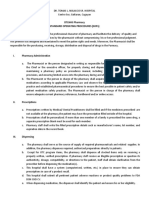
Professional Documents
Culture Documents
Attention Deficit Hyperactivity Disorder and Enuresis in Children and Adolescents
Uploaded by
Hendrikus Surya Adhi Putra0 ratings0% found this document useful (0 votes)
152 views8 pageseneurosis nocturnal
Original Title
eneurosis
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documenteneurosis nocturnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
152 views8 pagesAttention Deficit Hyperactivity Disorder and Enuresis in Children and Adolescents
Uploaded by
Hendrikus Surya Adhi Putraeneurosis nocturnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 8
Attention deficit hyperactivity disorder (ADHD), and
enuresis are among the most common psychoneurotic dis-
orders in children and adolescents. Enuresis is a patholog-
ical state associated with the lack of a developed skill in
controlling the urinary bladder, resulting in repeated
episodes of involuntary micturition during sleep or waking.
The International Classification of Disease 10th Edition
(ICD-10) [6] assigns this condition to the category of emo-
tional and behavioral disorders with onset in childhood and
adolescence. Under rubric F98.0, enuresis of non-organic
origin is defined as a disorder characterized by involuntary
passage of urine during the day and/or night, inappropriate
for age and mental development. The following diagnostic
criteria for enuresis are defined in the ICD-10: the chrono-
logical and mental ages of the child must be at least five
years; the frequency of episodes of micturition must be at
least two per month in children aged less than seven years
and at least one per month in children of seven years and
older; enuresis must not be a direct consequence of anatom-
ical anomalies of the urinary tract, epileptic seizures, neu-
rological disorders, or any other non-psychiatric disease;
involuntary micturition must be seen for at least three
months in a row.
Depending on age, enuresis is divided into primary and
secondary [1, 2, 4, 18]. Children with primary (persistent)
enuresis (8090% of cases) have never been able to control
micturition or have been able to control it for no more than
36 months. Secondary (acquired, regressive) enuresis
(1020% of cases) occurs when a prolonged period of con-
trol of micturition, lasting from several months (at least 36
months) to several years, is followed by recurrence of uri-
nary incontinence. The timing of episodes of micturition
Neuroscience and Behavioral Physiology, Vol. 41, No. 5, June, 2011
Attention Deficit Hyperactivity Disorder and Enuresis
in Children and Adolescents
N. N. Zavadenko,
1
N. M. Kolobova,
2
and N. Yu. Suvorinova
1
0097-0549/11/4105-0525
2011 Springer Science+Business Media, Inc.
525
Translated from Zhurnal Nevrologii i Psikhiatrii imeni S. S. Korsakova, Vol. 110, No. 2, pp. 5055, February,
2010.
The incidences of comorbid disorders and the status of neuropsychological executive functions were eval-
uated in two groups of patients aged 514 years: patients with attention deficit hyperactivity disorder
(ADHD) in combination with enuresis (53 patients) and ADHD without enuresis (71 patients). Most cases
of enuresis among patients of group 1 (50 of 53) had primary nocturnal enuresis. This group showed a sig-
nificant increase in the total number of cases of comorbidity with such disorders as oppositional-defiant
behavioral disorder, anxiety disorders, ticks, and encopresis, seen in 77.7% of cases as compared with
60.6% in group 2. The presence of enuresis in patients with ADHD was associated with a significant
increase in the incidence of anxiety disorders (54.7% as compared with 39.4%). In addition, at age 59
years, patients with ADHD with enuresis had a tendency to a higher frequency of oppositional-defiant
behavioral disorder and encopresis; those aged 1014 years showed an increase in the proportion with
obsessive-compulsive disorder and tics as compared with patients with ADHD without enuresis.
Assessment of measures of executive functions using the Wisconsin card sorting test revealed no differ-
ences between patients of the two groups.
KEY WORDS: attention deficit hyperactivity disorder (ADHD), enuresis, comorbidity, executive functions, treatment.
1
Department of Neurology and Neurosurgery, Faculty of
Pediatrics, Russian State Medical University, Moscow;
e-mail: zavadenko@mail.ru.
2
Morozov Pediatric City Clinical Hospital, Department of
Health, Moscow.
discriminate nocturnal enuresis, i.e., urine is passed invol-
untarily only at night (85% of cases), and daytime enuresis,
in which involuntary micturition occurs during the daytime
while the child is awake (in 5% of cases), and mixed-type
enuresis (daytime plus nocturnal), which is seen in about
10% of cases.
The main pathogenetic mechanisms of enuresis include
delay in maturation of the central nervous system (CNS),
impairments to activation reactions during sleep, inherited
mechanisms, impairments of the rhythm of antidiuretic hor-
mone secretion, the actions of psychological factors and
stress, and the effects of urological lesions [1, 2, 4]. The
clinical interaction between enuresis and other psychoneu-
rological disorders has been studied in relation to delays in
the rates of CNS maturation preventing the timely forma-
tion of voluntary control of micturition. The combination of
enuresis and externalized disorders, i.e., ADHD and behav-
ioral impairments, is quite widespread [9, 18]. Published
data indicate that the incidence of nocturnal enuresis is par-
ticularly high among children with ADHD, amounting to
2132%, which is 1.86 times higher than among their con-
temporaries [9, 13, 15]. Thus, investigation of 140 children
with ADHD detected nocturnal enuresis in 25% of cases as
compared with 10.8% in a group of 120 contemporaries [9].
A high incidence of nocturnal enuresis was observed in a
group of 204 children (170 boys and 34 girls) with ADHD
aged 513 years studied by ourselves: 14% among boys and
12% among girls [3]. Most patients with ADHD were diag-
nosed with primary nocturnal enuresis. The highest comor-
bidity of nocturnal enuresis with ADHD, 40%, was report-
ed by Bayens et al. [7], and may be associated with the
characteristics of this cohort of patients. In accordance with
the diagnostic criteria of the DSM-IV [10], 15.0% of
patients had the combined form of ADHD, while 22.5% had
ADHD with predominance of impairment of attention and
2.5% had ADHD with predominance of hyperactivity and
impulsivity. Dynamic observations of patients with ADHD
for two years showed that enuresis persisted in 72.5% [8],
which may indicate the stability of enuresis in ADHD and
its relative resistance to treatment. However, there have
been few studies of comorbidity in enuresis and the results
are contradictory. This particularly applies to the combina-
tion of enuresis with internalized disorders.
The aim of the present work was to identify the inci-
dences of comorbid disorders and the status of a number of
neuropsychological functions
1
in two groups of patients
patients with ADHD combined with enuresis and patients
with ADHD without enuresis.
MATERIALS AND METHODS
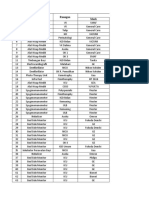
Group 1 (53 patients) included children with ADHD
and enuresis; group 2 (71 patients) included children with
ADHD without enuresis. Patients were aged from five to 14
years. The distribution of patients in terms of age and sex is
shown in Table 1. All patients were observed and investi-
gated in out-patient conditions.
The diagnosis of ADHD was established in accordance
with ICD-10 criteria [6] for hyperkinetic disorder (rubric
F90), which are similar to the DSM-IV criteria for the com-
bined form of ADHD [10]. Diagnoses of enuresis were also
made in accordance with ICD-10 criteria.
Comorbid disorders were identified using the full ver-
sion of the Diagnostic Questionnaire for the Detection of
Affective Disorders and Schizophrenia Present and
Lifetime (D-QEDS-PP) in children and adolescents, which
is a version adapted to the Russian language [5] of the orig-
inal methodology of the Kiddie-Schedule for Affective
Zavadenko, Kolobova, and Suvorinova 526
TABLE 1. Distribution of Study Patients by Age and Gender
Study groups
Number of patients
ADHD combined with enuresis ADHD without enuresis
Age 59 years 32 45
boys 20 36
girls 12 9
Age 1014 years 21 26
boys 19 21
girls 2 5
All patients 53 71
1
In the Russian literature, executive functions are often designat-
ed regulatory or programming functions or the control of mental
processes.
Disorders and Schizophrenia (Present and Lifetime Version)
[12]. The D-QEDS-PP is designed for the diagnosis of
ongoing and previous behavioral, affective, and psychotic
disorders, as well as enuresis, encopresis, nervous anorexia,
bulimia, disorders manifest as tics, alcohol and drug abuse,
post-traumatic stress disorder, and adaptation disorders.
Investigations included conversations with one or both par-
ents and the children themselves, supplemented with
reports from all available sources of information (school,
developmental charts, medical histories, etc.).
In neuropsychological investigation of patients, the
focus was placed on measures characterizing so-called
executive functions (EF), which are supported by the pre-
frontal areas of the frontal lobes of the brain. This was
addressed using a computerized version of the Wisconsin
card sorting test [11]. This was presented to patients aged
over 6.5 years. A row of four cards bearing images differing
in terms of three features, i.e., figure shape (triangles, stars,
crosses, circles), color (red, yellow, green, blue), and num-
ber (from one to four), was presented in the upper part of a
monitor screen in front of the patient. A total of 128 new
cards were presented during the investigation, each of
which had similarity to one of the four imaged in the upper
row. The subject had to sort the new cards, identifying by
themselves the feature by which they corresponded to the
images in the upper row. Each new card was moved to a
position beneath the card sharing this characteristic. Studies
included at least six series of tasks, each of which was com-
pleted after ten correct responses in a row. The total number
of responses could not exceed 128, so fewer than six series
was sufficient for a significant number of errors. The nature
of the task (i.e., the card selection principle) changed with-
out warning the subject after ten correct responses in a row
and the experimenter gave no advice, merely reporting the
correctness or incorrectness of responses. The main mea-
sures of the performance of the Wisconsin test are the num-
ber of series performed, the total number of errors, the pro-
portion of perseverative errors (%), the proportion of
non-perseverative errors (%), and the proportion of respons-
es at the conceptual level (%). Many children with ADHD
show reductions in these measures as compared with
healthy contemporaries.
RESULTS
Most (50 of 53) patients with ADHD in group 1 had
primary nocturnal enuresis; only one (a 12-year-old girl)
had secondary nocturnal enuresis and two (a six-year-old
girl and an 11-year-old boy) had primary daytime enuresis.
Comorbid disorders in children and adolescents with
ADHD of both groups consisted of oppositional-defiant
behavioral disorder and various forms of anxiety disorders,
as well as tics and encopresis (Table 2). Other impairments
which published data indicate can accompany ADHD,
including asocial behavioral disorder and mood disorder,
were not seen in our patients. However, attention is drawn
to the fact that among patients with ADHD and enuresis,
comorbid disorders were seen more frequently (77.4% of
cases), while among patients with ADHD without enuresis,
they were significantly less frequent (60.6%, p < 0.05). This
was mainly because group 1 showed a much higher inci-
dence of anxiety disorders than group 2 (54.7% vs. 39.4%,
p < 0.05), among which generalized anxiety disorder
(20.8% vs. 12.7%) and obsessive-compulsive disorder
(30.2% vs. 22.5%) were particularly frequent. Rarer cases,
with essentially similar frequencies in both groups of
patients, showed specific (simple) and social phobias.
Furthermore, some children of both groups were diagnosed
with separation-associated anxiety disorder and one boy
from group 1 had post-traumatic stress disorder.
Although the incidences of oppositional-defiant
behavioral disorder, tics, and encopresis among patients
with ADHD combined with enuresis and ADHD without
enuresis (Table 2) were similar, they were different in dif-
ferent age subgroups; this also applied to the incidence of
anxiety disorders. Figure 1 shows results obtained from
assessment of these states in age subgroups 59 years and
1014 years, which may reflect the behavioral characteris-
tics of patients with ADHD and enuresis at different age
periods. Thus, at 59 years, patients with ADHD and enure-
sis had higher incidences not only of anxiety disorders, but
also oppositional-defiant behavioral disorder than patients
with ADHD without enuresis (34.4% vs. 26.7%), and this
also applied to encopresis (9.4% vs. 4.4%). At age 1014
years, patients with ADHD and enuresis had markedly
higher incidences of obsessive-compulsive disorder (42.9%
vs. 23.1%) and tics (14.3% vs. 7.0%), while the incidence
of oppositional-defiant behavioral disorder, although
remaining at a quite high level, was lower (38.1%) than in
contemporaries with ADHD without enuresis (53.8%).
According to current concepts, the cause of the main
manifestations of ADHD consists of functional distur-
bances to the frontal lobes of the brain, particularly the pre-
frontal region, and the signs of ADHD are analyzed from
the point of view of inadequately formed EF. Thus, the
diagnosis of comorbid diseases in the present study was
supplemented by comparative evaluation of the state of EF
in patients of the two groups using the Wilcoxon card sort-
ing test, which is an informative method for assessing
abstract thought in patients aged more than 6.5 years, which
also addresses flexibility in solving cognitive tasks, the abil-
ity to switch attention, the capacity of working memory, and
the ability to maintain consistent responses. The test results
from the two groups of patients are presented in Table 3.
It follows from these results that in both age sub-
groups, the Wilcoxon test results in patients with ADHD
with enuresis and ADHD without enuresis were similar,
with no statistically significant differences between them.
Thus, the presence of enuresis was not accompanied by
Attention Deficit Hyperactivity Disorder and Enuresis in Children and Adolescents 527
additional deterioration in the status of EF in patients with
ADHD. Overall, test results showed the increases in the
proportions of erroneous responses typical for ADHD
patients, with both perseverative and non-perseverative
errors, along with a simultaneous decrease in the proportion
of correct responses; some improvement in these measures
in patients aged 1014 as compared with those aged 69
years was also quite consistently seen, though most patients
of both age subgroups produced lower results than expect-
ed on the basis of age norms.
DISCUSSION
The studies reported here showed that ADHD patients
aged 514 years were characterized by an increased inci-
dence of comorbidity for disorders such as oppositional-
defiant behavioral disorder, anxiety disorders, tics, and
encopresis. Among patients with ADHD without enuresis,
the total proportion of cases with comorbidity for these
same conditions was significantly lower, at 60.6%, com-
pared with 77.7% in group 1. The presence of enuresis in
ADHD was associated with an increased incidence of anx-
iety disorders, particularly because of generalized anxiety
and obsessive-compulsive disorders.
The two age subgroups of patients with ADHD com-
bined with enuresis showed the following characteristics.
At age 59 years, there was a tendency to higher incidences
of oppositional-defiant behavioral disorder and encopresis,
while at 1014 years of age there were minor increases in
the incidences of obsessive-compulsive disorder and tics
as compared with patients with ADHD without enuresis
(the difference was not statistically significant).
As the absolute majority of cases of enuresis among
the ADHD study patients had primary nocturnal enuresis
(50 of 53), these data can be applied to the combination of
ADHD with primary nocturnal enuresis. Delayed matura-
tion of the CNS plays a significant role among the main
mechanisms of the pathogenesis of both ADHD and prima-
ry enuresis. In particular, in the case of ADHD, this applies
to delayed maturation of the prefrontal cortex of the frontal
lobes, while disturbances of the rhythm of antidiuretic hor-
Zavadenko, Kolobova, and Suvorinova 528
TABLE 3. Results from the Wisconsin Card Sorting Test in Patients with ADHD (M m)
Parameter, %
Patients aged 69 years Patients aged 1014 years
ADHD combined with
enuresis (n = 16)
ADHD without enuresis
(n = 19)
ADHD combined with
enuresis (n = 19)
ADHD without enuresis
(n = 15)
Erroneous responses 31.7 3.5 33.0 3.0 21.2 2.4 22.5 3.0
Perseverant errors 15.1 1.9 17.4 2.1 10.3 0.8 9.3 1.4
Non-perseverative errors 16.4 2.1 15.6 1.3 11.0 1.7 12.9 2.0
Responses at the conceptual level 59.8 5.2 58.7 4.0 73.6 3.5 71.3 4.6
TABLE 2. Incidence of Comorbid Disorders in the Two Groups of Patients
Comorbid disorders ADHD combined with enuresis, % ADHD without enuresis, % p
Any comorbid disorder (one or more) 77.4 60.6 <0.05
Oppositional-defiant behavioral disorder 35.8 36.6
Anxiety disorders 54.7 39.4 <0.05
generalized anxiety disorder 20.8 12.7
simple phobias 5.7 11.3
social phobias 5.7 4.2
obsessive-compulsive disorder 30.2 22.5
Tics 9.4 7.0
Encopresis 5.7 4.2
Note. Total values for comorbid disorders were greater than 100% because some patients had two or more concomitant disorders.
mone (ADH) secretion are among the important patho-
genetic mechanisms of enuresis.
The circadian ADH secretion rhythm produces diurnal
variations in the volume of urine produced. Thus, in normal
subjects, less urine is produced at night than during the day,
because nocturnal ADH secretion is greater. In children
ADH secretion levels change with maturation and reach
values close to those in adults at about 12 years of age.
Delays in CNS maturation can produce impairments to the
circadian ADH secretion rhythm, including decreases in its
level during the night, which is clinically apparent in chil-
dren with nocturnal enuresis [1, 4]. Impairments to the reg-
ulation of ADH in primary nocturnal enuresis may be genet-
ically determined.
As many patients with primary nocturnal enuresis have
a deficiency of ADH secretion in the nocturnal hours,
desmopressin (Minirin) has received wide use in the treat-
ment of nocturnal enuresis, this being a synthetic peptide
analog of ADH [1, 4]. The antidiuretic effect of this agent is
greater than that of the natural hormone and its actions on
vessel walls and the smooth musculature of the internal
organs are minimized, so it does not produce significant
side effects. The mechanism of action of desmopressin in
enuresis consists of a decrease in nocturnal urine formation
in the renal canaliculi to a volume not exceeding the func-
tional capacity of the urinary bladder in children, allowing
retention until waking in the morning. The clinical efficacy
of desmopressin in the treatment of enuresis has been sup-
ported in a series of double-blind, placebo-controlled trials;
positive responses to treatment have been obtained in
5080% patients in different studies, though there is the
possible complication of recurrences after withdrawal of the
medication, such that treatment should be adequately pro-
longed [1, 18]. This agent is recommended as a first-line
therapy in patients with isolated primary nocturnal enuresis.
We have published clinical data on the value of its use in
patients with ADHD combined with enuresis [2], though
this question requires further study.
Another approach to the drug-based treatment of pri-
mary enuresis, which has been used for many years and is
regarded by some authors as the method of choice, is based
on the tricyclic antidepressants Melipramine (imipramine)
and amitriptyline. The precise mechanism of action of these
agents in enuresis is unclear, though it is believed not to be
associated with the antidepressant actions or with influ-
ences on the arousal systems of the brain or sleep.
Attention Deficit Hyperactivity Disorder and Enuresis in Children and Adolescents 529
Fig. 1. Incidences (%) of various comorbid disorders in the two subgroups of ADHD patients those aged 59 years (a) and those
aged 1014 years (b); 1) ADHD with enuresis; 2) without enuresis. ARVI = acute respiratory viral infections; AD = anxiety dis-
orders; GAD = generalized anxiety disorder; OCD = obsessive-compulsive disorder.
Melipramine has been shown to decrease the excitability of
the urinary bladder by means of its peripheral anticholiner-
gic and spasmolytic actions. The treatment of enuresis with
Melipramine is preferentially restricted to older children
and adolescents in whom desmopressin has failed to produce
the desired outcome. Positive responses to Melipramine are
obtained in about 40% of patients with enuresis [18].
However, the use of tricyclic antidepressants, especially for
prolonged periods, is associated with a number of risks to
health because of the side effects of these agents. In partic-
ular, the anticholinergic effects of tricyclic antidepressants
can be undesirable, inducing atonia of the urinary bladder
and urinary retention. Furthermore, other serious side
effects of thee agents are known, including cardiotoxicity,
suppression of hematopoiesis, and exacerbation of bron-
chial asthma.
Returning to the results of the present study, it should
be emphasized that enuresis is not an isolated condition in
a quite large proportion of children, such that the approach
to its treatment should be addressed in the context of the
detection and correction of all disorders and abnormalities
present in the affected child. In this regard, there is particu-
lar interest in the comorbidity of enuresis with ADHD, as
mutually exacerbating influences from these two conditions
cannot be excluded. It should be noted that the cause of the
high incidence of cases in which ADHD is associated with
enuresis is ultimately unclear, though it may be explained
by both the high incidence of each of these conditions in the
child population and the similarities in their pathogenetic
mechanisms. The leading role in the pathogenesis of both
ADHD and enuresis is currently believed to be a common
neurobiological factor, particularly delayed maturation of
the CNS and inherited mechanisms. Although the inheri-
tance of ADHD and enuresis appear not to be mediated by
the same genes, the molecular genetic basis of the comor-
bidity of ADHD and enuresis requires specific studies [18].
Cases of comorbidity of several conditions often gen-
erate problems in determining therapeutic strategies. In
these situations, the physician generally asks a series of
questions: which of the disorders is the more severe,
whether the conditions should be treated sequentially or
simultaneously, whether monotherapy should be used with
sequential changes in treatment agents when they are not
effective or whether combined treatment should be provid-
ed, etc. Considering the high incidence of the association of
enuresis and ADHD, the development of appropriate treat-
ment methods for such patients is of great scientific and
practical relevance.
One of the most promising directions in this area is the
use of the new drug atomoxetine hydrochloride (Strattera).
This is the only agent currently available in Russia which
was specifically developed and approved for the treatment
of ADHD. The high efficacy of atomoxetine in relation to a
wide spectrum of the abnormalities seen in ADHD has
received repeated support in controlled clinical trials and is
beyond doubt. In many of these studies, children with con-
comitant enuresis showed significant regression the signs of
both ADHD and enuresis [14, 16, 19]. Unfortunately, there
is as yet insufficient evidence of the efficacy of atomoxetine
in the treatment of enuresis without ADHD for the recom-
mendations for the use of atomoxetine to be widened to
include enuresis.
At the same time, children and adolescents with simul-
taneous ADHD and enuresis should start treatment using
atomoxetine monotherapy, as the stress in selecting treat-
ment should be on the timely and adequate correction of the
signs of ADHD, as the long-term consequences of ADHD
are more severe than those of enuresis. Furthermore, when
treating these patients with atomoxetine, the physician
expects regression of the signs of both ADHD and enuresis.
The grounds for this are provided by results of recent stud-
ies [16, 17], in which double-blind, randomized, placebo-
controlled trials demonstrated that atomoxetine treatment
led to decreases in the frequency or the cessation of noctur-
nal micturition in patients with enuresis both combined with
ADHD and without ADHD. In one of these studies, Sumner
et al. [17] noted the efficacy of atomoxetine in the treatment
of nocturnal enuresis in children and adolescents aged 618
years in out-patient conditions. Atomoxetine at a dose of 1.5
mg/kg/day was used in 42 children (of which 10 had ADHD)
for 12 weeks, while 41 children (17 with ADHD) received
placebo; treatment results were evaluated in terms of the
number of dry nights per week. Atomoxetine treatment of
children with enuresis significantly increased the number of
dry nights per week. A total of 15 atomoxetine-treated
children showed increases in the number of dry nights by
factors of two or more, while there were only six such
patients in the placebo group. The mean increase in the num-
ber of dry nights during atomoxetine treatment increased
from 1.5 at the beginning of treatment to three at the end.
Thus, atomoxetine therapy gave positive treatment effects in
nocturnal enuresis.
Thus, the combination of ADHD with enuresis in chil-
dren and adolescents is a complex problem from both the
clinical and the therapeutic points of view. A significant num-
ber of the study patients had comorbid pathology extending
beyond the range of the two disorders under discussion here
including affective disorders, behavioral impairments, and
tics. The multiple nature of the clinical signs has the result
that it is difficult to embrace the process of treating such
patients within a single algorithm. Atomoxetine monothera-
py has distinct advantages in children and adolescents with
ADHD combined with primary nocturnal enuresis, as it pro-
duces significant reductions in the severity of both ADHD
and enuresis. Furthermore, the positive effects of atomoxe-
tine should also be considered in other conditions comorbid
with ADHD, particularly anxiety disorders and oppositional-
defiant behavioral disorder and tics.
Zavadenko, Kolobova, and Suvorinova 530
REFERENCES
1. L. S. Baleva, I. V. Kazanskaya, N. A. Korovina, et al., Algorithms for
the Diagnosis and Treatment of Primary Nocturnal Enuresis in
Children (Methodological Guidelines for Physicians) [in Russian],
Russian Union of Pediatricians, Moscow (2005).
2. N. N. Zavadenko and N. M. Kolobova, Enuresis in children: the
search for new approaches to this problem, Vopr. Sovrem. Pediat., 3,
No. 5, 96100 (2004).
3. N. N. Zavadenko, Hyperactivity and Attention Deficit in Children
[in Russian], Akademiya, Moscow (2005).
4. I. V. Kazanskaya and T. V. Otpushchennikova, Enuresis: classifica-
tion, causes, diagnosis, and treatment, Vopr. Sovrem. Pediat., 1, 2027
(2004).
5. T. V. Kornilova, E. L. Grigorenko, and S. D. Smirnov, Adolescents at
Risk [in Russian], Piter, St. Petersburg (2005).
6. International Classification of Diseases (10th Edition). Classifi-
cation of Mental and Behavioral Disorders. Diagnostic Criteria for
Investigations [Russian translation] St. Petersburg (1994).
7. D. Bayens, H. Royers, P. Hoebecke, et al., Attention deficit hyper-
activity disorder in children with nocturnal enuresis, J. Urol., 171,
25762579 (2004).
8. D. Bayens, The Relationship between Attention Deficit Hyperactivity
Disorder and Enuresis in Children, PhD Thesis, Gent (2005).
9. J. Biederman, S. L. Santangelo, S. V. Faraone, et al., Clinical cor-
relates of enuresis in ADHD and non-ADHD children, J. Child.
Psychol. Psychiat., 36, 865877 (1995).
10. Diagnostic and Statistical Manual of Mental Disorders (4th edition
revision) (DSM-IV-TR), American Psychiatric Association, Wash-
ington, DC (2000).
11. R. K. Heaton, G. J. Chelune, J. L. Tallet, et al., Wisconsin Card Sorting
Test Manual (revised and expanded), Psychological Assessment
Resources (1999).
12. J. Kaufman, B. Birmaher, D. A. Brent, et al., Diagnostic Interview
Kiddie-Sads-Present and Lifetime Version (K-SADS-PL), University
of Pittsburgh School of Medicine (1996).
13. E. Ornitz, G. Hanna, and J. De Traversay, Prestimulation-induced
startle modulation in ADHD and nocturnal enuresis, Psycho-
physiology, 29, 437451 (1992).
14. S. Prasad, V. Harpin, L. Poole, et al., A multi-centre, randomised,
open-label study of atomoxetine compared with standard current
therapy in UK children and adolescents with attention deficit/hyper-
activity disorder (ADHD), Curr. Med. Res. Opin., 23, 379394
(2007).
15. W. L. Robson, J. Jackson, D. Blackhurst, and A. K. Leung, Enuresis
in children with ADHD, South. Med. J., 90, 503505 (1997).
16. J. P. Shatkin, Atomoxetine for the treatment of pediatric nocturnal
enuresis, J. Child Adolesc. Psychopharmacol., 14, 443447 (2004).
17. C. Summer, K. Schuh, V. Sutton, et al., Placebo-controlled study of
the effects of atomoxetine on bladder control in children with noc-
turnal enuresis, J. Child Adolesc. Psychopharmacol., 16, 699711
(2006).
18. A. Von Gontard and T. Neveus, Management of Disorders of Bladder
and Bowel Control in Childhood, Cambridge University Press,
Cambridge (2006).
19. M. Weiss, R. Tannock, Ch. Kratochvil, et al., A randomized, place-
bo-controlled study of once-daily atomoxetine in the school setting
in children with ADHD, J. Am. Acad. Child Adol. Psychiat., 44,
647655 (2005).
Attention Deficit Hyperactivity Disorder and Enuresis in Children and Adolescents 531
Reproducedwith permission of thecopyright owner. Further reproductionprohibited without permission.
You might also like
- Attention Deficit Hyperactivity Disorder in ChildrDocument8 pagesAttention Deficit Hyperactivity Disorder in Childrmarika arevadzeNo ratings yet
- Quality of Life in Patients With Neurogenic DysphagiaDocument8 pagesQuality of Life in Patients With Neurogenic DysphagiaDaniela OrtizNo ratings yet
- Pamj 25 82Document10 pagesPamj 25 82Pedro FlorNo ratings yet
- Anxiety Disorders Among Adolescents Referred To General Psychiatry For Multiple Causes: Clinical Presentation, Prevalence, and ComorbidityDocument10 pagesAnxiety Disorders Among Adolescents Referred To General Psychiatry For Multiple Causes: Clinical Presentation, Prevalence, and ComorbidityRatu CalistaNo ratings yet
- Robinson2012 Article ChildhoodEpilepsyAndAutismSpecDocument9 pagesRobinson2012 Article ChildhoodEpilepsyAndAutismSpecTheo KhouryNo ratings yet
- Cannabis Paper 2Document6 pagesCannabis Paper 2Carlos Eduardo Jorquera GonzálezNo ratings yet
- Epilepsy Surgery in Children With Drug-Resistant Epilepsy, A Long-Term Follow-UpDocument9 pagesEpilepsy Surgery in Children With Drug-Resistant Epilepsy, A Long-Term Follow-UpPutri IlhamiNo ratings yet
- Health-Related Quality of Life and Intellectual Functioning in Children in Remission From Acute Lymphoblastic LeukaemiaDocument7 pagesHealth-Related Quality of Life and Intellectual Functioning in Children in Remission From Acute Lymphoblastic LeukaemiaancoursNo ratings yet
- Original Paper Comorbidity of Epilepsy and Depression in Al Husseini Teaching Hospital in Holy Kerbala /iraq in 2018Document9 pagesOriginal Paper Comorbidity of Epilepsy and Depression in Al Husseini Teaching Hospital in Holy Kerbala /iraq in 2018sarhang talebaniNo ratings yet
- 3858 3871 PDFDocument14 pages3858 3871 PDFKerlyson SilvaNo ratings yet
- 472 1466 1 PB - 2Document6 pages472 1466 1 PB - 2Nazlia LarashitaNo ratings yet
- Emergency Delirium in PediatricDocument15 pagesEmergency Delirium in PediatricUzZySusFabregasNo ratings yet
- Medical Comorbidities in Children and AdolescentsDocument12 pagesMedical Comorbidities in Children and AdolescentsSalud-psicología-psiquiatria DocenciaNo ratings yet
- 2011 - IJCHP - The Leyton Obsessional Inventory-Child VersionDocument16 pages2011 - IJCHP - The Leyton Obsessional Inventory-Child VersionEsteysi Villarroel BernalesNo ratings yet
- Psychiatric Comorbidities Among Adolescents With and Without Anxiety Disorders: A Community StudyDocument6 pagesPsychiatric Comorbidities Among Adolescents With and Without Anxiety Disorders: A Community StudyLiliana PonteNo ratings yet
- Psychiatric Characterization of Children With Genetic Causes of HyperandrogenismDocument10 pagesPsychiatric Characterization of Children With Genetic Causes of HyperandrogenismnigoNo ratings yet
- Outcome in Childhood Guillain-Barré SyndromeDocument5 pagesOutcome in Childhood Guillain-Barré SyndromechristianFPTNo ratings yet
- v2 Issue 8 5Document14 pagesv2 Issue 8 5sarahNo ratings yet
- ADHD Syndrome and Tic Disorders Two Sides of The Same CoinDocument11 pagesADHD Syndrome and Tic Disorders Two Sides of The Same CoinEve AthanasekouNo ratings yet
- Sleep Problems in Children With Attention Deficit/Hyperactivity Disorder: Current Status of Knowledge and Appropriate ManagementDocument9 pagesSleep Problems in Children With Attention Deficit/Hyperactivity Disorder: Current Status of Knowledge and Appropriate ManagementGisele Elise MeninNo ratings yet
- Comorbid Mental Disorders in Children and Adolescents With Attention-Deficit:hyperactivity Disorder in A Large Nationwide StudyDocument12 pagesComorbid Mental Disorders in Children and Adolescents With Attention-Deficit:hyperactivity Disorder in A Large Nationwide StudyMarina HeinenNo ratings yet
- SMD in EpilepsyDocument11 pagesSMD in EpilepsyAndriani KhairunnisaNo ratings yet
- Barret, 2006Document7 pagesBarret, 2006Elisabet GobelliNo ratings yet
- Neurolupus 1Document13 pagesNeurolupus 1Josue LayedraNo ratings yet
- Obsessive-Compulsive Disorder in Children and Adolescents: Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and DiagnosisDocument7 pagesObsessive-Compulsive Disorder in Children and Adolescents: Epidemiology, Pathogenesis, Clinical Manifestations, Course, Assessment, and DiagnosisClarissa Castro RodríguezNo ratings yet
- Seputar A D H D Bu ErmaDocument8 pagesSeputar A D H D Bu ErmaheheheheheNo ratings yet
- QV STUDY 2012 Quality of Life of Methilfenidate Treatment - Pin-ChenDocument6 pagesQV STUDY 2012 Quality of Life of Methilfenidate Treatment - Pin-ChenDoniLeiteNo ratings yet
- Behavioral Effects of Rufinamide in LGSDocument6 pagesBehavioral Effects of Rufinamide in LGSkmarmol77No ratings yet
- Does Diagnostic Classification of Early-Onset Psychosis Change Over Follow-Up?Document9 pagesDoes Diagnostic Classification of Early-Onset Psychosis Change Over Follow-Up?Qwerty QwertyNo ratings yet
- The Effect of Simple Febrile Seizure On Attention Deficit Hyperactivity Disorder (ADHD) in ChildrenDocument7 pagesThe Effect of Simple Febrile Seizure On Attention Deficit Hyperactivity Disorder (ADHD) in ChildrenKoas PatoNo ratings yet
- Mental Health Problems in Austrian Adolescents: A Nationwide, Two Stage Epidemiological Study Applying DSM 5 CriteriaDocument17 pagesMental Health Problems in Austrian Adolescents: A Nationwide, Two Stage Epidemiological Study Applying DSM 5 CriteriaSevira NingrumNo ratings yet
- She Vell 2003Document15 pagesShe Vell 2003Ivan VeriswanNo ratings yet
- Evaluation of The Child With Global Developmental DelayDocument14 pagesEvaluation of The Child With Global Developmental DelaylauramwoodyardNo ratings yet
- Tourette Syndrome in The General Child Population: Cognitive Functioning and Self-PerceptionDocument9 pagesTourette Syndrome in The General Child Population: Cognitive Functioning and Self-PerceptionIdoia PñFlrsNo ratings yet
- JoHM 03 2018 ADHD KiGGS-Wave2Document8 pagesJoHM 03 2018 ADHD KiGGS-Wave2C ANo ratings yet
- 130 494 1 PB PDFDocument9 pages130 494 1 PB PDFhfathiardiNo ratings yet
- Journal Adhi DR Rini Behavioral Problems in Children With Epilepsy (Autosaved)Document33 pagesJournal Adhi DR Rini Behavioral Problems in Children With Epilepsy (Autosaved)Utomo SiswoNo ratings yet
- Cerebelo Habla InglesDocument8 pagesCerebelo Habla InglesKimberling LoyolaNo ratings yet
- A Detailed Semiologic Analysis of Childhood Psychogenic Nonepileptic SeizuresDocument6 pagesA Detailed Semiologic Analysis of Childhood Psychogenic Nonepileptic SeizuresNico NicoNo ratings yet
- 1 s2.0 S152550502300135X MainDocument8 pages1 s2.0 S152550502300135X MainilonaskorinNo ratings yet
- Emotional Health in Attention Deficit HyperactivitDocument5 pagesEmotional Health in Attention Deficit HyperactivitAzucena DONo ratings yet
- CHAPTER 02, Literature ReviewDocument27 pagesCHAPTER 02, Literature ReviewAyesha ArshedNo ratings yet
- Clinical Study: Vertigo in Children and Adolescents: Characteristics and OutcomeDocument6 pagesClinical Study: Vertigo in Children and Adolescents: Characteristics and OutcomeC Leite HendriyNo ratings yet
- 7b AUTISMManuscriptinPTJournal - May2011Document14 pages7b AUTISMManuscriptinPTJournal - May2011Carla Daniela Agüero VargasNo ratings yet
- Factor Analysis of The Pediatric Symptom Checklist in A Population of Children With Voiding Dysfunction And/or Nocturnal EnuresisDocument9 pagesFactor Analysis of The Pediatric Symptom Checklist in A Population of Children With Voiding Dysfunction And/or Nocturnal EnuresisCris RodriguesNo ratings yet
- Chiu 2020 Prevalence and Predictors of Mood in iRBD PDFDocument8 pagesChiu 2020 Prevalence and Predictors of Mood in iRBD PDFEl MoNo ratings yet
- Mental Health of Adolescents With Epilepsy in Enugu, Nigeria: A Cross-Sectional StudyDocument7 pagesMental Health of Adolescents With Epilepsy in Enugu, Nigeria: A Cross-Sectional Studyhasemana hasemanaNo ratings yet
- Screening of Generalized Anxiety Disorder in PatieDocument10 pagesScreening of Generalized Anxiety Disorder in PatieAprilia Chairun NisaNo ratings yet
- An Epilepsy Questionnaire Study of Knowledge and Attitudes in Canadian College StudentsDocument7 pagesAn Epilepsy Questionnaire Study of Knowledge and Attitudes in Canadian College StudentsToni HercegNo ratings yet
- Attention and Executive Functions of Children With Attention Deficit Hyperactivity DisorderDocument5 pagesAttention and Executive Functions of Children With Attention Deficit Hyperactivity Disordergion.nandNo ratings yet
- The Neural Correlates of Chronic Symptoms of Vertigo Proneness in HumansDocument20 pagesThe Neural Correlates of Chronic Symptoms of Vertigo Proneness in HumanspratiwifatmasariNo ratings yet
- Noutati Despre ADHDDocument17 pagesNoutati Despre ADHDMirela MaticanNo ratings yet
- Archive of SID: Ashrafalsadat Hakim, Simin Madhooshi, Ehsan ValaviDocument7 pagesArchive of SID: Ashrafalsadat Hakim, Simin Madhooshi, Ehsan ValaviAbdul AzizNo ratings yet
- Long-Term Follow-Up Ofthe Tips Early Detection in Psychosisstudy:Effectson 10-YearoutcomeDocument7 pagesLong-Term Follow-Up Ofthe Tips Early Detection in Psychosisstudy:Effectson 10-YearoutcomeELvine GunawanNo ratings yet
- Depressive Symptoms Are Prevalent in Childhood-Onset Systemic Lupus Erythematosus (cSLE)Document9 pagesDepressive Symptoms Are Prevalent in Childhood-Onset Systemic Lupus Erythematosus (cSLE)Random PersonNo ratings yet
- CBCL Profiles of Children and Adolescents With Asperger Syndrome - A Review and Pilot StudyDocument12 pagesCBCL Profiles of Children and Adolescents With Asperger Syndrome - A Review and Pilot StudyWildan AnrianNo ratings yet
- Asymmetric Tonic Neck Reflex and Symptoms of Attention Deficit and Hyperactivity Disorder in ChildrenDocument5 pagesAsymmetric Tonic Neck Reflex and Symptoms of Attention Deficit and Hyperactivity Disorder in ChildrenRSIAMOELIANo ratings yet
- Jansen 2000Document12 pagesJansen 2000dimasprastiiaNo ratings yet
- Endokrin4 PDFDocument6 pagesEndokrin4 PDFAdelina Wahyuni LubisNo ratings yet
- Diagnosis and Treatment of Children With Autism Spectrum DisordersFrom EverandDiagnosis and Treatment of Children With Autism Spectrum DisordersRating: 5 out of 5 stars5/5 (1)
- Acute Pain Management in Patients With Opioid ToleranceDocument6 pagesAcute Pain Management in Patients With Opioid ToleranceHendrikus Surya Adhi PutraNo ratings yet
- Single Versus Multi-Incisional Video-Assisted Thoracic Surgery: A Systematic Review and Meta-AnalysisDocument12 pagesSingle Versus Multi-Incisional Video-Assisted Thoracic Surgery: A Systematic Review and Meta-AnalysisHendrikus Surya Adhi PutraNo ratings yet
- DRAFT 1 Introduction and Literature ReviewDocument6 pagesDRAFT 1 Introduction and Literature ReviewHendrikus Surya Adhi PutraNo ratings yet
- Severe Sepsis and Septic Shock: Taking Advantage of Window of Opportunity. CMAJDocument1 pageSevere Sepsis and Septic Shock: Taking Advantage of Window of Opportunity. CMAJHendrikus Surya Adhi PutraNo ratings yet
- Development at Any Phase Is Always Linked With Technology and TechnologyDocument1 pageDevelopment at Any Phase Is Always Linked With Technology and TechnologyHendrikus Surya Adhi PutraNo ratings yet
- Black Box Warnings: Renal Failure Patients: Masters SB (2012)Document16 pagesBlack Box Warnings: Renal Failure Patients: Masters SB (2012)Hendrikus Surya Adhi PutraNo ratings yet
- Glion StudentsExcercise TemplateDocument49 pagesGlion StudentsExcercise TemplateHendrikus Surya Adhi PutraNo ratings yet
- How To Write&Present Paper 07Document24 pagesHow To Write&Present Paper 07Hendrikus Surya Adhi PutraNo ratings yet
- Vasopressors and Inotropes in ShockDocument8 pagesVasopressors and Inotropes in ShockRiska PashaNo ratings yet
- Adjunctive Pharmacotherapy For Cognitive Deficit in Schizoprenia PDFDocument8 pagesAdjunctive Pharmacotherapy For Cognitive Deficit in Schizoprenia PDFHendrikus Surya Adhi PutraNo ratings yet
- 4 DapusDocument1 page4 DapusHendrikus Surya Adhi PutraNo ratings yet
- 4 DapusDocument1 page4 DapusHendrikus Surya Adhi PutraNo ratings yet
- Logbook UdayanaDocument4 pagesLogbook UdayanaHendrikus Surya Adhi PutraNo ratings yet
- Blood Group IncompatibilityDocument7 pagesBlood Group IncompatibilityHendrikus Surya Adhi PutraNo ratings yet
- Attention Deficit Hyperactivity Disorder and Enuresis in Children and AdolescentsDocument8 pagesAttention Deficit Hyperactivity Disorder and Enuresis in Children and AdolescentsHendrikus Surya Adhi PutraNo ratings yet
- Vasopressors and Inotropes in ShockDocument8 pagesVasopressors and Inotropes in ShockRiska PashaNo ratings yet
- Critical Care Management PreeclampsiaDocument30 pagesCritical Care Management PreeclampsiaIqe ChanNo ratings yet
- Kidney Stones & Uretral Stones: What Are Stones and The Difference Between Kidney Stones and Ureteral Stones?Document21 pagesKidney Stones & Uretral Stones: What Are Stones and The Difference Between Kidney Stones and Ureteral Stones?Hendrikus Surya Adhi PutraNo ratings yet
- Resep ObatDocument1 pageResep ObatHendrikus Surya Adhi PutraNo ratings yet
- Eclampsia - A Global ProblemDocument5 pagesEclampsia - A Global ProblemHendrikus Surya Adhi PutraNo ratings yet
- Enuresis DataDocument9 pagesEnuresis DataHendrikus Surya Adhi PutraNo ratings yet
- Diuretics Best GivenDocument6 pagesDiuretics Best GivenHendrikus Surya Adhi PutraNo ratings yet
- Stem Cell OsteosarcomaDocument5 pagesStem Cell OsteosarcomaHendrikus Surya Adhi PutraNo ratings yet
- Chronic Granulomatous Mastitis - Diagnostic and Therapeutic ConsiderationsDocument4 pagesChronic Granulomatous Mastitis - Diagnostic and Therapeutic ConsiderationsHendrikus Surya Adhi PutraNo ratings yet
- Teaching Photo Radiology: Thorax EditionDocument0 pagesTeaching Photo Radiology: Thorax EditionHendrikus Surya Adhi PutraNo ratings yet
- Radiology Teaching Photo AbdomenDocument0 pagesRadiology Teaching Photo AbdomenHendrikus Surya Adhi PutraNo ratings yet
- Magnesium SulphateDocument9 pagesMagnesium SulphateNatália A. OliveiraNo ratings yet
- Annual Report 2010Document72 pagesAnnual Report 2010Yan-Lin Jubi LeeNo ratings yet
- Alemnesh MandeshDocument94 pagesAlemnesh MandeshDNo ratings yet
- Daftar Kalibrasi Alat 2020Document18 pagesDaftar Kalibrasi Alat 2020Budi SetyawanNo ratings yet
- Pediatric Nursing Flashcards2 - QuizletDocument50 pagesPediatric Nursing Flashcards2 - QuizletNursyNurseNo ratings yet
- Childrens Colour Trail TestDocument5 pagesChildrens Colour Trail Testsreetama chowdhuryNo ratings yet
- ID Penyakit Ginjal Kronik Derajat VDocument10 pagesID Penyakit Ginjal Kronik Derajat VNinaSakina AttamimiNo ratings yet
- Sales and Distribution Management PDFDocument30 pagesSales and Distribution Management PDFNalin SenthilNo ratings yet
- The Modern Technology of Radiation PhysicsDocument67 pagesThe Modern Technology of Radiation PhysicsNaomi Morales Medina0% (1)
- Communication Skills For Medicine Lloyd PDFDocument2 pagesCommunication Skills For Medicine Lloyd PDFLester10% (10)
- Brad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Document36 pagesBrad J Hornberger Cystoscopy Indications and Preparation. UAPA CME Conference 2012 (30 Min)Cristian OrozcoNo ratings yet
- Who NMH Nvi 18.3 EngDocument41 pagesWho NMH Nvi 18.3 EngZenard de la CruzNo ratings yet
- NST and Their FunctionsDocument5 pagesNST and Their FunctionsyazNo ratings yet
- Wellness Massage Q1 Mod 4Document21 pagesWellness Massage Q1 Mod 4Jea Caderao AlapanNo ratings yet
- Zyrtec: Tablet Core: Tablet CoatingDocument5 pagesZyrtec: Tablet Core: Tablet CoatingDwi WirastomoNo ratings yet
- Resume Template PharmacistDocument1 pageResume Template PharmacistHammad AslamNo ratings yet
- Hand Hygiene Audit March 19Document17 pagesHand Hygiene Audit March 19Sammie WainainaNo ratings yet
- Overt Diabetes in PregnancyDocument12 pagesOvert Diabetes in PregnancyGestne AureNo ratings yet
- Forensic MedicineDocument21 pagesForensic Medicineritika100% (3)
- CTD Question and AnswersDocument17 pagesCTD Question and AnswersPraveenaNo ratings yet
- Thesis Plan FormatDocument13 pagesThesis Plan FormatJotu ThakurNo ratings yet
- Pathophysiology of Pain in BiliodigestiDocument19 pagesPathophysiology of Pain in Biliodigestiprabowoaji12No ratings yet
- Achya - 3Document11 pagesAchya - 3Jannah Miftahul JannahNo ratings yet
- 1b. Pediatrics Subject Exam - Content Outline - NBMEDocument8 pages1b. Pediatrics Subject Exam - Content Outline - NBMEmeiraimNo ratings yet
- Standard Operating Procedures HospitalDocument5 pagesStandard Operating Procedures HospitalCindy Gabayeron100% (1)
- Aspirin Plus Clopidogrel As Secondary Prevention After Stroke or Transient Ischemic Attack: A Systematic Review and Meta-AnalysisDocument13 pagesAspirin Plus Clopidogrel As Secondary Prevention After Stroke or Transient Ischemic Attack: A Systematic Review and Meta-AnalysisshevmyrNo ratings yet
- ASPMN Position Statement Pain Assesement NonVerbalDocument9 pagesASPMN Position Statement Pain Assesement NonVerbalKitesaMedeksaNo ratings yet
- National Formulary of Unani Medicine Part Ia-O PDFDocument336 pagesNational Formulary of Unani Medicine Part Ia-O PDFMuhammad Sharif Janjua0% (1)
- Acupressure Points For Knee PainDocument7 pagesAcupressure Points For Knee Painلوليتا وردةNo ratings yet
- What Is LordosisDocument10 pagesWhat Is LordosisNisa ShaqiriNo ratings yet