Professional Documents
Culture Documents
Coursematerials
Uploaded by
Mohamed Elmasry0 ratings0% found this document useful (0 votes)
98 views65 pagesASCP - Transfusion Practice, WAIHA
Original Title
coursematerials
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentASCP - Transfusion Practice, WAIHA
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
98 views65 pagesCoursematerials
Uploaded by
Mohamed ElmasryASCP - Transfusion Practice, WAIHA
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 65
6730 Transfusion PracticesWarm Autoimmune
Hemolytic Anemia, Transfusion Triggers, and Managing
Blood Component Recalls and Withdrawals
Kimberly W. Sanford, MD, FASCP, MT(ASCP)
Phillip J. DeChristopher, MD, PhD, FASCP
Glenn E. Ramsey, MD, FASCP
2010 Annual Meeting San Francisco, CA
AMERICAN SOCIETY FOR CLINICAL PATHOLOGY
33 W. Monroe, Ste. 1600
Chicago, IL 60603
Program Content and Disclosure
The primary purpose of this activity is educational and the comments, opinions, and/or recommendations expressed by the faculty or authors
are their own and not those of the ASCP. There may be, on occasion, changes in faculty and program content.
In order to ensure balance, independence, objectivity, and scientific rigor in all its educational activities, and in accordance with ACCME
Standards, the ASCP requires all individuals in positions to influence and/or control the content of ASCP CME activities to disclose whether they
do or do not have any relevant financial relationships with proprietary entities producing health care goods or services that are discussed in the
CME activities, with the exemption of non-profit or government organizations and non-health care related companies. These relationships are
reviewed and any identified conflicts of interest are resolved prior to the activity. Faculty are asked to use generic names in any discussion of
therapeutic options, to base patient care recommendations on scientific evidence, and to base information regarding commercial
products/services on scientific methods generally accepted by the medical community. All ASCP CME activities are evaluated by participants for
the presence of any commercial bias and this input is utilized for subsequent CME planning decisions.
The individuals below have responded that they have no relevant financial relationships with commercial interests to disclose:
Course Faculty:
Kimberly W. Sanford, MD, FASCP, Phillip J . DeChristopher, MD, PhD, FASCP and Glenn E. Ramsey, MD, FASCP
Annual Meeting/ Weekend of Pathology & Educational Course Planning Committee/ Commission Members and Staff:
N. Volken Adsay, MD, FASCP Carolyn Burns, MD, FASCP Francois Cady, MD, FASCP
Michele L. Best, MT(ASCP), MASCP Nikolaj Lagwinski, MD Sondra Moran, MT(ASCP)
Cyril Fisher, MD, DSc, FRCPath, FASCP Steven H. Kroft, MD, FASCP Stacy Kiff, MT(ASCP)
Syed A. Hoda, MD, FASCP William E. Schreiber, MD, FASCP Suzanne Ziemnik, M.Ed.
Monica I. Ruiz, MD Daniel D. Mais, MD, FASCP
Kimberly W. Sanford, MD, FASCP Robert A. Goulart, MD, FASCP
Peggy Soung Sullivan, MD, FASCP Karen A. Brown, MS, MLS(ASCP)
Neil Crowson, MD, FASCP Lynnette G. Chakkaphak, MS, MT(ASCP
Syed Ali, MD, FASCP Amy J . Wendel, SCT(ASCP)
The individuals below have disclosed the following financial relationships with commercial interests:
Course Faculty:
Planning Committee/ Commission Members and Staff:
Elizabeth A. Wagar, MD, FASCP Becton Dickinson Honorarium Scientific Advisory Board
David J . Dabbs, MD, FASCP USLabs; Ventana Med Systems; Consultant service fees; Consulting
Dako
Dennis P. OMalley, MD, FASCP Clarient Salary, Stock Options Employee
David Grignon, MD, FASCP Integrated Lab. Automation Stock Shareholder
Solutions
Eric D. Hsi, MD, FASCP Allos; BD; Eli Lilly; Honorarium; Research Consultant
Facet Biotech Support
Charles Lombard, MD, FASCP Broncus Tech; Asthmatx; Stock Consultant
Neomend
Michael D. Feldman, MD, PhD, FASCP Aperio Technology, Inc., CRI Stock Options; Advisory Board; Consultant
Bioimagene Sponsored Research &
License Patents
Peter Banks, MD, FASCP Aperio Technology, Inc. Future Stock Options; Advisory Board; Consultant
Cambridge Past Stock Options
Andrew Churg, MD, FASCP Various Law Firms Regarding Consulting Fee Consultant/Expert Witness
Asbestos Disease
J oel Greenson, MD, FASCP Glaxo Smith Kline; Roche/ Consulting Fee Consultant
Genentech; Millennium Pharam;
Genetics Squared
Copyright 2010 by the American Society For Clinical Pathology
All Rights Reserved. Printed in the United States of America.
No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form
or by any means - electronic, mechanical, photocopying, recording, or otherwise
without the prior written permission of the publisher.
6730 Transfusion PracticesWarm Autoimmune Hemolytic Anemia, Transfusion Triggers, and
Managing Blood Component Recalls and Withdrawals
Review the complex serologic findings of warm autoantibodies and recommendations for transfusion
and communication with clinicians for these patients. You will learn about current transfusion targets,
data that indicate that transfusion triggers may be dangerous, and how to manage blood component
recalls and withdrawals to ensure patient safety. You will leave with the ability to:
Recognize, evaluate and assess serologic findings of patients with autoantibodies and warm
autoimmune hemolytic anemias and discuss transfusion recommendations.
Review current transfusion targets and analyze the data of why transfusion triggers may be
dangerous.
Review management of blood component recalls and withdrawals.
Directors:
Kimberly W. Sanford, MD, FASCP, MT(ASCP)
Virginia Commonwealth University
Phillip J . DeChristopher, MD, PhD, FASCP
Loyola University Medical Center
Glenn E. Ramsey, MD, FASCP
Northwestern University Medical School
3.0 CME Credits
TM
MOC: MK PC PBL
1
Warm autoimmune hemolytic
anemia and transfusion
American Society for Clinical Pathology
S F i San Francisco
Course 6730
Kimberly W. Sanford, M.D.
Department of Pathology
Virginia Commonwealth University
Kimberly W. Sanford, M.D.
Department of Pathology gy
Virginia Commonwealth University
CME Disclosure:
No relevant financial interests
Objectives to Learn
Etiologies of autoimmune hemolytic
anemia (AIHA)
Pathogenesis of warm autoantibodies &
drug induced hemolytic anemia drug induced hemolytic anemia
Lab tests evaluating warm autoantibodies
Complications of pretransfusion testing
Communicating transfusion
recommendations
2
Autoimmune hemolytic anemia
(AIHA)
IgG and/or IgM antibodies bind to red blood cell
(RBC) antigens and initiate destruction of
autologous RBCs
Complement (C) system
Reticuloendothelial system y
Does not require exposure to allogenic blood
Alloimmune hemolytic anemia
Exposure to allogenic RBC required
Pregnancy
Transfusion
AIHA
Incidence
1:80,000 100,000 annually
Affects all ages
Peak: 4-5
th
decade
Primary AIHA
Idiopathic Idiopathic
Secondary AIHA
Lymphoproliferative disorders
Systemic Lupus Erythematous (SLE)
Females higher incidence of primary and secondary
AIHA
Classification of AIHA by frequency
Warm AIHA (WAIHA): 70%
primary (idiopathic)
secondary
Cold AIHA (CAIHA): 15%
primary (idiopathic)
secondary
Drug induced immune hemolytic anemia: 12%
Paroxysmal cold hemoglobinuria : 2%
*Petz LD, Garratty G. Acquired immune hemolytic anemias. New York:
Churchill Livingstone, 1980.
3
Responsible Antibodies
41 % Warm autoantibodies (autoabs)
32% Cold autoabs
18% Drug induced abs
7% Mixed abs
2% PCH/DL abs
*Sokol RJ, Hewitt S, Stamps BK. Acta Haematol 1983;69:266-74
Warm Autoimmune Hemolytic
Anemia
Primary idiopathic
Most common
Typical testing pattern
Panreactivity
60%autoabs detected in saline 60% autoabs detected in saline
90% autoabs detected in PEG, gel or solid phase.
30% also have cold autoabs
Normal titers at 4 C
No reactivity at 30-37C
*Petz LD, Garratty G. Acquired immune hemolytic anemias. New York: Churchill
Livingstone, 1980.
Warm autoantibodies
Antibody detection methods that use PEG,
enzymes, columns, or solid-phase red
cell adherence generally enhance g y
autoantibodies.
*Leger RM. The positive direct antiglobulin test and immune-mediated
hemolysis. In: Roback J. ed: Technical Manual 16
th
edition.
4
WAIHA Pathophysiology
Microspheroctye in
C
C
C
Intravascular
hemolysis
Spleen
Remain
sequestered
Microspheroctye in
circulation
Phagocytosis by
macrophage
RBC autoab
Ab reacts with intrinsic RBC antigens
May or may not cause pathological effects in vivo
Study performed at UCLA
100 autoabs
29% hemolytic
Presence or absence of alloabs and hemolysis was
significant different
*Blackall DP, Wheeler CA. Transfusion 2007; 47:1332.
Presentation of patients with warm
autoabs
Highly variable
Asymptomatic
No decreased RBC survival No decreased RBC survival
Life threatening anemia
Fatigue, dizziness, pallor, palpitations, dyspnea
Dependent on marrow response
5
Etiologies of Autoabs
Immunoregulation breakdown
Loss of T-cell suppressor regulation
Overactive B cells
Leads to emergence of autoabs
.
Triggers for autoab formation
Infections
Increase ability of macrophages to phagocytose
coated RBC
Inflammatory process/disease a ato y p ocess/d sease
Lymphoproliferative disorder
Medications
Fludarabine
* Borthakur G, OBrien S, Wierda WG, et al. Br J Haematol
2007;136:800-5
Transfusion Stimulated Antibodies
Transfusion can stimulate allo-abs and autoabs
RBC autoimmunization recognized 60 years ago
*Dameshek W, Levine P. NEJM 1943;228:641-4.
Average incidence of alloimmunization after
t f i i 2 10% transfusion is 2-10%
*Hewitt, PE, et al. Br J Haematol 1988. 69:541-4.
*Schonewille H, et al. Transfusion 2006. 250-6.
Chronically transfused patients alloimmunization
rate 18-60%
*Rosse WF, et al.Blood 1990. 76:1431-7.
*Vichinsky EP, et al. NEJM 1990. 322:1617-21
6
Transfusion stimulated Autoabs
8535 patients transfused, 34 cases of +DATs
25% of eluates were panreactive
Autoab formation
Persisted beyond life span of transfused RBC
abs adsorb onto recipients antigen-negative RBC
Conclusions:
Alloimmunization stimulant for autoab formation
Autoab production after transfusion is higher than
reported.
*Ness PM, et al. Transfusion 1990. 30:688-93
2004 study by Young et al.
2618 patients transfused
121 patients developed autoabs
Positive direct antiglobulin test (DAT) and indirect antiglobulin
test (IAT)
41 patients developed alloabs and autoabs
12 developed autoabs temporally associated
with alloimmunization
80 ti t d l d t b 80 patient developed autoabs
Conclusions
Autoimmunization complication of transfusion
Conservative transfusion practices
*Young PP, et al Transfusion 2004. 44:67-72.
Antibodies coating RBC
Quantity and type of immunoglobulin coating RBC
influences hemolysis
IgG1 and IgG3 versus IgG2 and IgG4
Macrophage receptors for IgG1 and IgG3
IgG1 major subclass in AIHA
Complement on RBC accelerates removal
Spleen and liver remove coated RBC
*Gehrs BC, Friedberg RC. American Journal of Hematology 2002
7
Lab detection of autoabs
Ab screens and panels are panreactive.
Negative if high binding constant or low titer.
Autocontrol is positive
Patient RBC & patient plasma
DAT results for warm autoab
IgG positive +/- C3b
The predictive value of positive DAT
83% in a patient with hemolytic anemia
1.4% in patient without hemolytic anemia
*Kaplan HS, et al. Diagnostic Med 1985;8:29-32
DAT: sensitized RBCs + AHG
AHG reagent
Patient RBC
Patient RBC
Patient RBC
Antibody coating RBC
in vivo
DATs
Healthy adults
50-90 IgG molecules/RBC
5-40 C3d molecules/RBC
*Garratty G. Transfus Med Rev 1987;47-57.
*Freedman J. Transfus Med Rev 1987; 58-70
DAT detection
100-500 molecules of IgG per RBC
400-1100 molecules of C3d per RBC
1-15% of hospital patients have positive DATs
*Petz LD, Garratty G. Immune hemolytic anemias. 2004
8
Causes of positive DATs
Positive DATs with/without shortened RBC survivial
Autoabs to intrinsic RBC antigens
Alloabs bound to transfused donor RBC
Passively acquired alloabs
Maternal alloabs on fetal RBC
Abs against drugs bound to RBC membrane.
IgG or complement coating of cells due to
medications.
Adsorbed proteins/immunoglobulins on RBC
Hypergammaglobulinemias
IVIg
Investigating +DAT AABB Technical
Manual 15
th
ed
Elutions
Perform on all samples with IgG positive DAT
No need to perform eluate on C3 positive only
DAT DAT
Eluates can concentrate small amounts of IgG
antibody undetectable in plasma.
9
Elutions
Ab dissociates
from RBC
Elution
methods:
1. Heat
2. Lui Freeze-thaw
3. Acid elution
4. Digitonin acid
Test eluate with panel of cells
Alloantibody specificity
Delayed serologic transfusion reactions (DSTR)
Acute or delayed hemolytic transfusion reactions
(DHTR)
Hemolytic disease of the fetus or newborn (HDFN)
Panreactive eluates
Autoantibody
Eluate in WAIHA
Warm autoabs confirmed by elution
upon initial diagnosis
during pretransfusion testing during pretransfusion testing
Eluate reacts with virtually every cell tested.
10
Autoab specificity
Typically panreactive
Specificity for simple Rh antigens
D C E c e D, C, E, c, e
More commonly detected in LISS
Other specificities include
LW, Kell, Kidd, Duffy and Diego
Non reactive eluates
Eluate is Anti- A or B abs
Test A
1
and B cells with eluate.
Ab to low incidence antigen
79 % of hospital patients with + DATs have 79 % of hospital patients with DATs have
nonreactive eluates
One explanation for this is the non-specific uptake
of proteins on RBC especially in patients with
increased gamma globulin levels.
Medication
*Toy PT, Chin CA, Reid ME, Burns MA. Vox San 1985; 49:215-20.
3 Mechanisms of drug induced HA
Drug adsorption
Drug dependent Drug dependent
Autoimmune
induction
AABB Technical Manual 15th edition
11
Drug Adsorption Mechanism
Medication/metabolites bind to RBC
Penicillin covalently binds to RBC proteins
Anti-medication IgG ab sensitizes cell for
immune clearance immune clearance
DAT usually positive for IgG, eluate negative
Rarely causes hemolysis
7 days before hemolysis starts
Extravascular hemolysis
Drug adsorption Mechanism
AABB Technical Manual 15
th
edition
Drug-dependent Ab Mechanism
Medication/metabolite
binds transiently to
proteins on RBC
surface
Creates immunogen
Ab production Ab production
Binds to
drug/metabolites on
RBC
IgG /IgM can activating
C
Small amount of drug
required in sensitized
patients
AABB Technical Manual 15th edition
12
Drug dependent mechanism
Hemolysis abrupt, severe
Hours or days
Intravascular hemolysis
Massive hemoglobinemia/hemoglobinuria
Renal failure, DIC, shock
Medications
2
nd
and 3
rd
generation cephalosporins
NSAIDs
Autoimmune induction mechanism
Medication induces RBC
autoab
Medications
- Methyldopa, levodopa,
procainamide
11-36% of patients form
+DAT after 3 6 months +DAT after 3-6 months
<1% have clinical
hemolysis
Hemolytic anemia
Mild-moderate
extravascular hemolysis
Gradual anemia
Hemolysis may persist
weeks-months after drug
stopped
AABB Technical Manual 15th edition
Treatment for Drug induced HA
Withdraw the drug
Some instances hemolysis may persist but short
lived lived
Rarely requires treatment
13
Summary of Drug Induced HA
Type DAT +
due to
Serum Antibody Hematologic
Manifestations
Drug adsorption IgG, C3d Ab reacts with drug
coating RBC
Moderate
hemolysis,
extravascular
Drug-dependent C3d Ab to drug & RBC
membrane
Abrupt, severe
intravascular
hemolysis
Autoimmune
induction
IgG Autoab to RBC
membrane
Mild-moderate,
extravascular
hemolysis
Adsorption techniques
Detect underlying alloabs
Pretreatment of autologous cells to remove bound
autoab for adsorption of autoabs
Treatment:
Heat cells at 56C for 3-5 minutes and treatment with proteolytic
enzymes
ZZAP: mix of papain/ficin and DTT
PEG treatment
Treated cells incubated with plasma
Autoadsorptions
Multiple sequential autoadsorptions may be
necessary
Adsorbed plasma should have no reactivity with Adsorbed plasma should have no reactivity with
autologous RBC.
Perform full panels using absorbed plasma
14
Alloadsorptions
Patients transfused within 3 months
Reticulocyte harvest
Allogenic adsorptions
Use donor cells of different phenotypes to adsorb
autoabs autoabs
Only look to rule out clinically significant abs
Rh antigens, K, Fys, Jks, Ss.
R
1
R
1
, R
2
R
2
, rr
Abs to high frequency antigens cannot be excluded
since donor cells express antigen
Alloadsorption
Alloadsorption performed several times until nonreactive
>3 adsorptions can dilute specimen
React adsorbed plasma with panel cells p p
Phenotypes of adsorbing cells are known
If adsorb with Jk(a-) cell
Adsorbed plasma reacts with Jk(a+) panel cell
Interpret as underlying anti-Jk
a
Transfusion
Autoantibodies mask underlying
alloantibodies that increases the risk
of a hemolytic transfusion reaction of a hemolytic transfusion reaction,
therefore conservative transfusion
should be practiced
15
Selecting blood products
Adsorption techniques ruling out alloab before
transfusion
Underlying alloab, select ag negative blood
Autoab with ag specificity Autoab with ag specificity
Ag negative if active hemolysis
If no hemolysis, ag negative blood debatable
Even ag negative blood hemolyzed
Consider zygosity
Phenotypically matched RBC
Patient not chronically transfused
Not required
Chronically transfused patients
Patients with sickle cell anemia
C, E, K matched in sickle cell patients
Frequency of C, E, K, Fya, Fyb, Jkb and S ags different than
donors
Anti-C,E, K account for 60-98 % of allo-abs
Decreased alloimmunization rate from 3 to 0.5% per unit
*Vichinsky, EP et al. Transfusion 2001.1086-92
Crossmatching and Transfusion
Selecting blood products
Antigen neg for underlying alloabs
Perform autocontrol with full crossmatches
Least incompatible with autocontrol p
Transfusion should be reserved for life-threatening
anemia
Need to increase oxygen carrying capacity
Patients at risk
Cardiovascular disease
Cerebrovascular ischemia
16
Communication with clinicians
Direct contact with clinician
Gather patients history to assess risk of alloimmunization
Transfusion & pregnancy history
Determine need for transfusion Determine need for transfusion
Symtomatic anemia, bleeding, cardiovascular disease, other
comorbidities
Discuss investigation for underlying alloabs
Alloabs present or absent
Assure blood is ABO compatible
Risk of alloimmunization
Discuss laboratory investigation
Search for compatible blood is futile
Possibly phenotype patient
Clinician and blood bank physician together should
approve transfusion
Risk vs. benefit clinical decision
Conservative transfusion practice
Do not deprive patient of transfusions when anemia is severe
Transfuse slowly
If hemoglobin decreases consider underlying alloab
*Ness PM, Transfusion 2006. 46:1859-62.
Transfusing patients with WAIHA
Monitor closely & transfuse when medical team present
Patients with little in vivo destruction tolerate
transfusions
Survival of transfused RBC is similar to patient RBC
Suppress erythropoiesis Suppress erythropoiesis
Possibly intensifies autoantibody titer
Debatable
Increased risk of hemolysis
Hemolyze auto and transfused RBC
Increases complexity of serologic testing
Weigh risks vs. benefits of transfusion
17
Frequency of testing patient
AABB Standards require new sample every 3 days.
Some argue this is too frequent, unnecessary and
too costly for minimal reward.
Average incidence of alloimmunization after
transfusion is 2-10%
*Hewitt, PE, et al. Br J Haematol 1988. 69:541-4.
*Schonewille H, et al. Transfusion 2006. 250-6.
Alloimmunization rate in patients
with warm autoabs
Leger and Garratty demonstrated 40%
alloimmunization rate with alloantibodies after
transfusion
*Leger RM, Garraty G. Transfusion 1999:39:11-6
Branch and Petz reviewed 7 independent studies Branch and Petz reviewed 7 independent studies
demonstrated 12-40 % alloimmunization rate
*Branch DR, Petz LD. Transfusion 1999:39:6-10
Incidence of autoabs detected in coexistence with
newly detected alloab is up to 50%
*Wheeler CA, et al. Am J Clin Pathol 2004. 680-5
Summary of studies
Exclusion of underlying alloantibodies important
in this high risk group
I d ti it t l ith Increased reactivity not always seen with some
underlying alloantibodies.
18
Medical therapies
Glucocorticoids
Prednisone 60 mg/day for 10-14 days, then taper
70% demonstrate improvement
10% non-responders, can attempt 80-100 mg/day
Inhibits monocyte-RBC interaction in spleen
Rituximab
Monoclonal CD20 ab used to treat immune cytopenias
375mg/m
2
weekly for 4-6 weeks
Smaller maintenance dose in responders
Other therapies
Immunosuppressants
Cyclospoirine, mycophenolate, antithymocyte globulin
IVIG
Less effective with WAIHA vs. ITP
Blocks Fc receptors on macrophages in RES
Cytotoxic drugs Cytotoxic drugs
Use for patients not responding to steroids
Splenectomy is contraindicated
Azathioprine, cyclophosphamide, chlorambucil
Splenectomy
Delay until medical therapy fails
2/3 of patients demonstrate partial or complete response
Iron and Folate supplements
Conclusions
Patients with + autocontrols should have DATs
performed.
Positive broad spectrum DATs need monospecific IgG
and complement DAT performed.
Eluates
Adsorption techniques
Crossmatches
Communication with clinicians
Transfuse conservatively
Medical or surgical therapies
Treat underlying disease
19
References
Petz LD, Garratty G. Acquired immune hemolytic anemias. New York: Churchill
Livingstone, 1980
Sokol RJ, Hewitt S, Stamps BK. Autoimmune haemolysis: Mixed warm and cold
antibody type. Acta Haematol 1983;69:266-74
Blackall DP, Wheeler CA. Contemporaneous autoantibodies and alloantibodies.
Transfusion 2007;47:1332.
Borthakur G, OBrien S, Wierda WG, et al. Immune anaemias in patients with chronic
lymphocytic leukaemia treated with fludarabine, cyclophosphamide and rituximab-
incidence and predictors. Br J Haematol 2007;136:800-5.
Dameshek W. Levine P. Isoimmunization with rh factor in acquired hemolytic anemia.
N Engl J Med 1943;228:641-4. g ;
Hewitt PE, Macintyre EA, Devenish A, et al. A prospective study of the incidence of
delayed haemolytic transfusion reactions following peri-operative blood transfusion.
Br J Haematol 1988;69:541-4.
Rossee WF, Gallagher D, Kinney TR, et al. Transfusion and alloimmuniztion in sickle
cell disease. The cooperative study of sickle cell disease. Blood 1990. 76:1431-7.
Vichinsky EP, Earles A, Johnson RA, Hoag MS, Williams A, Lubin B.
Alloimmunization in sickle cell anemia and transfusion of racially unmatched blood.
NEJM 1990. 332:1617-21.
Gehrs BC, Friedberg RC. Autoimmune hemolytic anemia. American Journal of
Hematology 2002; 69: 258-71.
Ness ONm Shirey RS, Thoman SK, et al. The differentiation of delayed serologic and
delayed hemolytic transfusion reactions: incidence, long-term serologic findings and
clinical significance. Transfusion 1990.30:668-93
References
Schonewille H, van de Watering LMG, Loomans DSE, et al. Red blood cell
alloantibodies after transfusion: factors influencing incidence and specificity.
Transfusion 2006; 46:250-6.
Kaplan HS, Garratty G. Predictive value of direct antiglobulin test results. Diagnostic
Med 1985;8:29-32.
Garratty G. The significance of IgG on the red cell surface. Transfus Med Rev
1987;1:47-57.
Freedman J. The significance of complement on the red cell surface. Transfus Med
Rev 1987;1:58-70.
Toy PT, Chin CA, Reid ME, Burns MA. Factors associated with positive direct
antiglobulin tests in pretransfusion patients: a case control study. Vox Sang 1985;
49:215-20
Vichinsky EP, Luban NLC, Wright E, et al. Prospective RBC phenotype matching in a
stroke-prevention trial in sickle cell anemia: a multicenter transfusion trial. Transfusion
2001;41:1086-92.
Leger RM, Garratty G. Evaluation of methods for detecting alloantibodies.
Transfusion 1999;39:11-16.
Wheeler CA, Calhoun L, Blackall DP. Warm reactive autoantibodies : clinical and
serologic correlations. Am J Clin Pathol 2004;122:680-5.
Ness PM. How do I encourage clinicians to transfuse mismatched blood to patients
with autoimmune hemolytic anemia in urgent situations. Transfusion 2006. 46:1859-
62.
Leger RM. The positive direct antiglobulin test and immune mediated hemolysis. In:
Roback J. Combs MR, Grossman B, et al. eds. Technical Manual. 16
th
edition.
Bethesda, MD: AABB Press 2008:489-521.
Duffy TP. Autoimmune hemolytic anemia and paryoxysmal nocturnal hemoglobinuria.
In: Simon TL, Snyder EL, Stowell CP, et al. eds. Rossis Principles of Transfusion
Medicine. 4
th
edition. Bethesda, MD: AABB Press 2009:321-43.
9/21/2010
1
Transfusion Practices:
Managing Blood Component
Recalls and Withdrawals
American Society for Clinical Pathology
San Francisco 2010
Course 6730
1
Course 6730
Glenn Ramsey, MD
Department of Pathology
Northwestern University
Chicago, Illinois
Transfusion Practices:
Managing Blood Component
Recalls and Withdrawals
American Society for Clinical Pathology
San Francisco 2010
Course 6730
2
Course 6730
Glenn Ramsey, MD
CME Disclosure:
No relevant financial interests
Transfusion Practices:
Managing Blood Component g g p
Recalls and Withdrawals
Glenn Ramsey, MD
Department of Pathology
Northwestern University, Chicago, IL
LochDunvegan, Isle of Skye, Scotland
9/21/2010
2
Outline
Recalls and market withdrawals
Biological product deviation reports
Estimated 1 in 320 blood components
General management
4
Compliance, SOP, training, rapid action
Physician notification
Tangible risk of infection or adverse effect
Selected problems
High-risk transfusion?
More emerging infections
Types Of Notices About
Issued Blood Components
Lookback--donor now has infection (HIV, HCV, etc)
Recallproduct in violation of law, subject to legal action
5
Market Withdrawalless significant violation
Quarantineisolate unit, pending above determination
But most units have been transfused before notices
Platelets 5 days, RBCs 42 days storage
HIV & HCV Lookbacks
21 CFR 610.47, revised 2008
New lookbacks for HIV+& HCV+donors found now:
Donor services--
Quarantine in-dated products within 3 days
If donor confirmed+, trace past units as far back
as records permit (unless >12 months before a
ti t t)
6
negative test)
Transfusion services--
Trace recipients within 12 weeks of receiving
notice: Reasonable attempts
Incompetent or minor patient: find legal rep or
relative
Deceased recipient: HCV notice not required
HIVnext of kin notified
9/21/2010
3
Lookback Reports from Blood Establishments to FDA
Lookback Rule Revised, 2008
300
400
500
600
HCV
HIV
7
0
100
200
300
FY05 FY06 FY07 FY08 FY09
FDA Bi ol ogi cal Product Devi ati on Report, FY09
HIV
HBV
Recalls
21 CFR 7.3, 7.40 et seq.
Remove or correct products in violation of FDA law and
subject to legal action
Consignees should carry out instructions immediately
Class I: reasonable probability of serious adverse
8
Class I: reasonable probability of serious adverse
consequences or death
Class II: temporary or reversible adverse consequences
or remote probability of serious adverse conseq.
Class III: not likely to cause adverse consequences
Published in FDA Enforcement Report weekly
Ramsey G, Sherman LA. Transfusion 39:473,1999;40:253,2000
Bozzo T. Transfusion 39:439, 1999
Market Withdrawals
Products with minor violations, not subject to legal action
May be beyond control of manufacturer
E.g., post-donation information about donor
Not published by FDA, numbers of withdrawals or units
i l d k
9
involved are unknown
Biological product deviations often lead to withdrawals
9/21/2010
4
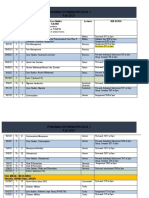
2006 Recalls
FDA Enforcement Reports (weekly), 2006
Ramsey G, Transfusion 47(suppl):34A, 2007
1,130 blood component recalls of 13,758 units
10
About 1 in 2,000 available blood components recalled
Common Recal l Reasons Wi thin Categori es, 2006
Other, 780
629
362 Temp
321 License
Other, 1332
2500
3000
3500
4000
4500
5000
i
t
s
11
411 Malaria
1062
Donor
Suitability
1686
Store Temp
1421
Arm Prep
1264
GMP 121 vCJD
313 Ship Temp
1342
Sterility 926
QC
Clots
Other, 331
Other, 104
Other, 61
0
500
1000
1500
2000
2500
Preparation Collection Store/Ship Inadeq Donor Hx RiskFactors
U
n
Biological Product Deviation Reporting
21 CFR 606.171, instituted 2001
Key elements of BPD scope:
Manufacturing
E.g., patient specimen, but not patient care
12
g , p p , p
Deviations affecting safety, purity, potency
No longer errors and accidents
Only if product was distributed
If not distributed, not reportable
Investigation still required (cGMP)
9/21/2010
5
Biological Product Deviation Reports
Licensed Facilities, FY 09 = 25,481
Donor-Related
Screening 1914
Collection 929
General
QC, Distribution 1662
Component Prep 420
FDAAnnual Summary, BPD
Reports, www.fda.gov
Collection 929
Viral Testing 39
Deferral 37
Post-Donation
Information 18,558
Component Prep 420
Routine Testing 289
Labeling 749
Miscellaneous 884
Biological Product Deviations:
Post-Donation Information
Travel
Malaria
vCJ D
Post-donation illness
History tattoo <12 mo
History tissue or organ tpt
Hx prior disease/surgery
Hx hepatitis or exposure
Sex partner: HIV grp O risk
Other exposures
14
Male-male sex
Medications
Antiandrogens
Retinoids
IV drug use
Pre- or post-donation
positive viral marker
Cancer before or after
donationno longer BPD
Biological Product Deviations:
Post-Donation Information
Highlighted by NIH/NHLBI for study by REDS-II*
Travel---malaria (tropics), variant CJ D (Europe)
Medicaldeferring illnesses or medications
High risk behaviors/exposure
Sexual (High-risk partner male sex with male)
*Retrovirus Epidemiology Donor
Study II
Sexual (High-risk partner, male sex with male)
Nonsexual (IVDU, jail)
Blood/disease exposurestattoo, piercing, needlestick
Transfusion 49 Suppl 3S:52A (x2), 2009--AABB meeting
Fed Reg 75:8080, 2/23/2010, planned donor survey
9/21/2010
6
Post-Donation Information: Donor Analysis
Licensed facilities, FDA BPD Annual Report, FY09:
93% of PDI donors knew information before donation
Only 7% discovered their PDI after donation
PDI discovery: later donation 93%; donor call 5%
16
Donor survey, Transfusion 49 Suppl 3S:52A, 2009
48% made two ineligible donations
Trends: male, older, better educated (travel)
Common Blood Components Recalls, vs.
Biological Product Deviations (Licensed)--Post Donation Information
1261 Other PDI
1159 Cancer 817 Tattoo
618 Male sex
603 Finasteride
421 IVDU
5398
Other
15,000
20,000
25,000
BPDs for PDI
(Includes 44 Potential Recalls)
PDI: 80% of all BPDs
Half involve >1 donation
3 components per BPD?
17
6562
Malaria
5659
vCJD
0
5,000
10,000
Preparation Collection Store/Ship Inadeq Donor
Hx
Risk Factors PDI BPDs
Units in Recalls:
Blood Component Notices in US:
Estimated Frequency
Recalls: 13,758 units in FDA FY06 Enforcement Reports
Market withdrawals:
Est. from Biological Product Deviations (FDA FY08)
Post-donation information, ?3 components/report:
18 500 BPDs x 3 =55 500 units
18
18,500 BPDs x 3 =55,500 units
Other BPDs, ?2 components/report:
7,000 BPDs x 2 =14,000 units
Estimated 83,000 units recalled or withdrawn
26,568,000 units available in US (AABB/HHS 2006)
0.31%, or 1 in 320 blood components in US
Northwestern Memorial Hospital, Chicago: 0.45%
9/21/2010
7
Outline
Recalls and market withdrawals
Biological product deviation reports
Estimated 1 in 320 blood components
General management
19
Compliance, SOP, training, rapid action
Physician notification
Tangible risk of infection or adverse effect
Selected problems
High-risk transfusion?
More emerging infections
CAP Lab Accreditation Checklist, 2010
Transfusion Medicine
TRM.42120, Phase II:
Identify/quarantine units from donors now reactive
in screening test
TRM.42135, Phase I:
20
Have SOP for managing quarantines, recalls,
withdrawals
TRM.42170, Phase II:
Follow FDA and CMS regulations/guidelines for
recipients given potentially infectious transfusion
HIV/HCV lookbacks & other guidelines
AABB Standards, 25th ed., 2008
7.0. Deviations, Nonconformances, and Complications
7.1 Nonconformances
7.1.4 Released Nonconforming Blood, Components
Evaluated to determine effect on quality
When quality may have been affected, report to
customer(other department or facility)
21
customer (other department or facility)
Maintain records of nature and action
Keep five years
7.4.6. Look-Back. Per FDA rules and recommendations
[FDA: Keep lookback records 10 years from notice]
9/21/2010
8
General Considerations I
Have a procedure for managing notifications
Training
Promptly follow instructions from blood supplier
24/7 access to fax or secure e-mail for large
22
notices
Quarantine units physically and electronically
Medical evaluation as needed
Get more info from blood supplier if needed
Donor (was/will be) tested later?
Ramsey, Transfusion Med Rev 18:36, 2004
General Considerations II
Document actions
If phone, then paper; track resolution
Database by unit? By recipient?
Keep records as required (5 yrs or lookbacks 10 yrs)
23
Keep records as required (5 yrs, or lookbacks 10 yrs)
Was Source Plasma or Recovered Plasma made and
sent elsewhere?
Oversight Options
Transfusion committee
Approve policies
Review significant notices
Improve awareness of potential for post-transfusion
bl
24
problems
Risk management/legal
Serious problems or large recalls
Patient/public relations assistance
9/21/2010
9
25 LochSnizort, Isle of Skye, Scotland
Outline
Recalls and market withdrawals
Biological product deviation reports
Estimated 1 in 320 blood components
General management
26
Compliance, SOP, training, rapid action
Physician notification
Tangible risk of infection or adverse effect
Selected problems
High-risk transfusion?
More emerging infections
Inform Transfusing Physician?
Our general approaches:
As required or recommended by FDA-yes
HIV, HCV lookback
If tangible potential for disease transmissionyes
27
If potential for transfusion reaction (sterility, storage):
check for reaction report
9/21/2010
10
Notify Physician? Yes or Suggested Yes:
FDA rule:
HIV lookback (patient or next of kin)
HCV lookback (patient alive)
Other donor/unit infection, confirmed:
HBV sAg or NAT*, Chagas, West Nile NAT
Bacteria in component or co-component
28
Bacteria in component or co component
Tangible potential infection risk:
HIV or hepatitis risk factor*
Malaria travelhigh-risk region and cellular unit
Improper donor screening or testing*
*Unless later donor testing rules out window period
Viral Marker Windows
Seroconversion periods important
Timing of donor exposure before donation
29
Timing of donor exposure before donation
Timing of subsequent testing (interim donations)
May rule out recipient exposure in some cases
When to test patients after transfusion
Window Periods (days)
Anti-HIV mean 22 range 6-38
HIV MP-NAT 9 7-12
Anti-HCV 70 54-192
HCV MP NAT 7 NA
30
HCV MP-NAT 7 NA
HBsAg 38-43 (06) 37-87 (05)
HBV MP-NAT 32-38 (06) NA
MP-NAT=Mini-pool nucleic acid test NA=not available
Busch, Transfusion 45:254, 2005
Kleinman, J Clin Virol 36(S1):S23, 2006
9/21/2010
11
Notify Physician? It Depends-I
If transfusion reaction occurred:
Donor or unit bacterial infection risk
Antibiotics, arm preparation, other sterility concern
Component content problem
Clots, hemolysis
St bl
31
Storage problem
Temperature, incorrectly extended expiration
Incorrect CMV status or leukoreduction
If recipient was at risk for CMV
Teratogenic medication (antiandrogen, retinoid)
If recipient was pregnant
Notify Physician? It Depends-II
Labeling problem:
Compatibility: blood type, crossmatch, antigen typing
If reaction or potential for delayed reaction
32
Collection bag or apheresis device problem
Evaluate details
Notify Physician? Suggested No:
Post-donation information:
vCJ D residence risk
Malaria travelMexico, Central America
Donor history of:
33
Cancer, post-donation illness
Viral screen, unconfirmed:
HBcAb; EIA+other markers not confirmed
Donor record/ID/unit number
No, but fix recipients unit-number record if needed
Unit quality control or volume
9/21/2010
12
Recalled Units: Physician Notification?
(Withdrawals Not Included)
Arm Prep or
Sterility
Storage Temp
RBCAg
Leukored?
Other
Other
Malaria, 411
44%: Txn Rxn?
5% More
Info
34
Other YES, 181
QC
Donor History
Adeq?
Other GMP
Testing, 204
46% No
6% Yes
Canadian Policy Recommendations
Heddle NM et al, Transfusion 48:2585, 2008
McMaster University survey; recommendations
Recipient notification issues include:
Develop national or provincial guidelines
35
Notices to hospitals should include recommendations
Hospital SOPs should address decision-making
Health care personnel should be given adequate
information for recipient notification if needed
Educate hospital CEOs and risk management personnel
Outline
Recalls and market withdrawals
Biological product deviation reports
Estimated 1 in 320 blood components
General management
36
Compliance, SOP, training, rapid action
Physician notification
Tangible risk of infection or adverse effect
Selected problems
High-risk transfusion?
More emerging infections
9/21/2010
13
High Concern for Viral Exposure?
Donor with recent confirmed viral exposure or new
confirmed infection? HBV, HCV, HIV?
Consult infectious disease service for advice about
recipient: immediate counseling and treatment?
37
Post-exposure prophylaxis information:
National PEPLine (24 hr)
1-888-HIV-4911 (448-4911)
General HIV therapy consultation:
National HIV Warmline (8am-8pm ET M-F)
1-800-933-3413
Post-Exposure Prophylaxis
CDC post-exposure prophylaxis (PEP) guidelines
see MMWR Recommendations & Reports
50(RR-11), 2001: Occupational HBV/HCV/HIV
54(RR-02), 2005: Non-occupational HIV
54(RR-09) 2005: Occupational HIV
38
54(RR-09), 2005: Occupational HIV
57(RR-6), 2008: Mass-casualty HBV/HCV/HIV exposure
NY State Dept Health: www.ceitraining.org
Current NY guidelines
Adult or pediatric, occupational or not
Post-Exposure Prophylaxis Timing
HIV and HBVrapid therapy if possible
HIV: antiretroviral medications
CDC: ASAP, within hours rather than days (05)
NY--ideally <2 hr, and generally not after 36 hr
But max time cannot be stated with certainty
39
y
HBV: If exposee not immune:
HBV Immune Globulin and vaccine
Ideally <24 hr, but not after 14 days
HCV: No effective PEP, not recommended
9/21/2010
14
Chagas+ Donor Lookback
AABB Bulletin #06-08, 12/13/06, recommendations:
Withdraw prior in-dated products when donor screen+
Lookback on all confirmed-positive donors prior units
Confirmed=positive on second test (RIPA, IFA, other)
40
Include all frozen units?infectious, but data limited
As far back as records go
Lookback recipient testing: Few if any infected recipients
without their own exposure risk have been found
Donors in US not as infectious as Latin Amer donors
More Emerging Agents
AABB Task Force, Emerging Infectious Disease Agents
Stramer SL, Transfusion 49(suppl), Aug 2009
Highest priority (in addition to vCJ D):
Babesia
41
Dengue
2010: Chronic fatigue syndrome and XMRV
Xenotropic murine-leukemia-virus-associated retrovirus
Other MLV-related viruses?
Babesia
Intraerythrocytic parasite, regionally endemic
Dozens of transfusion cases, several fatalities
Current donor deferral for history of illness (AABB)
Donor testing under consideration
42
Issues for evaluating past transfusions from +donors:
Transmissions have been from RBCs only
Illness incubation 1-9 weeks
Recipient susceptibility factors (in tick inoculations):
Infants, elderly, immunosuppressed, asplenic
9/21/2010
15
Dengue
Flavivirus, arthropod-borne like WNV, tropical climes
Endemic in Caribbean and US-Mexico border areas
40-80% antibody rates
Puerto Rico donor pilot testing, Amer Red Cross
1 in 1400 donations viremic
43
1 in 1400 donations viremic
Two transfusion infections seen in SE Asia
Donor testing if done would be NAT
Issues for evaluating past transfusions from +donors:
Incubation period until illness 3-14 days
Short-term viremia before-during infection/illness
Perhaps 120d donor deferral after +NAT, like WNV?
Chronic Fatigue Syndrome (CFS) and XMRV
Gammaretroviruses: feline, murine leukemia (MLV) viruses
Xenotropic Murine-leukemia-virus-associated RetroVirus
CFS: >6 months of fatigue, weakness, myalgia, impaired
memory or concentration, insomnia (CDC.gov)
Some studies link XMRV to CFS and prostate cancer
FDA/NIH PNAS 8/23/10 MLV l t d i RNA i
44
FDA/NIH, PNAS 8/23/10: MLV-related virus gag RNA in
CFS patients 87%, blood donors 7%
No evidence for transfusion transmission to date, but
AABB, Canada, Australia/NZ blood services, 2010:
Donor deferral for history of CFS diagnosis
No guidance included on past donations of new deferrals
Implication for past transfused units unknown at this time
DuntulmCastle ruins (Clan MacDonald), Isle of Skye
Harris (tweed) on horizon
9/21/2010
16
Outline Summary
Recalls and market withdrawals
Biological product deviation reports
Estimated 1 in 320 blood components
General management
46
Compliance, SOP, training, rapid action
Physician notification
Tangible risk of infection or adverse effect
Selected problems
High-risk transfusion
More emerging infections
9/21/2010
1
Transfusion Transfusion Triggers Triggers
2010 ASCP Annual Meeting
Friday, October 29, 2010
Phillip J. DeChristopher, MD, PhD
Medical Director, Transfusion Medicine / Blood Bank / Apheresis
Professor of Pathology
Loyola University Medical Center
Maywood, Illinois
(T) 708-327-2609
E-mail: pdechristopher@lumc.edu
Lecture Objectives
Overview of Some Complications of
Transfusion
Blood Component Types to Consider
Indications for Blood Use
Non-indications for Blood Use
Situations where Blood Use is Beneficial
Simplified Principles of Blood Management
Before You Pull that Trigger, Heres a
Number of Things to Consider
9/21/2010
2
Adverse Effects of Allogeneic Transfusion
1
Infectious Complications
Viral, bacterial contamination of platelets*
(1:3000), others (vCJ D, WNV, Chagas Disease,
babesiosis, Dengue fever)
Febrile and allergic reactions
Hemolytic transfusion reactions* (clerical error)
Mistransfusion incidence 1:16,000
Other
Microchimerism (50% of trauma pts @ discharge/
30% @ 1 year)
2
, graft vs. host disease
SIRS, TACO (1:350)
3
, TRALI
4
*
* Leading causes of morbidity and mortality
1. Goodnough, Crit Care Med 2003;31(12S)
2. Utter, Transfusion 2006;46
3. Rana, Transfusion 2006;46
4. Toy, Crit Care Med 2005;33(4)
Transfusion therapy is a set of processes,
not just a product
Recruitdonor
Screendonor
Collectunit
Preparecomponents
Infectious diseases
Pre-TXtesting
Medical reasonto TX
Issueunit
Administer atbedside
Monitor &evaluate
Product: Blood safety
Entire process: Blood transfusion safety
testing
AfterS. Dzik, MD BloodTransfusionService, MGH, Boston
Practice Guidelines are a Kind
of Practice Parameter
Standards
Accepted principlesof patient management
Practice variation NOT expected p
Guidelines
Recommendations / strategies for patient management
Practice variation is reasonable
Practice Options
Practice variation expected
Incorporate substantial patient- and physician-specific
information
9/21/2010
3
Defining Practice Guidelines
Consensus statements that are
systematically developed to assist
practitioner and patient decisions about
appropriate health care for specific clinical appropriate health care for specific clinical
circumstances
Field MJ. Clinical practice guidelines: Directions for a new agency. Institute of
Medicine, Washington, DC, National Academy Press. 1990.
Grading the Level of Evidence
Grade I
Randomized, controlled trials
Grade II-1
Non-randomized, controlled trials Non randomized, controlled trials
Grade II-2 Controlled observational studies
(e.g., cohort studies)
Grade II-3
Uncontrolled observational studies
Grade III Descriptive studies; expert opinion
WW II Medic Administers IV Plasma to Wounded GI:
The Value of Blood Transfusion was Recognized
Before Randomized Controlled Trials
9/21/2010
4
Red Blood Cell Unit
The 1988 NIH Consensus Conference on
Perioperative RBC Transfusion
Transfuse red blood cells to increase
oxygen-carrying capacity in anemic
patients
?Death knell to the 10/30 Rule
NIH Consensus Development Panel. Perioperative red cell transfusions. JAMA 1988;260:2700-03.
Differing Views on the RBC
Transfusion Target
The Internists View
Anemia cannot be defined numerically
RBC's are transfused to symptomatic, anemic patients
A i d h l i l dt bidit & Anemia and hypovolemia lead to severe morbidity &
mortality
Promulgated a [Hgb] trigger of 7 g / dL as
reasonable
Blood transfusion is an outcome to be avoided
American College of Physicians. Practice strategies for elective red blood cell transfusion practice
policies. Ann Intern Med. 1992;116:403-06.
9/21/2010
5
Differing Views on the RBC
Transfusion Target
The Surgeons View - Developed 11 Policies
Transfusion needs should be assessed on case-by-case basis
Blood should be transfused 1 unit at a time
Limit allogeneic exposure g p
Transfusion trigger on a sliding scale, patient-specific
Perioperative blood loss prevented or controlled
Consider autologous alternatives
Maximize oxygen delivery to surgical patient
RBC mass increased or restored (e.g., use of Fe
+2
or EPO)
Document reasons for and results of transfusion
Hospital transfusion policies developed cooperatively & reassessed
regularly
Spence RK. Blood Management Practice Guidelines Conference. Surgical red blood cell
transfusion practice policies. Am J Surg. 1995;170(suppl. 6A):3S-15S.
Differing Views on the RBC
Transfusion Target
The Anesthesiologists View
[Hgb] is an inappropriate basis... for transfusion
Promulgated 6 g / dL as reasonable laboratorytrigger
Additional Influences urging decision to transfuse RBC
Patients cardiopulmonary reserve
The rate and magnitude of blood loss
Oxygen consumption
Atherosclerotic disease
ASATask Forces Practice Guidelines for Perioperative Blood Transfusion
and Adjuvant Therapies. Anesthesiology. 2006;105:198-208.
Developing Transfusion Targets: Incorporating
Laboratory Trigger Numbers & Clinical J udgment
9/21/2010
6
Developing Transfusion Targets:
Incorporating Clinical Judgment
Duration of anemia
Ongoing indication of organ ischemia
Patients intravascular volume
Normovolemic anemia well-tolerated
Potential or actual ongoing bleeding (rate and
magnitude)
Patients risk factors for complications of
inadequate oxygenation
Low cardiopulmonary reserve
High oxygen consumption
Who is At Risk from Intravascular
Volume Depletion?
Myocardial Ischemia
Coronary artery disease
V l l h t di Valvular heart disease
Congestive heart disease
Cerebral Ischemia
History of TIAs
Previous thrombotic stroke
Heberts Randomized, Controlled
Study in Critical Care
Studied 838 euvolemic ICU patients admitted with
[Hgb] <9.0 g/dL
418randomlyassignedtorestrictive transfusionarm 418 randomly assigned to restrictive transfusion arm
RBC transfused only when [Hgb] fell <7.0 g/dL
RBC maintained between 7 - 9 g/dL
420 assigned to liberal transfusion arm
RBC transfused only when [Hgb] fell <10.0 g/dL
RBC maintained between 10.0 - 12.0 g/dL
Hebert PC, et al. N Engl J Med. 1999;340(6):409-17.
9/21/2010
7
Heberts Randomized, Controlled
Study in Critical Care
Study Variable % in Restrictive
Transfusion Arm
% in Liberal
Transfusion Arm
In-Hospital Mortality
Rate
22.2 28.2 (p=0.05)
APACHE <20 8.7 16.1 (p =0.03)
Age<55 years 5.7 13.0 (p =0.02)
30-day mortality 18.7 23.3 (p =0.11)
Clinically significant
cardiac disease
20.5 22.9 (p =0.69)
Blood Transfusion in Elderly
Patients with Acute MI
Retrospective study
78,974 Medicare beneficiaries, > 65 years old
Hospitalized with AMI Hospitalized with AMI
Categorized according to hematocrit on admission
Questioned an association between use of
transfusion and 30-day mortality
Found RBC transfusion decreased 30-day mortality
in elderly patients with MI
WuW-C, et al., N Engl J Med. 2001;345(17):1230-36.
Association of Blood Transfusion with 30-Day
Mortality in Elderly AMI Patients, by Hct
9/21/2010
8
Blood Transfusion in the Elderly with
Acute Myocardial Infarction
Data indicate a high prevalence of anemia among elderly
with AMI (43% had Hct < 39%)
Anemic patients had a higher 30-day mortality
Blood transfusion is effective in reducing short term
mortality rate among elderly, if their Hct is < 30.0% and
may be effective for patients with Hcts as high as 33.0%
Patients were less likely to receive transfusion if they
were white, had cardiac arrest, had a DNR order or who
had been admitted from nursing home
Relationship of Blood Transfusion &
Clinical Outcomes in Patients with ACS
Anemic patients with ischemic heart disease: Is
there definitive evidence to support transfusing
RBC?
Are we doing harm to such patients if we fail to
transfuse for Hgb < 10 g / dL?
Post hoc analysis of pooled data from 3 large Post hoc analysis of pooled data from 3 large
international trials of patients with acute coronary
syndromes
Patients grouped as whether they received RBCs
transfusion during hospitalization or not
Of 24, 112 patients in 3 studies, 10% had at least 1
blood transfusion, complete data on transfusion &
bleeding and outcomes
RaoSV, et al., JAMA2004;292(13):1555-62
Blood Transfusion in Patients with ACS
GUSTO IIb Trial strategies to open occluded
arteries, heparin vs. hirudin
PURSUIT Trial Platelet GPIIb/IIIa suppression
using Integrilin (eptifibatide)
PARAGON B Lamifiban vs. placebo
All 3 trials treated with aspirin in (80 to 325 mg/dL)
Transfusion data collected prospectively in each
Endpoints:
30-day all-cause mortality
30-day death or MI
Moderate bleeding not life threatening, required
transfusion; only 1
st
bleeding episode included in analysis
9/21/2010
9
Relationship of Blood Transfusion &
Clinical Outcomes in Patients with ACS
Study Variable Transfusion
(medianof 3.6units/
transfusedpatient)
No transfusion
Age(yr)
Female(%)
68.9
41.5
64.0 (p <.001)
33.6 (p <.001) Female(%) 41.5 33.6 (p .001)
Black race(%)
Body weight (Kg)
Comorbidities (HTN, DM,
stroke, hyperlipidemia)
5.1
74.0
27.9
3.9 (p <.002)
77.3 (p <.001)
20.6 (p <.001)
Hematocrits (%),
baseline/ nadir
39.9 / 29.0 41.7 / 37.6
(p <.001)
30-day MI
30-day death or MI
25%
29%
8%(p <.001)
10%(p <.001)
Some Conclusions: Transfusion of
Patients with Ischemic Heart Disease
Transfused patients were 3.94 x more likely (OR 3.26
4.75) to die within 30 days
At Hct < 25%, there was no relation between
transfusion and death
Data suggest Hcts as low as 25% may be tolerated in
otherwise stable patients with ischemic heart disease
Discrepancies vs. Wu, et al data:
Admitting Hcts vs. developing anemia (drivers of anemia such
as bleeding and procedures)
Transfusion data probably incomplete
Excluded patients younger than 65 years of age
Excluded patients dying within 48 hours
Pre-Op Hct & Post-op Outcomes in Older
Patients undergoing Noncardiac Surgery
Retrospective cohort study (132 U.S. VA Medical Centers)
310, 311 veterans, aged 65 years old
Underwent major noncardiac surgery, 1997 2004
St tifi d ti t di t ti h t it Stratified patients according to preoperative hematocrit
Outcome Measures:
30-day postoperative mortality
30-day composite postoperative mortality or cardiac events
Found 30-day mortality and cardiac event rates increased
monotonically (+ or -) with deviations from normal Hct
WuW-C, et al., JAMA2007;297(22):2481-88.
9/21/2010
10
Baseline Patient Characteristics by
Preoperative Hematocrit Level
Hematocrit, %
<39.0 39.0 53.9 >53.9
N =132, 970 N =176, 704 n =637
42.8% 56.9% 0.2%
Mean age ~ 73 y/o
Ca. 98% male; ca. 80% Caucasian
Cohort with anemia had the most female & nonwhite patients, the highest
prevalence of DM, cardiac disease, renal disease, infected wounds cancer and
preoperative transfusions
30-Day Postoperative Mortality &
Cardiac events by Hct Level
Hct, %
30-Day Mortality
Rates, %
30-Day Cardiac
Event Rates, %
Adjusted Odds
Ratio
< 18.0 35.4 14.6 2.42
18.0 20.9 26.8 8.6 1.68
24 0 26 9 14 9 4 4 1 33 24.0 26.9 14.9 4.4 1.33
30.0 32.9 8.4 3.1 1.21
36.0 38.9 3.5 1.8 1.12
45.0 47.9 1.5 0.9 1 (Ref.)
48.0 50.9 1.8 1.0 1.12
51.0 53.9 3.1 1.4 1.42
54 5.6 2.9 1.55
Issues Raised by the Wu Hct-
Surgery Study in the Elderly
Work highlights strengths of using high quality, large
observational databases
Allows for adjustments of many potentially
confounding variables common to surgical practice
The etiology and chronicity of abnormal Hcts could
not be related to the outcomes
No causality claimed, but authors provide several
classic lines of cause-effect relationship:
An appropriate temporal relationship
A strong association of predictor and outcome
An apparent dose-response relationship
Biologic plausibility related to cardiac physiology
9/21/2010
11
Issues Raised by the Wu Hct-
Surgery Study in the Elderly
Epidemiologic features speak to a real relationship between
Hct and outcome
Defining anemia in the elderly may have important clinical
implications p
Is anemia simply a marker of other conditions that confer
increased risk?
National guidelines recommend treatment only when Hct is <
18% to 21%; the majority of deaths are associated with only
modest degree of anemia (Hct 27.0% - 38.9%)
If anemia were a modifiable risk factor, should preoperative
transfusion be considered?
Systematic Review of RBC
Transfusion in the Critically Ill
45 studies with a median of 687 patients per study
Outcome measures
Mortality
Infection
MOF Syndrome
ARDS
Risks of RBC transfusion outweighed benefits in
42 of 45 studies!!
Marik &Corwin, Crit Care Med 2008;36(9):2667-74.
Association of Transfusion &
Risk of Death
Marik & Corwin, Crit Care Med 2008;36(9):2667-74.
9/21/2010
12
Association of Transfusion &
Risk of Infectious Complications
Marik & Corwin, Crit Care Med 2008;36(9):2667-74.
Association of Transfusion
& Risk Developing ARDS
Marik & Corwin, Crit Care Med 2008;36(9):2667-74.
Settings Wherein RBC Transfusion
Appears to be Beneficial
Neonates, especially premature neonates
Massive transfusion
Battlefield casualties
T ( i ili ) Trauma (civilian)
Surgery
Obstetrical hemorrhage
Liver transplantation
Chemotherapy-induced myelosuppression,
and stem cell transplantation
Sickle cell disease (selected indications)
9/21/2010
13
Reality Testing of the RBC
Transfusion Trigger
Hemoglobin Level
(g/dL)
Transfusion Decision
> 10
RBCs usually unnecessary
6 - 10
Grey Zone: Clinically correlate &
individualize
< 6
Almost always transfuse
3
Life-threatening
DO NOT Transfuse Red Blood Cells
To improve general well-being
To promote wound healing
In place of a hematinic In place of a hematinic
Prophylactically, in the absence of signs,
symptoms or risks
For volume expansion, when oxygen-
carrying capacity is adequate
Comments
about about
Platelets
9/21/2010
14
Flavors of Platelet
Concentrates
Random-donor pools
(pool size as low as 4)
Apheresis platelets
( single donor ) ( g )
Pre-Storage RD Pools
(leukoreduced,
bacteriologically tested,
counted for yield)
Apheresis platelets,
stored in InterSol, a
platelet additive solution
Platelet Concentrates
All platelet
concentrates have a
5-day Shelf Life
All Adult Doses
have a minimum
count of 3 x 10
11
platelets
Crossmatched and
HLA-typed platelets
are Apheresis, by
definition
Prophylactic Platelet Transfusion Dose
1271 patients with hypoproliferative
thrombocytopenia
Transfusion Trigger=10,000 / L
Randomly assigned to 3 doses
1.1 x 10
11
/ meter
2
2 2 x 10
11
/ meter
2
Slichter, et al.,NEJM 2010;362(7): 600-13
2.2 x 10 / meter
4.4 x 10
11
/ meter
2
Low dose led to decreased numbers
of platelets transfused, but increased
transfusions given
Doses between 1.1 and 4.4 x 10
11
/
meter
2
had no effect on the incidence
of bleeding
9/21/2010
15
When You Think You are Observing
Platelet Refractoriness
Rule out clinical causes
DIC states
Sepsis, infection, fever
Splenomegaly Splenomegaly
Medications
Repeat platelet counts 10 30 minutes,
posttransfusion
Please order a Panel Reactive Antibody Assay!
Request specialized platelets only in the setting of
documented immune-mediated refractoriness
Deciding to Transfuse Platelets:
Risk Assessment Issues
Medical vs. Surgical patient
Bleeding vs. Non-bleeding
Risks in surgical / obstetric patients g p
Type / extent of surgery
Ability to control bleeding
Actual / anticipated rate of bleeding
Factors affecting platelet function, such as
medications, extracorporeal circulation
such as bypass, renal failure, etc.
Bleeding Risks & Platelet Count are
Approximately Correlated
Platelet Platelet Count (10 Count (10
99
/L) /L)
< 5
Likelihood of Spontaneous
Hemorrhage
High
5 10
10- 50
> 50
Increased with
Trauma
Surgery
Ulceration
Variably Increased
Exceedingly Unlikely
9/21/2010
16
Recommendations for
Platelet Transfusion
Platelet Platelet Count (10 Count (10
99
/L) /L)
< 5
10 20
Transfusion Decision
Almost Always
Prophylaxis Window 10 20
< 50
50 - 100
100
Prophylaxis Window
for Medical Patients
Usually Indicated for Surgery &
Other Invasive Procedures
Based on Risk of Bleeding
Uncommonly Indicated: Consider
with known platelet dysfunction &
microvascular bleeding
Avoid Transfusing Platelets
In thrombocytopenia due to increased platelet
destruction (immune or microangiopathic)
Idiopathic thrombocytopenic purpura (ITP) p y p p p ( )
Thrombotic thrombocytopenic purpura (TTP)
Other microangiopathies (HUS, HELLP)
Platelet transfusion in these settings are rarely
indicated and usually ineffective You incur all
the risks, with little or no benefit
Fresh Frozen Plasma Unit
9/21/2010
17
Where in the Classical Cascade Do
the Coagulation Factors Belong?
Extrinsic Pathway
Factor I
Factor II
Intrinsic Pathway
Factors I, II, V
Factor VIII:C (also
ac o
Factor V
Factor VII
Factor X
Ag:vWF)
Factor IX
Factor X
Factor XI
Factor XII
Vitamin K-Dependent Factors
(all Synthesized in the Liver)
Factor II
Factor VII Factor VII
Factor IX
Factor X
Protein C
Protein S
Coagulation Factors
Factor Common Name Half-Life
I Fibrinogen 3 4 Days
II Prothrombin 2 3 Days
III Thromboplastin
Available fromvarious
tissues, suchas lung,
brain, kidney
IV Ionized Ca
++
Ubiquitous
V Ac-globulin
(proaccelerin)
12 36 hours
VI Nonexistent -
9/21/2010
18
Coagulation Factors
Factor Common Name Half-Life
VII
Proconvertin
(Prothrombin
Conversion Accelerator)
4 6 hours
VIIIC
Antihemophilic Factor
12 hours
IX
Christmas Factor
24 hours IX 24 hours
X
Stuart-Prower Factor
1 2 days
XI
Plasma Thromboplastin
antecedent
2 3 days
XII
Hagemans (contact)
factor
2 3 days
XIII
Fibrin Stabilizing Factor
(Profibrinoligase)
3 5 days
Plasma Components Available in the
United States other than FFP
24-Hour Plasma, known as FP24
Collected and separated from whole blood in
a time frame >8 hours, but <24 hours
F h lf lif i 1 h f Frozen shelf life remains 1 year, when frozen
at < 18
o
C
Use just like FFP
Delay time to freezing causes mild decrease
in activity of the labile Factors, V & VIII
84%of Factor VIII left after 8 hours; 64%after 24 hours
Plasma Components Available in the
United States other than FFP
Thawed Plasma
Stored at 1 6
o
C
Label change required after 24 hours
Used for up to 5 days (same indications as FFP)
Factor V and Factor VIII are labile and
progressively decrease over time
Hemostatic levels of FV & FVIII still available
9/21/2010
19
Clinical Indications for
Plasma Transfusion
Multiple factor deficiency with active
bleeding or prior to invasive procedure, and
Documented laboratory evidence of
ProlongedPT or PTT (15xmidpoint of thereference Prolonged PT or PTT (1.5 x midpoint of thereference
range)
Low Fibrinogen level
Low specific coagulation factor assay(s)
Typical clinical situations include
Liver disease
DIC states
Massive hemorrhage & transfusion in trauma
Clinical Indications for
Plasma Transfusion
Plasma exchange replacement fluid for
treating microangiopathies (such as
TTP, HUS, HELLP syndrome)
Documented congenital or acquired
coagulation factor deficiency
Deficiency of Protein S, Protein C or AT
(formerly known as AT-III)
[AT and Protein C concentrates are
available in the US]
Clinical Indications for
Plasma Transfusion
Massive transfusion and evidence of both
Continued (microvascular) bleeding
C i fi i il bl / Coagulation deficiency or unavailable PT / aPTT
Urgent reversal of Coumadin effect
To stop Coumadin-therapy related intracranial bleeding)
[Prior to surgery or other invasive procedure]
(Frequently done, but remains controversial!)
9/21/2010
20
Misuses of Plasma Transfusion
As a volume expander
As a nutritional source
Toenhancewoundhealing To enhance wound healing
Not a suitable source of immunoglobulins (in
patients with severe hypogammagloubulinemia)
Mild to moderate prolongation of PT or
aPTT prior to invasive procedures
Defining the INR
International Normalized Ratio =
(Patient PT / control PT )
ISI
, where ISI =
International Sensitivity Index
ISI, used by the local laboratory performing the PT
measurement determinedfor eachcommercial batch measurement, determined for each commercial batch
The ISI reflects the responsiveness of a given
thromboplastin to a reduction in Vitamin K-dependent
coagulation factors compared to WHO reference
material.
Highly sensitive thromboplastins (ISI ~1.0) are now
made by recombinant technology with defined
phospholipid content
Lab Screening Tests as a Trigger
to Transfuse Plasma
No increased risk of hemorrhage / oozing
if the PT / aPTT is no more prolonged than
1.3 X upper limit of reference range
NOT an
INR = 1.5
pp g
- or -
1.5 X midpoint of reference range
Abnormality Clinical Coagulopathy
9/21/2010
21
The INR of Fresh Frozen Plasma
The INR of FFP is 1.1
(range 0.9 to 1.3)
It is not surprising that
giving FFP has little
effect on minimally effect on minimally
elevated PTs
FFP will affect the INR
only when there is a
big difference between
the FFP and the
patients plasma
And What if Plasma is Transfused?
Mean change of 0.03
INR units / unit of FFP
transfused
Mildly abnormal PTs
just dont change much
with FFP transfusion
INRs above 3 have a INRs above 3 have a
more significant change
per unit of FFP
Mildly prolonged PT
values (13 17 sec) do
not correlate with RBC
loss
Only 10% of patients
had the PT re-checked
after transfusion!!
Holland, et al., Transfusion 2005;45:1234-5
An Analysis of the Literature
Normal vs. Abnormal Coagulation Tests
Pre-procedure
coagulation
tests are lousy
predictors of
who is going to
bleed
Prophylactic
plasma
transfusion does
not result in
fewer bleeding
events
J Segal, W Dzik, et al., Transfusion 2005;45 (9): 1413-25.
9/21/2010
22
CRYOPRECIPITATED AHF
Cold-insoluble portion of plasma processed from FFP
Plasma proteins not soluble at 1 - 6
o
C
Estimated Contents of Plasma
Factors in Cryoprecipitated AHF
Constituent Constituent
Fibrinogen
Approximate Content
150 mg (minimum)
Factor VIII:C
Von Willebrand Factor
Factor XIII
80 IU (minimum)
80 120 Units
40 60 IU
Cryoprecipitate:
Clinical Indications
Hypofibrinogenemia
E.g., in consumptive coagulopathies such as DIC
Isolated fibrinogen deficiency with active bleeding Isolated fibrinogen deficiency with active bleeding
or in patients at risk
vonWillebrands Disease or Hemophilia A (use only
when commercial concentrates are unavailable)
Fibrin surgical adhesive
Isolated Factor XIII deficiency
9/21/2010
23
Use of Blood Components: Use of Blood Components:
Dosage Considerations Dosage Considerations
Blood Component Blood Component
RBC RBC
Dosage: Goals
Variable Number of Units:
Reverse Symptomatic Anemia
Enhance Oxygen-carrying Capacity
Platelets Platelets
Plasma Plasma
Cryoprecipitate AHF Cryoprecipitate AHF
- Use Apheresis Platelets or Pools -
Provide 1Adult Dose at atime
(nominally 3x 10
11
platelet count):
To ReduceHighRisksof Bleeding
10 15 mL / Kg Body Weight: To
Achieve Hemostatic Levels
Provide 1 Adult Dose, pool of 5 units
To Replete Fibrinogen Level
What is Blood Management?
1
Blood management is an
evidence-based,
multidisciplinaryprocess that
isdesigned to promote the
optimal useof bloodproducts optimal use of blood products
throughout the hospital.
The goal of blood management
is ensure the safe and efficient
use of the many resources
involved in the complex process
of blood component therapy.
1
Boucher & Hannon, Pharmacotherapy 2007;27(10)
Blood Management
What is it?
The promotion of the appropriate use of blood
Improvement of patient outcomes by the
d t f bl d prudent use of blood
What is it not (but might include)
Bloodless Medicine
Bloodless Surgery
No Blood
9/21/2010
24
Why Blood Management?
Blood isa precious resource that saves lives
Blood is often in short supply
The number of eligible, willing blood donors is
dropping
The cost of blood continues to rise
The decision to transfuse remains unavoidably
unsafe, but some risks and complications may
be avoidable
Principles of Blood Management
Focus on the patients best interest: Patient-Centered
Grounded in scientific validation and evidence-based
practice
Use a multidisciplinary teamapproach p y pp
Physician-driven
Multidisciplinary and multi-professional
Effective
Achieve change through education & training
Must have an institutional commitment to excellence
Principles of Blood Management
Operational Issues
Risk reduction instituted in the preoperative setting
Restricting certain medications or nutritional
supplements
Restrictions appropriate for the surgical procedure
Use of surgical devices, medications and techniques
to reduce blood loss
Use of peri-operative blood salvage
Planned cooperation among multiple levels of care
9/21/2010
25
Do Not Pull That Transfusion Do Not Pull That Transfusion
Trigger Trigger Absent Patient Assessment Absent Patient Assessment
Summary Summary Statements Statements
Establish Institutional Guidelines based on
available literature / experience
Embrace / Implement / Teach Principles of
Blood Management
Avoid Transfusion Triggers Avoid Transfusion Triggers
Transfuse Targets: Patient-centered
Assessments when benefit > risk
Transfuse the right patient, at the right time,
with the right dose of the right component
Minimize or avoid transfusion whenever
possible
ASCP 2010 Annual Meeting
Selected Bibliography to Transfusion Triggers
Friday, October 29, 2010
Phillip J. DeChristopher, MD, PhD
General Guidelines
Miller Y, Bachowski G, Benjamin R, et al. Practice Guidelines for Blood Transfusion: A
Compilation from Recent Peer-Reviewed Literature, Second Edition. Washington, DC:
American National Red Cross, 2007.
Roseff SD. (Ed.), Pediatric Transfusion: A Physicians Handbook, Third Edition, Bethesda,
MD: AABB Press, 2009.
Waters J H (Ed.), Perioperative Blood Management: A Physicians Handbook, 1
st
Edition,
Bethesda, MD: AABB Press, 2006.
American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and
Adjuvant Therapies, Practice Guidelines for Perioperative Blood Transfusion and Adjuvant
Therapies, Anesthesiology 2006; 105(1), 198-208.
Triulzi DJ (Ed.), Blood Transfusion Therapy, A Physicians Handbook, Seventh Edition,
Bethesda, MD: AABB Press, 2002.
Guidelines for Use of Red Blood Cells
Napolitano LM, et al., Clinical practice guideline: Red Blood cell transfusion in adult trauma
and critical care, Crit Care Med 2009; 37:3124-57.
Marik PE and Corwin HL, Efficacy of red blood cell transfusion in the critically ill: A systemic
review of the literature, Crit Care Med 2008; 36:2667-2674.
West MA, Shapiro MB, Nathens AB, et al., Guidelines for Transfusion in the Trauma Patient, J
Trauma 2006;61:436-39.
Corwin HL and Hebert P. Avoiding a blood transfusion: How much is it worth? (Editorial).
Crit Care Med 2005;33(3):672-74.
Guidelines for Use of Platelets
Slichter SJ , et al., Dose of Prophylactic Platelet Transfusions and Prevention of Hemorrhage, N
Eng J Med 2010; 362(7): 600-13.
McGrath T, et al., Platelet Transfusion in Cardiac Surgery Does Not Confer Increased Risk for
Adverse Morbid Outcomes, Ann Thorac Surg 2008; 86: 543-53.
Greeno E, McCullough J , Weisdorf D, Platelet Utilization and the Transfusion Trigger: A
Prospective Analysis, Transfusion 2007; 47: 201-205.
Brecher ME, The platelet prophylactic transfusion trigger: When expectations meet reality,
Transfusion 2007; 47: 188-91.
Stanworth SJ , et al., Platelet Transfusion Prophylaxis for Patients with Haematological
Malignancies: Where to Now?, Br J Haematol 2005; 131: 588-95.
Guidelines for Use of Plasma
Roback J D, et al. Evidence-based practice guidelines for plasma transfusion, Transfusion 2010;
50:1227-39.
Kitchens CS, Alving BM and Kessler CM. Consultative Hemostasis and Thrombosis, 2
nd
Edition. Philadelphia: W. B. Saunders Co., 2007.
American Society of Anesthesiologists Task Force on Perioperative Blood Transfusion and
Adjuvant Therapies, Practice Guidelines for Perioperative Blood Transfusion and Adjuvant
Therapies, Anesthesiology 2006; 105(1), 198-208.
Holland LL and Brooks J P. Toward Rational Fresh Frozen Plasma Transfusion. The Effect of Plasma
Transfusion on Coagulation Test Results. Am J Clin Pathol 2006; 126:133-39.
Segal J B and Dzik, WH on behalf of the Transfusion Medicine / Hemostasis Clinical Trials
Network, Paucity of studies to support that abnormal coagulation test results predict bleeding in
the setting of invasive procedures: An evidence-based review, Transfusion 2005; 45(9), 1413-
1425.
British Committee for Standards in Haematology, Blood Transfusion Task force. Guidelines for
the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol 2004; 126:
11-28.
Stanworth SJ , Brunskill SJ , Hyde CJ , et al. Is Fresh Frozen Plasma Clinically Effective? A
Systematic Review of Randomized Controlled Trials, Br J Haematol 2004; 126: 139-52.
Guidelines for Use of Cryoprecipitate
Sorensen B and Bevan D, A critical evaluation of cryoprecipitate for replacement of
fibrinogen, Br J Haematol 2010; 149: 834-43.
Thorarinsdottir HR, et al., Effects of fibrinogen concentrate administration during severe
hemorrhage, Acta Anaesthesiol Scand 2010; 54: 1077-82.
Callum J L, et al, Cryoprecipate: The Current State of Knowledge, Transf Med Rev
2009; 23(3): 177-88.
You might also like
- Self-assessment Q&A in Clinical Laboratory Science, IIIFrom EverandSelf-assessment Q&A in Clinical Laboratory Science, IIIRating: 3 out of 5 stars3/5 (1)
- MLS ASCP Exam Recall Questions Flashcards - QuizletDocument8 pagesMLS ASCP Exam Recall Questions Flashcards - Quizletyeliz kurt100% (2)
- Breast MCQ Questions on Pathology Findings, Risk Factors and Treatment OptionsDocument55 pagesBreast MCQ Questions on Pathology Findings, Risk Factors and Treatment OptionsAhmad Adel Qaqour94% (16)
- ASCP Recalls 2017-2018 Flashcards - Quizlet - AmgadDocument80 pagesASCP Recalls 2017-2018 Flashcards - Quizlet - AmgadShiv Prajapati100% (16)
- Transfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeFrom EverandTransfusion Medicine for Pathologists: A Comprehensive Review for Board Preparation, Certification, and Clinical PracticeRating: 3 out of 5 stars3/5 (1)
- UW-STEVENS POINT MEDICAL TECHNOLOGY ASCP EXAM GUIDEDocument1 pageUW-STEVENS POINT MEDICAL TECHNOLOGY ASCP EXAM GUIDEDeanne LambanNo ratings yet
- ML7111 EXTRA PRACTICE QUESTIONS ANSWERSDocument15 pagesML7111 EXTRA PRACTICE QUESTIONS ANSWERSCleo Salvador100% (4)
- Code of Ethics Guidance DocumentDocument30 pagesCode of Ethics Guidance DocumentASHVINBHAI VACHHANI100% (1)
- BOC Study Guide Errata 09082010Document42 pagesBOC Study Guide Errata 09082010D.L67% (3)
- CLS Internship ManualDocument216 pagesCLS Internship ManualtaghamdNo ratings yet
- 1358453842.3856hematology Question BankDocument182 pages1358453842.3856hematology Question BankKay BristolNo ratings yet
- ASCPi ApplicationDocument48 pagesASCPi ApplicationMarian Keit BaconNo ratings yet
- CCRN-PCCN Review RenalDocument11 pagesCCRN-PCCN Review RenalGiovanni MictilNo ratings yet
- Virtual EAV: The Electro-Dermal Screening TestDocument21 pagesVirtual EAV: The Electro-Dermal Screening Testmich100% (1)
- CeramFab Inc. & WYG Refractories SuitDocument27 pagesCeramFab Inc. & WYG Refractories SuitBenjamin DuerNo ratings yet
- Slle Examination Content Guideline - March 05 PDFDocument16 pagesSlle Examination Content Guideline - March 05 PDFYahya Alkamali100% (1)
- ASCP Certification SOP PDFDocument2 pagesASCP Certification SOP PDFDeanne LambanNo ratings yet
- Clinical ChemistryDocument10 pagesClinical ChemistryChristina AtefNo ratings yet
- Clinical Chemistry Board ReviewDocument14 pagesClinical Chemistry Board ReviewWellaBaylasNo ratings yet
- Mls Study Guidelines AscpDocument5 pagesMls Study Guidelines AscpCielamae Orbeta100% (1)
- Haematology Ascp RecallDocument7 pagesHaematology Ascp RecallMona AliNo ratings yet
- Board of Directors: Ascp-Ascp Certification & Qualification Comparison ChartDocument1 pageBoard of Directors: Ascp-Ascp Certification & Qualification Comparison ChartMustaffah KabelyyonNo ratings yet
- Ascp International Procedures BookDocument25 pagesAscp International Procedures BookDegee O. Gonzales100% (1)
- Pass Ascp 2020 LatestDocument6 pagesPass Ascp 2020 LatestLorelie ChenNo ratings yet
- BOC Study Guide: The MostDocument17 pagesBOC Study Guide: The MostDeanne LambanNo ratings yet
- Virology ASCPDocument24 pagesVirology ASCP2131443No ratings yet
- Study Stacks - Chemistry Table Review PDFDocument14 pagesStudy Stacks - Chemistry Table Review PDF장주연100% (1)
- ASCP Recalls 11Document3 pagesASCP Recalls 11Cristina Vergel De DiosNo ratings yet
- Immuno For ASCP ReviewDocument25 pagesImmuno For ASCP ReviewWl SorianoNo ratings yet
- ASCP Recalls 5Document9 pagesASCP Recalls 5Cristina Vergel De DiosNo ratings yet
- Ascp Pointers MicroDocument73 pagesAscp Pointers Microraica56_362842087100% (5)
- Study Stack - Hematology Tests 3-4 Table ReviewDocument5 pagesStudy Stack - Hematology Tests 3-4 Table Review장주연No ratings yet
- Study Stack - MLT Table ReviewDocument3 pagesStudy Stack - MLT Table Review장주연No ratings yet
- HeamatologyDocument45 pagesHeamatologypikachuNo ratings yet
- Study Stack - M (ASCP) EXAM Table Review PDFDocument9 pagesStudy Stack - M (ASCP) EXAM Table Review PDF장주연100% (2)
- Simulated No.1 General Rule:: ExceptDocument29 pagesSimulated No.1 General Rule:: ExceptJie FuentesNo ratings yet
- Correct Answers to Multiple Choice Questions on Clinical Laboratory TopicsDocument31 pagesCorrect Answers to Multiple Choice Questions on Clinical Laboratory Topicspikachu100% (1)
- Transfusion TherapyDocument14 pagesTransfusion TherapyCMLNo ratings yet
- Recalls Ascp (Exam) - 2021 - 240103 - 185452Document16 pagesRecalls Ascp (Exam) - 2021 - 240103 - 185452gaber 230100% (1)
- Blood BankingDocument5 pagesBlood BankingTel LyNo ratings yet
- Mls Imls Reading ListDocument3 pagesMls Imls Reading ListPeng KwanNo ratings yet
- Ascpi Recalls 2016Document9 pagesAscpi Recalls 2016Zylene GabrielNo ratings yet
- CH 6 The ABO Blood Group SystemDocument3 pagesCH 6 The ABO Blood Group SystemDixie DumagpiNo ratings yet
- ABO Blood Group DiscrepanciesDocument9 pagesABO Blood Group DiscrepanciesRichard SiahaanNo ratings yet
- FEB 2017 RecallsDocument2 pagesFEB 2017 RecallsLucid LynxNo ratings yet
- Antibody IdentificationDocument27 pagesAntibody Identificationhamaada100% (1)
- Blood Groups and Blood Bank Testing FundamentalsDocument19 pagesBlood Groups and Blood Bank Testing FundamentalsJessica TuNo ratings yet
- Clinical Chemistry - Theory, Analysis, CorrelationDocument344 pagesClinical Chemistry - Theory, Analysis, Correlationaristides.quinteroNo ratings yet
- Lab ValuesDocument5 pagesLab Valuespragya_devkotaNo ratings yet
- ASCP Recalls and Lab Tests GuideDocument22 pagesASCP Recalls and Lab Tests Guidebaihern24No ratings yet
- Abo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTDocument14 pagesAbo Typing Discrepancies: Rene Jesus Alfredo R. Dinglasan, RMTdirenjan100% (1)
- Immunohematology: The Science of Blood GroupsDocument4 pagesImmunohematology: The Science of Blood Groupsosama1381971No ratings yet
- Toaz - Info Recalls March PRDocument8 pagesToaz - Info Recalls March PRNyeinlinn Maung100% (1)
- Books and clinical lab science review points for exam preparationDocument1 pageBooks and clinical lab science review points for exam preparationTinay100% (1)
- ASCPi Recalls Sep 23 2017Document3 pagesASCPi Recalls Sep 23 2017Jaine SalongaNo ratings yet
- Review in Clinical MicrosDocument103 pagesReview in Clinical MicrosSyvelmarie Tinte100% (1)
- Important new certification infoDocument28 pagesImportant new certification infoMuhammad umarNo ratings yet
- Medical Laboratory Sample QuestionsDocument6 pagesMedical Laboratory Sample Questionszopito100% (1)
- Microbiology ReviewerDocument64 pagesMicrobiology ReviewerMariel Abatayo0% (1)
- Practice Questions 1Document12 pagesPractice Questions 1Cha100% (1)
- BOC 6th EdDocument79 pagesBOC 6th EdIseth ISeth100% (1)
- Senior Medical Laboratory Technician: Passbooks Study GuideFrom EverandSenior Medical Laboratory Technician: Passbooks Study GuideNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Surviving A New His: A Guide To Help Blood Bank Leaders Manage Successful IntegrationDocument4 pagesSurviving A New His: A Guide To Help Blood Bank Leaders Manage Successful IntegrationMohamed ElmasryNo ratings yet
- Treatment of Autoimmune Hemolytic Anemias - HaematologicaDocument13 pagesTreatment of Autoimmune Hemolytic Anemias - HaematologicaMohamed ElmasryNo ratings yet
- AABB Disastophndbkv2Document128 pagesAABB Disastophndbkv2Mauricio Vanessa Juliana Koury PalmeiraNo ratings yet
- XV - Quality Assurance in The Blood BankDocument5 pagesXV - Quality Assurance in The Blood BankMohamed ElmasryNo ratings yet
- Standard Operating Procedures For Blood Bank Processes in PakistanDocument204 pagesStandard Operating Procedures For Blood Bank Processes in PakistanMohamed Elmasry100% (4)
- (PAkistan Guidelines For Quality ControlDocument27 pages(PAkistan Guidelines For Quality ControlErick MattosNo ratings yet
- Trima Accel The Art of Blood CollectionDocument7 pagesTrima Accel The Art of Blood CollectionMohamed ElmasryNo ratings yet
- The Ps and Qs in Qulity SystemsDocument4 pagesThe Ps and Qs in Qulity SystemsMohamed ElmasryNo ratings yet
- Standard Operating Procedures For Blood Bank Processes in PakistanDocument204 pagesStandard Operating Procedures For Blood Bank Processes in PakistanMohamed Elmasry100% (4)
- R P F C: Esponse LAN LOW HartDocument1 pageR P F C: Esponse LAN LOW HartMohamed ElmasryNo ratings yet
- FDA 2013-715 Bacterial Detection Testing Draft Guidance 12-4-14 - 2Document36 pagesFDA 2013-715 Bacterial Detection Testing Draft Guidance 12-4-14 - 2Mohamed ElmasryNo ratings yet
- In 003 ISBT 128 For Blood Components An Introduction v3Document19 pagesIn 003 ISBT 128 For Blood Components An Introduction v3Mohamed ElmasryNo ratings yet
- How Do I Approach A Case of Warm-Reactive AutoantibodiesDocument4 pagesHow Do I Approach A Case of Warm-Reactive AutoantibodiesMohamed ElmasryNo ratings yet
- Blood Bank Quality ProgramDocument28 pagesBlood Bank Quality ProgramMohamed Elmasry100% (1)
- Educational Goals of Residents Rotation in Transfusion MedicineDocument10 pagesEducational Goals of Residents Rotation in Transfusion MedicineMohamed ElmasryNo ratings yet
- Educational Goals of Residents Rotation in Transfusion MedicineDocument10 pagesEducational Goals of Residents Rotation in Transfusion MedicineMohamed ElmasryNo ratings yet
- Clinical Guide To Blood TransfusionDocument181 pagesClinical Guide To Blood TransfusionMohamed Elmasry100% (3)
- Guide Selection Assessing SuitabilityDocument238 pagesGuide Selection Assessing SuitabilityMohamed Elmasry100% (1)
- BMJ Learning User GuideDocument16 pagesBMJ Learning User GuideMohamed ElmasryNo ratings yet
- BSCH TTP GuidelinesDocument13 pagesBSCH TTP GuidelinesMohamed ElmasryNo ratings yet
- Training for Safe Blood Collection and TransfusionDocument82 pagesTraining for Safe Blood Collection and TransfusionMohamed Elmasry0% (1)
- Blood Group System OutlineDocument12 pagesBlood Group System Outlinesoul_filled_booksNo ratings yet
- Bhutan National External Quality Assessment Scheme Blood Group SerologyDocument31 pagesBhutan National External Quality Assessment Scheme Blood Group SerologyMohamed ElmasryNo ratings yet
- BRM Hem V9P1Document13 pagesBRM Hem V9P1Mohamed ElmasryNo ratings yet
- Warm Autoadsorption-Are We Wasting Our TimeDocument13 pagesWarm Autoadsorption-Are We Wasting Our TimeMohamed ElmasryNo ratings yet
- Approach To Antibody IdentificationDocument4 pagesApproach To Antibody IdentificationMohamed ElmasryNo ratings yet
- ArryhthmiaDocument16 pagesArryhthmiaMohamed ElmasryNo ratings yet
- Q and A in Antibody IdentificationDocument29 pagesQ and A in Antibody IdentificationMohamed ElmasryNo ratings yet
- Transfusion Support of Autoimmune Hemolytic AnemiaDocument7 pagesTransfusion Support of Autoimmune Hemolytic AnemiaMohamed ElmasryNo ratings yet
- Tobacco Smoking-Associated Alterations in The Immune Microenvironment of Squamous Cell CarcinomasDocument7 pagesTobacco Smoking-Associated Alterations in The Immune Microenvironment of Squamous Cell CarcinomasKamado NezukoNo ratings yet
- Amaryl M PI - May 2018marylDocument11 pagesAmaryl M PI - May 2018marylvicky upretiNo ratings yet
- Vensim Model IndexDocument4 pagesVensim Model Indexkaren dejoNo ratings yet
- Lecture 1 PharmacodynamicsDocument55 pagesLecture 1 PharmacodynamicsAuthor Nauman ShadNo ratings yet
- Canine Perineal TumoursDocument11 pagesCanine Perineal TumoursSUSANA SAM RODRIGUEZNo ratings yet
- Cyclic Progesterone Therapy Patient HandoutDocument1 pageCyclic Progesterone Therapy Patient HandoutMuhammadRizalNNo ratings yet
- Geriatric OtolaryngologyDocument26 pagesGeriatric OtolaryngologySari RakhmawatiNo ratings yet
- Knee Pain and HomoeopathyDocument4 pagesKnee Pain and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (3)
- Bladder Substitution and Urinary DiversionDocument58 pagesBladder Substitution and Urinary DiversionlifespotNo ratings yet
- Li-Rads Core 2018Document60 pagesLi-Rads Core 2018CharleasyNo ratings yet
- Et-Lec 14 Wax TherapyDocument64 pagesEt-Lec 14 Wax TherapyAngelic khanNo ratings yet
- Compounded Sterile Products Stability Compendium-AntineoplasticsDocument0 pagesCompounded Sterile Products Stability Compendium-AntineoplasticsRahmalia 'lia Cudby' PrihanantoNo ratings yet
- Breast Cancer AwarenessDocument5 pagesBreast Cancer AwarenessdrrskhanNo ratings yet
- NO CANCER RISK EPA 2012 Chemicals - EvaluatedDocument29 pagesNO CANCER RISK EPA 2012 Chemicals - EvaluateduncleadolphNo ratings yet
- Gastro ExamDocument2 pagesGastro ExamJessica Brittain-GeorgeNo ratings yet
- OSU Orthopaedics Accomplishments Report 2010Document32 pagesOSU Orthopaedics Accomplishments Report 2010osuorthopaedicsNo ratings yet
- Weed The PeopleDocument1 pageWeed The PeopleJaycee PascualNo ratings yet
- Curriculum Vitae: I. Personal InformationDocument5 pagesCurriculum Vitae: I. Personal InformationbernabasNo ratings yet
- Gentics PDFDocument7 pagesGentics PDFHarpreet KaurNo ratings yet
- All You Need Know About Mouth CancerDocument7 pagesAll You Need Know About Mouth CancerKaknika KapoorNo ratings yet
- Basic Dharmafect ProtocolDocument4 pagesBasic Dharmafect ProtocolXimenaBandaNo ratings yet
- Pdhpe Assessment Task Term 1 Drug Use in AdolescentsDocument10 pagesPdhpe Assessment Task Term 1 Drug Use in Adolescentsapi-463236687100% (2)
- Buter t1 Case Studies CalendarDocument4 pagesButer t1 Case Studies Calendarapi-602288180No ratings yet
- Turner Syndrome, Klinefelter Syndrome, Down SyndromeDocument78 pagesTurner Syndrome, Klinefelter Syndrome, Down SyndromeTasya100% (3)
- Word Perioperative NursingDocument19 pagesWord Perioperative NursingGerald Resubal Oriña100% (1)
- Uveal Coloboma: The Related SyndromesDocument3 pagesUveal Coloboma: The Related Syndromeslavinia diaNo ratings yet