Professional Documents
Culture Documents
Nri1005 Mdscs Poster
Uploaded by
Aldair FigueroaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nri1005 Mdscs Poster
Uploaded by
Aldair FigueroaCopyright:
Available Formats
Bone marrow
HSCs
CMPs
Macrophages
Dendritic cells
Blood and peripheral
tissues under physiological
conditions
Blood and peripheral tissues under
pathological conditions
Monocyte precursors
Monocytic MDSCs (1020%)
Monocytic
MDSC
Monocytic
MDSC
Granulocyte
Granulocytic
MDSC
Blood
vessel
Monocyte/
macrophage
Granulocyte precursors Granulocytes
Granulocytic MDSC
Inducers of normal
myeloid cells
GM-CSF
G-CSF
M-CSF
SCF
FLT3
IL-3
Inducers of MDSCs
Tumour cells: GM-CSF, G-CSF,
M-CSF, SCF and VEGF
Stromal cells associated with
tumours: IL-1, IL-4, IL-6, IL-10,
IL-13, IFN, PROK2 and PGE
2
Infection: dsRNA, LPS, HSP,
CpG DNA, flagellin, C5a, S100A8,
S100A9, IFN and GM-CSF
Trauma: IL-1, HSP, C5a, S100A8,
S100A9, IFN and GM-CSF
TYK2 JAK2
ONO
cGMP
P P
P
S
T
A
T
6
JAK3 JAK1 P P
P
S
T
A
T
1
JAK1
NOS2
MYD88
TLR
P
P
IL-6, GM-CSF, G-CSF,
M-CSF, VEGF and IL-10
Expression of MYC,
BCL-X
L
, cyclin D1,
S100A8 and S100A9
ARG2 NOS3
NOS2
NO
ONOO
(RNS)
O
2
NADPH oxidase
Proliferative arrest
Loss of CD3 chain
Loss of peptideMHC binding
Altered transmission
of IL-2 signal
Induction of T
Reg
cells
L-cysteine
L-arginine
L-arginine
L-arginine
ARG1
ARG2
NOS3
NADPH
oxidase
High levels
of ROS
IL-4 and IL-13 IFN and IL-1 TGF
and IL-10
H
2
O
2
ONOO
NO O
2
TLR ligands: dsRNA,
LPS, HSP, CpG DNA
and flagellin
Cytokine
receptor
p50 p65
NF-B
Cytoplasm
Nucleus
Proliferation and survival of IMCs;
suppression of differentiation
Expression of ARG1,
NOS2, IL-10 and COX2
NADPH
oxidase
complex
S100A9 S100A8
ARG1
NOS2
High levels
of NO
H
2
0
2
(ROS)
H
2
0
PI3K
GCN2
EIF2A
mTOR
Cell
cycle
Altered mRNA
transcription
Nitration of tyrosine
residues on TCR
Nitrosylation
of cysteine
residues
Inhibition of
JAK3, STAT5,
AKT and ERK2
phosphorylation
Altered
TCR function
CD3
TCR
T cell
?
Metastatic tumour site
Tumour cell
survival and invasion
Angiogenesis
MDSCs
TGF
MMP2
MMP13
MMP14
VEGFA
bFGF
ARG1
TGF
MMP7
MMP9
MMP12
Site of tissue injury
Angiogenesis
Collagen synthesis
Fibrosis
Tissue remodelling
MDSCs
FOXP3
expression IL-2R
IL-2
IL-10?
Decreased
mRNA
stability
TCR
MHC
class II
IL-10
TGF
IL-10?
CD40L
CD40
IFN
Primary tumour site
Lymphangiogenesis
Angiogenesis
TAM
MDSCs
Erythrocyte
VEGFA
bFGF
IL-1
MMP7
MMP9
MMP12
TNF
VEGF
IL-6
NO
PROK2
MMP9
VEGFC
VEGFD
?
?
S
T
A
T
3
Expression of TGF,
ARG1 and NOS2
TAM
Tumour
?
?
TNF
IL-1
Granulocytic MDSCs (8090%)
IMCs
?
T cell suppression
MDSCs can suppress T cell effector
functions in various ways. Several
factors can modulate the expression
levels of ARG, NADPH oxidase and
NOS in MDSC subsets, with the final
effect on the microenvironment
including depletion of l-arginine,
release of RNS and ROS (with ONOO
and H
2
O
2
being the most prevalent
molecules, respectively) or unopposed
production of high NO levels.
Moreover, l-cysteine can be
sequestered by MDSCs. All of these
molecules influence the intracellular
signalling pathways that control T cell
proliferation after antigen stimulation.
MDSC-mediated immune suppression
can also be associated with the
expansion of T
Reg
cell populations.
In secondary lymphoid organs,
MDSC-mediated suppression requires
the direct presentation of antigens
by MDSCs to T cells. The activity of
MDSCs can also be enhanced by
activated T cells in this way. At tumour
sites, microenvironmental signals
support constitutive activation of the
immunosuppressive programme in
MDSCs, which affects nearby T cells
in an antigen-nonspecific manner.
Tumorigenesis and tissue repair
MDSCs in the tumour environment produce factors that support tumour growth by directly
promoting tumour angiogenesis and lymphangiogenesis. In addition, MDSCs might be able to
differentiate into TAMs that have similar activity. MDSCs can also migrate to distant tissues and
participate in the formation of a pre-metastatic niche by promoting local angiogenesis
and the survival of arriving tumour cells. MMPs produced by MDSCs can
support tumour cell invasion. By similar mechanisms, MDSCs can migrate to a
site of tissue injury and participate in tissue remodelling and angiogenesis.
Myeloid-derived suppressor cells
Vincenzo Bronte and Dmitry Gabrilovich
To protect the host from the harmful effects of excessive
immune stimulation during acute and chronic infections,
and to limit the generation of autoimmune responses
towards tissue antigens released by trauma, the bone
marrow is stimulated to release immature myeloid cells
(IMCs) into the blood. These IMCs and some of their
progeny, which might include certain tumour-associated
macrophages (TAMs), can restrain the activation of
T cells. They are therefore known as myeloid-derived
suppressor cells (MDSCs) to highlight their common
myeloid origin and immunoregulatory properties. It is
now clear that MDSCs also have poorly defined roles in
wound healing and tissue repair. Tumours have evolved
to harness these properties of MDSCs to restrain
antitumour immunity and to promote tumour expansion
in the surrounding environment and at distant sites,
through effects on angiogenesis and metastasis. New
therapies to restrain MDSC activity are crucial for the
efficient control of tumour cells by immune responses.
Protocols to generate MDSCs might be useful in
pathologies involving excessive immune stimulation,
such as autoimmune diseases and transplant rejection.
Abbreviations
ARG, arginase; bFGF, basic fibroblast growth factor; BCL-X
L
,
B cell lymphoma X
L
; C5a, complement component 5a;
CCR2, CC-chemokine receptor 2; cGMP, cyclic guanosine
monophosphate; CMP, common myeloid progenitor; COX2,
cyclooxygenase 2; CXCR, CXC-chemokine receptor;
CX
3
CR1, CX
3
C-chemokine receptor 1; dsRNA, double-
stranded RNA; EIF2A, eukaryotic translation initiation factor
2; ERK2, extracellular-signal-regulated kinase 2; FLT3, FMS-
like tyrosine kinase 3; FOXP3, Forkhead box P3; GCN2, also
known as EIF2A kinase 4; G-CSF, granulocyte colony-
stimulating factor; GM-CSF, granulocytemacrophage
colony-stimulating factor; H
2
O
2
, hydrogen peroxide; HSC,
haematopoietic stemcell; HSP, heat shock protein; IFN,
interferon-; IL, interleukin; IL-2R, IL-2 receptor; JAK, Janus
kinase; LPS, lipopolysaccharide; M-CSF, macrophage
colony-stimulating factor; MMP, matrix metalloproteinase;
mTOR, mammalian target of rapamycin; MYD88, myeloid
differentiation primary response protein 88; NF-B, nuclear
factor-B; NO, nitric oxide; NOS, nitric oxide synthase;
ONOO
, peroxynitrite; PECAM1, plateletendothelial cell
adhesion molecule 1; PGE
2
, prostaglandin E
2
; PI3K,
phosphoinositide 3-kinase; PROK2, prokineticin 2 (also
known as BV8); RNS, reactive nitrogen species; ROS, reactive
oxygen species; S100A8, S100 calcium-binding protein A8;
SCF, stemcell factor (also known as KIT ligand); STAT, signal
transducer and activator of transcription; TCR, T cell
receptor; TGF, transforming growth factor-; TLR, Toll-like
receptor; TNF, tumour necrosis factor; T
Reg
cell, regulatory
T cell; TYK2, tyrosine kinase 2; VEGF, vascular endothelial
growth factor; VEGFR1, VEGF receptor 1.
Affiliations
Vincenzo Bronte is at the Istituto Oncologico Veneto,
Via Gattamelata 64, 35128 Padova, Italy.
Dmitry Gabrilovich is at the H. Lee Moffitt Cancer Center and
Research Institute, University of South Florida, MRC 2067,
12902 Magnolia Drive, Tampa, Florida 33612, USA.
e-mails: enzo.bronte@unipd.it; dmitry.gabrilovich@moffitt.org
The authors declare no competing financial interests.
Edited by Kirsty Minton and Olive Leavy; copyedited by
Gemma Ryan; designed by Simon Bradbrook.
(2010) Macmillan Publishers Ltd. All rights reserved.
http://www.nature.com/nri/posters/mdscs
References available online.
BioLegend (www.biolegend.com)
BioLegend is your resource for world-class quality antibodies and other reagents for biomedical research,
provided at an outstanding value. Founded in 2002, BioLegend is located in the heart of the
biotechnology community in San Diego, California. Our experienced leaders were co-founders of
PharMingen, nowBDBiosciences. Our product areas include cell immunophenotyping, cytokines and
chemokines, adhesion, cancer research, T regulatory cells, stemcells, innate immunity, cell-cycle analysis,
apoptosis, and T helper subsets. All of BioLegends reagents are supported by superior customer service
and come with a 100%quality guarantee. Our aggressive product development program, through
technology licensing, collaborations, and internal hybridoma development, produces strategic reagents
for use in a variety of applications including flowcytometry, ELISA, immunoprecipitation, Western
blotting, immunofluorescence microscopy, immunohistochemistry, customLuminex assays, and in vitro or
in vivo functional assays. BioLegend offers the broadest selection of fluorochrome conjugates for multi-
color flowcytometry. BioLegend offers a wide array of customassays and services, including
development of multicolor flowcytometry panels to meet our customers specific needs. BioLegend is the
preferred vendor for flowcytometry reagents at Harvard University, and we are a proud sponsor of just
about every immunology society in the world.
Generation and accumulation
MDSCs are an intrinsic part of the myeloid cell lineage and are a heterogeneous population
comprised of myeloid cell progenitors and precursors of granulocytes, macrophages and dendritic
cells. In healthy individuals, IMCs generated in the bone marrow differentiate into mature
granulocytes, macrophages or dendritic cells. Various cytokines and soluble factors released during
pathological conditions, such as cancer, infection, trauma and autoimmunity (and after bone marrow
transplantation), cause the proliferation of IMCs and a partial block of their differentiation. This
results in the accumulation of MDSCs, which then migrate to secondary lymphoid organs and
tissues (such as the tumour site), where they exert their effects on other cell populations.
Activation and proliferation
The proliferation of MDSCs is associated with activation of these cells in a pathological context. Activation is mediated through
several transcription factors and results in the upregulation of expression of immunosuppressive factors, such as ARG1 and NOS2,
upregulation of activity of the NADPH oxidase complex and an increase in the production of NO, ROS, RNS and cytokines.
IMMUNOLOGY
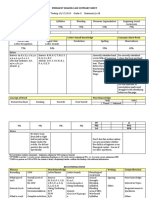
Therapies to restrain the activity of MDSCs
Therapeutic agent* Type of cancer tested Effect on MDSCs Refs
COX2 inhibitor
(SC58236)
Mammary carcinoma
(mice)
Inhibition of
proliferation
1
Amino-biphosphonate Mammary tumours
(mice)
Inhibition of
proliferation
2
Phosphodiesterase-5
inhibitor (sildenafil
and tadalafil)
Mammary carcinoma,
colon carcinoma and
fibrosarcoma (all mice)
Inhibition of
proliferation and of
suppressive effects
3
KIT-specific antibody Colon carcinoma
(mice)
Inhibition of
proliferation
4
Nitroaspirin Colon carcinoma
(mice)
Inhibition of
suppressive effects
5
Triterpenoid Colon carcinoma,
thymoma and lung
cancer (all mice)
Inhibition of
suppressive effects
6
All-trans retinoic acid Sarcoma and colon
carcinoma (mice)
Metastatic renal cell
carcinoma (human)
Inhibition of
proliferation
7
8
25-hydroxyvitamin
D3
Head and neck cancer
(human)
Moderate inhibition
of proliferation
9
Gemcitabine Lung and breast
cancer (mice)
Inhibition of
proliferation
10,
11
VEGF-trap
Solid tumours (human) None 12
VEGF-specific
antibody (avastin)
Metastatic renal cell
cancer (human)
Weak inhibition of
proliferation
13
Doxorubicin-
cyclophosphamide
Breast cancer (human) Weak inhibition of
proliferation
14
Antagonists for CXCR2
(S-265610) and CXCR4
(AMD3100)
Breast cancer (mice) Inhibition of
proliferation
15
Tyrosine kinase
inhibitor (sunitinib)
Renal cell cancer
(human)
Weak inhibition of
proliferation
16
PROK2-specific
antibody
Various tumours of
human and mouse
origin in nude mice
Inhibition of
proliferation
17
*The agents described in these studies were used for the purpose of targeting
MDSCs but, by their nature, these agents are not specific for MDSCs.
The VEGF-
trap is a fusion protein that binds all forms of VEGFA and placental growth factor.
Therapeutic induction of MDSCs
Source of MDSCs Type of immune
pathology tested
Effect of MDSCs Refs
Activated following
CD8
+
T cell-induced
acute enterocolitis
Inflammatory
bowel disease
(mice)
Inhibition of antigen-specific CD8
+
T cells
18
Generated in vitro
from mouse embryonic
stem cells
Graft-versus-host
disease (mice)
Prevention of disease following
adoptive transfer of MDSCs
19
Induced by
perioperative
treatment with CD28-
specific antibodies
Kidney allograft
transplant (mice)
Maintenance of graft tolerance 20
Induced by endotoxin Skin allograft
transplant (mice)
Prolongation of graft survival
following adoptive transfer of MDSCs
21
MDSC markers
Marker Mouse splenic MDSCs Human peripheral blood MDSCs
C
D
1
1
b
G
r
1
L
y
6
C
L
y
6
G
C
D
3
1
(
P
E
C
A
M
1
)
F
4
/
8
0
C
D
1
d
C
D
1
6
C
D
3
2
C
D
5
4
C
D
6
8
C
D
8
0
C
D
1
1
5
C
D
1
2
4
C
C
R
2
C
X
3
C
R
1
C
D
1
1
b
C
D
1
4
C
D
1
5
C
D
1
6
C
D
3
3
C
D
6
6
b
C
D
1
2
4
V
E
G
F
R
1
H
L
A
-
D
R
Expression
level
Granulocytic MDSCs High High Low High + + + Low + High + + Low + + + +
Monocytic MDSCs High Mid High + + + + High + + + + Low + + + + Low
20 Macmillan Publishers Limited. All rights reserved 10
References
1. Sinha, P., Clements, V. K., Fulton, A. M. & Ostrand-Rosenberg, S. Prostaglandin E2 promotes tumor progression by
inducing myeloid-derived suppressor cells. Cancer Res. 67, 45074513 (2007).
2. Melani, C., Sangaletti, S., Barazzetta, F. M., Werb, Z. & Colombo, M. P. Amino-biphosphonate-mediated MMP-9
inhibition breaks the tumorbone marrow axis responsible for myeloid-derived suppressor cell expansion and
macrophage infiltration in tumor stroma. Cancer Res. 67, 1143811446 (2007).
3. Serafini, P. et al. Phosphodiesterase-5 inhibition augments endogenous antitumor immunity by reducing myeloid-
derived suppressor cell function. J. Exp. Med. 203, 26912702 (2006).
4. Pan, P. Y. et al. Reversion of immune tolerance in advanced malignancy: modulation of myeloid-derived suppressor cell
development by blockade of stem-cell factor function. Blood 111, 219228 (2008).
5. De Santo, C. et al. Nitroaspirin corrects immune dysfunction in tumor-bearing hosts and promotes tumor eradication
by cancer vaccination. Proc. Natl Acad. Sci. USA 102, 41854190 (2005).
6. Nagaraj, S. et al. Anti-inflammatory triterpenoid blocks immune suppressive function of myeloid-derived suppressor
cells and improves immune response in cancer. Clin. Cancer Res. (in the press).
7. Kusmartsev, S. et al. All-trans-retinoic acid eliminates immature myeloid cells from tumor-bearing mice and improves
the effect of vaccination. Cancer Res. 63, 44414449 (2003).
8. Mirza, N. et al. All-trans-retinoic acid improves differentiation of myeloid cells and immune response in cancer patients.
Cancer Res. 66, 92999307 (2006).
9. Lathers, D., Clark, J., Achille, N. & Young, M. Phase 1B study to improve immune responses in head and neck cancer
patients using escalating doses of 25-hydroxyvitamin D3. Cancer Immunol. Immunother. 53, 422430 (2004).
10. Suzuki, E., Kapoor, V., Jassar, A. S., Kaiser, L. R. & Albelda, S. M. Gemcitabine selectively eliminates splenic Gr-1
+
/
CD11b
+
myeloid suppressor cells in tumor-bearing animals and enhances antitumor immune activity. Clin. Cancer Res.
11, 67136721 (2005).
11. Sinha, P., Clements, V. K., Bunt, S. K., Albelda, S. M. & Ostrand-Rosenberg, S. Cross-talk between myeloid-derived
suppressor cells and macrophages subverts tumor immunity toward a type 2 response. J. Immunol. 179, 977983
(2007).
12. Fricke, I. et al. Vascular endothelial growth factor-trap overcomes defects in dendritic cell differentiation but does not
improve antigen-specific immune responses. Clin. Cancer Res. 13, 48404848 (2007).
13. Kusmartsev, S. et al. Oxidative stress regulates expression of VEGFR1 in myeloid cells: link to tumor-induced immune
suppression in renal cell carcinoma. J. Immunol. 181, 346353 (2008).
14. Diaz-Montero, C. M. et al. Increased circulating myeloid-derived suppressor cells correlate with clinical cancer stage,
metastatic tumor burden, and doxorubicin-cyclophosphamide chemotherapy. Cancer Immunol. Immunother. 58, 4959
(2009).
15. Yang, L. et al. Abrogation of TGF signaling in mammary carcinomas recruits Gr-1
+
CD11b
+
myeloid cells that promote
metastasis. Cancer Cell 13, 2335 (2008).
16. van Cruijsen, H. et al. Sunitinib-induced myeloid lineage redistribution in renal cell cancer patients: CD1c
+
dendritic cell
frequency predicts progression-free survival. Clin. Cancer Res. 14, 5884-5892 (2008).
17. Shojaei, F. et al. Bv8 regulates myeloid-cell-dependent tumour angiogenesis. Nature 450, 825831 (2007).
18. Haile, L. A. et al. Myeloid-derived suppressor cells in inflammatory bowel disease: a new immunoregulatory pathway.
Gastroenterology 135, 871881 (2008).
19. Zhou, Z. et al. Development and function of myeloid-derived suppressor cells generated from mouse embryonic and
hematopoietic stem cells. Stem Cells 13 Jan 2010 (doi:10.1002/stem.301).
20. Dugast, A. S. et al. Myeloid-derived suppressor cells accumulate in kidney allograft tolerance and specifically suppress
effector T cell expansion. J. Immunol. 180, 78987906 (2008).
21. De Wilde, V. et al. Endotoxin-induced myeloid-derived suppressor cells inhibit alloimmune responses via heme
oxygenase-1. Am. J. Transplant. 9, 20342047 (2009).
20 Macmillan Publishers Limited. All rights reserved 10
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Physical Chemical Changes Lesson 2 ReflectionDocument2 pagesPhysical Chemical Changes Lesson 2 Reflectionapi-360585476No ratings yet
- The New Barbarians at The Gate - Debt-Based TakeoversDocument61 pagesThe New Barbarians at The Gate - Debt-Based TakeoversWho's in my Fund100% (1)
- Unit-16 Field Administration PDFDocument14 pagesUnit-16 Field Administration PDFSara LopezNo ratings yet
- Sale of Goods (Sales of Goods Act 1957)Document5 pagesSale of Goods (Sales of Goods Act 1957)Yee Zhi XuanNo ratings yet
- BITS Pilani MBA Project Work Course HandoutDocument20 pagesBITS Pilani MBA Project Work Course Handoutshashank_khatri3728No ratings yet
- SSRN Id2468243Document18 pagesSSRN Id2468243Bhawani ShankerNo ratings yet
- Letter From Julius Eckman To Solomon Nunes Carvalho, San Francisco 1855 (Transcription of Original Manuscript)Document3 pagesLetter From Julius Eckman To Solomon Nunes Carvalho, San Francisco 1855 (Transcription of Original Manuscript)magnesmuseumNo ratings yet
- CHP 3 - Classical Theory of DevDocument29 pagesCHP 3 - Classical Theory of DevSardar Khawar0% (1)
- Fract FaultDocument50 pagesFract FaultLeonardo Sierra LombarderoNo ratings yet
- Observation Checklist: (Brown, 2000)Document3 pagesObservation Checklist: (Brown, 2000)Putri AliarezaNo ratings yet
- Holy Prophet PBUHDocument1 pageHoly Prophet PBUHWaqas AbbasiNo ratings yet
- Controlled Writing ActivityDocument1 pageControlled Writing ActivityytakwaleNo ratings yet
- Artica Web DocumentationDocument30 pagesArtica Web Documentationsnake972No ratings yet
- Congratulations! You're Almost Done!: English 2, V14, Segment 2 Exam Review GuideDocument16 pagesCongratulations! You're Almost Done!: English 2, V14, Segment 2 Exam Review GuideSophia VinsNo ratings yet
- Larvicidal Activity of Some Saponin Containing Plants Against The Dengue Vector Aedes Aegypti.Document11 pagesLarvicidal Activity of Some Saponin Containing Plants Against The Dengue Vector Aedes Aegypti.Dr. Jawale Chetan S.100% (1)
- Recognition Day 2023 - Bartolabac-Straight FeatureDocument3 pagesRecognition Day 2023 - Bartolabac-Straight FeatureAnne BartolabacNo ratings yet
- Thompson-EOARD SpaceDocument15 pagesThompson-EOARD SpaceafosrNo ratings yet
- Bread and Pastry TG PDFDocument19 pagesBread and Pastry TG PDFAmpolitoz86% (7)
- F R LeavisDocument7 pagesF R LeavisAravind G Krishnan67% (3)
- Bad Meetings British English Teacher Ver2 BWDocument7 pagesBad Meetings British English Teacher Ver2 BWANo ratings yet
- Unit 1 ss7g8b Ethinic GroupsDocument36 pagesUnit 1 ss7g8b Ethinic Groupsapi-233036636No ratings yet
- TCMP Manual Provides Guidance for Inmate RehabilitationDocument159 pagesTCMP Manual Provides Guidance for Inmate RehabilitationDONALDO BRITAÑANo ratings yet
- Indian Political SystemDocument25 pagesIndian Political SystemAyeza AmerNo ratings yet
- Paediatrics MCQ PointsDocument117 pagesPaediatrics MCQ PointstharikaneelawathuraNo ratings yet
- Food ValuesDocument2 pagesFood ValuesMiss L. NelNo ratings yet
- Emergent Reader Case Summary SheetDocument2 pagesEmergent Reader Case Summary Sheetapi-503192153No ratings yet
- FORM 1 Chapter 5 Perimeter, Area and Volume 2014Document18 pagesFORM 1 Chapter 5 Perimeter, Area and Volume 2014Amjad RanaNo ratings yet
- Books of Allah: Guidance from God's Holy ScripturesDocument3 pagesBooks of Allah: Guidance from God's Holy ScripturesHesti ulia sariNo ratings yet
- Music Ministry Meeting - Sept. 22Document5 pagesMusic Ministry Meeting - Sept. 22Anima PurpleNo ratings yet
- Toaru Majutsu No Index SS - KanzakiDocument2 pagesToaru Majutsu No Index SS - KanzakiJstar55555No ratings yet