Professional Documents
Culture Documents
02: Cell Responses To Injury
Uploaded by
NYUCD170 ratings0% found this document useful (0 votes)
349 views15 pages6/30/14
Original Title
02: Cell Responses to Injury
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document6/30/14
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
349 views15 pages02: Cell Responses To Injury
Uploaded by
NYUCD176/30/14
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 15
Transcribed by Sofiya Khazanovich June 30, 2014
General Pathology Lecture 2 Cell Responses to Injury by Dr. Kinnally
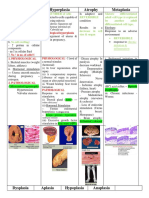
Slide 1 Cellular response to injury
Kinnally - So, hi guys. You can hear me in the back right? I cant believe the summers over and its not
even the 4
th
of July, right? Dont worry, you get time in August, right? You get time in August. Ok, so,
cellular response to injury, now I must tell you that, let me see if this is going to work
Slide 2 Objectives
Kinnally You guys know who I am, you know what the asterisks mean. And you know what the
objectives mean, so you might want to just take a look at them when you start to read or study for this
course. So again, heres the name of the textbook that were going to be using and a lot of this is in the
textbook, except the stuff thats on apoptosis and necrosis, because thats a rapidly changing field, so I
figured Id kind of get you more up to date than our textbook.
Slide 3 Pathology
Kinnally Im going to skip this because in fact Dr. Phelan just did this.
Slide 4 Image
Kinnally So Ill start here. This is sort of the summary of the lecture that Im going to give. Were going
to talk about the normal cell and its ability to adapt to stresses, and these are the different things that it
can do to adapt to stress. Or if its injured then it will have some sort of a reversible effect and if that
reversible injury doesnt go away, or the cell is not able to adapt to that injury, then the cell will die, and
thats not reversible. And theres three ways to die, even though I only put two up here. Whats missing?
Autophagy. I know, its been 6-8 months, and its not so easy. What were going to do is were going to
start out talking about reversible injury and adaptation and then move into irreversible injury, necrosis,
apoptosis, and then autophagy.
Slide 5 Why are cell responses, particularly cell death, important to you?
Kinnally And this is why you should care about this lecture. And its always important to put that into a
context, like why do I need to know this, right? We need to know this because the response to injury can
be reversible if you as a clinician give the appropriate therapy. Also know that you guys are the ones that
can diagnose stage 1 and stage 2 oral cancers. Its the dentists that pick this stuff up. That is really
important, and cancer is often associated with a disruptive cell death program, and well talk about that.
Its important to realize that most chemotherapeutic agents actually turn on cell death programs. Now
we have to figure out which ones are more appropriate for oral tissues, thats your realm.
Immunosuppressants interfere with cell death and they can cause some issues, and you might want to
modify dosage based on the oral response, the adaptation to that drug by the oral tissues. Also in the
future know that what youre learning now will have applications in ten years, therapies are being
developed which are not out yet. But you need to have a framework in which to put them, and thats
why we talk about it. Can you treat someone to turn off cell death programs before you do an extraction
and thereby reduce the volume of tissue that dies during that extraction? I dont know, but its possible.
Or is periodontal disease actually due to a premature onset of cell death? And if we can actually modify
that cell death program, maybe we can reduce periodontal disease. Youre going to have to think about
this in the next ten or 20 or 30 years.
Slide 6 Cellular Responses
Transcribed by Sofiya Khazanovich June 30, 2014
Kinnally The first thing were going to talk about is cellular responses to adaptations. Cellular
adaptations to stimuli, and theres several of these. Then well talk about reversible responses to injury
and then well talk about cells dying.
Slide 7 Hypertrophy
Kinnally Hypertrophy. I know I see some of you guys in the gym. Youre trying to hypertrophize your
biceps. Hypertrophy: this is just a definition, an increase in cell size often augmenting functional
capacity. You want big muscles, well it turns out that because muscles are more or less nonproliferative,
or have low proliferative potential, then you tend to see hypertrophy in cells that are like that. Can you
think of another one that would respond to an increase in functional demand by increasing in size? The
heart is close to my heart, the heart is the one that we often talk about or perhaps that we understand
most about hypertrophy. It clinically often results in the increase of the organ or tissue.
Slide 8 Image
Kinnally When someone is pregnant, they have a tremendous increase, a hypertrophy, of the uterus.
This is a normal size uterus here and a gravid uterus here. If you look at the cellular level, you see these
small spindly muscle cells in the normal, but the gravid are much bigger cells. This also is hypertrophy.
Slide 9 Hypertrophy
Kinnally You get again, hypertrophy in the heart, you have an increase in the cell size of the
cardiomyocytes, this is in response to increased work load. When we talked about the cardiovascular
system in organ systems, whats really a bad thing for your heart? High blood pressure, ok. High blood
pressure means theres a constant increase in the workload that the heart has to push against to get
those and maintain those valves open to eject the blood. So if you can decrease the blood pressure you
can decrease the workload. However, the cells respond with hypertrophy to an increase in workload in
the heart. And so a normal myocyte looking like this will become an adapted myocyte with much more
contractile apparatus in that cell. Which means it can contract with more strength. But an interesting
thing happens as you constantly have this stimulation to hypertrophy, to overcome this increase in
workload, or maybe just to manage the increase in workload. That is that the heart, the wall of the
ventricle increases in thickness and look what happens to the size or volume of the heart here. So, it
kind of fills in the ventricle, right? That changes your end diastolic volume, right? So because you cant
fit that much blood in a heart that looks like this, so the wall of the ventricle becomes thickened, and so
in fact you try to keep hypertrophying the heart until it fills in the ventricle, and that actually decreases
the ability to generate ejection, and cardiac output. Theres a balance to these things.
Slide 10 Causes of Hypertrophy
Kinnally What are some of the causes of hypertrophy? Well, during pregnancy or even during puberty,
theres a production of hormones that results in hypertrophy of the sex organs. You can have
exogenous for example if someone were to take anabolic steroids and get beefed up anybody watch
John Stewart yesterday, with Paul Rudd? It was hilarious. I will continue that thought Ok, but then you
can have pathological hypertrophy where prolonged stress, if you have high blood pressure and you
dont treat it, that is a prolonged stress, you can have a hemodynamic stress which ends up being a
cardiac hypertrophy, an increase of the size of the heart, and in fact decreases the ability of the heart to
generate cardiac output, by this over extensive hypertrophy. So a little bit is good, too much is not good.
Slide 11 Image
Kinnally So we are now starting to understand some of the signaling that goes on linked to cardiac
hypertrophy. Theres an increase in work needed to eject the blood, against that high blood pressure,
Transcribed by Sofiya Khazanovich June 30, 2014
and this is sensed by mechanical sensors, probably integrins in the ECM. But theres also agonists like
angiotensin II, that extremely strong vasoconstrictor that might be another mechanism underlying
cardiac hypertrophy. And then theres growth factors, these come down and they signal transcription
factors which end up increasing the amount of, for example, contractile proteins. So you have an
increase in the number of myofibrils, in each cell, which increases the cell size, and increases the
mechanical performance, at least to some point. And that enables you to handle the increase in work
load at least for some time. So cardiac hypertrophy is one of the more interesting ones that we study,
and more and more is being learned about the signaling pathways associated with this adaptation to
stress. But again, I just wanted to remind you that hypertrophy of the heart is good to a point, but then
youll have a diminishing return on cardiac output if it is excessive.
Slide 12 - Hyperplasia
Kinnally Hyperplasia is an increase in the cell number, often associated with an increase in organ size.
You usually see hypertrophy and hyperplasia together in cells that are capable of proliferating. So youd
see both happening. It can be hormonal, or compensatory, but stem cells likely contribute to this
increase in the number of cells, thereby increasing the organ size and thereby increasing in the function
of that organ. But please remember that hyperplasia may also be the beginning of a cancerous lesion.
Cancer is really a lack of control of growth, and so its good to increase it somewhat, but at some point
you want to stop that increase in cell number.
Slide 13 Image
Kinnally This is the wrong term, isnt it? What would you call that? Gingival enlargement. I cant
control myself, I always come back to this. This is a normal epidermis here, and you see how thick it is,
but here you have an epidermal hyperplasia, and this can be caused by a myriad of things like sunlight,
or chemical irritants, or whatever. And again, this is an increase in the growth of the gingiva where you
would have to actually excise this gingiva to reveal the normal teeth below.
Slide 14 Causes of Hyperplasia
Kinnally So you can again have hormonal, it can be pathological if its excessive like in the endometrial
lining of the uterus, you can have compensation if someone donates half of their liver, or one lobe of
their liver to a relative, then that liver will actually regrow. At least to some extent. So that can be
compensatory hyperplasia. You can have a secondary polycythemia if you go to higher elevation, if you
go to climb Mount Everest, which I guess is not happening this summer, you would actually try to
accommodate or get accustomed to this increase in altitude which would reduce your ability to carry
oxygen. By staying there for a little while before you try to go to the next level of Mount Everest, this
increased functional demand is caused by reduction in air pressure and oxygen in the air, so you have
more and more blood cells. You can also have hyperplasia because of persistent cell injury, and this will
be epithelial or gingival hyperplasia in response to smoking, drinking, drugs, and whatever. Chewing
tobacco.
Slide 15 Mechanism of Hyperplasia
Kinnally What is the mechanism? Well we talked about hypertrophy, but in hyperplasia it again has
some growth factor driven proliferation of mature cells, but there is an input from stem cells as well.
Slide 16 Atrophy
Kinnally So the next adaptation is atrophy. So hypertrophy, hyperplasia, and now atrophy. This is a
decrease in cell size and a decrease in cell function. Often linked to a decrease in the size or function of
the organ, and probably the most common you would think of would be if you broke your arm, and your
Transcribed by Sofiya Khazanovich June 30, 2014
arm is put into a cast, and then you dont use it for 8 weeks, and it decreases in size. Its an adaptive
response in which the cell shrinks in volume and shuts down some of its differentiated function,
whereas in cardiac hypertrophy you end up with larger heart muscle cells, here you would have a
decrease in the muscle cell size. This reduces its energy needs, and also has been linked to autophagy,
which again decreases the cell size.
Slide 17 Image
Kinnally If you looked at a normal brain of a young adult, versus an older man the size of the brain
decreases. And later on Ill show you some sections of atrophied brain due to a decrease in circulation,
or a decrease in innervation to small sections, so parts of the brain can actually decrease in size.
Slide 18 Causes of Atrophy
Kinnally Right here, see that? So if you have, this would be a lack of, or a diminished blood supply most
likely, in this region. It decreased in size because its not getting as much blood, could be due to
atherosclerosis or something like that. It may not be an acute situation or rather an adaptation to a
reduction in circulation. The physiological causes of atrophy are decrease in work load, for example if
you have a cast, or a decrease in the size of the uterus after you have a baby, or endocrine stimulation.
Slide 19 Mechanisms Underlying Atrophy
Kinnally So atrophy is a very common response to certain stimuli. You have a decrease in metabolism,
which decreases protein synthesis. If you think about whats going on at the molecular level, the cells
decrease in size for two reasons, one is autophagy, and secondly remember ubiquitin and the
proteasome pathway? Proteasome is that tube and proteins get fed in there and theyre broken down
into amino acids and then recycled after theyve been tagged by ubiquitins.
Slide 20 Metaplasia
Kinnally Next, dont worry we only have two more adaptations. Metaplasia is kind of a cool thing. This
is most common is a switch between columnar and squamous epithelium. It actually happens when the
stems cells are reprogrammed not to form columnar epithelium, but rather to form squamous
epithelium, stratified squamous is what this is called right here. So this diagram... so the switch, if they
started out being columnar, they become squamous, or if they started out squamous theyd become
columnar, probably the most common is this stratified squamous epithelium to columnar epithelium in
the esophagus, linked to something called Barrett metaplasia, and if you have acid reflux this might be
happening at the base of your esophagus. So you give up the strength of the squamous epithelium I
guess for the goblet cells of the columnar epithelium in terms of protection. But it is fully reversible,
which is kind of cool.
Slide 21 Causes of Metaplasia
Kinnally Its usually due to persistent injury, for example if you smoke itll happen in your bronchi. If
you have GERD or gastroesophageal reflux disease, it will happen in your esophagus. Or if you have a
chronic infection it may happen in the endocervix. Again its due to reprogramming of stem cells in the
adult tissues.
Slide 22 Image
Kinnally This is just simply showing the endocervix, switching between squamous epithelium and
columnar epithelium here. And this is a switch from squamous to columnar in the esophagus.
Slide 23 Epithelial Dysplasia
Transcribed by Sofiya Khazanovich June 30, 2014
Kinnally Last one is dysplasia. Dysplasia is sometimes thought of as precancerous, you have an altered
size or shape or organization of the tissue. Very often seen in epithelium, called epithelial dysplasia.
Again, caused by persistent injury, smoking, sunlight, and things of that nature.
Slide 24 Cervical Dysplasia
Kinnally So if you look here you see this nice layering of the squamous epithelium, stratified. You can
see the nuclei decrease in size and they collapse and then they essentially disappear as you get to the
surface. Right here, however, you have a cervical dysplasia, very disorganized, its not layered like it is
over here, the nuclei are prominent even near the surface, which is not how its supposed to be. So the
size, shape, and organization are changes.
Slide 25 Table 1: Cellular Reponses to Injury
Kinnally This table summarizes what weve talked about so far. And that is cellular responses to injury
and these are the physiological stimuli and the cellular adaptations. Whether they be hyperplasia, or
hypertrophy, atrophy, metaplasia, or even dysplasia. And now were going to move on and start talking
about this injury and what happens when cells are reversibly and then irreversible injured.
Slide 26 Reversible Changes Induced by Injury
Kinnally The first thing that happens when you have a reversible stress or injury to cells is that cells
start to swell. And you get something called hydropic swelling. You also get a coalescence of lipid
droplets in the cytoplasm, so if you look at them in electromicrographs, this is clearly visible. But, when
they used to have autopsies on TV, and the first thing they do is weigh the organ, remove it and then
weigh it. They take out the liver or heart and weigh it, because they can tell whether or not if its
stressed, if the body has been stressed before death, then you have swelling of various organs, and they
can tell about time of death and things like that, because it doesnt happen because if you werent
stressed before cell death, before the person died. What happens is as the cell swells they lose microvilli
and they start to bleb. Blebbing is the out pouching of the plasma membrane. Mitochondria and ER
swells, ribosomes fall off, and the nucleus starts to clump.
Slide 27 Image
Kinnally This is sort of a summary right here, we have the normal ER, and your swollen ER.
Mitochondria a little bit swollen but not too swollen, heres the blebbing, and the chromatin is starting
to clump. But if you remove that issue, and what that issue often is, is if you dont have proper
circulation then you dont have proper oxygenation, and then you dont have proper ATP production,
then you end up with hydropic swelling. First thing that happens. So, this is totally reversible and the cell
can return to normal. For example, when someone is having a heart attack and they go to the hospital
and their coronary artery is blocked, they give them a clot buster and that reopens the circulation to
that section of the heart, so if you do this quickly enough, you can have reversible changes. But at some
point, it becomes irreversible and the cell dies, and typically the cell dies by the process of necrosis. And
were going to talk about that.
Slide 28 Progression of changes induced by cell injury
Kinnally So theres a progression of cell injury. Originally, as far as function declines, it will continue to
decline but can be reversed for some time and Im not going to say fifteen minutes, Im not going to say
two hours, it depends strongly on the nature of the cell and the nature of the injury. But theres a
certain time when things are reversible. Cell function has declined, but the response is reversible. But
then you start to have some biochemical changes, and this is irreversible. First come biochemical
Transcribed by Sofiya Khazanovich June 30, 2014
alterations, and the result is ultra-structural changes, which can then be detected at the level of the light
microscope or during an autopsy when you weigh the organ.
Slide 29 Image
Kinnally This is an example of some of the changes that occur at the light and the electromicroscopic
level. This is normal kidney tubules, these are swollen, some of the nuclei are kind of clumpy, the
cytoplasm is starting to reduce its red intensity, here you get a disorganization during necrosis, this is
not reversible. If you look at the electron microscope level, these are mitochondria, see how thick they
are? Theyre about twice as thick during reversible injury, but you see how gigantic they are if its
necrotic and the cells are dead? You have here microvilli, you lose the microvilli as the cell swells, and
then the plasma membrane disrupts when the cell dies.
Slide 30 Hydropic Swelling
Kinnally Hydropic swelling is an increase in cell volume. The cytoplasm starts to look paler and more
dilute. But the nucleus is not strongly affected, its normal in its location. So hydropic swelling is
reversible cell injury. And why does it happen? Usually it happens because you dont have enough ATP.
If you dont have enough ATP, what is the number one utilization or energy cost in the cell? Sodium-
potassium ATPase. So Sodium-potassium ATPase falls, you have an accumulation of sodium in the cell,
and water rushes in causing swelling. Its reversible because if you restore the ability to make ATP, then
the Sodium-potassium ATPase starts to work, pumping out the sodium, water follows, and everybodys
happy.
Slide 31 Hydropic swelling is a reversible adaptation to injury
Kinnally This is again more pictures of what it looks like. You can see that this area of the liver looks
much less dense than the rest of it. This area is undergoing hydropic swelling, and you can see here the
cytoplasm is very dilute compared to here. And the nuclei are actually a little bit smaller, so its starting
to clump. This is normal and this is kind of clumped.
Slide 32 Morphological patterns of necrotic pathway
Kinnally Were going to look at dead cells. What happens to necrotic cells? Now necrosis has been
around for a long long time. And necrosis at the level of the microscope or just looking at the tissue, a
gross level, doesnt necessarily tell you what the mechanism of cell death is. But since necrosis has been
around for a very long time, we still dont understand it, and actually were starting to understand it
much better, but there are six defined kinds of necrosis, and were going to talk about them. Again this
is not necessarily defining the mechanism, but rather what it looks like. Its defining the pathology of the
disease. So the first is coagulative necrosis, is if you have a heart attack. Liquifactive, this is if you have a
bacterial infection and you have pus, gangrenous is kind of a combination of coagulative and liquifactive,
caseous necrosis is more or less specific to TB, fat necrosis happens when you have pancreatitis and
pancreatic enzymes leak into the abdomen, and fibrinoid necrosis is a vasculitis associated with blood
vessels.
Slide 33 Coagulative necrosis
Kinnally This is a normal heart, and this is a heart thats been stained... theyve both been stained to
look at viable tissue. If it doesnt stain red then its dead. This region right here is a myocardial infarct
and it doesnt stain. So whats happened here is this normal myocyte has been reversibly and then
irreversibly harmed. Probably due to atherosclerosis, someone has a clogged coronary artery, youre not
getting blood and nutrients to the heart, and the heart tissue then dies. A lot of what happens is the
architecture is maintained, and the tissue is firm, but its coagulating due to pH changes because when
Transcribed by Sofiya Khazanovich June 30, 2014
the cells lyse, they also lyse lysosomes, and the lysosomes then kill or fix essentially the protein in the
cytoplasm.
Slide 34 Coagulative necrosis in myocardium
Kinnally This is at the light microscopy level. These are normal myocytes, and here you can see after
coagulative necrosis, the nuclei are very contracted, very darkly stained, fragmented... but the general
structure of the cell looks pretty good. But its not functioning.
Slide 35 Liquifactive necrosis
Kinnally In fact, the heart stops beating after just 60 seconds of hypoxia, so if you dont constantly give
the heart cells oxygen and food and take away waste, they stop beating very rapidly. So in liquifactive
necrosis, you can have an infection caused by bacteria or by funguses. And then you have an invasion of
leukocytes to eat the bacteria or the fungus and they have hydrolases to digest the dead cells. Now
normally, these are absorbed, that is taken away, very rapidly, but if the digestion of dead cells happens
faster than that material can be removed, then you have something called the formation of pus. So
liquifactive, if you need to remember it this way, liquifactive means you have a liquification of the tissue,
and the formation of pus. You always have leukocytes. Now, I dont know that the mechanism is well
understood but you also see the same thing in cerebral infarcts without bacterial infection.
Slide 36 Image
Kinnally This is in the skin, you have an abscess formed in this region with lots of invading leukocytes.
Slide 37 Image
Kinnally This is in the brain, if you have a stroke or a lack of circulation to one region, then you have
liquifactive necrosis in the brain. Where the structure is dissolved.
Slide 38 Gangrene of 1-4
th
toes of a diabetic
Kinnally This is gangrene. I have trouble looking at this one. Anyway, in gangrene you have essentially
a combination of the infection and coagulative necrosis.
Slide 39 Image
Kinnally In caseous necrosis, thats hard to believe that thats a lung right? But, this is someone that
has TB. And it is this region here, the cheesy necrotic region in here, but its more or less just in TB.
Slide 40 Image
Kinnally This would be fat necrosis, again if you have pancreatitis and the pancreatic enzymes are
leaked into the abdominal cavity, then they will do this to any fat thats hanging around. And you can
see that there. Its a saponification of the mesentery.
Slide 41 Image
Kinnally And this would be fibrinoid necrosis. And that would be this thing right here. So heres your
blood vessel, and this pink ring around here is an area of necrosis because antibodies have accumulated
in this area and eventually the cells die.
Slide 42 Mechanisms of cell injury
Kinnally Those are several forms of necrosis, each having their own cause, selective for the type of cell
that youre looking at. But in general, the same things happen to kill a cell. And probably foremost would
be a loss of ATP or ATP production because ATP even though youve been hearing this since you were in
Transcribed by Sofiya Khazanovich June 30, 2014
the third grade, ATP is the energy currency of the cell, and it really actually is. So if you dont have
enough ATP, then all kinds of bad things will happen. Were going to go through them. Now
mitochondrial damage leads to a decrease in ATP, but actually it can be separate because if you
remember from cell biology, remember I talked about them being deathsomes and they contain
materials which upon release then activate the cell death pathways. You can have the entrance of
calcium, and calcium being a second messenger normally is in the cell at about 10-8M but outside the
cell its how many, 10-3M, so thats a huge gradient. Five orders of magnitude across the plasma
membrane, and if a little bit leaks in, it can activate all kinds of things, for example calcium activated
proteases which would then chew up the cell. Furthermore, they will modify your mitochondria, and
well talk about that in a few minutes. Now, reactive oxygen species or oxidative stress damages lipids,
proteins, and DNA. I dont think its effect on carbohydrates is that severe. One of the most important
things is membrane damage, if you have damage to the plasma membrane, then the cellular contents,
you lose your homeostasis when you lose that barrier. And you dump cytoplasmic proteins into the
ECM. But almost more importantly, before that happens, if you have breakdown of the lysosomal
membranes, then you have release of all of these enzymatic you have enzymatic digestion of the cell.
Breakdown or lysis of membranes is very bad, that will also decrease the pH and again fix the proteins.
Theres something called the unfolding protein response. When proteins are not being folded properly
in the ER, which can be linked to a reduction in ATP by the way, you can have DNA damage as well, both
of these things will result in activation of the process of programmed cell death. So all of these things in
combination or alone can cause cell death. Most commonly it would be mitochondrial damage, and the
inability to maintain ATP levels, along with membrane damage, would be the two most significant
reasons a cell will die.
Slide 43 Consequences of ATP depletion
Kinnally So now I want to make sure that you understand the consequences of ATP depletion and the
steps that happen. So if you have a reduction in ATP and why would that happen? You can have
ischemia, right? Failure to circulate the blood in a certain region. That decreases the sodium potassium
ATPase activity, it also decreases the Calcium-ATPase activity, so you have an influx of calcium and an
influx of sodium. You also have potassium leaking out, so youve thrown away one of the standards of
cellular homeostasis and that is the maintenance of ionic gradients. These ionic gradients are so
important to so many things. So many transport mechanisms and osmotic pressure and all of those
things get thrown out the window when you dont have enough ATP. You end up with swelling of the ER
and the cell, loss of microvilli, and blebbing of the plasma membrane. When you dont have enough ATP
you stimulate glycolysis until you dont have any glycogen left, but that increases lactic acid and drops
the pH. Which is okay, but the cell is actually only functioning between a very small pH range. It doesnt
like big pH changes and when your pH changes become significant you get protein fixation but you also
get nuclear chromatin clumping, so that your transcription translation is messed up as well. Again, you
dont have enough ATP, the ribosomes fall off the RER, you drop your protein synthesis, and you start to
deposit, you make these little puddles of lipid inside the cell.
Slide 44 Consequences of mitochondrial damage
Kinnally So mitochondrial damage, and you guys know I dont know anything about mitochondria,
right? Ok, mitochondria make the ATP, and the consequences of damaging is the opening of two pores.
If you open the permeability transition pore, the cell dies by the process of necrosis. If you open the
mitochondrial apoptosis induced channel, the cell dies by the process of apoptosis. So, the
consequences of mitochondrial damage are one of these two things. Now interestingly, PTP or
activation of necrosis occurs by cytosolic calcium elevations, reactive oxygen species formation, or
oxidative stress, or depolarization of the mitochondria, all open this channel called PTP. And when that
Transcribed by Sofiya Khazanovich June 30, 2014
happens you lose your mitochondrial membrane potential if you havent already lost it, and then you
cant make any more ATP and it becomes a cyclical event, a vicious down spiral. If you open MAC then
you release cytochrome C and other apoptotic proteins and you enter apoptosis. So messing with your
mitochondria is not a good idea.
Slide 45 Loss of calcium homeostasis
Kinnally If you have loss of calcium homeostasis, the important secondary messenger, then you can
release calcium from the ER and any mitochondrial reserves of calcium, they activate cellular enzymes
alternatively they open the permeability transition pore which again decreases ATP production. We go
back here, you have phospholipases, proteases, nucleases, everything is messed up. You end up with
DNA damage, membrane damage, a lack of ATP, and the cell is going to die.
Slide 46 Oxidative Stress
Kinnally Oxidative stress, this is tightly linked to mitochondria because mitochondria make most of the
active oxygen species in the cell. You have production of superoxide which leads to peroxide and
possibly hydroxyradical, but all of these can interact with protein, lipid, and DNA, modifying them, and
making them nonfunctional. So here, reactive oxygen species reacts with fatty acids, which then disrupts
the plasma membrane, proteins which gives you a loss of enzyme activity, or DNA breaks mutations and
so on. But your body has a bunch of mechanisms to remove these reactive oxygen species or free
radicals. First is superoxide dismutase, it removes superoxide into peroxide, which is much less reactive.
Superoxide dismutase in mitochondria is known to be mutated in something called ALS or Lou Gehrigs
Disease, and you can see here that that would be right at the heart, if you dont have superoxide
dismutase, here, then youre not going to be able to break down those free radicals, and that free
radicals will eventually destroy your mitochondria and destroy your cells and happens in the nervous
system first. Theres also glutathione peroxidase and catalase, especially in peroxisomes.
Slide 47 Membrane damage
Kinnally So the membrane damage that can happen is theres two membranes, or three membranes
that are actually really important. The plasma membrane for delineation of the outside of the cell, the
mitochondria because they contain these pro-death factors, and the lysosomes because they contain
those enzymes that can autodigest the cells. So, reactive oxygen species breaks down lipids, which
breaks down membranes. Phospholipase activation, again, breakdown membranes, increase calcium in
the cytoplasm activates proteases, all of these and then theres that structure the cytoskeleton of the
cell, which actually maintains cell structure. If you start to protease that away into nothingness, then of
course youre going to put great stress on the membranes and cause membrane damage. And again
.lysosomes, plasma membrane, and mitochondria are the three that get damaged to which those three
is the most dangerous or most important.
Slide 48 Necrotic pathology
Kinnally So weve been talking about necrosis, necrotic pathology, but how do cells actually die? Thats
what were going to talk about now.
Slide 49 Cells injured irreversibly when
Kinnally And the three ways that you can die. So, DNA damage causes death by apoptosis. Whats the
guardian of the genome called? P53, yes, very important protein. P53 is mutated in half of the cancers
around. So if you dont have P53, you dont die by apoptosis, so that cancer cells continue to grow when
they shouldnt grow, that make sense? So very important. In autophagy, you have a lack of food. And
then the body starts to autodigest itself in a very controlled manner, it encloses mitochondria inside
Transcribed by Sofiya Khazanovich June 30, 2014
these membranes and then digests them, very controlled, so you dont have release of these
proapoptotic factors into the cytosol. But eventually, theres no food, no food, no food, and then you
die. You starve to death. And the third mechanism is necrosis where membranes are damaged or ATP
levels are not restored. And when theyre not restored, what happens to that cell that starts swelling
and keeps swelling? It pops. Death by necrosis.
Slide 50 Three ways to die
Kinnally So, three ways to die. Apoptosis, autophagy, and necrosis are the three, and the underlying
mechanisms, while there is overlap, which is just starting to be understood at this point, they have
different underlying mechanisms.
Slide 51 Image
Kinnally So I showed this to you last year, because I thought it was funny. You could laugh. I know its
the first day of class, but youre D2s now, right? Ok, this is very controlled, this is not, and this is fade
away. Ok.
Slide 52 Image
Kinnally Now the molecular players in programmed cell death, the three processes of programmed cell
death, autophagy, apoptosis, and necrosis, are now becoming known. And everybody is so surprised, it
used to be autophagy was not thought of as a cell death program. It is now recognized as a cell death
program. So, your body tries to survive, the cells try to survive, and then they cant survive, and you
switch to one of these other alternatives of autophagy, apoptosis, or necrosis, but there are survival
programs where if you have a lot of DNA damage for example, your body up regulates the enzymes that
will fix those broken pieces of DNA. And then if it fails, P53 which is the protein that turns on, its the
transcription factor that turns on all of those enzymes to fix the DNA, if it doesnt then P53 then turns on
the Bcl-2 killer proteins, and so the killer protein tries to fix the cell and then kills the cell if it isnt fixed.
But thats not what is shown here. This is an illustration, it doesnt have an asterisk on it. That means
dont try to memorize this. Believe me, next week the pattern will be different. Its still being developed.
There are various proteins that are overlapping in the pathways of autophagy and apoptosis, theres the
Bcl-2 family, and in necrosis and apoptosis it seems to be this new interesting one called the Rip1 or Rip1
kinase, seems to be a very important player in something called necrotosis versus apoptosis. But, you
see Rip1 is here and here in the necrosis pathway but its also here in the apoptosis pathway, and its
also in the survival pathway. So Rip1 is going to turn out to be very important. And this Rip1 kinase is
actually a therapeutic target for inhibiting and so if we can inhibit Rip1 kinase maybe we can block all of
these, we dont know yet.
Slide 53 Autophagy
Kinnally Were going to back up a little and talk very briefly about autophagy. You have formations of
autophagic vacuoles, if there is a nutrient depletion. Youre not getting enough food, probably due to a
decrease in circulation to that region. You get a signal, you get formation of these autophagic vacuoles
which then fuse very cleanly with lysosomes which then degrade whatever was in there, and you have
release of nutrients into the cytosol. Here you can see a peroxisome and mitochondria inside an
autophagolysosome. So these are being broken down. Typically the mitochondria are depolarized at this
point, theyre not making ATP, theyre not functioning, and thats why those are first targeted for
autophagy.
Slide 54 Image
Transcribed by Sofiya Khazanovich June 30, 2014
Kinnally I thought that this was kind of a cool picture. This is actually out of my lab. These are normal
cells, and these are cells treated with an inhibitor of a drug, but it in five minutes caused this enormous
amount of autophagy, and you see these vacuole formations, these little bubbles are vacuoles inside
these cells. So this is in salivary gland cells.
Slide 55 Hypoxia vs. Ischemia vs. Ischemia-reperfusion injury
Kinnally Now I want to talk a little bit about hypoxia again, a little bit more about hypoxia, ischemia,
and ischemia-reperfusion injury, because they cause necrosis. Now we wanted to get some clinical stuff
in here. So, hypoxia is a reduction in oxygen. So when do you get hypoxic? Hypoxia is not a restricted
circulation to one region caused by a clot or atherosclerosis, ok? Its when you have an overall reduction
in the oxygen carrying capacity of the blood, and how can that happen? Or the amount of oxygen
dissolved in the blood is reduced. You could be at high altitude. Your ability to get oxygen into your
circulatory system is reduced because the air pressure of oxygen is reduced. You could also have
congestive heart failure, and in congestive heart failure you usually have pulmonary edema, so the
surface area in the lungs where you have that exchange of oxygen is reduced, and so the ability of
oxygen to get into the red blood cells and CO2 to leave is reduced, so your ability to perfuse or
oxygenated blood is reduced. COPD is the other one, again chronic obstructive pulmonary diseases like
emphysema, you dont have proper oxygenation, reduction in surface area of capillaries and alveoli,
reduces the transport of oxygen into the blood. But theres very different from ischemia, which is when
you have reduced blood flow to a specific area. For example if you have a blood clot or atherosclerosis,
reducing the delivery of blood to one region for example in the heart. So the supply of oxygen and
metabolic substrates is reduced including glucose. That doesnt happen up here, here its a delivery of
oxygen and removal of CO2, but glucose is being delivered to the cells during hypoxia, its not being
delivered to the cells during ischemia. So ischemic tissues are injured more rapidly than hypoxic tissues
because ischemia gives you a double whammy. Now whats really kind of paradoxical is something
called ischemia-reperfusion injury, and whats really terrible is that if you have a blood clot or
atherosclerosis, and you go in and you get one of those blood clotters, or youve had a stroke and its
only within an hour or so, and you get to the hospital and they give you a clot buster, thats great. They
re-oxygenate the area and save cells. But lets say its been four or six hours. They cant give the clot
buster because of ischemia reperfusion injury. When you reperfuse that area you actually kill more cells.
Why would that happen? What happens is the mitochondria for example become fully reduced, they
have no place to send their electrons, so theyre all in the electron transport system, you bring oxygen in
suddenly, and it just rips. And it makes a ton of reactive oxygen species, and that reactive oxygen species
then kills a bunch of cells. So, ischemia reperfusion injury is death upon reperfusion after ischemia
caused mostly by reactive oxygen species, but theres also a component caused by complement, by IgM
antibodies and cytokines in the inflammatory response. So its really terrible, but again, you have that
line, that reversible versus irreversible line that has been drawn in the sand.
Slide 56 Image
Kinnally So this really just summarizes what Ive said already. If you have ischemia, you have
reversible, you have a reduction in oxygen available to mitochondria, so ATP levels drop, the ability to
remove sodium from cytoplasm and potassium into cytoplasm is reduced, you have an influx of calcium
and a deflux of potassium. You also have an increase in glycolysis which leads to a drop in pH due to
lactic acid, and a decrease in the amount of stored glycogen. Other effects are detachment of ribosomes
from RER, decrease in protein synthesis, and lipid deposition. Here you have that line in the sand that
goes from reversible to irreversible, and those are typically due to mitochondrial damage or inability to
restore mitochondrial function or membrane damage either to the plasma membrane or to the
lysosomes. So, just remember cardiac cells stop beating after 60 minutes but you can restore their
Transcribed by Sofiya Khazanovich June 30, 2014
activity for quite a long time after that. But remember that slide I showed you, function drops and then
biochemical changes linked to irreversible changes come up, so you first lose function and then you
become irreversibly damaged.
Slide 57 Image
Kinnally I just thought Id show you this if you have calcium overload, calcium is released from the ER,
an influx from the plasma membrane, you can then have opening of the permeability transition pore in
mitochondria and a loss of membrane potential. When you lose membrane potential in you
mitochondria you lose the ability to make ATP. The mitochondria swell, the outer membrane ruptures,
dumping things into the cytoplasm that shouldnt be there, and this kills the cell.
Slide 58 Image
Kinnally Again, this is the necrotosis pathway, and again theres no asterisk on this because it will
change next week. But again we have rip kinase and theres an overlap between necrosis and apoptosis,
but you can inhibit necrosis using necrostatin but you have to remember that theres a yin and a yang to
all of these things. Just like hypertrophy of the heart is a good thing until its not. Inhibiting things like
necrosis or apoptosis are a good thing until theyre not because necrosis for example also plays a role in
things like wound healing and the immune response as does apoptosis. So inhibiting these forever is not
necessarily a solution, but understanding the processes that are going on can make our ability to
develop therapeutics much better.
Slide 59 Apoptosis: 70 billion cells/day
Kinnally So, now were going to move to apoptosis. And this does have an asterisk on it. So, 70 billion
cells a day, thats a lot of cells. How many cells do we have? Ten to the thirteenth or fourteenth cells.
Whats a billion? Ten to the ninth? Thats a lot, thats a large fraction of the cells turning over. Apoptosis
is important in tissue homeostasis. You want that organ to remain the same size. So you want
proliferation and death to match. When they dont match thats when you end up with pathology. It
plays an important part in embryogenesis, for example the hands starts out as a ball, becomes a plate,
and then the cells between the digits die. Involution happens in both the uterus and the lactating breast.
Its used constantly for ridding the body of self-reactive lymphocytes and inflammatory neutrophils. So
Dr. McCutcheon is going to talk a lot about apoptosis and you have to understand that apoptosis is very
closely linked to the immune response. But apoptosis doesnt cause inflammation, but its used by the
immune system during the immune response. Now apoptosis becomes pathological if you knock out
P53, you dont recognize DNA damage and then you fail to induce apoptosis. Normally P53 says that cell
has busted up DNA, kill it, or kill yourself kind of thing. Then theres UPR or unfolded protein response,
and some infections can also cause pathological apoptosis.
Slide 60 General Characteristics of Apoptosis
Kinnally The general characteristics, you guys have seen this before. You have loss of lipid bilayer,
asymmetry, normally phosphatyl serine has a tiny little head group compared to other lipids like PC
phosphatyl choline, so PS is normally on the inner leaflet of the plasma membrane, but during apoptosis
it flips to the outer leaflet and acts as an eat me signal to lymphocytes, so macrophages. You get nuclear
shrinkage, DNA laddering, thats shown right here, Ill talk more about that in a minute. The membranes
blebbing but it was blebbing already, but the cell will round up and lose its attachment to other cells and
eventually the last thing that happens is a loss of plasma membrane integrity as this cell turns into this.
Slide 61 Image
Transcribed by Sofiya Khazanovich June 30, 2014
Kinnally So this is a comparison of necrosis and apoptosis. During necrosis the cell is swelling and
during apoptosis the cell is shrinking. So thats dramatically a very big difference. The next thing is that
you have progressive injury and you have an inflammation caused during necrosis, a breakdown in
plasma membrane integrity, and mitochondria swell, they become dysfunctional. In apoptosis in fact the
mitochondria function for a long time. You have cell shrinkage and you have membrane blebbing and
eventually the formation of something called apoptotic bodies, as the cell releases small parts of itself
for phagocytosis by macrophages.
Slide 62 Necrosis vs. Apoptosis
Kinnally And this is just the same thing I just said only in words. Necrosis is not thought to be as well
controlled but were finding out as time goes by that its not the uncontrolled process that we used to
think it is. Apoptosis is a well-controlled suicide. You have necrosis is often caused by poison, trauma, or
infection. Apoptosis you can have cell signaling as well as things like DNA damage that cause apoptosis.
This one induces in the inflammatory response and this does not. That is a major difference. The cells
just disappear after apoptosis. They do not cause an immune response, otherwise we would have a lot
of pus around. Again, theyre both cleared by the immune system, apoptosis is regulated by Bcl2 family
proteins, and plasma membrane is lost first in necrosis and last in apoptosis.
Slide 63 Key players in apoptosis
Kinnally Were going to talk briefly about the key players but this is kind of a review of the stuff that
you know from last year. I know its all crystal clear coming back to you now. Caspases are the
executioners of death, endonucleases chew up DNA, the Bcl2 family proteins are the rheostats,
mitochondria are involved in storage of those Bcl2 family proteins, theres also death receptors located
on the plasma membrane which can activate apoptosis.
Slide 64 Caspases
Kinnally Alright, caspases exist as zymogens, they are cysteine proteases, theres at least 14 different
kinds, and they execute apoptosis by cleaving a restricted set of proteins. What happens is the
cytoplasm becomes dissolved, theres all these fibrils and things like that inside, theres something
called gelsolin which gives a jello like quality to the cytoplasm, and that gets cleaved and so the
cytoplasm liquefies. The caspase activated DNAse is CAD, is cleaved activating the caspase activated
DNAse, which then chews up the DNA, the nucleus collapses on itself as PARP is broken down, and PAK2
which gives structure to the plasma membrane is broken down and thats what gives rise to the
membrane blebbing that you have.
Slide 65 Endonucleases
Kinnally Endonucleases break down DNA and this is normal DNA, this is DNA from an apoptotic cell,
and this is DNA from a necrotic cell. Here you have endonucleases cleaving between the nucleosomes of
the DNA sort of like cleaving between pearls on a string, and thats what gives rise to this beautiful
ladder. It doesnt happen in such an orderly fashion in necrosis, its more random and so you end up
with a smear, if you look at the DNA of the necrotic tissue. And again, if its normal the cell is not dying,
then the DNA is very big and it doesnt enter into these agarose gels.
Slide 66 Image
Kinnally There are two pathways for apoptosis and they converge at activation of executioner
caspases, which is right there, that red box. P53 is there monitoring for DNA damage and resulting in the
activation of executioner caspases. Bcl2 family proteins are there regulating the mitochondrial response.
But as I said there are two pathways for apoptosis, which converge right here. There is the intrinsic or
Transcribed by Sofiya Khazanovich June 30, 2014
mitochondrial pathway, and there is the extrinsic or death receptor pathway which takes a signal from
the outside, for example tumor necrosis factor or FAS ligand, the external initiator of apoptosis is out
here, whereas the mitochondrial pathway usually targets things like DNA damage from the inside.
Slide 67 Image
Kinnally This is the Blc2 family of proteins, having anti and pro apoptotic factors. They actually work
together to balance one another. If you have an overexpression of the proapoptotic proteins, like BAX
and BIK, then you die prematurely. An example would be in neurodegenerative disease. If the anti-
apoptotic proteins, for example Bcl2, Bclxl and others are overexpressed, then you fail to die when you
should die. You fail to die when you should die and that becomes cancer. So its very important
nowadays as it turns out that theres a bunch of anti-apoptotic proteins and some of them are listed
right here, if someone has a cancerous growth what they do is they genotype it or they characterize it,
and they look for the expression levels of these proteins because now they have specific inhibitors of
things like Bcl2 or Mcl1. So they can knock down the overexpressed anti-apoptotic protein and then
enable the cells to enter the death pathways as they should. And the really good thing about it is that
this doesnt cause any of the side effects that you normally have with chemotherapy, so theyre much
easier on the person. So tumor signatures can lead to personalized medicine.
Slide 68 Image
Kinnally But here I wanted to show you some work in our lab, which is the formation of MAC, or the
mitochondrial apoptosis induced channel. Bax translocates to the mitochondrial outer membrane
forming a channel we call MAC, releasing cytochrome c which binds apath1 and procaspase9 to form the
apoptosome which activates caspases and kills the cell. But if you can overexpress Bcl2 then youll
prevent release of cytochrome c and prevent cell death linked to degenerative diseases for example. So
cytochrome c is not released when these proteins are bound up with Bcl2.
Slide 69 Cells kill other cells by inducing apoptosis
Kinnally Cells kill other cells by inducing apoptosis and this is mostly done by the immune system
through the extrinsic pathway of apoptosis. This also happens with Fas ligand and happens with tumor
necrosis factor, and Im sure Dr. McCutcheon will give you a lot more details. Also they have killer
lymphocytes injecting granzymes through something called perforin. If you are virally infected. If you
have a virus inside, intracellular virus, then the immune system will kill that virus infected cell using
something called granzyme to activate apoptosis.
Slide 70 Features of apoptosis essential to the immune response
Kinnally This probably should have two asterisks on it. Even though weve talked about this before,
features of apoptosis essential to the immune response is actually really important to become part of
your normal thinking. The important reason is that cells autodigest during apoptosis before they lose
plasma membrane integrity. So everything is contained, the last step is release of these dissolved or
digested things into the ECM after the pathogens are destroyed. If you had necrosis, then that would be
the first thing that happened, the plasma membrane pops, so activation or complete cleavage and
digestion of these intracellular pathogens wouldnt happen.
Slide 71 Macroscopic inspection
Kinnally Another thing I wanted to mention briefly is macroscopic inspection may not reveal what kind
of death it is, but the type of death may change the treatment that you apply. For example a Bcl2
inhibitor would not be used for necrosis whereas necrostatin would not be used for autophagy. So as we
understand these pathways, well be able to develop better therapies.
Transcribed by Sofiya Khazanovich June 30, 2014
Slide 72 Important
Kinnally And we dont know all the answers, but therapeutic approaches are ongoing and you need to
stay current in your profession. Now I have these two movies, Im not going to show them. You saw
them last year but Ill put them in the same folder and one is intrinsic apoptosis and the other is
extrinsic. Any questions? Thank you!
You might also like
- Circadian Rhythm Reset for Better Sleep and MetabolismDocument22 pagesCircadian Rhythm Reset for Better Sleep and Metabolismfyrtenheimer100% (1)
- Weight Training: A Beginners Guide to Building a Leaner, Bigger, Stronger Body, Naturally and EasilyFrom EverandWeight Training: A Beginners Guide to Building a Leaner, Bigger, Stronger Body, Naturally and EasilyRating: 5 out of 5 stars5/5 (5)
- Cancer Is DEAD Cancer Cures From A To ZDocument169 pagesCancer Is DEAD Cancer Cures From A To Zcamjob80% (5)
- Autoimmune Matrix DR Peter Osborne EbookDocument68 pagesAutoimmune Matrix DR Peter Osborne EbookSoftMan100% (1)
- Secrets of Mind Body HealingDocument17 pagesSecrets of Mind Body Healingtemporal130100% (1)
- Natures.n1 Healing - SecretDocument29 pagesNatures.n1 Healing - Secretwikorv8497No ratings yet
- Deep Muscle Therapy 1 Intro 06Document33 pagesDeep Muscle Therapy 1 Intro 06Enyaw DroffatsNo ratings yet
- Biology PDFDocument29 pagesBiology PDFThePhantomStranger100% (1)
- The Heart of Flow PDFDocument72 pagesThe Heart of Flow PDFBenjamin Rüffin100% (2)
- Energy Blueprint 4 Secrets To Fatigue 6 Science Backed Strategies To Dramatically Increase Your EnergyDocument32 pagesEnergy Blueprint 4 Secrets To Fatigue 6 Science Backed Strategies To Dramatically Increase Your EnergyFuerza VitalNo ratings yet
- Vagus Nerve Exercises To Rewire Your Brain: Stimulate Your Vagus Nerve With Natural Self-Healing Daily Exercises For Anxiety, Depression, Trauma & OverthinkingFrom EverandVagus Nerve Exercises To Rewire Your Brain: Stimulate Your Vagus Nerve With Natural Self-Healing Daily Exercises For Anxiety, Depression, Trauma & OverthinkingNo ratings yet
- 3 Interview Transcripts From The Superhuman Energy SummitDocument54 pages3 Interview Transcripts From The Superhuman Energy SummitFuerza VitalNo ratings yet
- Joe Rozencwajg InterviewDocument17 pagesJoe Rozencwajg InterviewGold SunriseNo ratings yet
- The Uplink: Issue No.5Document2 pagesThe Uplink: Issue No.5taichi7No ratings yet
- Patho Supplement Handout For Sept 2018 UPDATED May 2018 PDFDocument25 pagesPatho Supplement Handout For Sept 2018 UPDATED May 2018 PDFemely p. tango100% (1)
- Chronic Fatigue: Defeating Permanent Fatigue and Starting the Day with Renewed StrengthFrom EverandChronic Fatigue: Defeating Permanent Fatigue and Starting the Day with Renewed StrengthRating: 5 out of 5 stars5/5 (2)
- Klinghardt Introduction To Light and The Human BiofieldDocument14 pagesKlinghardt Introduction To Light and The Human BiofieldPoorni ShivaramNo ratings yet
- Healthy, Happy Gut Summit™: Everything You Need To Know About Probiotics Michael RuscioDocument15 pagesHealthy, Happy Gut Summit™: Everything You Need To Know About Probiotics Michael RuscioMiha VucNo ratings yet
- Auto Immune Disease and Fibromyalgia: The Traumatic Brain Injury Connection: TRAUMATIC BRAIN INJURY: TBI & POST-CONCUSSION SYNDOME: PCS, #3From EverandAuto Immune Disease and Fibromyalgia: The Traumatic Brain Injury Connection: TRAUMATIC BRAIN INJURY: TBI & POST-CONCUSSION SYNDOME: PCS, #3No ratings yet
- CH Dreaming NeurogenesisDocument31 pagesCH Dreaming NeurogenesisrommelsousaNo ratings yet
- Homeo TipsDocument146 pagesHomeo TipsBalaji Siddhu100% (2)
- Homeo TipsDocument124 pagesHomeo TipsAditya uniyal100% (2)
- Lesson: Dr. Leon Hammer, M.DDocument14 pagesLesson: Dr. Leon Hammer, M.DRocío JMNo ratings yet
- Secrets of Mind Body HealingDocument19 pagesSecrets of Mind Body HealingCarolBhagavatiMcDonnellNo ratings yet
- The Thyroid SolutionDocument21 pagesThe Thyroid SolutionJosh Bill100% (1)
- Diagnosing and treating chronic stressDocument8 pagesDiagnosing and treating chronic stressAlex Maric Dragas100% (1)
- Chronic Fatigue: Defeating Permanent Fatigue and Starting the Day with Renewed Strength (Chronic Fatigue Syndrome, Tiredness, Burnout)From EverandChronic Fatigue: Defeating Permanent Fatigue and Starting the Day with Renewed Strength (Chronic Fatigue Syndrome, Tiredness, Burnout)No ratings yet
- The Whole Brain Diet: the microbiome solution to heal depression, anxiety, and mental fog without prescription drugsFrom EverandThe Whole Brain Diet: the microbiome solution to heal depression, anxiety, and mental fog without prescription drugsNo ratings yet
- DR Sarno Free - Report - 11!09!11Document9 pagesDR Sarno Free - Report - 11!09!11Crisalcala100% (3)
- Heal Yourself in 15 DaysDocument37 pagesHeal Yourself in 15 DaysAtma Love100% (3)
- Migraines and Epilepsy: How to Find Relief, Live Well, and Protect Your BrainFrom EverandMigraines and Epilepsy: How to Find Relief, Live Well, and Protect Your BrainNo ratings yet
- You Are Your Own Best Medicine: A Doctor's Advice on the Body's Natural Healing PowersFrom EverandYou Are Your Own Best Medicine: A Doctor's Advice on the Body's Natural Healing PowersRating: 4 out of 5 stars4/5 (2)
- Pandemics Have Occurred Throughout The DecadesDocument4 pagesPandemics Have Occurred Throughout The DecadesPhiNo LupHt DindudNo ratings yet
- The Importance of Symptomatic Treatment 1376187581Document4 pagesThe Importance of Symptomatic Treatment 1376187581giullianosilva4874No ratings yet
- Understanding Atrophy, Hypertrophy and HyperplasiaDocument30 pagesUnderstanding Atrophy, Hypertrophy and HyperplasiaFiras Anaya100% (1)
- Medical English: Explaining Investigations and ProceduresDocument41 pagesMedical English: Explaining Investigations and Proceduresfiorella lombardiNo ratings yet
- Q: What Are The Origins of The Stress Response?Document5 pagesQ: What Are The Origins of The Stress Response?Ser Jhun ChangNo ratings yet
- Facing Neu Ent Fearlessly: Ro AssessmDocument7 pagesFacing Neu Ent Fearlessly: Ro AssessmokipashaNo ratings yet
- Article On CellsDocument5 pagesArticle On CellsCad NoviceNo ratings yet
- Antiepileptic Drugs Guide: Seizure Causes & MedicationsDocument15 pagesAntiepileptic Drugs Guide: Seizure Causes & MedicationsTod KembleNo ratings yet
- Mast Cell Activation Syndrome - The Functional Medicine ApproachDocument34 pagesMast Cell Activation Syndrome - The Functional Medicine Approach0xcffaaNo ratings yet
- Power Over Suffering: Discovering and Overcoming Hidden Sources of PainFrom EverandPower Over Suffering: Discovering and Overcoming Hidden Sources of PainNo ratings yet
- Introduction To Biology 1Document17 pagesIntroduction To Biology 1Samuel PonceNo ratings yet
- Mindfulness Health Benefits of MeditationDocument6 pagesMindfulness Health Benefits of MeditationDaniel BustamanteNo ratings yet
- Fasting Can Save Your Life and Multiple SclerosisDocument3 pagesFasting Can Save Your Life and Multiple SclerosisJonas Sunshine Callewaert100% (1)
- Emu Sept 2013 Part 2Document28 pagesEmu Sept 2013 Part 2jbrazg84No ratings yet
- Free Somatics: Reawakening The Minds Control of Movement, Flexibility, and Health PDFDocument6 pagesFree Somatics: Reawakening The Minds Control of Movement, Flexibility, and Health PDFRajesh S VNo ratings yet
- Index: 22/8/14 1 Natural Happiness: The Truth About Exercise and DepressionDocument11 pagesIndex: 22/8/14 1 Natural Happiness: The Truth About Exercise and DepressionSiliconNo ratings yet
- Wild Horses - The Stress of CaptivityDocument16 pagesWild Horses - The Stress of CaptivityAmerican Wild Horse PreservationNo ratings yet
- Nikolai Amosov's Anti-Aging GymnasticsDocument3 pagesNikolai Amosov's Anti-Aging Gymnasticsmladen1858948No ratings yet
- NeurologyDocument15 pagesNeurologyed192kbNo ratings yet
- How To Stop Lying To Ourselves: A Call For Self-Awareness: REYNA, Kristinelou Marie N. STEM II - MendeleevDocument15 pagesHow To Stop Lying To Ourselves: A Call For Self-Awareness: REYNA, Kristinelou Marie N. STEM II - MendeleevRosemarie R. ReyesNo ratings yet
- [English] After Watching This, Your Brain Will Not Be the Same _ Lara Boyd _ TEDxVancouver [DownSub.com] (1)Document12 pages[English] After Watching This, Your Brain Will Not Be the Same _ Lara Boyd _ TEDxVancouver [DownSub.com] (1)Maulana Yazid Al AnnuriNo ratings yet
- (General Pathology) - (Wound Healing) by (Dr. Craig)Document24 pages(General Pathology) - (Wound Healing) by (Dr. Craig)NYUCD17No ratings yet
- Special Report: New Treatment For People With Dizziness and Balance Disorders by Dr. Keith LynchDocument9 pagesSpecial Report: New Treatment For People With Dizziness and Balance Disorders by Dr. Keith LynchlynchchiropracticNo ratings yet
- July Fibromyalgia Newsletter 2Document4 pagesJuly Fibromyalgia Newsletter 2JodieLynNo ratings yet
- Research Essay Final Draft - May 1-Avery CentersDocument13 pagesResearch Essay Final Draft - May 1-Avery Centersapi-609271780No ratings yet
- KNH 413 Case Study 4Document12 pagesKNH 413 Case Study 4api-272540385100% (1)
- Fall Newsletter Nov 14Document1 pageFall Newsletter Nov 14NYUCD17No ratings yet
- Reminders:: T Shirt Design Contes T!Document1 pageReminders:: T Shirt Design Contes T!NYUCD17No ratings yet
- Happy: TurkeyDocument8 pagesHappy: TurkeyNYUCD17No ratings yet
- Week of October 26th, 2015 - Class of 2017 NewsletterDocument9 pagesWeek of October 26th, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of September 5Document1 pageWeek of September 5NYUCD17No ratings yet
- Week of November 30th, 2015 - Class of 2017 NewsletterDocument9 pagesWeek of November 30th, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Fall Newsletter #3Document1 pageFall Newsletter #3NYUCD17No ratings yet
- Week of September 12Document1 pageWeek of September 12NYUCD17No ratings yet
- Happy: TurkeyDocument8 pagesHappy: TurkeyNYUCD17No ratings yet
- Week of November 2nd, 2015 - Class of 2017 NewsletterDocument10 pagesWeek of November 2nd, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of November 9th, 2015 - Class of 2017 NewsletterDocument9 pagesWeek of November 9th, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of October 5th, 2015 - Class of 2017 NewsletterDocument8 pagesWeek of October 5th, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of October 19th, 2015 - Class of 2017 NewsletterDocument9 pagesWeek of October 19th, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of September 14, 2015 - Class of 2017 NewsletterDocument7 pagesWeek of September 14, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of September 28, 2015 - Class of 2017 NewsletterDocument8 pagesWeek of September 28, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of September 21st, 2015 - Class of 2017 NewsletterDocument8 pagesWeek of September 21st, 2015 - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of September 8th - Class of 2017 NewsletterDocument8 pagesWeek of September 8th - Class of 2017 NewsletterNYUCD17No ratings yet
- Week of September 8th - Class of 2017 NewsletterDocument8 pagesWeek of September 8th - Class of 2017 NewsletterNYUCD17No ratings yet
- September 2, 2015 MinutesDocument3 pagesSeptember 2, 2015 MinutesNYUCD17No ratings yet
- Week of August 31st - Class of 2017 NewsletterDocument7 pagesWeek of August 31st - Class of 2017 NewsletterNYUCD17No ratings yet
- 10-17-14 MinutesDocument2 pages10-17-14 MinutesNYUCD17No ratings yet
- Week of August 31st - Class of 2017 NewsletterDocument7 pagesWeek of August 31st - Class of 2017 NewsletterNYUCD17No ratings yet
- July 8, 2015 Meeting MinutesDocument2 pagesJuly 8, 2015 Meeting MinutesNYUCD17No ratings yet
- 1-23-15 MinutesDocument2 pages1-23-15 MinutesNYUCD17No ratings yet
- September 2, 2015 MinutesDocument3 pagesSeptember 2, 2015 MinutesNYUCD17No ratings yet
- D2 Council Meeting Minutes: 12:00 - 1:00pm Room 8SDocument3 pagesD2 Council Meeting Minutes: 12:00 - 1:00pm Room 8SNYUCD17No ratings yet
- 2-20-15 MinutesDocument2 pages2-20-15 MinutesNYUCD17No ratings yet
- 1-9-15 MinutesDocument3 pages1-9-15 MinutesNYUCD17No ratings yet
- Effect of Oncoxin Oral Solution in HER2-Overexpressing Breast CancerDocument12 pagesEffect of Oncoxin Oral Solution in HER2-Overexpressing Breast Cancerleonaldy sintesahealthNo ratings yet
- Anil Kumar (Cell Biology) - 1Document11 pagesAnil Kumar (Cell Biology) - 1BISWANATH ROUTNo ratings yet
- FCVM 09 875434Document16 pagesFCVM 09 875434Sebastian WallotNo ratings yet
- Types of Cell Death: Apoptosis, Necrosis and AutophagyDocument10 pagesTypes of Cell Death: Apoptosis, Necrosis and AutophagyShreya NandyNo ratings yet
- Abhrak Bhasma (Biotite Mica Nanoparticles) Induces Cytotoxicity in Adenocarcinoma Human Alveolar Basal Epithelial Cells (A549)Document6 pagesAbhrak Bhasma (Biotite Mica Nanoparticles) Induces Cytotoxicity in Adenocarcinoma Human Alveolar Basal Epithelial Cells (A549)International Journal of Innovative Science and Research Technology100% (1)
- Nobel Prize winning research on programmed cell deathDocument1 pageNobel Prize winning research on programmed cell deathArgo DalapatiNo ratings yet
- Aids 2013Document404 pagesAids 2013kovaron80No ratings yet
- Apoptosis en Tejidos OralesDocument4 pagesApoptosis en Tejidos Oralesangie catalina estupiñan mirandaNo ratings yet
- CellDocument14 pagesCellSyrian AsadNo ratings yet
- Topic 1 and Topic 6Document71 pagesTopic 1 and Topic 6Majd MerieNo ratings yet
- Pentapods Products - Your Delicious Future 2300ADDocument4 pagesPentapods Products - Your Delicious Future 2300ADrutiusNo ratings yet
- S807 Mini Review v4Document37 pagesS807 Mini Review v4Daen de LeonNo ratings yet
- Ehac 604Document13 pagesEhac 604Edward ElBuenoNo ratings yet
- tmpD824 TMPDocument12 pagestmpD824 TMPFrontiersNo ratings yet
- Hypertrophy Hyperplasia Atrophy MetaplasiaDocument20 pagesHypertrophy Hyperplasia Atrophy MetaplasiaYunQingTanNo ratings yet
- 01introduction To PathologyDocument71 pages01introduction To PathologyAishwarya PanchalNo ratings yet
- Cell DeathDocument21 pagesCell DeathBlaNo ratings yet
- Cluster of Differentiation Antigen PosterDocument1 pageCluster of Differentiation Antigen PosterReeti R. Bhat100% (1)
- Thesis Final 1Document40 pagesThesis Final 1John Paolo OcampoNo ratings yet
- Molecular Mechanism of Aloe Barbadensis MillerDocument8 pagesMolecular Mechanism of Aloe Barbadensis MillerSusyana IrianiNo ratings yet
- G0703017291 PDFDocument20 pagesG0703017291 PDFRed DiggerNo ratings yet
- Journal of Clinical and Experimental PharmacologyDocument13 pagesJournal of Clinical and Experimental PharmacologyCodruta Sandi100% (1)
- J Ournal J Ournal: Bioprocessing BioprocessingDocument10 pagesJ Ournal J Ournal: Bioprocessing BioprocessinghakancengizNo ratings yet
- REFERAT - Ppt.pathophysiology of PROM-noviDocument16 pagesREFERAT - Ppt.pathophysiology of PROM-noviFrisma Indah Permatasari100% (1)
- Nanocolloids For Nanomedicine and Drug DeliveryDocument274 pagesNanocolloids For Nanomedicine and Drug Deliveryenock-readersNo ratings yet
- Honey - The Natural Sweetener Become A PR PDFDocument13 pagesHoney - The Natural Sweetener Become A PR PDFLiyeta AlexinaNo ratings yet
- Franco 2017Document12 pagesFranco 2017ReshmaaRajendranNo ratings yet
- Role of Oxidative Stress in Semen Quality of Infertile MenDocument9 pagesRole of Oxidative Stress in Semen Quality of Infertile MenAyadPalaniNo ratings yet





















































![[English] After Watching This, Your Brain Will Not Be the Same _ Lara Boyd _ TEDxVancouver [DownSub.com] (1)](https://imgv2-1-f.scribdassets.com/img/document/720241560/149x198/bd20610543/1712300807?v=1)