Professional Documents
Culture Documents
Fungal Infection
Uploaded by
zeepharmacist100%(1)100% found this document useful (1 vote)
103 views95 pagesPPT
Copyright
© © All Rights Reserved
Available Formats
PPS, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPPT
Copyright:
© All Rights Reserved
Available Formats
Download as PPS, PDF, TXT or read online from Scribd
100%(1)100% found this document useful (1 vote)
103 views95 pagesFungal Infection
Uploaded by
zeepharmacistPPT
Copyright:
© All Rights Reserved
Available Formats
Download as PPS, PDF, TXT or read online from Scribd
You are on page 1of 95
FUNGAL INFECTIONS
Fungal infection Treatment
Most common fungal
infections
1- Candidiasis
It is caused by infection with species of the
genus Candida, predominantly with Candida
albican
Types:
candidiasis Vaginal - a
Presentation: -
1- Itching and irritation in the vaginal area.
1- Candidiasis
2-A burning sensation, especially during intercourse or
while urinating
3-Redness and swelling of the area
4-Vaginal pain and soreness
5-Thick, white, odor-free vaginal discharge with a
cottage cheese appearance
1-Treatment:
1- mild to moderate symptoms and infrequent
episodes of infection
a-Short-course vaginal therapy:
Candidiasis
- one-to-three-day regimen of an antifungal cream,
ointment, tablet or suppository
-The medication of choice is azole antifungal
family:
butoconazole, clotrimazole ,miconazole and
terconazole .
The oil-based nature of these agents in cream
and suppository form can weaken latex condoms
and diaphragms
-Side effects :
A- slight burning or irritation during application
Candidiasis
B- Single-dose oral medication fluconazole (Diflucan) to
be taken by mouth.
2- Treatment for a complicated cases
a- Long-course vaginal therapy includes an azole
medication in the form of a vaginal cream, ointment,
tablet or suppository. The duration of treatment is
usually seven to 14 days.
b- Multidose oral medication instead of vaginal
therapy: two or three doses of fluconazole to be taken
by mouth.
***this therapy isn't recommended for pregnant
women.
Candidiasis
c- Maintenance therapy: For recurrent infections
- It starts after the initial treatment clears infection
-It include:
I-fluconazole tablets taken by mouth once a week for
six months.
II- Clotrimazole as a vaginal tablet (suppository) used
once a week instead of an oral medication
Candidiasis
b- Oropharyngeal candidiasis
Presentation
I-Children and adults
a-Creamy white lesions on tongue, inner cheeks
and on the roof of mouth, gums and tonsils
b-Lesions with a cottage cheese-like appearance
c-Pain
d-Slight bleeding if the lesions are rubbed or
scraped
Candidiasis
e- Cracking and redness at the corners of the mouth
f- Loss of taste
II- Infants and breast-feeding mothers
a- white mouth lesions
b- infants may have trouble feeding or and irritable.
c- Unusually red, sensitive or itchy nipples
d- Unusual pain during nursing or painful nipples
between feedings
Candidiasis
Treatment
A- For infants and nursing mothers
1- A mild topical antifungal medication for baby and
mother.
Example: miconazole
2- If baby uses a pacifier or feeds from a bottle, rinse
nipples
and pacifiers in a solution of equal parts water and
vinegar
daily and allow them to air dry to prevent fungus growth.
3-If mother use a breast pump, rinse any of the
detachable
parts that come in contact with milk in a vinegar and
water
solution.
Candidiasis
B- For healthy adults and children
1-Eating unsweetened yogurt
2-Taking acidophilus capsules or liquid
Yogurt and acidophilus don't destroy the fungus,
but they can help restore the normal bacterial flora
in the body.
3-If infection persists, Topical antifungal medication
can be used
Candidiasis
C- For adults with weakened immune systems
1-Antifungal medication ( lozenges, tablets or a
liquid that can be swish in mouth and then
swallow). Example: nystatin.
2-Amphotericin B that can be used when other
medications aren't effective.
Candidiasis
C- skin lesion
-Presentation:
1-itching
2- Red and growing skin rash. This rash with
discrete
borders
3- Rash usually appear on the skin
folds, genitals, middle of the body,
buttocks, and under the breasts
Candidiasis
-Treatment:
1-Topical azole antifungal: clotrimazole
(Canesten ), econazole (Pevaryl),
ketoconazole
( Nizoral), miconazole (Dactarin )
2-topical terbinafine (Lamisil )
3-Topical nystatin
4-Refractory cases: need systemic treatment with
azole ( fluconazole)
1. Candidiasis
D- Disseminated candidiasis:
This is frequently associated with multiple deep
organ infections or may involve single organ
infection.
2- Dermatophytoses
2-Dermatophytoses
a-tinea capitis : Superficial fungal infection of the
skin of the scalp, eyebrows, and eyelashes,
- Presentation
1-One or more round
patches of scaly skin
2-Scaly, gray or reddened
areas
2- Dermatophytoses
3-Patches have small black dots where the
hair has broken off at the scalp
4-Tender or painful areas on the scalp
- Treatment:
1-Drug of choice : Systemic administration of
Griseofulvin
Recommend dose:
20-25 mg/kg/d for 6-8 weeks
2- Dermatophytoses
2-Topical treatment alone is not recommended
because it is ineffective
3-alternative systemic therapy:
ketoconazole, itraconazole, terbinafine, and
fluconazole (itraconazole and terbinafine are used
most commonly)
4-Selenium sulfide shampoo may reduce the risk
of
spreading the infection
2- Dermatophytoses
b-Tinea coropris ( ringworm infection of the
body )
it is a superficial dermatophyte on the on the
top layer of your skin (skin
regions other than the scalp,
groin, palms, and soles).
Presentation
1- A ring-shaped rash that is
itchy, red, scaly and slightly
raised.
2- Dermatophytoses
2- The rings usually flat scaly area on the skin,
which
may be red and itchy.
- Treatment
1- antifungal lotion or cream
***Topical therapy should be applied to the
lesion and at least 2 cm beyond this area once
or twice a day for at least 2 weeks
2- Dermatophytoses
a- The topical azoles (econazole, ketoconazole,
clotrimazole, miconazole, oxiconazole,
sulconazole, sertaconazole)
b-Luliconazole (Luzu) is an imidazole topical
cream approved by the FDA in November 2013 for
treatment tinea corporis
FDA approves luliconazole for treatment of tinea
corporis
2- Dermatophytoses
FDA recently approved the azole antifungal
luliconazole 1% cream the first topical azole
antifungal
agent with a 1-week (rather than 2-week), once-
daily
treatment regimen for the management of tinea
cruris
and tinea corporis in adults aged 18 years or
older.
Luliconazole was also approved for the treatment
of
interdigital tinea pedis in adults, a regimen that
requires a 2-week treatment period.
2- Dermatophytoses
Allylamines (eg, naftifine, terbinafine) - c
2- Severe cases need systemic therapy
: griseofulvin, Systemic azoles (eg, fluconazole,
itraconazole, ketoconazole)
(athlete's foot ) pedis Tinea - c
It is a dermatophyte infection of
the soles of the feet and the
interdigital spaces
Athlete's foot
2- Dermatophytoses
It occurs most commonly in people whose feet
have become very sweaty while confined within
tight-fitting shoes.
- Presentation
1- Scaly rash that usually causes itching, stinging and
burning.
2- Some cases: blisters or ulcers.
3- Some cases: chronic dryness and scaling on the
soles that extends up the sides of the feet
2- Dermatophytoses
- Treatment:
1- Topical treatment:
a- imidazole:clotrimazole, econazole, miconazole,
ketoconazole and luliconazole) "Luliconazole, an
imidazole topical cream, is applied once daily for 2
weeks "
b- Ciclopirox cream
c- terinafine and naftitine
2- Dermatophytoses
2-oral drugs in severe cases : Itraconazole,
Terbinafine, and fluconazole
3-Topical urea to decrease scaling.
3- Pityriasis versicolor ( Tinea
versicolor)
- Presentation
- Hypopigmented or hyperpigmented macules
and
patches on the chest and the back.
- The color of each lesion varies
from almost white to reddish
brown or fawn colored. A fine,
dustlike scale covers the lesions.
3- Pityriasis versicolor ( Tinea
versicolor)
- Treatment:
1-Clotrimazole cream or lotion
2-Miconazole cream
3- Ketoconazole and Selenium sulfide shampoo
4- Terbinafine (Lamisil) cream or gel
- Instructions
A thin layer of the topical agent applied once or twice
a day on affected area for at least two weeks.
4- Fungal nail infections
(onychomycosis)
Onychomycosis is a fungal infection of the
toenails or
fingernails.
Causes:
1-Most common cause is Dermatophytes ( Tinea
ungum )
2-Candida (yeasts )
3- molds
4- Fungal nail infections
(onychomycosis)
- Presentation:
There are different classifications
of nail fungus depending on type
of fungus and manifestation.
- Common symptoms:
1- A painful and erythematous area
around and underneath the nail
and nail bed
2- Nail thickening, ridging, discoloration, and
occasional nail loss
4- Fungal nail infections
(onychomycosis)
3-Infected nails may separate from the nail bed.
- Treatment :
1-Topical antifungal:
-Topical treatment used for mild to moderate cases
-Agents: Amorolfine (Loceryl), Ciclopirox (
Mycoster) .
2-Oral medication:
Most effective treatments are terbinafine (Lamisil)
and itraconazole (Sporanox)
4- Fungal nail infections
(onychomycosis)
Oral medication recommended for:
1- DM patients
2- If patient has cellulitis or history of cellulitis
3- If patient has pain or discomfort from nail infection
- These Drugs help growing a new nail free of
infection,
slowly replacing the infected portion of nail. these
medications will be taken for six to 12 weeks, and
the end
result of treatment seen after the nail grows back
completely (It may take four months or longer to
eliminate
an infection)
4- Fungal nail infections
(onychomycosis)
To decrease the adverse effects and duration of
oral therapy, topical treatments may be
combined with oral antifungal management
Most common fungal
infection s
5- Aspergillosis
- Commonly affects respiratory tract
- Invasive forms can affect heart, brain and skin
- Drug of choice: Voriconazole
6- Cryptococcosis
- Most common form: cryptococcal meningitis
Treatment : amphotericin B and flucytocine for 2
weeks then followed by fluconazole for 8 weeks or
until culture is positive
Most common fungal
infection s
7-histoplasmosis
Histoplasmosis is an infection caused by
breathing in
spores of a fungus often found in bird and bat
droppings
Antifungal Drugs
I-Azole family:
- M.O.A
-Inhibit sterol synthesis in fungal cell membranes,
this
lead to increase cell permeability and osmotic
pressure
- Drugs:
1-ketoconazole (Nizoral)
- Systemic Ketoconazole
It has slow onset of action and need long duration
of
therapy
1- ketoconazole
- Off-label use :
1- Cushing syndrome :ketoconazole Inhibits
steroidogenes process through inhibiting P450
enzymes includes the first step in cortisol
synthesis, cholesterol side-chain cleavage, and
conversion of 11-deoxycortisol to cortisol
2- Dose Range : 600-800 mg/day PO
1- ketoconazole
Tablets are not recommended as first-line
treatment; should be used only when other
effective antifungal therapy is not effective or
tolerated and the potential benefits are
considered to outweigh the potential of
hepatotoxicity
Usual dose range: -
200-400 mg/day PO
1- ketoconazole
Black Box Warnings
A-Hepatotoxicity has occurred with oral use,
including some fatalities or requiring liver
B-May cause QT prolongation
- Coadministration with dofetilide, quinidine,
pimozide, cisapride, methadone, disopyramide,
dronedarone, and ranolazine is contraindicated
1- ketoconazole
- Ketoconazole can cause elevated plasma
concentrations of these drugs (by CYP3A4
inhibition)
and may prolong QT intervals, sometimes
resulting in
life-threatening ventricular dysrhythmias
such as
torsades de pointes
Most common side effects:
- Nausea,vomiting,diarrhea, constipation, and
abdominal pain
- Rare : hepatotoxicity
Drugs interaction:
Enhance anticoagulant effects of warfarin
1- ketoconazole
Ketoconazole( nizoral) Potentially Fatal
Liver Injury, Risk of Drug Interactions and
Adrenal Gland Problems
July 26, 2013
Audience: Internal Medicine, Infectious Disease.
ISSUE: FDA is taking several actionsrelated to Nizoral
(ketoconazole) oral tablets, including limiting the drugs
use,
warning that it can cause severe liver injuries and adrenal
gland
problems, and advising that it can lead to harmful drug
interactions with other medications. FDA has approved
label
changes and added a new Medication Guide to address
these
safety issues. As a result, Nizoral oral tablets should not be
a
first-line treatment for any fungal infection. Nizoral should
be
used for the treatment of certain fungal infections, known
as
endemic mycoses, only when alternative antifungal
therapies are
not available or tolerated.
1- Ketoconazole
Topical Ketoconazole
- Indication and dose
1-Seborheic Dermatitis
a-Foam: apply to affected area q12hr for 4 wk
b-Cream: apply q12hr for 4 wk or until clear
c-Shampoo: apply twice weekly for 4 wk with at
least 3 days between each shampoo
2-Tinea Versicolor
a-Shampoo: twice weekly for 4 wks allowing 3
days between shampoo
3-Tinea corporis, Tinea Cruris, Tinea pedis
Cream: Apply once daily to cover affected area for
2
weeks (6 weeks for tinea pedis)
1- Ketoconazole
1- Ketoconazole
*** When combined with corticosteroid ,
ketoconazole is useful in treating :
Atopic dermatitis, diaper rash, eczema, and
psoriasis
2-Fluconazole (Diflucan)
-It achieves good penetration into cerebrospinal fluid
so can be used for treating fungal meningitis
- It excreted largely in the urine and can be used for
treating candiduria
Drugs interaction: -
1- Avoid concomitant use with cisapride and
terfenadine
2- It increases level of phenytoin, warfarin,
sulfonylurea and cyclosporine
2-Fluconazole (Diflucan)
- Dose:
1-Oropharyngeal & esophageal candidiasis:
200mg , orally on first day then continue 100mg,
orally , daily
2-Vaginal candidiasis: 150mg as single dose
3-Cryptoccocal meningitis: 400mg, orally on day 1
then 200mg, orally daily
4-Candida UTI: 50-200mg, orally, qday
2-Fluconazole (Diflucan)
- Caution
1- Hepatotoxicity reported with use; use with
caution in patients with hepatic impairment
2- When driving vehicles or operating machines,
it should be taken into account that dizziness or
seizures may occasionally occur
3- Itraconazole (Sporanex)
-Need acid media for optimal absorption
-It is potent CYP4503A4 inhibitor
* Doses
-Onychomycosis:
1-Fingernails: pulse dose regimen: 200mg, twice
daily
for 1 week, repeat the course after 3 week off-time
2-toenails with or without fingernails involvement:
200mg , daily for 12 weeks
3- Itraconazole (Sporanex)
3- Oral candidiasis: oral solution: 100-200 mg/day
for at least 3 weeks, continued for 2 weeks after
symptom resolution
Drugs interaction:
- avoid co-administration with antacids, H2-
blockers
and proton pump inhibitors
- Containdicated with cisapride, dofetilide, ergot
derivatives, lovastatin, simvastatin, quinidine, and
triazolam
3- Itraconazole (Sporanex)
Black Box Warning
Congestive heart failure - 1
Negative inotropic effects reported with IV
administration; reassess therapy if signs or
symptoms of CHF occur during administration
Onychomycosis - 2
Onychomycosis treatment contraindicated in
patients with ventricular dysfunction or history
of heart failure.
3- Itraconazole (Sporanex)
Caution
-Discontinue if liver disease develops, and perform
liver
function tests; readministration discouraged
" Itraconazole is contraindicated for treating
onychomycosis in pregnant or intend on becoming
pregnant "
Most common side effects
- Nausea
4-Voriconazole (Vfend)
- Broad spectrum antifungal and used in life
threatening infection and refractory cases
Dose:
Esophageal candidiasis: 200mg, orally, q12hrs
*** Take oral form 1 hr before or after meal
Most common side effects:
Visual changes (photophobia, color changes,
increased
or decreased visual acuity, or blurred vision occur
in
21%)
4-Voriconazole (Vfend)
Warning:
Avoid intense or prolonged exposure to direct
sunlight; in patients with photosensitivity skin
reactions, squamous cell carcinoma of the skin
and melanoma have been reported during long-
term therapy
5- Posaconazole
- licensed for treatment of invasive cases
unresponsive to conventional therapy
-Food increases oral availability so preferred to take
the dose with full meal
-Most common side effects
nausea & headache
-Drugs interactions:
1-avoid concomitant use with cimetidine, phenytoin,
and rifbutin
5- Posaconazole
2- Coadministration with sirolimus; increases
sirolimus
blood concentrations
Dose
oropharyngeal candidiasis
-oral suspension: 100 mg , PO BID on Day 1, then
100
mg PO qDay for 13 days
-Refractory to itraconazole and/or fluconazole: 400
mg
PO BID; duration based on severity of disease and
response
Newly approved formulation of
Posaconazole
1-FDA has approved a new formulation of posaconazole
(Noxafil,
Merck), The agency approved posaconazole 100-mg delayed-
release
tablets, given as a loading dose of 300 mg (three 100-mg
delayed-
release tablets) twice daily on the first day, followed by a once-
daily
maintenance dose of 300 mg (three 100-mg delayed-release
tablets)
on the second day of therapy. Merck also markets posaconazole
(also
as Noxafil) in a 40 mg/mL oral suspension, which is dosed 3 times
daily.
Posaconazole delayed-release tablets and oral suspension are
indicated
for the prophylaxis of invasive Aspergillus andCandida infections
in
patients aged 13 years and older who are at high risk of
developing
these infections because of being severely immunocompromised
Newly approved formulation of
Posaconazole
2-FDA has approved an intravenous (IV) formulation of the
posaconazole (Noxafil, Merck), according to the company.
Posaconazole injection is indicated in patient at least 18 years
of age, whereas the delayed-release tablets and oral
suspension are
indicated in patients aged 13 years and older. Posaconazole is
indicated for prophylaxis of invasive Aspergillus and Candida
infections in patient who are at high risk of developing these
infections because of being severely immunocompromised,
such as
hematopoietic stem cell transplant recipients with graft-vs-host
disease or those with hematologic malignancies with prolonged
neutropenia from chemotherapy.
6-Clotrimazole (Canestin)
Indication
For fungal skin infection, vaginal candidiasis and otitis
externa
Dose
1-vaginal cream:
a- 1 %: insert 1 applicatorfulvaginal cream at bedtime
for 7 consecutive days
b- 2 %: insert 1 applicatorfulvaginal cream at bedtime
for 3 consecutive days
2-topical cream and solution: apply to affected area twice
daily
for 7 consecutive days
7-Econazole (Pevaryl)
Indication
tinea pedis, Tinea cruris, Tinea corporis, Tinea
versicolor and cutaneous candidiasis
Dose
1-Tinea pedis, cruris, corporis, versicolor: apply cream
to
affected area qDay
2-Cutaneous candidiasis: apply cream to affected area,
BID
Treatment duration
Tinea cruris, corporis, versicolor, cutaneous candidiasis:
for 2
weeks
Tinea pedis: for 4 weeks
8-Miconazole ( Dactarin )
- Used for:
Tinea - 1
a-Tinea cruris, corporis & cutaneous
canidiasis: apply to affected area BID for 2 weeks
b-Tinea versicolor: apply once daily to affected
area
for 2 weeks
c-Tinea pedis: apply BID to affected area for 4
weeks
8-Miconazole ( Dactarin )
2-Vulvovaginal candidiasis
a-Vaginal 2% cream : once daily , before sleep
for 7days.
b-100 mg vaginal suppository once daily , before
sleep for 7days .
c- 200 mg vaginal suppository once daily , before
sleep for 3 day
Polyene Antifungals
Polyene Antifungal
It binds to sterols in fungal cell membrane,
leading to alterations in cell permeability and
cell
death
1-Amphotericin B
- It is most effective antifungal agents in the
treatment of systemic fungal infection,
especially in immunocompromised patients
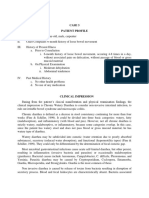
Type Advantage Disadvantage
Conventional cheap Toxic and side effects
common
Lipid formulation Less toxic and side effects
Given when conventional
thearapy contraindicated
because of toxicity especially
nephrotoxicity or when
respone inadequate
Expensive
- Types
1-Amphotericin B
1-Amphotericin B
Precaution
1-infusion-related reaction: fever, chills, vomiting,
nausea, headache, hypotension, dyspnea,
tachypnea (need test dose before start Infusion)
" A test dose is advisable before the first
infusion, the patient should be observed for at
least 30 min after the test dose "
Premedication with acetaminophen,
diphenhydramine,hydrocortisone should be used
for patient who have previously experienced acute
adverse reaction
1-Amphotericin B
2- Nephrotoxicity: need dose adjustment
or drug D/C or change to liposomal form
3-electrolyte abnormalities :
Hypokalemia, hypomagnesemia, and
hypocalcemia
4-CNS effects: headache, peripheral
neuropathy,
malaise, depression, seizure, hallucination
2-Nystatin( Mycostat)
2-nystatin
Indication and Dose
1-Cutaneous or mucocutaneous Candida
infections:
apply 2-3 times daily for 2 weeks
2-vaginal infections: I tab daily at bedtime for 2
weeks
3- GI candidal infection:
a- oropharngeal candidiasis :
Oral suspension: 400,000-600,000 units PO q6hr;
swish
in mouth several minutes and then swallow
Nystatin
b-Intestinal candidiasis
-Oral tablets: 500,000-1,000,000 units q8hr
-Powder: 1/8 to 1/4 teaspoonful in 1/2 cup of water
(500,000-1,000,000 units) PO q8hr
Flucytosine
Flucytocin
M.O.A
It penetrates fungal cells and converted to
fluorouracil, then incorporated to the RNA of
fungal cell. This action leads to defect protein
synthesis
Indications
-Used alone not recommended
-It is used with amphotericin B in synergistic
combination for treatment of severe systemic
fungal
infection ( meningitis, septicemia, endocarditis,
etc)
Flucytosine
Dose
-Candidiasis & Cryptococcus infection : 50-150
mg/kg/dose, orally, q6hr
Caution
Bone marrow depression can occurs
Black Box Warnings
Use extreme caution in patients with renal
impairment
Monitor hematologic, renal, and hepatic function
Review instructions thoroughly before
administration
Griseofulvin
Griseofulfin
M.O.A
-It inhibits fungal cell activity by interfering with
mitotic
spindle structure
- it deposit in keratin precursor cells and is tightly
bound to new keratin, and this increases resistance
to
fungal invasion
-It is mechanism of action similar to colchicines ( it
may
used for gout treatment
Griseofulvin
Indication
Treatment of susceptible tinea infections of
skin,body,hair and nails
Dose
a- Microsize (orally)
1-Tinea corporis, cruris, or capitis: 500 mg/day
2-Tinea pedis: 1000 mg/day
b-Ultramicrosize (orally)
1-Tinea corporis, cruris, or capitis: 375 mg/day
2-Tinea pedis : 250 mg, q8hr
Griseofulvin
Duration of treatment Dependent on
infection site
1-Tinea corporis: 2-4 weeks
2-Tinea capitis: 4-6 weeks; may be up to 8-12
weeks
3-Tinea pedis: 4-8 weeks
"Absorption increased with fatty meals"
Griseofulvin
Most common Side effects
- Headache, lethargy, syncope, confusion,
lethargy,
impaired performance, and skin rash
Severe skin reactions (eg, Stevens-Johnson
syndrome,
toxic epidermal necrolysis) and erythema
multiforme
reported, some resulting in hospitalization or
death;
discontinue if severe skin reaction occurs
Griseofulvin
Drugs interaction
1-it increases the metabolism of warfarin and
lead to decrease prothrombin time
2-Oral contraceptive may increase amenorrhea
or increase breakthrough bleeding
Echinocandins
Echinocandins
1-caspofungin
2-micafungin
3-anidulafungin
-They cause cell wall lysis
-have activity againt candida spp and aspergillus
species
-available as Injection dosage form
Synthetic allylamine
M.O.A
Inhibits squalene monooxygenase and this lead to
interruption of fungal sterol biosynthesis
1- Terbinafine ( Lamisil )
Oral systemic preparation
Indication and dose
1-Onychomycosis
250 mg (1 tablet) PO daily for 6 weeks (fingernail)
or
12 weeks (toenail)
Terbinafine ( Lamisil )
2- Tinea pedis ( off-label use ) 250 mg/day PO for
2- 6 weeks
3- Tinea corporis and tinea crusis 250 mg/day PO
for 2-4 weeks
Common side effects
1-headache
2-taste disturbances
3-visual disturbances
4-skin rash
Terbinafine ( Lamisil )
Topical preparation
Indication and dose
1- Tinea Pedis
Apply to affected area BID until significant
clinical improvement (no more than 4 weeks)
2-Tinea corporis and cruris
Apply daily for 1 week (no more than 4 weeks)
Terbinafine cutaneous solution
( Lamisil once)
Indication
It is a single dose treatment for tinea pedis
Side effect
burning, dryness, pruritis, rash, irritation
Terbinafine cutaneous solution
( Lamisil once)
- How to use: apply to both feet, even if
signs
are visible only on one foot. When applied
to
the feet, the medication dries quickly to a
colourless film. The drug delivers into the
skin
where it lasts for a number of days to kill the
fungus .after applying the drug, patient must
not wash or splash feet for 24 hours
Naftifine ( Exodril)
2-Naftifine ( Exodril)
Indication & Dose
1- 1% cream treatment
-Used for treatmen of tinea pedis, tinea cruris,
and tinea corporis
-apply BID to the affected areas plus a 0.5-inch
margin of healthy surrounding skin for 4 weeks
Naftifine ( Exodril)
2- 2% cream or gel
-Used for treatment of interdigital tinea pedis,
tinea cruris, and tinea corporis
-Apply daily to the affected areas plus a 0.5-inch
margin of healthy surrounding skin for 2 weeks
Caution
Avoid use of occlusive dressings
Amorolfine ( Loceryl)
Amorolfine
Indication
Topical treatment of nail infections caused by fungi
(onychomycosis)
Dose
Apply to affected toenails or fingernails once or twice
weekly
Duration
- Fingernails: 6 months - Toenails: 9-12
months
Ciclopirox ( Mycoster)
Ciclopirox
M.O.A
Synthetic benzylamine
It inhibits intermediary in synthesis of ergosterol, an
essential component of fungal cell membranes
Indication and dose
1-Mild to moderate onychomycosis of fingernails &
toenails:
1- topical solution: apply over entire nail plate daily
before sleep or 8 hours before washing to all affected
nails
Ciclopirox ( Mycoster)
2-Tinea pedis, Tinea corporis, Tinea cruris, Tinea
vesicolor, and cutaneous candidiasis :
Cream and suspension: apply BID; gently
massage into affected areas; if no
improvement after 4 weeks re-evaluate
diagnosis
3-Seborrheic dermatitis:
-Gel: Apply BID; gently massage into affected
areas; if no improvement after 4 weeks re-
evaluate diagnosis
Tolnaftate
Tolnaftate
M.O.A
distort the hyphae and stunt mycelial growth in
susceptible fungi
Indication & Dose
Superficial fungal infection
apply BID for 2-3 weeks
Clioquinol
Clioquinol
It is used for fungal skin infection : apply two to
four times a day up to 4 weeks
Newly approved drugs:
1-Luliconazole ( Luzu)
- FDA has approved the azole antifungal
luliconazole
1% cream to treat fungal infections
- Luliconazole 1% cream is indicated for the
topical
treatment of interdigital tinea pedis (athlete's foot),
tinea cruris and tinea corporis , in adults aged 18
years
and older.
1-Luliconazole ( Luzu)
It is the first topical azole antifungal agent
approved to treat tinea cruris and tinea corporis
with a 1-week, once-daily treatment regimen. All
other currently approved treatments require 2
weeks of treatment. For interdigital tinea pedis,
the treatment period is 2 weeks, once daily
2- Efinaconazole
Efinaconazole
- It is used for the topical treatment of
onychomycosis.
- Efinaconazole is an inhibitor of sterol 14-
demethylase and is more effective in vitro than
terbinafine, itraconazole, ciclopirox and amorolfine
against dermatophytes, yeasts and non-
dermatophyte
molds.
- The mean mycological cure rate for
efinaconazole is
similar to the oral antifungal itraconazole and
exceeds
the efficacy of topical ciclopirox
- efinaconazole 10% nail solution is an effective
topical monotherapy for distal and lateral
subungual onychomycosis (<65% nail
involvement, excluding the matrix) that shows
further potential use as an adjunct to oral and
device-based therapies.
2- Efinaconazole
Pregnancy category and breast
feeding
Breast feeding Pregnancy category Drug
Enters breast milk C Ketoconazole
use caution as topical,
vaginal not known
C Miconazole
Not recommended C Fluconazole
Enter breast milk so
weigh risk against
benefits
C Itraconazole
not known if excreted in
breast milk, weigh
risk/benefit
D Voriconazole
unknown; weigh
risk/benefit
C Posaconazole
Pregnancy category and
breast feeding
Breast feeding Pregnancy Drug
use with caution B Clotrimazole
-Conventional:
contraindicated
-liposomal: not
recommended
B Amphotericin B
1-systemicNot known if
excreted in breast milk; use
caution
2-Topical: no studies
3-vaginal: Poorly
distributed in breast milk
1-systemic: c
2-topical: B
3-vaginal:A
Nystatin
not recommended c Flucytocin
Avoid use X Griseofulvin
Avoid use B terbinafine
Pregnancy category and
breast feeding
Breast feeding Pregnancy Drug
avoid unless
potential benefit
outweigh risk
avoid unless
potential benefit
outweigh risk
Amorolfin
not known if
distributed in breast
milk
B
Ciclopirox
Use caution B
Naftifine
Unknown C
Tolnaftate
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Title: Cutting Surfaces To Cut UproarDocument1 pageTitle: Cutting Surfaces To Cut UproarzeepharmacistNo ratings yet
- Biotransformation of DrugsDocument36 pagesBiotransformation of DrugszeepharmacistNo ratings yet
- Training Work Sheet For TraineesDocument2 pagesTraining Work Sheet For TraineeszeepharmacistNo ratings yet
- Multi Topic EssayDocument3 pagesMulti Topic Essayzeepharmacist100% (4)
- Multi Topic EssayDocument3 pagesMulti Topic Essayzeepharmacist100% (4)
- IELTS Listening Practice Test Answer SheetDocument2 pagesIELTS Listening Practice Test Answer SheetzeepharmacistNo ratings yet
- XPEBC Anatomy Physiology Pathophysiology QuestionsxDocument12 pagesXPEBC Anatomy Physiology Pathophysiology Questionsxzeepharmacist100% (1)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nutrients: The Antiviral, Anti-Inflammatory E Medicinal Herbs and Mushrooms and Sars-Cov-2 InfectionDocument13 pagesNutrients: The Antiviral, Anti-Inflammatory E Medicinal Herbs and Mushrooms and Sars-Cov-2 Infectionmmbire@gmail.comNo ratings yet
- 1908 Juvenile Dermatomyositis - Advances in Clinical Presentation, Myositis Specifc Antibodies and TreatmentDocument13 pages1908 Juvenile Dermatomyositis - Advances in Clinical Presentation, Myositis Specifc Antibodies and TreatmentFlorian LamblinNo ratings yet
- Prescribing Information: (Methoxsalen, USP)Document9 pagesPrescribing Information: (Methoxsalen, USP)Jeliny Bintan MaisuriNo ratings yet
- Formula For Calculating The IV Flow RateDocument16 pagesFormula For Calculating The IV Flow Rateblythe RiveroNo ratings yet
- Neurocysticercosis An Update On Diagnosis,.10Document9 pagesNeurocysticercosis An Update On Diagnosis,.10RENZO ALEJANDRO ACUÑA FLORESNo ratings yet
- Para PBL CompleteDocument9 pagesPara PBL CompleteMerill Harrelson LibanNo ratings yet
- 3, Annex-3, Tables-13 A and B, 2018-19Document6 pages3, Annex-3, Tables-13 A and B, 2018-19Sumit BiswasNo ratings yet
- Norovirus - CDCDocument1 pageNorovirus - CDCDibyajyoti RabhaNo ratings yet
- Republic of The Philippines DOH Regional Office XIII Butuan City Midwife Ii Narrative ReportDocument1 pageRepublic of The Philippines DOH Regional Office XIII Butuan City Midwife Ii Narrative ReportLAURENCE ALBIOSNo ratings yet
- Cda Revalida Caregiving NC 2020Document7 pagesCda Revalida Caregiving NC 2020Rowena Lalongisip De LeonNo ratings yet
- Anaphy and Patho of AppendicitisDocument3 pagesAnaphy and Patho of AppendicitisArt Christian RamosNo ratings yet
- Berberine Containing PlantsDocument30 pagesBerberine Containing PlantsmubeenNo ratings yet
- Reptile Nutritional DiseasesDocument9 pagesReptile Nutritional DiseasesDiah PiastutiNo ratings yet
- Sepsis 23 Dic. 2021Document2 pagesSepsis 23 Dic. 2021Zonia GuzmanNo ratings yet
- Pamphlet InsideDocument1 pagePamphlet Insideapi-2408549370% (1)
- Medical IdiomsDocument14 pagesMedical IdiomsLeidy RodriguezNo ratings yet
- Seamless Care - DR SH LeungDocument38 pagesSeamless Care - DR SH Leungmalaysianhospicecouncil6240No ratings yet
- Tepid Sponging: Preparation of ArticlesDocument3 pagesTepid Sponging: Preparation of ArticlesNeelofur Ibran Ali100% (4)
- Bino - Lec - Midterm Exam - Yellow - PadDocument11 pagesBino - Lec - Midterm Exam - Yellow - PadDanielle SangalangNo ratings yet
- Crohn's DiseaseDocument46 pagesCrohn's Diseaseuttarasingh100% (3)
- 2017 PTMAZEiftDocument4 pages2017 PTMAZEiftAnindya DeNo ratings yet
- ScenarioDocument3 pagesScenarioporo rowNo ratings yet
- Exam ReviewDocument4 pagesExam ReviewMya Thomas100% (1)
- PenileDocument2 pagesPenileAREOLA Vera SophiaNo ratings yet
- Tachdjian's Pediatric Orthopaedics v.4Document660 pagesTachdjian's Pediatric Orthopaedics v.4Leonardo Garay QuinteroNo ratings yet
- Pediatric Respiratory EmergencyDocument35 pagesPediatric Respiratory EmergencyImran FaisalNo ratings yet
- ESOFAGITISDocument13 pagesESOFAGITISliliana delgadoNo ratings yet
- Aetiology, Pathology and Management of Enterocutaneous FistulaDocument34 pagesAetiology, Pathology and Management of Enterocutaneous Fistulabashiruaminu100% (4)
- Guided ImageryDocument4 pagesGuided ImageryDita Citra AndiniNo ratings yet
- Written Report "Osteoarthritis": Catanduanes State University College of Health Sciences Department of NursingDocument4 pagesWritten Report "Osteoarthritis": Catanduanes State University College of Health Sciences Department of NursingMezil NazarenoNo ratings yet