Professional Documents
Culture Documents
Immunology and Serology
Uploaded by
Justin Jofer Tan100%(1)100% found this document useful (1 vote)
776 views8 pagesMT
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentMT
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
776 views8 pagesImmunology and Serology
Uploaded by
Justin Jofer TanMT
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 8
IMMUNOLOGY AND SEROLOGY
Immunology and serology laboratories focus on
1. identifying antibodies (proteins made by a type of white blood cell in response to an
antigen -- a foreign protein -- in the body).
2. investigating problems with the immune system such as autoimmune diseases (when the
body's immune system turns on its own tissues) and immunodeficiency disorders (when a
body's immune system is underactive).
3. determining organ compatibility for transplantation.
Immunology-study of the bodys ability to resist infection & all of the phenomena
connected with the defense mechanisms of the body.
History of Immunology
Edward Jenner-demonstrated that protection from smallpox could be generated by the
transfer of postural material from cowpox lesions on the nipples of the cows.
Louis Pasteur- demonstrated that injection of killed microbes provided protection upon
subsequent exposure to the live counterpart.
Ely Metchnikoff-demonstrated that certain blood cells could ingest foreign materials
(phagocytes)
Jules Bordet-discovered complement
Robert Kaus- discovered precipitins
Emil Alolf von Behring-worked on Serum Therapy
Antigen (Ag)
a substance that elicits an immune response when introduced to the tissues of an
animal
stimulate Abs formation
characterized by a complex molecule, soluble in body fluids and foreign
Antibody (Ab)
a protein associated with a gamma globulin fraction of blood serum, substance
formed in response to antigenic stimulus
The synthesis, or manufacture, of antibodies is initiated when a foreign substance,
referred to as an antigen, enters the body.
Lymphocytes respond to the foreign substance by making an antibody with a molecular
arrangement that fits the shape of molecules on the surface of the substance so that the antibody
combines with it.
Common antigens are the protein components of bacteria and viruses. These antigens
may enter the body during infection or may be deliberately introduced by vaccination in order to
stimulate the production of antibodies.
The binding of antibodies to the surfaces of bacteria, viruses, or toxins can neutralize and
eliminate these harmful substances in any or all of three ways:
(1) By directly inactivating them,
(2) By enabling other blood cells to engulf and destroy them (Phagocytosis), and/or
(3) By weakening their surfaces and rendering those vulnerable to destruction by other
blood proteins (collectively called complement).
Immunoglobulin (Ig)
Basic structure:
2 Light chains (214 amino acids; 25,000 MW)
2 antigenic markers --- kappa & lambda
2 Heavy chains (440 amino acids; 50,000 70,000 MW)
becomes Y shape after binding to Ag
Y shape rich in proline and attack by proteolytic enzymes
Fc-fragment lack the ability to bind to Ag
MECHANISM of NONSPECIFIC HOST DEFENSE
A. SKIN
few m.o. capable of penetrating intact skin
may enter sweat or sebaceous glands, hair follicles
sweat & sebaceous secretions --- antimicrobial properties
tend to eliminate pathogenic organisms
lysozyme
an enzyme, dissolves some bacterial cell wall on tears, respiratory & cervical
secretions
Skin resistance may vary with age
B. MUCOUS MEMBRANES
Respiratory tract film of mucus covers the surface driven upward by ciliated cells mucus
& tears contain lysozyme
MECHANISM of NONSPECIFIC IMMUNOLOGIC MECHANISM
A. PHAGOCYTOSIS (monocytes, neutrophils, macrophages)
B. RETICULOENDOTHELIAL SYSTEM (RES)
C. INFLAMMATORY RESPONSE
D. FEVER
Substances capable of inducing fever
1. Endotoxins (Gram negative bacteria)
2. Cytokines (released from lymphoid cells)
HYPERSENSITIVITY REACTIONS
Allergy- a condition in which an immune response results in an exaggerated or
inappropriate reactions that are harmful to the host.
MAIN TYPES of HYPERSENSITIVITY REACTIONS:
Type I: Immediate (Anaphylactic) Hypersen. Rxn.
Type II: Cytotoxic Hypersensitivity rxn.
Type III: Immune Complex Hypersensitivity rxn.
Type IV: Cell mediated (delayed) HP
Immunity- condition under which an individual is protected from the disease
Two general types of immunity
Innate Immunity
Acquired Immunity
Types of Acquired Immunity
1. ACTIVE IMMUNITY
a. Naturally Acquired Active Immunity
-develops from exposure to an infectious agent
b. Artificially Acquired Active Immunity
-occurs through vaccination
2. PASSIVE IMMUNITY
a. Naturally Acquired Passive Immunity
b. Artificially Acquired Passive Immunity
Vaccine - typically contains an agent that resembles a disease-causing microorganism, and is
often made from weakened or killed forms of the microbe or its toxins
Types of Vaccines
1. Live, attenuated vaccines-contain weakened microbes that multiply at only low levels,
inducing a strong immune response
2. Inactivated vaccines-contain killed pathogens, which induce a weaker immune response
3. Toxoid vaccines- contain inactivated toxins (toxoids)
4. Subunit vaccines- contain only those parts of the antigens that stimulate a strong
immune response
5. Conjugate vaccines-are created by attaching bacterial capsule polysaccharides to a
toxoid
6. DNA vaccines-depend on the ability of some cells to take up and translate foreign DNA
and to display the resulting proteins, inducing a strong immune response
7. Recombinant vector vaccines-involve DNA incorporated into an attenuated pathogen
Passive Immunity- develops when antibodies enter the body from outside source
Types:
1. Naturally acquired passive immunity (congenital immunity)- occurs when antibodies
pass from mother to fetus
2. Artificially acquired passive immunity- involves injection of antibody-rich serum into
a body
Serology-is the study of blood serum (the clear fluid that separates when blood clots)
Beginning of Serology:
Serology as a science began in 1901. Austrian American immunologist Karl
Landsteiner (1868-1943) identified groups of red blood cells as A, B, and O. From that
discovery came the recognition that cells of all types, including blood cells, cells of the body,
and microorganisms carry proteins and other molecules on their surface that are recognized by
cells of the immune system.
Karl Landsteiner -An Austrian physician by training, Landsteiner played an integral part in the
identification of blood groups. He demonstrated the catastrophic effect of transfusing with the
wrong type of blood
Purpose:
Diagnose of certain disease
Checking blood typing
Terms used in evaluating test methodology:
1. Sensitivity
Analytical Sensitivity ability of a test to detect very small amounts of a substance
Clinical Sensitivity ability of test to give positive result if patient has the disease (no
false negative results)
2. Specificity
Analytical Specificity ability of test to detect substance without interference from cross-
reacting substances
Clinical Specificity ability of test to give negative result if patient does not have disease
(no false positive results)
3. Affinity
-strength of binding between a single antigenic determinant and an individual antibody
combining site.
4. Avidity
- a measure of the overall strength of binding of an antigen with many antigenic
determinants and multivalent antibodies
5. Dilution
- Estimating the antibody by determining the greatest degree to which the serum may be
diluted without losing the power to given an observable effect in a mixture with specific
antigen
6. Titer
- Different dilutions of serum are tested in mixture with a constant amount of antigen and
greatest reacting dilution is taken as the measure or Titer
7. Seroconversion
- the development of detectable specific antibodies to microorganisms in the blood serum
as a result of infection or immunization.
8. Seroreversion
- when the tests can no longer detect antibodies or antigens in a patients serum
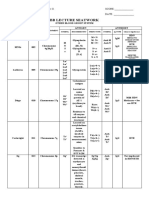
Immunology and Serology Tests
1. Precipitation
Principle
-Soluble antigen + antibody (in proper proportions) > visible precipitate
-Lattice formation (antigen binds with Fab sites of 2 antibodies)
Examples
-Double diffusion (Ouchterlony)
-Single diffusion (radial immunodiffusion)
-Imunoelectrphoresis
-Immunofixation
2. Agglutination
Principle
-Particulate antigen + antibody > clumping
-Lattice formation (antigen binds with Fab sites of 2 antibodies forming bridges between
antigens)
Examples
-Direct agglutination (Blood Bank)
-Passive Hemagglutination (treat RBC's with tannic acid to allow adsorption of protein
antigens)
-Passive latex agglutination (antigen attached to latex particle)
3. Neutralization reactions
-Similar in principle and interpretation of results
-Antibody-binding
-Hemagglutination inhibition
-Neutralization (antibody neutralizes toxin)
-After binding, antibody is not available to react in indicator system
Results:
-NO agglutination or NO hemolysis = positive reaction
-Agglutination or hemolysis = negative reaction (antibody not bound in origin
4. Compliment Fixation
-Antibody and antigen allowed to combine in presence of complement
-If complement is fixed by specific antigen-antibody reaction, it will be unable to
combine with indicator system
Precautions:
-Serum must be heat-activated
-Stored serum becomes anti-complementary
-Extensive QC/standardization required
-Only use for IgM antibodies
5. Imunoelectrphoresis (IEP) Qualitative
-A serum sample is electrophoresed through an agar medium.
-A trough is cut in the agar and filled with Ab.
-A precipitin arc is then formed because Ag diffuses radially and Ab from a trough
diffuses, the reactants meet in optimal proportions for precipitation.
6. Enzyme immunoassay( EIA/ELISA)
-Sandwich technique
-Monoclonal or polyclonal antibody adsorbed on solid surface (bead or microtiter plate)
-Add patient serum; if antigen is present in serum, it binds to antibody coated bead or
plate
-Add excess labelled antibody (antibody conjugate); forms antigen-antibody-labelled
antibody sandwich (antibody in conjugate is directed against another epitope of antigen
being tested)
-Add substrate, incubate, and read absorbance
-Washing required between each step
-Absorbance is directly proportional to antigen concentration
7. ELISA
-Enzyme-linked immunosorbent assay, also called ELISA, enzyme immunoassay or EIA,
is a biochemical technique used mainly in immunology to detect the presence of an
antibody or an antigen in a sample. The ELISA has been used as a diagnostic tool in
medicine
-Because the ELISA can be performed to evaluate either the presence of antigen or the
presence of antibody in a sample
8. Nephelometry
Procedure
-Serum substance reacts with specific antisera and forms insoluble complexes
-Light is passed through suspension
-Scattered (reflected) light is proportional to number of insoluble complexes; compare to
standards
Examples
-Complement component concentration
-Antibody concentration (IgG, IgM, IgA, etc.)
-Immunofluorescence
9. Immunofluorescence
-Direct add fluorescein-labeled antibody to patient tissue, wash, and examine under
fluorescent microscope
-Indirect add patient serum to tissue containing known antigen, wash, add labeled
antiglobulin, wash, and examine under fluorescent microscope
Examples
-Testing for Antinuclear Antibodies (ANA)
-Fluorescent Treponemal Antibody Test (FTA-Abs)
10. Fluorescence polarization immunoassay (FPIA)
Principle
-Add reagent antibody and fluorescent-tagged antigen to patient serum
Positive test
-Antigen present in patient serum binds to reagent leaving most tagged antigen unbound
-Unbound labeled antigens rotate quickly reducing amount of polarized light produced
Negative test
-If no antigen present in patient serum, tagged antigen binds to reagent antibody
-Tagged antigen-antibody complexes rotate slowly giving off increased polarized light
11. Flow Cytometry
-Method of choice for T- and B-cell analysis (lymphocyte phenotyping)
Principle
-Incubate specimen with 1 or 2 monoclonal antibodies tagged with fluorochrome
-Single cells pass through incident light of instrument (laser) which excites fluorochrome
and results in emitted light of different wavelength
-Intensity of fluorescence measured to detect cells possessing surface markers for the
specific monoclonal antibodies that were employed
-Forward light scatter indicates cell size or volume
90 side-scattered light indicates granula
-Common Uses: DNA analysis, Reticulocyte counts, Leukemia/lymphoma classification,
CD 4 cell estimations in AIDS/ HIV patients
12. Rheumatoid factor
- To classify arthritis and diagnose rheumatoid arthritis
13. VDRL A standard test for Syphilis
-NONTREPONEMAL ANTIGEN TESTS.
-Nontreponemal antigen tests are used as screeners. They measure the presence of reagin,
which is an antibody formed in reaction to syphilis. In the venereal disease research
laboratory (VDRL) test, a sample of the patient's blood is mixed with cardiolipin and
cholesterol. If the mixture forms clumps or masses of matter, the test is considered
reactive or positive. The serum sample can be diluted several times to determine the
concentration of reagin in the patient's blood.
14. HLA Typing (Human leukocyte antigens)
- To determine compatibility in organ transplantation, to determine paternity and to
diagnose HLA-related disorders
Sources:
http://www.umm.edu/pathology-info/immuno.htm
http://www.biology.arizona.edu/immunology/tutorials/immunology/main.html
http://www.nfstc.org/pdi/Subject02/images/pdi_s02_m02_01_b.2.swf
http://www.umm.edu/pathology-info/immuno.htm
http://en.wikipedia.org/wiki/Vaccine
http://www.suite101.com/content/history-of-immunology-a34638\
http://trevor.butler.edu/~jshellha/323/History.html
http://en.wikipedia.org/wiki/Timeline_of_immunology
http://www.authorstream.com/Presentation/aSGuest49551-417885-immunology-science-
technology-ppt-powerpoint/
http://www.authorstream.com/Presentation/doctorrao-238007-serology-diagnosis-infectious-
diseases-science-technology-ppt-powerpoint/
Serology-ppt by Dr. T. V. Rao M.D.
You might also like
- SEC Cover SheetDocument1 pageSEC Cover Sheetlito7769% (35)
- Clinical Chemistry Notes - AbiDocument34 pagesClinical Chemistry Notes - AbiAnya Ignacio100% (1)
- Reviewer - Immunoserology - Part 1Document12 pagesReviewer - Immunoserology - Part 1Joshua Trinidad0% (1)
- Introduction to ImmunohematologyDocument16 pagesIntroduction to ImmunohematologyJoshua TrinidadNo ratings yet
- Urinalysis and Body Fluids Q & ADocument79 pagesUrinalysis and Body Fluids Q & ADarla YsavelNo ratings yet
- Anion Gap CalculationDocument13 pagesAnion Gap CalculationDams ZainalNo ratings yet
- Histologic TechniquesDocument12 pagesHistologic TechniquesCatherine MerillenoNo ratings yet
- Immunohematology Trans by KTRC (Wala Ito Sa Book)Document21 pagesImmunohematology Trans by KTRC (Wala Ito Sa Book)Angelo ErispeNo ratings yet
- MUST To KNOW in Clinical ChemistryDocument53 pagesMUST To KNOW in Clinical ChemistryMonkey LuffyNo ratings yet
- Immunology & Serology Review Notes George Vincent Gellena, RMT, Mls (Ascpi)Document9 pagesImmunology & Serology Review Notes George Vincent Gellena, RMT, Mls (Ascpi)Angelo Jude CobachaNo ratings yet
- Clinical Chemistry Notes Without Blanks LegitDocument43 pagesClinical Chemistry Notes Without Blanks LegitPearl Isabelle SudarioNo ratings yet
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Cupressus: Structure, Reproduction and Life CycleDocument35 pagesCupressus: Structure, Reproduction and Life CycleHaripriya m100% (3)
- IMS - Intro To Immunology and SerologyDocument3 pagesIMS - Intro To Immunology and SerologyJeanne RodiñoNo ratings yet
- SerologyDocument442 pagesSerologyPura Javier100% (2)
- SerologyDocument84 pagesSerologyngsusannasuisum100% (2)
- Histopathology: Ann Fatima G. Quindao, RMT, LPT, MPHDocument108 pagesHistopathology: Ann Fatima G. Quindao, RMT, LPT, MPHMarry Grace CiaNo ratings yet
- Clinical Microscopy ExamDocument3 pagesClinical Microscopy ExamKarla GiorlaNo ratings yet
- Histopath ReviewerDocument43 pagesHistopath ReviewerMika De VeraNo ratings yet
- Clinical Chemistry NotesDocument24 pagesClinical Chemistry Notesclower112100% (3)
- Ereviewer. Mtlaws. Prelims and Midterms PDFDocument8 pagesEreviewer. Mtlaws. Prelims and Midterms PDFCatlyn RivalNo ratings yet
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- Antibody IdentificationDocument74 pagesAntibody IdentificationNilver Zenteno100% (3)
- ISBB Immunology ReviewDocument9 pagesISBB Immunology ReviewNathan DrakeNo ratings yet
- HistopathDocument23 pagesHistopathElla SalesNo ratings yet
- Hematology EssentialsDocument4 pagesHematology EssentialsAlfred ChowNo ratings yet
- Enterobius Vermicularis: Ciulla Chapter 8 - ParasitologyDocument13 pagesEnterobius Vermicularis: Ciulla Chapter 8 - ParasitologySalve Rachelle BillenaNo ratings yet
- Platelet CountDocument2 pagesPlatelet CountSirias_black100% (2)
- BB NotesDocument5 pagesBB NotesFait HeeNo ratings yet
- MUST To KNOW in Immunology and SerologyDocument18 pagesMUST To KNOW in Immunology and SerologyRona Salando50% (2)
- Blood Banking Course BookDocument2 pagesBlood Banking Course BookShukr Wesman BlbasNo ratings yet
- CM Handouts Clinical MicrosDocument33 pagesCM Handouts Clinical Microsrenato renato100% (1)
- Reviewer - Immmunohematology - Part 2Document29 pagesReviewer - Immmunohematology - Part 2Joshua TrinidadNo ratings yet
- Hematology2 - Laboratory TestsDocument3 pagesHematology2 - Laboratory Testskthmnts100% (1)
- Histopath Guide QuestionsDocument2 pagesHistopath Guide QuestionsMartin ClydeNo ratings yet
- Intro To Medtech Clinical Chemistry ReviewerDocument11 pagesIntro To Medtech Clinical Chemistry Reviewerjesanndei100% (1)
- Beginings of MTDocument65 pagesBeginings of MTMel JamitoNo ratings yet
- Chapter 1: An Overview of Clinical LaboratoryDocument13 pagesChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Clinical Chemistry 2Document22 pagesClinical Chemistry 2Rubenne Miles ElagasNo ratings yet
- Mtap - Immunohema Transfusion MedicineDocument9 pagesMtap - Immunohema Transfusion MedicineMoira Pauline LibroraniaNo ratings yet
- Other Blood Group System AssignmentDocument5 pagesOther Blood Group System AssignmentMary ChristelleNo ratings yet
- Immuno SeroDocument80 pagesImmuno SeroDocAxi Maximo Jr AxibalNo ratings yet
- Immunology & Serology: Preliminaries: Romie Solacito, MLS3CDocument12 pagesImmunology & Serology: Preliminaries: Romie Solacito, MLS3CRomie Solacito100% (2)
- Ciulla - MycoDocument13 pagesCiulla - MycoSalve Rachelle BillenaNo ratings yet
- Medical Laboratory Science Review Harr Robert R.Document28 pagesMedical Laboratory Science Review Harr Robert R.Arriel A. Aranggo50% (2)
- Histopathologic and Cytologic Techniques Lecture: General Pathology: An IntroductionDocument11 pagesHistopathologic and Cytologic Techniques Lecture: General Pathology: An IntroductionTheresa BergonioNo ratings yet
- MT Books (Acts)Document2 pagesMT Books (Acts)Kenji Hipol Akinaga100% (1)
- CSF Analysis Provides Insights into Neurological ConditionsDocument8 pagesCSF Analysis Provides Insights into Neurological ConditionsMoira Pauline LibroraniaNo ratings yet
- Clinical ChemistryDocument8 pagesClinical Chemistryleizej29No ratings yet
- MT Laws Reviewer MidtermsDocument6 pagesMT Laws Reviewer MidtermsKyaru Fuentes100% (1)
- Immunohematology Handouts UpdatedDocument15 pagesImmunohematology Handouts UpdateddmclmllNo ratings yet
- Group 6 - Immunohematology - Blood BankingDocument8 pagesGroup 6 - Immunohematology - Blood Bankingjulo_05No ratings yet
- BIEN 500 Systems Physiology for Biomedical Engineers: Hemostasis and Blood CoagulationDocument16 pagesBIEN 500 Systems Physiology for Biomedical Engineers: Hemostasis and Blood CoagulationRezaTiansahNo ratings yet
- NotesCM (CEFI)Document30 pagesNotesCM (CEFI)Ces MangaNo ratings yet
- Medical TechnologyDocument13 pagesMedical Technologyangelina buenaNo ratings yet
- CIULLA CHAPTER 9 - KEY VIRUSESDocument9 pagesCIULLA CHAPTER 9 - KEY VIRUSESSalve Rachelle Billena100% (1)
- Clinical Chemistry KeyNotes For Board ExaminationDocument12 pagesClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (1)
- CLINICAL CHEMISTRY GUIDEDocument10 pagesCLINICAL CHEMISTRY GUIDEDeniel BusiNo ratings yet
- Hematology Guide for Anemia and Iron MetabolismDocument46 pagesHematology Guide for Anemia and Iron MetabolismGiannis GkouzionisNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Basic Taxation Aban ReviewerDocument50 pagesBasic Taxation Aban ReviewerJustin Jofer TanNo ratings yet
- AAA Succession PDFDocument157 pagesAAA Succession PDFBoy Omar Garangan DatudaculaNo ratings yet
- Spring Harvest Agri Trading IncDocument1 pageSpring Harvest Agri Trading IncJustin Jofer TanNo ratings yet
- Demand FVT Corp. 54 TrinidadDocument1 pageDemand FVT Corp. 54 TrinidadJustin Jofer TanNo ratings yet
- Rule 112Document2 pagesRule 112Justin Jofer TanNo ratings yet
- FinalDocument2 pagesFinalJessica FordNo ratings yet
- Forms and Elements of A ContractDocument1 pageForms and Elements of A ContractJustin Jofer TanNo ratings yet
- Risk For InjuryDocument2 pagesRisk For InjuryJustin Jofer TanNo ratings yet
- Respiratory Assessment, Intervention and EvaluationDocument1 pageRespiratory Assessment, Intervention and EvaluationJustin Jofer TanNo ratings yet
- Tan 1Document3 pagesTan 1Justin Jofer TanNo ratings yet
- PhenobarbitalDocument2 pagesPhenobarbitalJustin Jofer TanNo ratings yet
- Risk For InjuryDocument2 pagesRisk For InjuryJustin Jofer TanNo ratings yet
- AUTOPSYDocument57 pagesAUTOPSYsafina khstoonNo ratings yet
- Books for Physiology, Anatomy, Kinesiology and Physical Therapy - KuyangPT on TwitterDocument1 pageBooks for Physiology, Anatomy, Kinesiology and Physical Therapy - KuyangPT on TwitterDATHAN NEVIN LEUNGNo ratings yet
- PERINÉ PPT - PPSXDocument10 pagesPERINÉ PPT - PPSXCuscatleca Extra suaveNo ratings yet
- Koss2012, Citologia Del Tracto Urinario-Convertido Traducido Version 2.5Document142 pagesKoss2012, Citologia Del Tracto Urinario-Convertido Traducido Version 2.5Jaime Enrique Betanzos TeobalNo ratings yet
- Ten Pussy Eating CommandmentsDocument13 pagesTen Pussy Eating CommandmentsSophie Jenkin100% (2)
- C. RicciaDocument43 pagesC. RicciaCalvin Yudha L100% (1)
- Respiratory System HandoutDocument15 pagesRespiratory System HandoutJei SanNo ratings yet
- Disturbances in Perception and CoordinationDocument240 pagesDisturbances in Perception and CoordinationJeaneline Pagasian Enon50% (2)
- AMYLOIDOSISDocument16 pagesAMYLOIDOSISSourav NathNo ratings yet
- K32E Alle N WWDocument180 pagesK32E Alle N WWKirilKocevskiNo ratings yet
- S53 - FPSC NFC Location D-819, Part A, C V Raman Marg, Near Fortis Escort Hospital, New Friends Colon New DelhiDocument8 pagesS53 - FPSC NFC Location D-819, Part A, C V Raman Marg, Near Fortis Escort Hospital, New Friends Colon New DelhiSohaib DurraniNo ratings yet
- Medical Neurobiology - Peggy Mason, PHDDocument4 pagesMedical Neurobiology - Peggy Mason, PHDARIJENIWA ADEMULEGUN VICTORNo ratings yet
- Medical Terminology CH 9Document104 pagesMedical Terminology CH 9ياسين المسطو100% (1)
- EmgDocument6 pagesEmgDhabia AhmedNo ratings yet
- Respiratory Assessment LandmarksDocument15 pagesRespiratory Assessment LandmarksChilled Moo MooNo ratings yet
- IHM Manual VTCTDocument57 pagesIHM Manual VTCTEnvie AestheticsNo ratings yet
- Chapter 8 - Transport in PlantsDocument3 pagesChapter 8 - Transport in PlantsLeann LeeNo ratings yet
- Human Nervous System Anatomy and PhysiologyDocument20 pagesHuman Nervous System Anatomy and PhysiologyIvy Jan OcateNo ratings yet
- AUBF Lec Renal Function I PDFDocument4 pagesAUBF Lec Renal Function I PDFBanana QNo ratings yet
- 1st Prof MBBS Supplementary 10 Years CompilationDocument67 pages1st Prof MBBS Supplementary 10 Years CompilationDebasis PramanikNo ratings yet
- Antenatal Power PointDocument135 pagesAntenatal Power PointBULARON, Gerry Mar ANo ratings yet
- Hirschsprung PathophysiologyDocument4 pagesHirschsprung PathophysiologyJona SuarezNo ratings yet
- Reproductive SystemDocument7 pagesReproductive SystemRiaz siddiquiNo ratings yet
- Pathology Notes HemalathaDocument117 pagesPathology Notes HemalathapriyagerardNo ratings yet
- EXAM1 Study Guide Biol 211 PalomarDocument21 pagesEXAM1 Study Guide Biol 211 PalomarKathleen RussellNo ratings yet
- Immuno OncologyDocument4 pagesImmuno OncologydanieleNo ratings yet
- Hemodynamic Disorders ExplainedDocument114 pagesHemodynamic Disorders ExplainedlydNo ratings yet
- Diferenciacion de Hematogonias y LinfoblastosDocument6 pagesDiferenciacion de Hematogonias y LinfoblastosSusan RamosNo ratings yet
- Benign Prostatic Hyperplasia: A Case Analysis OnDocument70 pagesBenign Prostatic Hyperplasia: A Case Analysis OnAngelica RelanaNo ratings yet