nurses and physicians.
The GEE analysis compensated for the baseline heterogeneity
(differences existing before the intervention) between the
experimental and control groups and the effects of maturation
(changes in outcome variables resulting from the passage of
time). To control for the effect of pain intensity on patient
satisfaction, this study factored the mean pain intensity (worst
pain + average pain + least pain + painnow/4) intothe analytic
model. As hypothesised in this study, patients in the experi-
mental group displayed a greater degree of satisfaction regard-
ing pain management. The patients satisfaction with regard to
pain management was a signicant mediator between barriers
to using analgesics and analgesic adherence. The Sobel test
described by Baron and Kenny (1986) and Preacher and Hayes
(2004) was used to examine the mediating effects of variables.
In this manner, we were able to estimate the direct, indirect and
total effects of the causal relationships involving this mediating
variable. In this study, the Sobel test under the SAS SAS system
(version 8.2) was used to assess the mediating role of patient
satisfaction on barriers to using analgesics and analgesic
adherence.
Ethical approval
This study obtained approval from the Human Subject
Committee of the hospital. All subjects signed written
informed consent forms.
Results
Demographic information
The participants in this study suffered from various forms of
cancer, including nasopharyngeal (21%), breast (18%), oral
(16%), liver (13%), lung (6%), colorectal (6%) and various
others (20%). In the experimental group, 61% of the
participants were women. The mean age was 55 (SD
1438). The mean years of education were 774 (SD 423).
The mean KPS score was 81 (SD 138). The mean pain
intensity score was 331 (SD 137) before intervention.
Among these participants in the experimental group, the
cancer identied in 77% of the test subjects had metastasised.
In the control group, 60% of the patients were women.
The mean age was 59 (SD 1660). The mean years of
education were 857 (SD 488). The mean KPS score was 85
(SD 114). The mean pain intensity score was 376 (SD 194)
before intervention. Among these participants in the control
group, the cancer identied in 70% of the test subjects had
metastasised. No signicant difference was displayed be-
tween the two groups regarding the prescriptions (ex:
NSAID, codeine/tramadol, morphine, fentanyl, adjuvant
drugs) provided by physicians. No signicant demographic
differences were noted between the two groups, with the
exception of treatment status (i.e. patients who received
chemotherapy or radiotherapy vs. those who received
neither), which reached signicance (p = 002).
Determining whether the pain education programme
improved patient satisfaction with the pain management
provided by nurses
There was no signicant difference at baseline (p = 01065) in
patients satisfaction levels between the two groups. The
control group showed a signicant maturation effect in the
second and fourth weeks (p = 00027 and p = 00073).
However, the elevation slope of the experimental group
was signicantly higher than that of the control group in both
the second (p < 00001) and fourth weeks (p = 00002),
after adjusting for the effects of treatment and mean pain
intensity. Clearly, the pain education programme signicantly
increased patient satisfaction with the nurses. The satisfac-
tion felt by the experimental group regarding the pain
management of nurses increased signicantly from 395
during the pretest to 518 by the fourth week. On the
contrary, the satisfaction felt by the control group was 428
during the pretest and 472 by the fourth week. Although
both groups displayed a signicant elevation in satisfaction
levels from the pretest to the fourth week, only a minimal
increase in patient satisfaction was observed between the
second week and the fourth week (Fig. 2; Table 1).
Determining whether the pain education programme
improved patient satisfaction with pain management
conducted by physicians
The baseline scores of the experimental group were signi-
cantly lower than the control group with regard to satisfac-
tion with the pain management conducted by physicians
P-L Chou and C-C Lin
1862 2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869
(p = 00002). The control group showed signicant matura-
tion in the second week (p = 00415). However, the elevation
slope of the experimental group was signicantly greater than
the control group in both the second (p < 00001) and the
fourth weeks (p < 00001) after adjusting for baseline
heterogeneity, the effect of treatment and mean pain inten-
sity. The pain education programme signicantly improved
patient satisfaction with physicians. The satisfaction felt by
the experimental group regarding the pain management of
physicians increased signicantly from 454 during the pretest
to 564 by fourth week. In contrast, the satisfaction felt by the
control group was 511 during the pretest and 545 by the
fourth week. Despite the signicant improvement in satisfac-
tion in both groups between the pretest and the fourth week,
only a slight improvement was observed in patient satisfac-
tion between the second week and the fourth week (Fig. 3;
Table 2).
Determining the mediating role of patient satisfaction
with nurses to barriers in using analgesics and adherence
to the prescribed use of analgesics
One of the objectives of this study was to determine whether
patient satisfaction with nurses was a mediating factor
between barriers to using analgesics and adherence to the
prescribed use of analgesics. The results revealed that in the
experimental group, patient satisfaction with pain manage-
ment was a mediator between barriers to using analgesics and
adherence to the prescribed use of analgesics (p < 00001),
accounting for 4773% of the observed mediation (Table 3).
However, no mediation relationship was observed in the
control group. Figure 4 shows a path analytic model of the
relationships related to patient satisfaction with nurses,
barriers to analgesic use and adherence to the prescribed
use of analgesics.
Determining the mediating role of patient satisfaction
with physicians on barriers to the use of analgesics and
adherence to the prescribed use of analgesics
This study examined patient satisfaction with physicians to
determine whether a mediating relationship existed between
satisfaction and barriers to the use of analgesics and
adherence to the prescribed use of analgesics. The results
showed that in the experimental group, patient satisfaction
with pain management was a mediator between barriers to
using analgesics and adherence to the prescribed use of
analgesics (p < 00001), accounting for 4556% of the
mediation (Table 3). However, no mediating relationship
Patients satisfaction with nurses (n = 61)
1
2
3
1
2 3
0
1
2
3
4
5
6
Test time
S
c
o
r
e
Experimental group
Control group
Experimental
395 507 518
Control
428 47 472
1 2 3
Figure 2 Patients satisfaction score with nurses of Experimental
Group and Control Group (1 = pretest, 2 = second week, 3 = fourth
week). Note: Score was estimated with a generalised estimating
equations model of the patient satisfaction with nurses.
Table 1 Generalised estimating equations model of the patient satisfaction with nurses (n = 61)
Variable
Regression
coefcient
Standard
deviation Z p
Intercept 42817 02391 1791 <00001
Experimental vs. control group 02321 01438 161 01065
Second week vs. pretest 04204 01401 300 00027*
Fourth week vs. pretest 04358 01624 268 00073*
Interaction between second week and group 06991 01561 448 <0001*
Interaction between fourth week and group 07895 02134 370 00002*
Treatment status (yes vs. no) 02535 01539 165 00995
Mean pain intensity (worst pain + average pain + least pain + pain now/4) 00646 00421 153 01248
Interaction between second week and group shows the difference between the experimental and control groups in change between pretest and
second week. Interaction between fourth week and group shows the difference between experimental and control groups in change from pretest
to fourth week. The change in the experimental group is represented by the change in the control group plus the interaction term.
*p < 005.
Pain management Pain education to improve pain management
2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869 1863
was evident in the control group. Figure 5 displays a path
analytic model of the relationships between patient satisfac-
tion with physicians, barriers to analgesic use and adherence
to the prescribed use of analgesics.
Discussion
Very few studies have examined the effectiveness of inter-
vention on patient satisfaction with pain management. Even
fewer studies have shown signicant improvements in patient
satisfaction with pain management, despite implementing
educational interventions. One long-term study (de Wit et al.
1997) conducted in the Netherlands in 1997 focused on 313
homecare patients with cancer. During hospitalisation, health
care professionals conducted face-to-face pain education
followed by a telephone-delivered reiteration of pain educa-
tion on the third and seventh days following discharge. The
researchers found no signicant improvement in satisfaction
with pain control, despite a reduction in pain intensity (de
Wit et al. 1997). Yates et al. (2004) conducted a pain
education programme with 189 homecare patients with
cancer. During the return visit, the health care professionals
administered a pain education session with the patients and
conducted a telephone interview one week after the visit.
Although the programme enhanced the perception of control
in the minds of patients, no signicant difference in patient
satisfaction with pain management was observed between the
rst week and second month following the intervention
(Yates et al. 2004). This may be attributed to the fact that the
interviews on pain education were conducted over the
telephone without face-to-face contact between patients and
medical staff. In addition, the education did not involve any
family members. In this study, however, pain education
consisted of an extended, face-to-face intervention involving
patients and family caregivers.
Previous studies have revealed that the level of patient
satisfaction with pain control might be inuenced by multiple
factors. Sherwood identied three factors inuencing the
patients satisfaction feel regarding pain management. These
factors included previous experience with pain (affecting
beliefs and attitudes regarding pain management and expec-
tations about pain); patient appraisals of health care profes-
sionals (if the health care professionals managed pain with
empathy, care, sufcient knowledge and technique); and
personal experience managing pain (such as the involvement
of family caregivers in the treatment plan and the develop-
ment of effective strategies to cope with pain) (Sherwood
et al. 2000). Studies have also investigated the satisfaction
felt by patients with terminal cancer regarding pain manage-
ment using phenomenology. These studies revealed three
1
2
3
1
2
3
0
1
2
3
4
5
6
Test time
S
c
o
r
e
Experimental group
Control group
Experimental
group
454 552 564
Control
group
511 541 545
1 2 3
Patients satisfaction physicians (n = 61)
Figure 3 Patient satisfaction with physicians in the Experimental and
Control Groups (1 = pretest, 2 = second week, 3 = fourth week).
Score was estimated by generalised estimating equations model of
patient satisfaction with physicians.
Table 2 Generalised estimating equations model of patients satisfaction with physicians (n = 61)
Variable
Regression
coefcient
Standard
deviation Z p
Intercept 51124 01894 270 <00001
Experimental vs. control group 05722 01535 373 00002*
Second week vs. pretest 02970 01457 204 00415*
Fourth week vs. pretest 03396 01853 183 00069*
Interaction between second week and group 06812 01579 431 <00001*
Interaction between fourth week and group 07566 01953 387 00001*
Treatment status (yes vs. no) 00359 00875 041 06817
Mean pain intensity (worst pain + average pain + least pain + pain now/4) 01437 00371 387 00001
Interaction between second week and group shows the difference between the experimental and control groups in change between pretest and
second week. Interaction between fourth week and group shows the difference between experimental and control groups in change from pretest
to fourth week. The change in the experimental group is represented by the change in the control group plus the interaction term.
*p < 005.
P-L Chou and C-C Lin
1864 2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869
themes inuencing patient satisfaction with pain manage-
ment: communication, planning and trust. Patients expect
health care professionals to communicate in an open and
honest manner regarding pain management. After physi-
cians and nurses gain the trust of patients, patients show an
increased willingness to participate in the pain management
plan (Bostrom et al. 2004). Other factors that may con-
tribute to patient satisfaction with pain management
include a greater degree of social support (Jamison et al.
1993) and the physicianpatient relationship, manifesting
itself as an awareness of empathy and condence in
physicians and nurses (Jamison et al. 1993), such that
patients trust their health care providers (McCracken et al.
1997, Jensen et al. 2004). In addition, a recent study
revealed the four main factors inuencing satisfaction with
the quality of pain management. These included adminis-
tering treatment in a respectful manner, the provision of a
safety net, the efcacy of pain management and the
involvement of the patient as a partner. Among the four
factors, a collaborative relationship between patients and
health care professionals was the most important factor in
pain management determining the degree of control per-
ceived by patients (Beck et al. 2010).
In this study, several factors may explain how providing
pain education contributes to improving patient satisfaction
with pain management. Long-term engagements consisting of
multiple face-to-face visits with systematic pain education
provided patients with the opportunity to discuss how pain
management ought to be implemented. Such discussions
provided the opportunity to describe pain symptoms, evaluate
the effectiveness of medication and discuss the pain manage-
ment plan with physicians and nurses during every clinical
visit. In addition, researchers encouraged patients to take
an active role in their pain treatment and health care
BQT
score
Adherence
049* 085*
Without mediation: 087*
With mediation: 046*
Patient
satisfaction
with nurses
Figure 4 The mediation relationship of patient satisfaction with
nurses on the Barriers Questionnaire-Taiwan form score and anal-
gesic adherence in the experimental group. *p < 005.
BQT
score
Adherence
047* 084*
Without mediation: 087*
With mediation: 047*
Patient
satisfaction
with physicians
Figure 5 The mediation relationship of patient satisfaction with
physicians on the Barriers Questionnaire-Taiwan form score and
analgesic adherence in the experimental group. *p < 005.
Table 3 Sobel test for the mediation effects of patient satisfaction with nurses and physicians on the barriers adherence relationship in the
experimental group
Std b SE p-value
Test of mediation pathway of patient satisfaction with nurses
Barriers (predictor) adherence (outcome) 087 014 <00001
Barriers (predictor) satisfaction (mediator) 049 008 <00001
Satisfaction (mediator) adherence (outcome) 085 016 <00001
Barriers (predictor) adherence (outcome) with mediator 046 015 00028
Mediation results Per cent of the total effect
that is mediated:
4743%
Test statistic: 393 p-value: <00001
Test of mediation pathway of patient satisfaction with physicians
Barriers (predictor) adherence (outcome) 087 014 <00001
Barriers (predictor) satisfaction (mediator) 047 008 <00001
Satisfaction (mediator) adherence (outcome) 084 017 <00001
Barriers (predictor) adherence (outcome) with mediator 047 015 00022
Mediation results Per cent of the total effect
that is mediated:
4556%
Test statistic: 382 p-value: 00001
p-value at 005 level.
Std b, standardised beta coefcient; SE, standard error.
Pain management Pain education to improve pain management
2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869 1865
professionals were expected to keep lines of communication
open regarding the outcomes of pain management interven-
tion. When patients experience care and empathy delivered in
a consistent manner, they perceive their relationship with
health care professionals as collaborative. These factors may
contribute to improving perceptions of pain management.
The factors that inuence adherence are multidimensional.
Several scholars have taken a socio-psychological perspective
in suggesting several factors that inuence patient adherence,
including the physicianpatient relationship, the communi-
cative skills of physicians, the provision of information and
social support (Cameron 1996, Ryan 1999, Lowe et al.
2000). The behaviour and attitudes displayed by health care
professionals can positively or negatively inuence the
adherence of patients (Cameron 1996). One important factor
contributing to the under-treatment of cancer pain is a lack of
adherence to the therapeutic regimen (Lin et al. 2006, Tzeng
et al. 2008, Valeberg et al. 2008). In previous studies, pain
interventions signicantly increased patients knowledge of
pain, but did not improve their adherence to taking analgesics
(Wells et al. 2003, Miaskowski et al. 2004). These results
indicate that merely enhancing patient knowledge with
regard to medication does not signicantly improve adher-
ence to taking prescribed medication. Patient adherence is
inuenced by multidimensional elements, such as socio-
psychological perspectives, which health care professionals
must consider when attempting to break down barriers that
prevent patients with cancer from taking analgesics. Such
considerations could be far more effective than merely
focusing on enhancing patient knowledge. Improving patient
satisfaction with medical care is another way to increase
adherence to prescribed analgesic use, thereby improving the
management of cancer pain.
Results of this study indicate that the implementation of
pain education noticeably increased satisfaction scores dur-
ing the second- and fourth-week follow-ups, compared with
the satisfaction scores in the pretest. Nevertheless, the scores
of the experimental group regarding satisfaction with pain
management provided by nurses signicantly improved from
507 in the second week to 518 by fourth week. In addition,
satisfaction with the pain management provided by physi-
cians increased from 552564 by the fourth week. How-
ever, this incremental improvement was insufcient to
achieve statistical signicance. This study adopted a Likert
six-point scale for the satisfaction questionnaire. Patients
satisfaction felt towards the pain management provided by
nurses was 395 during the pretest, which was between
somewhat unsatised and somewhat satised. In the
second week, the level of satisfaction signicantly increased
to display a score between satised and extremely satised.
On the other hand, patient satisfaction with their physician
was between somewhat satised and satised with a score
of 454 during the pretest, signicantly improving to a point
between satised and extremely satised by the second
week. The above results reveal that patients felt satised to
extremely satised by the second week of pain education.
However, no signicant difference in the change of satisfac-
tion felt by patients was observed during the fourth week.
Because this study only tracked patient satisfaction for four
weeks, no demonstrable change in follow-up satisfaction was
observed. This study suggests several possible explanations
for the lack of signicant changes in satisfaction between the
second and fourth weeks. First, the score regarding the
satisfaction of pain management displayed extremely right-
skewed distribution. Owing to the inuence of ceiling effect,
the margin of improvement was limited. In addition, long-
term follow-up investigation regarding the ongoing commu-
nication between cancer outpatients and physicians revealed
that dimensions such as interest/engagement or friendliness/
warmth were signicantly correlated with the patients
satisfaction felt towards physicians one week or three -
months after outpatient visits. In addition, the correlation
coefcient showed nearly no change, suggesting that there
were no signicant changes in patient satisfaction with
physicians over the short-term or the long-term (Ong et al.
2000). Other studies have also mentioned that testretest
reliability related to satisfaction with physicians was moder-
ately correlated after four weeks (r = 041) (Lam et al. 2005).
Meanwhile, the testretest coefcient regarding patient
satisfaction adopted by the consultation satisfaction ques-
tionnaire was 082 within three weeks (Baker & Whiteld
1992). These studies revealed that patient satisfaction
regarding physicians is relatively stable correlated across
time. Additionally, we must not exclude the degree to which
subsequent interaction with other staff members or patients
cloud these relationships. Because this study only collected
follow-up data for four weeks, we were unable to investigate
long-term changes with regard to satisfaction. Therefore, we
suggest a future study including long-term follow-ups to
gauge changes in the level of patient satisfaction with pain
management.
This study was limited by several factors. First, it was not a
double-blind study. Second, patient satisfaction with physi-
cians or nurses accounted for 45564773% of the mediation
effect on barriers to using analgesics and adherence to the
prescribed use of analgesics. Other factors, such as social
circumstances or medication side effects may have inuenced
these relationships, but remain unexplored. Third, the sample
size used to conduct the Sobel test used to estimate the
mediation effect was small.
P-L Chou and C-C Lin
1866 2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869
This is the rst study investigating pain education as a way
to improve the long-term patient satisfaction feel towards
pain management, with an examination of the mediating
effect of patient satisfaction on pain control. This study
found that systematic, face-to-face pain education involving
multiple visits with patients and family caregivers can result
in the long-term enhancement of patient satisfaction with
pain management.
Conclusions
This study veried that patient satisfaction is a mediator with
regard to the barriers to using analgesics and analgesic
adherence. The outcome of the study not only supports the
efcacy of pain education programmes among patients,
family caregivers and medical personnel to improve patient
satisfaction but also emphasises the important role of patient
satisfaction in improving analgesic adherence in patients with
cancer. This change in behaviour could ultimately result in
improvements in the management of cancer pain.
Relevance to clinical practice
Patient satisfaction with physicians and nurses operates
partially as a mediating factor and cannot be discounted
when attempting to improve adherence to the prescribed use
of analgesics. The results of this study show that with respect
to the control of cancer pain, the enhancement of patient
satisfaction can signicantly improve patient adherence. If
physicians and nurses attend only to the delivery of knowl-
edge concerning medication, they may fail to convey to
patients the respect, empathy and active listening patients
need to feel fully satised with their physicians and nurses and
improve patient adherence to the prescribed use of analgesics.
Acknowledgements
The NSC 89-2314-B-083-069 from the National Science
Council in Taiwan funded this study. The authors thank Ms
Denise Dipert for her careful review and for editing this
manuscript.
Contributions
Study design: PLC, CCL; data collection and analysis: PLC
and manuscript preparation: PLC, CCL.
Conict of interest
None declared.
References
Afilalo M & Tselios C (1996) Pain relief
versus patient satisfaction. Annals of
Emergency Medicine 27, 436438.
Agency for Health Care Policy and Research
(1994) Public Health Service. Manage-
ment of Cancer Pain. AHCPR publ. no.
94-0592, AHCPR, Public Health Ser-
vice, U.S. Department of Health and
Human Services, Rockville, MD.
Agency for Healthcare Research and Qual-
ity (2001) Management of Cancer Pain.
AHRQ Publication No. 02-E002.
Agency for Healthcare Research and
Quality, U.S. Department of Health
and Human Services, Rockville, MD.
Baker R & Whitfield M (1992) Measuring
patient satisfaction: a test of construct
validity. Quality in Health Care 1, 104
109.
Baron RM & Kenny DA (1986) The mod-
erator-mediator variable distinction in
social psychological research: concep-
tual, strategic and statistical consider-
ations. Journal of Personality and
Social Psychology 51, 11731182.
Beck SL, Towsley GL, Berry PH, Lindau K,
Field RB & Jensen S (2010) Core as-
pects of satisfaction with pain man-
agement: cancer patients perspectives.
Journal of Pain and Symptom Man-
agement 39, 100115.
Bos A, Vosselman N, Hoogstraten J &Prahl-
Andersen B (2005) Patient compliance:
a determinant of patient satisfaction?
The Angle Orthodontist 75, 526531.
Bostrom B, Sandh M, Lundberg D &
Fridlund B (2004) Cancer-related pain
in palliative care: patients perceptions
of pain management. Journal of Ad-
vanced Nursing 45, 410419.
Buccheri G, Ferrigno D & Tamburini M
(1996) Karnofsky and ECOG perfor-
mance status scoring in lung cancer: a
prospective, longitudinal study of
536 patients from a single institution.
European Journal of Cancer 32, 1135
1141.
Cameron C (1996) Patient compliance: rec-
ognition of factors involved and sug-
gestions for promoting compliance with
therapeutic regimens. Journal of
Advanced Nursing 24, 244250.
Chang MC, Chang YC, Chiou JF, Tsou TS
& Lin CC (2002) Overcoming patient-
related barriers to cancer pain man-
agement for home care patients: a pilot
study. Cancer Nursing 25, 470476.
Ferrell BR, Rhiner M & Ferrell BA (1993)
Development and implementation of a
pain education program. Cancer 72,
34263432.
Gordon DB, Pellino TA, Miaskowski C,
McNeill JA, Paice JA, Laferriere D &
Bookbinder M (2002) A 10-year review
of quality improvement monitoring in
pain management: recommendations
for standardized outcome measures.
Pain Management Nursing 3, 116130.
Hirsh AT, Atchison JW, Berger JJ, Waxen-
berg LB, Lafayette-Lucey A, Bulcourf
BB & Robinson ME (2005) Patient
satisfaction with treatment for chronic
pain: predictors and relationship to
compliance. The Clinical Journal of
Pain 21, 302310.
Pain management Pain education to improve pain management
2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869 1867
Hsieh FY (1991) SSIZE: a sample size pro-
gram for clinical and epidemiologic
studies. American Statistician 45, 338.
Jain PN, Myatra SN, Kakade AC & Sareen
R (2008) An evaluation of postopera-
tive epidural analgesia in acute pain
service in an Indian cancer hospital (a
preliminary experience of patient satis-
faction survey). Acute Pain 10, 914.
Jamison RN, Taft K, OHara JP & Ferrante
FM (1993) Psychosocial and pharma-
cologic predictors of satisfaction with
intravenous patient-controlled analge-
sia. Anesthesia and Analgesia 77, 121
125.
Jensen MP, Mendozac T, Hanna DB, Chen
C & Cleeland CS (2004) The analgesic
effects that underlie patient satisfaction
with treatment. Pain 110, 480487.
Lam WWT, Fielding R, Chow L, Chan M,
Leung GM & Ho EYY (2005) Brief
communication: the Chinese medical
interview satisfaction scale-revised
(C-MISS-R): development and valida-
tion. Quality of Life Research 14,
11871192.
Lebow J (1982) Consumer satisfaction with
mental health treatment. Psychological
Bulletin 91, 244259.
Liang KY & Zeger SL (1986) Longitudinal
data analysis using generalized liner
models. Biometrika 73, 1322.
Lin CC (2000) Applying the American Pain
Societys QA standards to evaluate the
quality of pain management among
surgical, oncology, and hospice in-
patients in Taiwan. Pain 87, 4349.
Lin CC (2001) Congruity of cancer pain
perceptions between Taiwanese patients
and family caregivers: relationship to
patients concerns about reporting pain
andusing analgesics. Journal of Painand
Symptom Management 21, 1826.
Lin CC & Ward SE (1995) Patient-related
barriers to cancer pain management in
Taiwan. Cancer Nursing 18, 1622.
Lin CC, Chou PL, Wu SL, Chang YC & Lai
YL (2006) Long-term effectiveness of a
patient and family pain education
program on overcoming barriers to
management of cancer pain. Pain 122,
271281.
Lowe C, Raynor DK, Purvis J, Farrin A &
Hudson J (2000) Effects of a medicine
review and education programme for
older people in general practice. British
Journal of Clinical Pharmacology 50,
172175.
Max M, Donoven M, Portenoy RK, Clee-
land CS, Ready LB, Carr DB, Edwards
WT, Simmonds MA & Evans WO
(1991) American Pain Society quality
assurance standards for relief of acute
pain and cancer pain. In Proceedings of
the IV th World Congress on Pain
(Bond M, Charlton J & Woolf C eds).
Elsevier, Amsterdam, pp. 186189.
McCracken LM, Klock PA, Mingay DJ,
Asbury JK & Sinclair DM (1997)
Assessment of satisfaction with treat-
ment for chronic pain. Journal of Pain
and Symptom Management 14, 292
299.
Meakin R & Weinman J (2002) The Med-
ical Interview Satisfaction Scale (MISS-
21) adapted for British general practice.
Family Practice 19, 257263.
Merkouris A, Ifantopoulos J, Lanara V &
Lemonidou C (1999) Patient satisfac-
tion: a key concept for evaluating and
improving nursing services. Journal of
Nursing Management 7, 1928.
Miaskowski C, Nichols R, Broady R & Sy-
nold T (1994) Assessment of patient
satisfaction utilizing the American Pain
Societys quality assurance standards on
acute and cancer pain. Journal of Pain
and Symptom Management 9, 511.
Miaskowski C, Dodd MJ, West C, Paul SM,
Tripathy D, Koo P & Schumacher K
(2001) Lack of adherence with the
analgesic regimen: a significant barrier
to effective cancer pain management.
Journal of Clinical Oncology 19, 4275
4279.
Miaskowski C, Dodd M, West C, Schum-
acher K, Paul SM, Tripathy D & Koo P
(2004) Randomized clinical trial of the
effectiveness of a self-care intervention
to improve cancer pain management.
Journal of Oncology 22, 17131720.
Morisky DE, Green LW & Levine DM
(1986) Concurrent and predictive
validity of a self-reported measure of
medication adherence. Medical Care
24, 6774.
Ong LM, Visser MR, Lammes FB & de
Haes JC (2000) Doctor-Patient com-
munication and cancer patients quality
of life and satisfaction. Patient Educa-
tion and Counseling 41, 145156.
Panteli V & Patistea E (2007) Assessing
patients satisfaction and intensity of
pain as outcomes in the management of
cancer-related pain. European Journal
of Oncology Nursing 11, 424433.
Preacher KJ & Hayes AF (2004) SPSS and
SAS procedures for estimating indirect
effects in simple mediation models.
Behavior Research Methods, Instru-
ments, & Computers 36, 717731.
Rich MW, Gray DB, BeckhamV, Wittenberg
C & Luther P (1996) Effect of a multi-
disciplinary intervention on medication
compliance in elderly patients with
congestive heart failure. The American
Journal of Medicine 101, 270276.
Ryan AA (1999) Medication compliance
and older people: a review of the liter-
ature. International Journal of Nursing
Studies 36, 153162.
Rybacki JJ (2002) Improving cardiovascular
health in postmenopausal women by
addressing medication adherence issues.
Journal of the American Pharmaceuti-
cal Association 42, 6371.
Sherwood G, Adams-McNeill J, Starck PL,
Nieto B & Thompson CJ (2000)
Qualitative assessment of hospitalized
patients satisfaction with pain man-
agement. Research in Nursing &
Health 23, 486495.
Simons LE, Logan DE, Chastain L & Ce-
rullo M (2010) Engagement in multi-
disciplinary interventions for pediatric
chronic pain: parental expectations,
barriers and child outcomes. The Clin-
ical Journal of Pain 26, 291299.
Simpson SH, Johnson JA, Farris KB &
Tsuyuki RT (2002) Development and
validation of a survey to assess barriers
to drug use in patients with chronic
heart failure. Pharmacotherapy 22,
11631172.
Sterman E, Gauker S & Krieger J (2003)
Continuing education: a comprehensive
approach to improving cancer pain
management and patient satisfaction.
Oncology Nursing Forum 30, 857864.
Syrjala KL, Abrams JR, Polissar NL, Hans-
berry J, Robison J, DuPen S, Stillman
M, Fredrickson M, Rivkin S, Feldman
E, Gralow J, Rieke JW, Raish RJ, Lee
DJ, Cleeland CS & DuPen A (2008)
Patient training in cancer pain man-
agement using integrated print and vi-
deo materials: a multisite randomized
controlled trial. Pain 135, 175186.
Tsai PS, Chen PL, Lai YL, Lee MB & Lin
CC (2007) Effects of electromyography
biofeedback-assisted relaxation on pain
in patients with advanced cancer in a
palliative care unit. Cancer Nursing 30,
347353.
P-L Chou and C-C Lin
1868 2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869
Tzeng JI, Chang CC, Chang HJ & Lin CC
(2008) Assessing analgesic regimen
adherence with the Morisky Medica-
tion Adherence Measure for Taiwanese
patients with cancer pain. Journal of
Pain and Symptom Management 36,
157166.
Valeberg B, Miaskowski C, Hanestad B,
Bjordal K, Moum T & Rustoen T
(2008) Prevalence rates for and predic-
tors of self-reported adherence of
oncology outpatients with analgesic
medications. The Clinical Journal of
Pain 24, 627636.
Wang XS, Mendoza TR, Gao SZ & Clee-
land CS (1996) The Chinese version of
the Brief Pain Inventory (BPI-C): its
development and use in a study of
cancer pain. Pain 67, 407416.
Ward SE & Gordon D (1994) Application
of the American Pain Society qual-
ity assurance standards. Pain 56, 299
306.
Ward SE, Goldberg N, Miller-McCauley V,
Mueller C, Nolan A, Pawlik-Plank D,
Robbins A, Stormoen D & Weissman
DE (1993) Patient-related barriers to
management of cancer pain. Pain 52,
319324.
Ward S, Donova M & Max MB (1998) A
survey of the nature and perceived
impact of quality improvement activi-
ties in pain management. Journal of
Pain and Symptom Management 15,
365373.
Wells N, Hepworth JT, Murphy BA, Wujcik
D & Johnson R (2003) Improving
cancer pain management through pa-
tient and family education. Journal of
Pain and Symptom Management 25,
344356.
de Wit R, van Dam F, Zandbelt L, van
Buuren A, van der Heijden K, Leenh-
outs G & Loonstra S (1997) A pain
education program for chronic cancer
pain patients: follow up results a ran-
domized controlled trial. Pain 73, 55
69.
de Wit R, van Dam F, Loonstra S, Zandbelt
L, van Buuren A, van der Heijden K,
Leenhouts G & Huijer Abu-Saad H
(2001) The Amsterdam Pain Manage-
ment Index compared to eight fre-
quently used outcome measures to
evaluate the adequacy of pain treatment
in cancer patients with chronic pain.
Pain 91, 339349.
Yates P, Edwards H, Nash R, Aranda S,
Purdie D, Najman J, Skerman H &
Walsh A (2004) A randomized con-
trolled trial of a nurse-administered
educational intervention for improving
cancer pain management in ambulatory
settings. Patient Education and Coun-
seling 53, 227237.
Zeger SL & Liang KY (1992) An overview
of methods for the analysis of longitu-
dinal data. Statistics in Medicine 11,
18251830.
The Journal of Clinical Nursing (JCN) is an international, peer reviewed journal that aims to promote a high standard of
clinically related scholarship which supports the practice and discipline of nursing.
For further information and full author guidelines, please visit JCN on the Wiley Online Library website: http://
wileyonlinelibrary.com/journal/jocn
Reasons to submit your paper to JCN:
High-impact forum: one of the worlds most cited nursing journals and with an impact factor of 1194 ranked 16 of 70
within Thomson Reuters Journal Citation Report (Social Science Nursing) in 2009.
One of the most read nursing journals in the world: over 1 million articles downloaded online per year and accessible in over
7000 libraries worldwide (including over 4000 in developing countries with free or low cost access).
Fast and easy online submission: online submission at http://mc.manuscriptcentral.com/jcnur.
Early View: rapid online publication (with doi for referencing) for accepted articles in nal form, and fully citable.
Positive publishing experience: rapid double-blind peer review with constructive feedback.
Online Open: the option to make your article freely and openly accessible to non-subscribers upon publication in Wiley
Online Library, as well as the option to deposit the article in your preferred archive.
Pain management Pain education to improve pain management
2011 Blackwell Publishing Ltd, Journal of Clinical Nursing, 20, 18581869 1869
This document is a scanned copy of a printed document. No warranty is given about the accuracy of the copy.
Users should refer to the original published version of the material.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Effects of Market Orientation On Business Performance - Vodafone Ghana PDFDocument102 pagesThe Effects of Market Orientation On Business Performance - Vodafone Ghana PDFhortalemos100% (1)
- Recommendation From Jamie NordhagenDocument1 pageRecommendation From Jamie Nordhagenapi-244230664No ratings yet
- PPPPC Meeting Minutes 071614Document5 pagesPPPPC Meeting Minutes 071614api-244230664No ratings yet
- Recommendation From Renee AbdellaDocument2 pagesRecommendation From Renee Abdellaapi-244230664No ratings yet
- Signed Final Evaluation 2014Document3 pagesSigned Final Evaluation 2014api-244230664No ratings yet
- Thank You Patient 1Document2 pagesThank You Patient 1api-244230664No ratings yet
- Ce Record 2014 Aurora Davis v2Document1 pageCe Record 2014 Aurora Davis v2api-244230664No ratings yet
- Kudos Email 10 11 13Document1 pageKudos Email 10 11 13api-244230664No ratings yet
- Kudos Email 8 25 13Document2 pagesKudos Email 8 25 13api-244230664No ratings yet
- Thank You New Grad 1Document2 pagesThank You New Grad 1api-244230664No ratings yet
- Focuspdca 7 26 14Document2 pagesFocuspdca 7 26 14api-244230664No ratings yet
- Advisor Checklist CompletedDocument7 pagesAdvisor Checklist Completedapi-244230664No ratings yet
- Kudos Email 8 2 14Document1 pageKudos Email 8 2 14api-244230664No ratings yet
- Kudos Email 3 29 14Document1 pageKudos Email 3 29 14api-244230664No ratings yet
- Preceptor Council AttendanceDocument2 pagesPreceptor Council Attendanceapi-244230664No ratings yet
- Lo6 FeedbackDocument2 pagesLo6 Feedbackapi-244230664No ratings yet
- Preceptor Council AttendanceDocument2 pagesPreceptor Council Attendanceapi-244230664No ratings yet
- Hcahps BMT Data BeforeDocument1 pageHcahps BMT Data Beforeapi-244230664No ratings yet
- Kudos Email 1 13 14Document1 pageKudos Email 1 13 14api-244230664No ratings yet
- Pain Severity Satisfaction With Pain ManagementDocument10 pagesPain Severity Satisfaction With Pain Managementapi-244230664No ratings yet
- January Staff Meeting MinutesDocument3 pagesJanuary Staff Meeting Minutesapi-244230664No ratings yet
- PSC Meeting Agenda 4 2014Document1 pagePSC Meeting Agenda 4 2014api-244230664No ratings yet
- Hcahps Omg Data BeforeDocument1 pageHcahps Omg Data Beforeapi-244230664No ratings yet
- Pain Minutes 031914Document2 pagesPain Minutes 031914api-244230664No ratings yet
- Presentation of Pain Patient Education ToolDocument10 pagesPresentation of Pain Patient Education Toolapi-244230664No ratings yet
- Do Patients Beliefs Act As BarriersDocument13 pagesDo Patients Beliefs Act As Barriersapi-244230664No ratings yet
- Cancer Pain Part 2Document7 pagesCancer Pain Part 2api-244230664No ratings yet
- Cancer Patients Barriers To Pain ManagementDocument12 pagesCancer Patients Barriers To Pain Managementapi-244230664No ratings yet
- Email From Mandy 7 14 14Document1 pageEmail From Mandy 7 14 14api-244230664No ratings yet
- Daisy Nomination Bill ValentineDocument2 pagesDaisy Nomination Bill Valentineapi-244230664No ratings yet
- 1 +Endah+SetyowatiDocument11 pages1 +Endah+Setyowatiebdscholarship2023No ratings yet
- Project Management Framework Through Critical Success Factors For Delivering Power Transmission Construction ProjectDocument24 pagesProject Management Framework Through Critical Success Factors For Delivering Power Transmission Construction ProjectAchintya GhatakNo ratings yet
- SmartPLS UtilitiesDocument11 pagesSmartPLS UtilitiesplsmanNo ratings yet
- Analysis of The Influence of Company Size On The Timeliness of Financial Reporting by Mediating Profitability and Leverage in Companies Listed On The Indonesian Stock ExchangeDocument7 pagesAnalysis of The Influence of Company Size On The Timeliness of Financial Reporting by Mediating Profitability and Leverage in Companies Listed On The Indonesian Stock ExchangeInternational Journal of Business Marketing and ManagementNo ratings yet
- Process Anleitung Alle ModelleDocument90 pagesProcess Anleitung Alle Modellenarjirolu gcpNo ratings yet
- The Saving Behavior of Public Vocational High School Students of Business and Management Program in Semarang SitiDocument8 pagesThe Saving Behavior of Public Vocational High School Students of Business and Management Program in Semarang SitiDaniel Lee Eisenberg JacobsNo ratings yet
- 38 30 PBDocument8 pages38 30 PBMahusay Neil DominicNo ratings yet
- Edi Sugiono, Dewi SV. (2019) - Work Stress, Work Discipline and Turnover Intention On Performance Mediated by Job SatisfactionDocument6 pagesEdi Sugiono, Dewi SV. (2019) - Work Stress, Work Discipline and Turnover Intention On Performance Mediated by Job SatisfactionSiapa KamuNo ratings yet
- Morgades Bamba2019 PDFDocument7 pagesMorgades Bamba2019 PDFArif IrpanNo ratings yet
- Conclusion PDFDocument5 pagesConclusion PDFSamatorEdu TeamNo ratings yet
- Effects of Birth Ball Exercise On Pain and Self-Efficacy During Childbirth: A Randomised Controlled Trial in TaiwanDocument18 pagesEffects of Birth Ball Exercise On Pain and Self-Efficacy During Childbirth: A Randomised Controlled Trial in TaiwanRana Yuda StiraNo ratings yet
- Abdullah & Hwei - Acceptance Forgiveness and Gratitude (Jurnal)Document23 pagesAbdullah & Hwei - Acceptance Forgiveness and Gratitude (Jurnal)Siti Rahmah Budi AswadiNo ratings yet
- The Mediation Role of Organization Citizenship Behaviour Between Employee Motivation and Productivity: Analysis of Pharmaceutical Industries in KRGDocument13 pagesThe Mediation Role of Organization Citizenship Behaviour Between Employee Motivation and Productivity: Analysis of Pharmaceutical Industries in KRGMonika GuptaNo ratings yet
- SPSS and SAS Procedures For Estimating Indirect Effects in Simple Mediation ModelsDocument26 pagesSPSS and SAS Procedures For Estimating Indirect Effects in Simple Mediation ModelsUff NadirNo ratings yet
- Data Analysis TechniquesDocument16 pagesData Analysis TechniquesAltaf KhanNo ratings yet
- Determinant Analysis of Employee Performance and Organizational Commitment As An Intervening Variable in Building A Clean Serving Bureaucracy AreaDocument12 pagesDeterminant Analysis of Employee Performance and Organizational Commitment As An Intervening Variable in Building A Clean Serving Bureaucracy AreaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Role of Management and Trade Union Leadership On Dual Commitment: The Mediating Effect of The Workplace Relations ClimateDocument18 pagesThe Role of Management and Trade Union Leadership On Dual Commitment: The Mediating Effect of The Workplace Relations ClimateSK KHURANSAINo ratings yet
- Testing Mediation Using Medsem' Package in StataDocument17 pagesTesting Mediation Using Medsem' Package in StataAftab Tabasam0% (1)
- Measuring The Critical Effect of Marketing Mix On Customer Loyalty Through Customer Satisfaction in Food and Beverage Products PDFDocument12 pagesMeasuring The Critical Effect of Marketing Mix On Customer Loyalty Through Customer Satisfaction in Food and Beverage Products PDFINTESSO N.V.No ratings yet
- Irawan Et Al (2019) (Perilaku Organisasi)Document16 pagesIrawan Et Al (2019) (Perilaku Organisasi)Dinda PotabugaNo ratings yet
- Statistical Mediation Analysis Using Sobel Test and Process MacroDocument20 pagesStatistical Mediation Analysis Using Sobel Test and Process MacroxxproangelxxNo ratings yet
- The Mediation Role of Change Management in Employee DevelopmentDocument14 pagesThe Mediation Role of Change Management in Employee DevelopmentIJELS Research JournalNo ratings yet
- 4 - The Influence of Social Media Promotion Strategies On Price Mediated Purchase Decisions (Case Study at PT. Lazada Bandung)Document8 pages4 - The Influence of Social Media Promotion Strategies On Price Mediated Purchase Decisions (Case Study at PT. Lazada Bandung)Haren Servis PrinterNo ratings yet
- Jurnal InternasionalDocument9 pagesJurnal InternasionalDwi Nur Cahyani AgustinNo ratings yet
- The Effect of Product Quality and Service Quality On Customer Loyalty Mediated by Customer Satisfaction (Evidence On Kharisma Store in Belu District, East Nusa Tenggara Province)Document14 pagesThe Effect of Product Quality and Service Quality On Customer Loyalty Mediated by Customer Satisfaction (Evidence On Kharisma Store in Belu District, East Nusa Tenggara Province)yuskaraNo ratings yet
- EN The Impact of Marketing Mix Towards Cust PDFDocument9 pagesEN The Impact of Marketing Mix Towards Cust PDFZe ArtNo ratings yet
- Enfermeras Taiwan Con Litwin y StringerDocument10 pagesEnfermeras Taiwan Con Litwin y StringerSebastián Andres Peña RojoNo ratings yet
- Mediation Analysis of Organizational Justice and Job SatisfactionDocument33 pagesMediation Analysis of Organizational Justice and Job SatisfactionAsif Khan NiaziNo ratings yet
- The Cross-Level Mediating Effect of PsychologicalDocument16 pagesThe Cross-Level Mediating Effect of PsychologicalFabián Henríquez CarocaNo ratings yet