Professional Documents
Culture Documents
ORL Interns Notes
Uploaded by
Daphne Ongbit JaritoCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ORL Interns Notes
Uploaded by
Daphne Ongbit JaritoCopyright:
Available Formats
Page 1 of 1 Otorhinolaryngology /epcapul UPCM09
OTORHINOLARYNGOLOGY
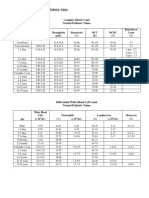
MASTOID SERIES (MaST M[eyer]aS[chuller]Townes)
Townes View Meyers View Schullers View
Projection AP projection of the skull with
the beam source 30 above
the canthomeatal line
AP projection of the skull with the head
turned 45 toward the side one wishes
to examine & the beam source 45
above the canthomeatal line
Lateral projection of the skull with the
beam source 30 above the
canthomeatal line
View Clear view of the foramen,
comparison of the petrous
pyramid & mastoids
Provides axial view of the external
auditory meatus, mastoid, & petrous
bone
Shows extent of pneumatization of the
mastoid
(1) Pneumatic well-developed mastoid
air cells
(2) Diploic with few large air cells
(3) Sclerotic with opacity due to
calcification
PARANASAL SINUS SERIES
Waters View Caldwell View Skull Lateral Basal View
Occipitomental view or
chin-nose view
Occipitofrontal view
orforehead-nose view
Submentovertical view
Projection Patients head is tilted
with the nose & the chin
on the film,
orbitomeatal line is 37
from the film, x-rays are
directed horizontally
PA viewofthe skull with
the beam 15-20 from
the horizontal
Pts infraorbitomeatal
line is parallel to the
film, x-rays
perpendicular to the
infraorbitomeatal line
through the sella turcica
Best view Maxillary sinus
Open mouth Waters
view sphenoid sinus
Frontal sinus Sphenoid sinus Zygomatic arch
fractures
Also shows Frontal & anterior
ethmoid sinuses
Nasal bones, requested
if suspecting nasal
fractures together with
Nose STL
Anterior ethmoid &
sphenoid sinuses,
lamina papyracea
Posterior ethmoid,
frontal, & maxillary
sinues & sella turcica
Sphenoid, posterior
ethmoid, maxillary &
frontal sinuses
Panorex View
Provides the best view of the mandible
Requested when suspecting mandibular fractures (most common site being the angle, having the thinnest bone), dentoalveolar
abscess (DAA), ameloblastoma, & oseteomyelisis of the mandible
Neck soft tissue lateral (Neck STL)
Requested when suspecting foreign body lodged in the neck, epiglottitis (seen as thumb sign), laryngotracheobronchitis (seen
as steeple sign)
CXR AP-L to include the neck and abdomen
Requested when suspecting foreign body in the aerodigestive tract
Possible for children, otherwise request for CXR AP-L to include the neck (or a separate STL when not possible), plain abdomen
Nose soft tissue lateral (Nose STL)
Requested together with Waters view when suspecting nasal bone fractures
IMPACTED CERUMEN
Signs and Symptoms
a. sense of ear fullness
b. otalgia (ear pain) usually felt after getting water into the ear, because the cerumen swells, impinging on the pain
receptors in the external ear. May occur with secondary otitis externa because of the clumsy efforts to remove the
cerumen.
c. Conductive hearing loss usually not clinically significant. On Webers, there is lateralization to the affected ear (may not
be appreciated when impaction is not significant)
THE EAR
RADIOLOGY
Text
Page 2 of 2 Otorhinolaryngology /epcapul UPCM09
Treatment
Softening of cerumen with baby oil or commercially available ceruminolytics, such as Docusate Na (Otosol) 0.5% X 10mL (Lie on
the side, turning the head sideways, slightly towards the surface on which you are lying. Fill the ear canal & stay in this position for 5
minutes then insert a cotton wool plug. Repeat to the other ear if necessary. Max of 2 consecutive nights.). Have the pt come back
after 1 week for aural irrigation with clean lukewarm water. Aural irrigation is done with the stream directed behind the cerumen and
not directly at it, which may push it further down the canal.
OTITIS EXTERNA
May result from ear manipulation (e.g. sharp metal objects) or the presence of foreign objects/foreign body (FB)
Most common etiologic agent is Staphylococcus aureus, a normal flora of the external ear
Classification
a. Diffuse swimmers ear. Swelling of the entire external auditory meatus (EAC)
b. Circumscribed furunculosis. There is only a circumscribed swelling affecting the hairy portion of the EAC
Signs and Symptoms
a. otalgia
b. serous ear discharge
c. tenderness on manipulation of pinna or tragus
d. hearing loss if swelling occludes the external ear
e. swelling on otoscopy
Otitis Externa Otitis Media
Pain Severe Not as severe
Tenderness on pinna / tragus Present Absent
Fever Absent Present
History of URTI Usually none Usually present
History of ear manipulation Present Absent
Hearing Not impaired Impaired
Mastoid series Normal With evidence of mastoiditis
Treatment
a. Systemic oral antibiotic treat the infection. For children: Cloxacillin 50 mg/kg/day in 4 divided doses X 7 days
(125mg/5mL preparation)
b. Topical steroid reduce the swelling; usually prepared with antibiotic
1. Corticosporin: Hydrocortisone + Polymyxin B + Neomycin
2. Aplosyn: Fluocinilone + Polymyxin B + Neomycin
3. Synalar: Fluocinolone + Polymyxin B + Neomycin
c. Oral analgesic for pain.
1. For the elderly or those with PUD: COX-2 Inhibitors
i. Etoricoxib (Arcoxia) 120 mg OD preferred by ENT
ii. Celecoxib (Clebrex 200mg OD
iii. Rofecoxib (Vioxx) 25 mg OD
2. On a full stomach: Mefenamic Acid 500mg QID prn
3. For children: Paracetamol 10 mg/kg/day prn (125mg/5mL and 250mg/5mL preparations)
d. Aural toilette is done prior to application of Corticosporin.
If there is no response after 1 week, then suspect Pseudomonas infection and give a quinolone with anti-Pseudomonas activity
such as Ciprofloxacin 500 mg tab
ACUTE OTITIS MEDIA
Infection of the middle ear <4 weeks
Usually results from obstruction of the Eustachian Tube (ET), which serves as drainage of the middle ear. Sniffing too hard
causes a negative pressure in the middle ear, closing the ET tube; blowing the nose hard creates a positive pressure in the
middle ear, opening the ET tube
Obstruction can be either
a. Mechanical e.g. benign or malignant tumors
b. Functional e.g. cleft palate
Cloxacillin 500mg/cap 1 cap PO QID X 7 days (adults)
Corticosporin Otic Drops 3gtts TID X 7 days
Etoricoxib 120 mg/tab 1 tab OD prn for pain (adults)
Aural toilette with H2O2 3 gtts TID X 7 days priorto application of Corticosporin
Avoid ear manipulation
TCB after after 7 days for reassessment.
Apply 3 baby oil drops 3gtts TID X 7 days on affected ear
Avoid ear manipulation (AEM)
TCB after 7 days for aural irrigation
Sample Chart Entry
Sample Chart Entry
Page 3 of 3 Otorhinolaryngology /epcapul UPCM09
Predisposing factors
a. young age ET is wider, shorter & more horizontal compared to adults
b. immunocompromised state causes recurrent URTI
c. altitude changes
d. bottle feeding greater risk than breastfeeding
e. congenital defects (cleft palate)
f. benign or malignant masses in the nasopharynx
Stages
a. Hyperemia onset of disease; presents with otalgia, ear fullness, hearing loss, fever, (+) peripheral congestion of the ear
drum on otoscopy
b. Exudative pouring of fluid in the middle ear; presents with increased otalgia, ear fullness, hearing loss and fever
c. Suppurative rupture of TM with discharge; presents with mucupurulent discharge, decreased pain, decreased fever, but
increased hearing loss
d. Resolution / Complications a surgical ear is those with complications
e. Coalescence thickening of mucoperiosteum drainage is blocked venous stasis local inflammation?
decalcification pus; nocturnal fever; simple mastoidectomy
Treatment
a. Antibiotic to treat the infection
1. For children, give Amoxicillin 40 mg/kg/day divided in 3 doses X 14 days (125mg/5mL and 250mg/5mL
preparations available)
2. If with TM perforation, such as during the stage of suppuration, a topical antibiotic such as Corticosporin, may
be given because of perforation allows for the delivery of the drug into the ear.
3. If there is no response after 1 week, suspect Pseudomonas infection and give a quinolone with anti-
Pseudomonas activity like Ciprofloxacin
b. Aural toilette is done only if there is active discharge. It is done prior to application of corticosporin.
c. ET opening exercises are done to open the ET and thus provide drainage of middle ear secretions
1. Valsalva maneuver Ask pt to blow nose against a closed mouth and nose opens ET
2. Toynbee maneuver Ask pt to swallow with mouth & nose closed opens ET
3. Chewing gum
Complications
a. Extracranial complications (FLAPS)
Facial nerve paralysis
Labyrynthitis
Abscess
Subperiosteal abscess
Bezolds abscess abscess in the SCM
Cittellis abscess - digastric
Petrositis Gradenigos syndrome (DRE)
Diplopia due to lateral rectus palsy
Retroorbital pain due to involvement of the optic nerve
Ear discharge
Sensorineural hearing loss
b. Intracranial complications (MATH)
Meningitis most common
Abscess (epidural, subdural, cerebral)
Thrombophlebitis picket-fence fever(caused by emboli of abscess)
Hydrocephalus
CHRONIC SUPPURATIVE OTITIS MEDIA (CSOM)
Infection of the middle ear >4 weeks; persistent ear discharge on a perforated ear >6weeks
Fever not a constitutional sign
Classification
a. Active (+) discharge
b. Inactive (-) discharge > 3 months
c. Quiescent (-) discharge < 3 months
Treatment
Mastoid series is requested to assess pneumatization of the mastoid and aseess for cholesteatoma
Pure tone audiometry and speech test to assess severity of hearing loss
Tympanometry is requested if TM is retracted, dull or suspecting chronic infection of the middle ear
Amoxicillin 500mg/cap 1 cap TID X 14 days
Corticosporin otic 3 gtts TID X 14 days (only if suppurative)
Aural toilette with H2O2 3 gtts TID X 14 days (only if suppurative)
AEM, increase OFI, KED
Frequent ET opening exercises
TCB after 7 days for re-assessment
Sample Chart Entry
Page 4 of 4 Otorhinolaryngology /epcapul UPCM09
Benign Dangerous
Perforation is central regardless of size or shape Perforation is total or located at the margin, attic (pars flaccida)
or postero-superior
Mucosa lining in the middle ear is edematous Mucosa around the perforation is replaced by stratified
squamous epithelium. Cholesteatomatous debris may be seen
around the perforation or in the attic
There may be granulation tissue or polyps arising from the
middle ear mucosa
Granulation or polyps are frequently seen in the canal obscuring
the drainage
Discharge is mucoid to purulent & non-foul smelling Discharge is purulent & foul-smelling
Hearing loss is conductive Hearing loss is conductive and sensorineural
Mastoid series show no cholesteatoma Mastoid series reveal cholesteatoma. On PE, there may be
posterior auricular or subperiosteal abscess or fistula.
CHOLESTEATOMA
Concurrent with CSOM
Seen radiographically as an enlarged mastoid antrum (>1cm). It appears as a radiolucency surrounded by areas of sclerosis with
no trabeculations. Bony destruction or erosions may be seen. Clinically, there is pearly white ear discharge, very foul smelling
with TM perforation.
Plain & contrast CT scan with 1mm temporal bone cuts is requested if clinically positive for cholesteatoma for OR planning prior
to possible tympanomastoidectomy
AURAL POLYP
Squamous hypertrophy from the middle or external ear
PRESBYCUSIS
Hearing loss related to aging process
Normal otoscopy
SENSORINEURAL HEARING LOSS
May be due to chronic exposure to loud noise, as a complication of CSOM, as a result of infection or tumor
On Weber, there is lateralization to the unaffected ear
PTA-ST
TCB once with results
PTA-ST
For possible application of hearing aid
TCB once with results
Mastoid series
PTA-ST
Cranial CT scan, plain & contrast, with 1mm temporal bone cuts
Pen G 4 million units IV LD ( ) ANST then 2 million units q6h
Clindamycin 600mg IV LD ( ) ANST then 300mg q6h
Corticosporin otic 3 gtts TID (only if suppurative)
Aural toilette with H2O2 3 gtts TID (only if active)
AEM, increase OFI, KED
Frequent ET opening exercises
TCB after 7 days for re-assessment
Mastoid series
PTA-ST
Amoxicillin 500mg/cap 1 cap TID X 14 days
Corticosporin otic 3 gtts TID X 14 days (only if active)
Aural toilette with H2O2 3 gtts TID X 14 days (only if active)
AEM, increase OFI, KED
Frequent ET opening exercises
TCB after 7 days for re-assessment
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Page 5 of 5 Otorhinolaryngology /epcapul UPCM09
SPEECH DELAY SECONDARY TO HEARING IMPAIRMENT
First, rule out other causes such as autism
EXTERNAL AUDITORY CANAL BLEEDING SECONDARY TO EAR MANIPULATION
Rule out other causes
Antibiotic is given due to damage to EAC mucosa predisposing to infection
SINUSITIS
Most common etiologic agents: S. pneumonia, H. influenza, Moraxella catarrhalis, anaerobes
Signs and Symptoms
a. nasal obstruction
b. mucopurulent nasal discharge
c. paranasal pain
d. headache
e. paranasal tenderness
f. congested nasal mucosa on rhinoscopy
g. absent illumination(frontal / maxillary sinuses)
h. fever may be present
i. opacities on x-ray
Classification
a. Acute - < 3 months
b. Chronic - > 3 months, most common cause is untreated acute sinusitis; usually mized flora
Treatment
Nasal douche is prepared by mixing 1 tsp rock salt, 1 tsp baking soda, and 1L of boiled tap water made to cool.
ALLERGIC RHINITIS
Signs and Symptoms
a. rhinorrhea
b. sneezing (>4x/day, usually in the morning)
c. nasal obstruction
d. nasal pruritus
e. congested nasal mucosa on rhinoscopy
f. allergic salute (crease near the tip of the nose due to frequent rubbing)
g. allergic shiners (skin hyperpigmentation below the lower eyelid)
h. triggers may be present; most common allergens are household dust mite, cockroach, grass pollen, molds
i. family history of allergy
j. personal history of bronchial asthma or eczema
PNS series
Co-amoxiclav 625 mg/cap TID or 1g BID X 7 days
Increased OFI
Nasal douche BID on each nostril, increased OFI
TCB after 1 week for re-asessment
Co-amoxiclav 625 mg/cap TID or 1g BID X 7 days
Increased OFI
TCB after 1 week for re-asessment
Suction
Cloxacillin 500 mg/cap 1 cap QID X 7 days
Etoricoxib 120 mg/tab 1 tab OD prn for pain
TCB after 1 week for re-assessment
PTA-ST
Refer to Pedia for evaluation and co-management
TCB once with results
THE NOSE
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Page 6 of 6 Otorhinolaryngology /epcapul UPCM09
Treatment
a. Topical steroid relieve the inflammation
1. Fluticasone (Flixotide) Fluticasone nasal spray 2 puffs / nostril BID X 14 days & prn Usually prescribed by
ENT
2. Budesonide (Budecort) nasal spray 64 mcg/dose [X 120 doses] Initially 2 puffs in each nostril daily.
Maintenance: 1 puff in each nostril daily.
b. Oral anti-pruritus
1. Cetirizine (Virlix) 10 mg/tab 1tab OD at HS X 14 days & prn
2. Loratidine (Claritin) 10 mg/tab 1tab OD at HS X 14 days & prn
c. Decongestant are not of proven benefit and may cause rebound rhinitis (rhinitis medicamentosa) if used for more than 5
days
NASAL POLYPOSIS
Usually arises from the osteomeatal complex (MIM HUBAd: Middle meatus, Infundibulum, Maxillary sinus ostium, Hiatus
semilunaris, Uncinate process, Bulla ethmoidalis, Agger nasi)
Signs and Symptoms
a. Nasal obstruction may cause sinusitis due to obstruction of the drainage of frontal and maxillary sinuses
b. Anosmia
c. Rhinorrhea (watery to mucoid)
d. Smooth, gelatinous, semitransparent to pale white mass on anterior rhinoscopy
Grading
0 No polyps
I Polyps do not prolapse beyond the middle turbinate & may require endoscopy for visualization
II Polyps extend below the middle turbinate. Visible with nasal speculum.
III Polyps touching the nasal floor. May occlude the entire nasal cavity. May be seen through the vestibule without the aid of a
nasal speculum
Comparison of Nasal Polyp & Turbinates
Nasal Polyps Turbinates
Color skinned grapes Pink to red
Decongestant effect (-) (+)
Mobility Mobile Fixed
Sensation (-) (+)
Location Usually at osteomeatal complex Along entire lateral nasal wall
Consistency Soft Hard
Treatment
a. Surgery: (PEA) Polypectomy, Ethmoidectomy, Anthrostomy. Done under LA if middle-aged. Done under GA in children &
elderly.
b. Steroids given 1 week prior to OR to decrease the swelling & minimize bleeding intraop
1. Prednisone 10mg/kg OD X 1 week prior to OR
2. Methylprednisolone 16 mg 2 tab OD every other day for 1 week
c. SAPOD clearance: CBC with PC & DC, BUN/Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
NASAL FOREIGN BODY
Usually presents as a unilateral, foul-smelling, purulent nasal discharge, usually in children & handicapped
Removal may be done with theuse of Hartmann forceps, alligator forceps, or a blunt right-angled hook. Done in office setting with
the use of restraints for uncooperative patients, especially children.
INVERTING PAPILLOMA
Most common benign neoplasm in the nose & sinuses
Pre-malignant lesion usually unilateral
10% develops SCCA
Complete excision
PEA/LA c/o minor OR
Prednisone 10mg/kg OD X 1 week prior to OR
SAPOD clearance: CBC with PC & DC, BUN/Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
TCB once with results for OR scheduling
Fluticasone nasal spray 2 puffs / nostril BID X 14 days & prn
Cetirizine (Virlix) 10 mg/tab 1tab OD at HS X 14 days & prn
Avoid exposure to allergen
Refer to Allergy Clinic Re: Skin testing
TCB after 2 weeks for re-assessment
Sample Chart Entry
Sample Chart Entry
Page 7 of 7 Otorhinolaryngology /epcapul UPCM09
Hyperthyroidism Hypothyroidism
Nervousness Fatigue, lethargy
Weight loss Weight gain
Excessive sweating Cool, dry, coarse skin; loss of hair
Warm, smooth, moist skin Swelling of the face, hands, legs, non-pitting edema
Heat intolerance Cold intolerance
Muscular weakness, tremor Weakness, muscle cramps, arthralgia, paresthesia
Lid lag, exophthalmos, stare Peri-orbital puffiness
Palpitations, hyperdynamic cardiac pulsations, accentuated S1 Decreased intensity of heart sounds
Tachycardia Bradycardia
SBP, DBP SBP, DBP
Frequent bowel movements Constipation
Toxic SSx: Heat intolerance, palpitations, dysphagia/dyspnea, finger tremors
NODULAR NON-TOXIC GOITER (NTNG)
Present as an asymmetric anterior neck mass (ANM) that moves with deglutition and usually nodular on palpation; no or minimal
symptoms of hypo/hyperthyroidism
DIFFUSE TOXIC GOITER (DTG)
Presents as symmetric ANM which moves with deglutition and smooth on palpation; with symptoms of hyperthyroidism
FT4 is requested and not total T4 because it is the active form. Free T3 is only requested when both FT4 & TSH are normal and
the pt is clinically hyperthyroid. Between the two, TSH is more diagnostic of hyperthyroidism.
NODULAR TOXIC GOITER
Not very common; presents as an asymmetric ANM which moves with deglutition and nodular on palpation, but presents with
symptoms of hyperthyroidism
Treatment
FNAB is done because of higher rate of occurrence of CA in nodular goiter
DIFFUSE NONTOXIC GOITER
Not very common, presents with symmetric ANM which moves with deglutition and smooth on palpation but has no symptoms of
hyperthyroidism
Treatment
FNAB is not done due to low incidence of CA in DNTG. Thyroid scan is requested to determine the size and activity of the ANM.
Thyroid scan
FT4. TSH
TCB once with results
FNAB
FT4, TSH
PTU 50mg/tab 2 tabs TID (Maximum of 600mg/day)
Propranolol 10mg/tab 1 tab BID (for tachycardia, palpitations, and anxiety)
Refer to ENDO re: NTG
FT4, TSH
CBC with PC & DC
12L ECG
PTU 50mg/tab 2 tabs TID (Maximum of 600mg/day)
Propranolol 10mg/tab 1 tab BID (for tachycardia, palpitations, and anxiety)
Refer to ENDO re: DTG
FNAB
FT4, TSH
TCB once with results
THE THYROID GLAND
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Page 8 of 8 Otorhinolaryngology /epcapul UPCM09
Most common complications of thyroid surgery
a. Hemorrhage if this occurs post-op, remove the sutures immediately to protect the airway
b. Hypocalcemia occurs if all parathyroid glands are inadvertently removed or if ischemia occurs
c. Recurrent laryngeal nerve transaction Pt would present with hoarseness
BELLS PALSY
Facial nerve paralysis (CN VII) usually following viral infection
Grading of Facial Nerve Involvement
1-2 risorius involved; cant smile
3-4 cheeks involved
5 orbicularis involved; cant close eyes
6 frontalis involved; cant wrinkle forehead
TEMPOROMANDIBULAR JOINT DYSFUNCTION
Most common: Myofascial pain and dysfunction, usually the result of bruxism or jaw clenching, related to stress/ anxiety/
depression/ chronic pain.
Less commonly due to mechanical problem or OA. Or primary internal derangement of joint (has clicking during open/close)
leading to disc displacement, due to many causes.
Etiology
a. Traumatic (OA, condylar fx, TMJ subluxation, whiplash, capsulitis synovitis)
b. Dental (malocclusion, reconstruction, poor fitting prosthesis/ dentures/ orthodontics)
c. Iatrogenic (ETT intubation, surgical)
d. Systemic (RA, gout, Pagets, psoriasis)
e. Infectious (GC, syphilis, TB, actinomycosis, RF, Lyme dz --> cyclic pain q1-3mo lasting 7-14d)
f. Congenital (aplasia, hyperplasia, hypoplasia, bifid condyle)
g. Others: stress, bruxism, idiopathic, myofascial pain.
3 Cardinal features
a. orofacial pain Classic: pain in front of tragus with radiation to ear/ lower jaw/ cheek/ temple. Preauricular, temporal, ear that
may radiates to head/face/eye. Pt also may c/o pain in the neck/ shoulder, tinnitus, H-A, insomnia. Pain worse in AM, may
occur in cyclical episodes
b. restricted jaw function - Jaw movement is described as a tightness/ sticking/ catching/locking.
c. noise in the joint (crunch-pop-grind).
Physical Examination
a. Clicking TMJ
b. Check ROM
1. Open & close, <30mm between teeth is abnormal. Should be able to insert your digits 2,3,4 in between pts incisor
teeth.
2. Check the lateral excursion of mandible, ask pt to move his jaw from side to side. Palpate masseter and temporalis m.
Note any excessive occlusal wear, tooth mobility, buccal mucosal ridging, lateral tongue scalloping.
Treatment
a. Conservative effective for 80%: education, stress reduction/ relaxation therapy, modify chewing and other habit that cause
excessive jaw movement. Massage, local moist heat and aerobic exercise. NSAIDs & restricted opening, soft diet to
reduce painful loads.
b. Silicone Night Guard = Interocclusional Appliance/ splint stabilize an occlusion & dec the load on the inflamed joint X 4-
6 week trial
c. Closed reduction and Bartons Manuever
TONSILLITIS
Most commonly caused by Streptococcus sp.
Treated with Clindamycin 150mg/tab (children) or 300mg/tab (adults) a tab TID X 1 week
Soft diet X 1 week
Etoricoxib 120 mg/tab 1 tab OD X 1 week for pain
Wear dentures all the time except during sleep
EMG-NCV
Prednisone 5mg/tab 4 tabs AM, 3 tabs lunch, 2 tabs PM X 2 weeks
Etoricoxib 120 mg/tab for pain
Refer to Neuro
Refer to Ophtha re: Exposure keratitis
THE UPPER AERODIGESTIVE TRACT
Sample Chart Entry
Sample Chart Entry
Page 9 of 9 Otorhinolaryngology /epcapul UPCM09
TONSILOPHARYNGITIS
Treated with Roxithromycin 150mg/tab BID X 1 week
CHRONIC HYPERTROPHIC TONSILS
Treated with tonsillectomy if with indications:
Absolute indications:
a. Malignancy
b. Obstructive sleep apnea
c. Dysphagia leading to significant weight loss
Relative indication: Recurrent tonsillitis (>6x/year)
LARYNGITIS
Acute if <4 weeks; Chronic if >4 weeks.
LARYNGOPHARYNGEAL REFLUX
Characterized by foreign body sensation in the throat
Treated with Omeprazole 20mg/tab 1 tab OD X 2 weeks
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
Characterized by retrosternal chest pain
Treated with Omeprazole 20mg/tab 1 tab OD X 2 weeks
Diet modification: No spicy & sour food, eat small-portioned meals
Sleep at 30 angle and rest the voice
FOREIGN BODY INGESTION
Pt may feel pain on the anatomic location where the FB was lodged (cricopharynx, notch on esophagus, arch of the aorta, L
bronchus, lower esophageal sphincter)
Diagnostics is through radiographic studies which may be repeated every 12 hours. FB appears slit-like when in the esophagus
on lateral x-rays. If FB is in the stomach, refer to Surgery. If it is in the airway but beyond the main bronchi, refer to TCVS. ENT
manages FB in the esophagus and upper airway (trachea & main bronchi)
Barium swallow is done when plain radiographs are non-diagnostics. It is not requested if FB is metallic.
CELLULITIS
ABSCESSES
SOFT TISSUE INFECTIONS
Cloxacillin 500mg/cap 1 cap QID X 7 days
Etoricoxib 120 mg/tab 1 tab OD prn for pain
TCB after 1 week for re-assessment
NPO now
IVF: D5 0.9 NaCl 1L X 8
CXR-APL to include neck and abdomen (in children)
CXR-APL to include the neck, plain abdomen (in adults, a separate neck STL may be requested when not possible)
Lonazolac 200mg/tab 1 tab BID X 2 weeks
Voice rest
Increased OFI
Warm saline gargle
TCB after 2 weeks once with results
For tonsillectomy/GA
SAPOD clearance: CBC with PC & DC, BUN/Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
TCB once with results for OR scheduling
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Page 10 of 10 Otorhinolaryngology /epcapul UPCM09
Include dentoalveolar abscess (DAA), tonsillar abscess, parotid abscess, and parapharyngeal abscess
Treatment
a. Incision and Drainage. Local analgesic is not used since it is not effective in the presence of an abscess.
b. Antibiotics. To cover for G (+) & (-), Pen G is given. To cover for anaerobes, Clindamycin or Metronidazole.
1. For adults:
i. Pen G 4 million units IV LD ( ) ANST then 2 million units q6h
ii. Clindamycin 600mg IV LD ( ) ANST then 300 mg q6h OR
Metronidazole 500mg IV LD ( ) ANST then 250 mg q6h
2. For children:
i. PenG 50,000 units/kg IV LD ( )ANST then 25,000 units/kg q6h
ii. Clindamycin 20 mg/kg IV LD ( ) ANST then 10 mg/kg q6h OR
Metronidazole 15 mg/kg IV LD ( ) ANST then 7.5 mg/kg q6h
3. Preparations
i. Pen G is available in 1 million units/amp preparation
ii. Clindamycin is available in 1,600 mg/amp preparation
4. After IV loading and I&D, the pt may be sent home with the following meds:
i. Pen G 250 mg/tab 1 tab QID to complete 7days (40,000 units = 250mg)
ii. Clindamycin 300mg/tab 1 tab QID to complete 7 days
LUDWIGS ANGINA
Abscess dissecting the muscle planes of the chin which pushes the floor of the mouth upwards
Palpated as a board-like mass in the floor of the mouth
Usually originates forma DAA
Commonly caused by Borrelia or spirochete which is responsive to Pen G / Metronidazole / Clindamycin
REACTIVE LYMPHADENOPATHY
Usually has a focus of infection
Commonly due to dental carries, hair lice, skin infection in the head and neck
Should rule out TB adenitis
TB ADENITIS
May or may not present with chronic cough (>2 weeks), weight loss, failure to gain weight, anorexia
Should rule out reactive LAD
PAROTIDITS
FNAB
CXR AP-L
Sputum AFB X 3
TCB once with results
FNAB
Co-amoxiclav 625 mg/tab TID or 1 g/tab BID X 7 days
TCB after 1 week for re-assessment
S/P I & D
Pen G 4 million units IV LD ( ) ANST then 2 million units q6h
Clindamycin 600mg IV LD ( ) ANST then 300 mg q6h OR
Etoricoxib 120mg/tab 1 tab OD prn for pain
MGH
Advised
TCB after 1 week for re-assessment
S/P I & D
Pen G 4 million units IV LD ( ) ANST then 2 million units q6h
Clindamycin 600mg IV LD ( ) ANST then 300 mg q6h OR
Etoricoxib 120mg/tab 1 tab OD prn for pain
MGH
Advised
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Page 11 of 11 Otorhinolaryngology /epcapul UPCM09
If viral (mumps), treatment is supportive with Etoricoxib 120 mg/tab 1 tab OD prin for pain, bed rest, increased OFI, and
avoidance of close contact with household members
If bacterial, treat with Co-amoxiclav 625 mg/tab TID or 1 g/tab BID X 7 days
NASAL BONE FRACTURE
Common due to its midline location on the face
Most common mechanism of injury is mauling, followed by vehicular accidents
Usually associated with a history of impact to the midfacial area
Said to be neglected if fracture >14 days post-injury
Signs and Symptoms
a. crepitation
b. step-down deformity
c. nasal speculum deviation
d. shortening of the nose
e. increased mobility of the nose
f. anosmia
g. epistaxis
h. CSF rhinorrhea
Treatment
a. Imaging Radiographic studies cannot distinguish between recent and old fractures. Therefore, these are not useful for
medico-legal cases, with a high rate of false negatives and false positives.
1. Waters view information regarding lateral displacement
2. Nose STL demonstrates fracture in the anterior nasal bone
b. Packing control bleeding using antibiotic impregnated nasal pack for 2-5 days. Antibiotics are given as prophylaxis
because nasal bone fractures are usually associated with lacerations of the nasal mucosa or skin.
c. Antibiotics Penicillin (Cloxacillin) and first generation cephalosporin (Cefalexin Cefalexin 500mg cap or 125mg/5mL
suspension) are usually given as prophylactic antibiotics.
d. Pain Medications
e. Closed reduction is done when swelling has subsided to allow for better assessment of the deformity. In children, swelling
usually subsides in <3 days while in adults, it takes 3-5 days. If with airway compromise, dont wait for the swelling to
subside.
f. Open reduction with internal fixation (ORIF) is done only if the fracture is comminuted.
Complications
a. septal hematoma irreversible damage to the underlying cartilage can occur within 3-4 days if not drained
b. infection
c. CSF leak
MAXILLARY FRACTURE
Classification
Lefort I (Guerin fracture) Lefort II (Pyramidal fracture) Lefort III (Craniofacial dysjunction)
Horizontal separation. The palate is
separated form the rest of the maxilla.
Midfacial fracture. The palate with the
maxilla is separated from the zygoma &
ethmoids.
The maxilla and the zygoma are
separated from the cranium passing
through the fronto-ethmoid and the fronto-
zygomatic sutures.
Imaging: Waters view, Caldwell view, Lateral view. CT scan
Waters View
Nose STL
Cloxacillin 500mg/cap 1 cap QID X 7 days
Etoricoxib 120 mg/tab 1 tab OD prn for pain
Cold compress X 15 min TID for the 1
st
24 hours then warm compress thereafter
TCB after
MAXILLO-FACIAL TRAUMA
Sample Chart Entry
Page 12 of 12 Otorhinolaryngology /epcapul UPCM09
MANDIBULAR FRACTURE
Types of muscles acting on Fracture Segments
a. Posterior group upward, forward movement; stronger group. Masseter, lateral & medial pterygoids, & temporalis
b. Anterior group down, backward movement. Geniohyoid, digastric, mylohyoid, genioglossus
Types of mandibular fracture
a. Favorable muscle forces tend to keep fragments together
b. Unfavorable muscle forces tend to pull fragments apart
Imaging studies
a. Panorex view single best radiograph
b. AP- oblique, modified Townes
ZYGOMATIC FRACTURE
Types
a. simple fracture of the arch
b. trimolar or tripod fracture involves all 3 suture lines
c. quadripod fracture maxillary-zygomatic buttress considered
Imaging: Waters, axial or submentovertical views.
CLEFT LIP
May be unilateral or bilateral
Classification
a. Complete cleft reaches the vestibule
b. Incomplete does not reach the vestibule
Rule of Ten: Pt should be at least 10 lbs, 10 weeks, and has 10 mg/dL Hgb
CLEFT PALATE
Reconstruction is performed before 2 years of age to aid in normal speech development. Early attention to nutrition is important
because sucking is impaired.
Thallwitz classification: L_A_H_S_H_A_L_
Divide the key areas of the face (Lip, Alveolus, Hard palate & Soft palate) into thirds. LAH right, HAL - left
LEVELS OF LYMPH NODES
IA submental
IB submandibular
II, III, IV along SCM
V posterior triangle
VI pre-tracheal
VII - paratracheal
NASOPHARYNGEAL CARCINOMA
Presents with epistaxis, nasal obstrucstion, anosmia, constitutional SSx of malignancy
On rhinoscopy, (+) for fungating mass in the nasopharynx
Staging
Primary tumor stage
T1 Tumor confined to nasopharynx
T2 Tumor extends to soft tissues of oropharynx or nasal fossa
T2a Without parapharyngeal extension
T2b With parapharyngeal extension
T3 Tumor invades bony structures or paranasal sinuses
T4 Tumor with intracranial extension or involvement of cranial nerves, infratemporal fossa, hypopharynx, or orbit
Stage groupings
Punch Biopsy /LA
SAPOD Clearance: CBC with DC & PC, BUN, Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
TCB once with results
HEAD & NECK TUMORS
CLEFT LIP AND PALATE
Sample Chart Entry
Page 13 of 13 Otorhinolaryngology /epcapul UPCM09
I T1 N0 M0
IIA T2a N0 M0
IIB T1,2a N1 M0; T2b N0, N1 M0
III T1,2 N2 M0; T3 N0,1,2 M0
IVA T4 N0,1,2 M0
IVB Any T N3 M0
IVC Any T Any N M1
Treatment
Primary tumors: RT alone (bilateral) is used for both the primary tumor and the regional nodal metastases. Surgery is not feasible
because of the inadequacy of the surgical margins at the base of the skull and the frequent involvement of the retropharyngeal and
cervical nodes bilaterally.
PAROTID TUMOR
Benign tumors are more common than malignant ones
If bilateral, probably Warthins tumor
Most common histologic types are
1. Benign mixed tumor major salivary gland; with pseudopods so remove mass with margins; with 1% malignant
transformation.
2. Malignant adenoid cystic CA more common in minor salivary glands.
3. Mucoepidermoid cyst - malignant
Staging of Salivary Gland Carcinoma
Primary tumor stage
TX Primary tumor cannot be assessed
T0 No evidence of primary tumor
T1 Tumor <2 cm without extraparenchymal extension
T2 Tumor >2 cm but <4 cm extraparenchymal extension
T3 Tumor >4 cm but <6 cm or having extraparenchymal extension without seventh cranial nerve involvement
T4 Tumor invades base of skull or seventh nerve or is >6 cm
Stage groupings for major salivary gland carcinomas
I T1,2,3 N0 M0
II T3 N0 M0
III T1,2 N1 M0
IV T4 N0 M0; T3,4 N1 M0; any T N2,3 M0; any T any N M1
MAXILLARY CARCINOMA
Most common type is SCCA, followed by adenoid cystic CA
MUCOUS RETENTION CYST
Originates from the maxillary sinuses
Usually not touched, but may do puncture via Caldwell-luc if hard enough
LARYNGEAL CARCINOMA
Presents with hoarseness (other causes included VC mass, VC inflammation, VC paralysis)
Involvement of the cricoid cartilage indicates a subglottic extension which has a poorer prognosis
Pt is sent to the ER if with dyspnea for emergency tracheostomy and then possible admission for further work-up
Total laryngectomy with next dissection is done for proven laryngeal CA
Staging
Primary Tumor
FNAB
SAPOD Clearance: CBC with DC & PC, BUN, Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
TCB once with results
FNAB
SAPOD Clearance: CBC with DC & PC, BUN, Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
TCB once with results
Direct laryngoscopy with biopsy of laryngeal mass/LA
SAPOD Clearance: CBC with DC & PC, BUN, Crea, RBS/FBS, Na, K, Cl, U/A, 12L ECG, CXR
TCB once with results
Sample Chart Entry
Sample Chart Entry
Sample Chart Entry
Page 14 of 14 Otorhinolaryngology /epcapul UPCM09
Supraglottis Glottic Subglottic
Tis Carcinoma-in-situ Carcinoma-in-situ
T1 Tumor confined to site of origin with normal
mobility
Tumor confined to vocal cord(s) with
normal vocal cord mobility
T1a limited to one vocal cord
T1b with involvement of anterior
commisure
Tumor confined to subglottic
area
T2 Tumor involves adjacent supraglottic sites or
glottis without fixation
Supraglottic or subglottic extensionof
tumor with normal or impaired mobility
Tumor extension to vocal cords
with normal or impaired cord
mobility
T3 Tumor limited to larynx with fixation or extension
to involve postcricoid area, medial wall of
pyriform sinus or pre-epiglottic space
Tumor confined to larynx with cord
fixation
Tumor confined to larynx with
cord fixation
T4 Massive tumor extending beyond the larynx to
oropharynx, skin or soft tissues of neck, or
destruction of thyroid cartilage
Massive tumor with thyroid cartilage
destruction or extension beyond
confines of larynx or both
Massive tumor with cartilage
destruction or extension beyond
confines of larynx
Nodal Involvement
Nx minimum requirements to assess the regional nodes cannot be met
NO no clinically positive nodes
N1 clinically positive homolateral nodes
N2 contralateral or bilateral nodes not fixed
N3 fixed nodes
Distant Metastasis
Mx minimum requirements for assessment of distant metastasis cannot be met
MO no distant metastasis
M1 distant metastasis present
Staging
I T1 NO MO
II T2 NO MO
III T3 NO MO; T1, T2, T3 N1 MO
IV T4 NO MO; T4 NO MO; Any T N2, N3 MO; Any N M1
Indications for Emergency Tracheostomy
a. Foreign body occluding the airway
b. Retropharyngeal abscess
c. Tetanus
d. Severe myasthenia gravis
e. Laryngeal CA with Obstruction
THYROID CARCINOMA
PAPILLARY CANCER
Most common, affect younger patients.
Psammoma bodies are usually present in histologic sections.
Distant metastases to lungs, bone, skin, and other organs occur late.
Papillary = Popular = Psammoma = Palpable lymph nodes = Positve
131
I uptake = Positive prognosis = Post-op
131
I scan to
diagnose/treat metastases
Staging
Primary tumor (T)
TX: Primary tumor cannot be assessed.
T0: No evidence of primary tumor is found.
T1: Tumor size is 2 cm or less in greatest dimension and is limited to the thyroid.
T2: Tumor size is greater than 2 cm but less than 4 cm, and tumor is limited to the thyroid.
T3: Tumor size is greater than 4 cm, and tumor is limited to the thyroid or any tumor with minimal extrathyroidal extension
(extension to sternothyroid muscle of perithyroid soft tissues).
T4a: Tumor extends beyond the thyroid capsule and invades any of the following: subcutaneous soft tissues, larynx, trachea,
esophagus, or recurrent laryngeal nerve.
T4b: Tumor invades prevertebral fascia, mediastinal vessels, or encases the carotid artery.
Regional lymph nodes (N)
NX: Regional nodes cannot be assessed.
N0: No regional node metastasis is found.
N1a: Metastasis is found in level VI (pretracheal and paratracheal, including prelaryngeal and Delphian) lymph nodes.
N1b: Metastasis is found in unilateral, bilateral, or contralateral cervical or upper/superior mediastinal lymph nodes.
Distant metastasis (M)
MX: Distant metastasis cannot be assessed.
M0: No distant metastasis is found.
M1: Distant metastasis is present.
Stages
Stage Younger Than 45 Years Age 45 Years and Older
Page 15 of 15 Otorhinolaryngology /epcapul UPCM09
I Any T, Any N, M0 T1, N0, M0
II Any T, Any N, M1 T2, N0, M0
III T3, N0, M0, T1, T2, T3, N1a, M0
IVa T1, T2, T3, N1b, M0, T4a, N0, N1, M0
IVb T4b, any N, M0
IVc Any T, any N, M1
FOLLICULAR CANCER
Peak incidence at 40 years of age.
They tend to invade blood vessels and to metastasize hematogenously to visceral sites, particularly bone. Lymph node
metastases are relatively rare, especially compared with papillary cancers.
Hrthle cell cancer is a variant of follicular carcinoma and has a relatively aggressive metastatic course.
Follicular = Far-away metastasis = Female (3:1) = FNAB NOT (diagnosed by tissue structure) = Favorable prognosis
Staging
Stage Younger Than 45 Years Age 45 Years and Older
I
Any T, any N, M0 (Cancer is in the thyroid
only)
T1, N0, M0 (Cancer is in the thyroid only and may be found in one or both
lobes)
II
Any T, any N, M1 (Cancer has spread to
distant organs)
T2, N0, M0 and T3, N0, M0 (Cancer is in the thyroid only and is larger than
1.5 cm)
III
T4, N0, M0 and any T, N1, M0 (Cancer has spread outside the thyroid but
not outside of the neck)
IV Any T, any N, M1 (Cancer has spread to other parts of the body)
MEDULLARY THYROID CANCER
Secrete calcitonin. ACTH, histaminase, and an unidentified substance that produces diarrhea may also be secreted by these
tumors. Large amounts of amyloid are evident by histologic examination.
Metastases are mostly found in the neck and mediastinal lymph nodes and may calcify. Widespread visceral metastases occur
late.
Medullary = MEN II = aMyloid = Median lymph node dissection = Modified neck dissection if lateral nodes are positive
Staging
I Cancer is less than 1 centimeter (about 1/2 inch) in size.
II Cancer is between 1 and 4 centimeters (about 1/2 to 1 1/2 inches) in size.
III Cancer has spread to the lymph nodes.
IV Cancer has spread to other parts of the body.
ANAPLASTIC GIANT AND SPINDLE CELL CANCER
Occur most often in patients older than 60 years of age. Anaplastic thyroid cancers are aggressive cancers, which rapidly invade
surrounding local tissues and metastasize to distant organs.
There is no number staging system used for anaplastic cancer.
Other tumors found in the thyroid include Hodgkin lymphomas, a variety of soft tissue sarcomas, and metastatic cancers of lung,
colon, and other primary sites. Small cell cancers of the thyroid are rare, are histologically similar to lymphoma, and spread to both
lymph nodes and distant sites.
References:
Braganza, RA, Otolaryngology, Head & Neck Surgery.
Blackbourne, L. Surgical Recall 4
th
ed. 2006.
Caparas, et. al. Basic Otolaryngology. 1993.
Class 2004. Otorhinolaryngology Reviewer.
eMedicine
Jarell et. al. Surgery NMS. 5
th
ed. 2008.
Oncology. 4th Ed.
www.craniofacialcenter.com/book/Trauma/Trauma_3.htm
www.medscape.com
You might also like
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- ORL Interns NotesDocument15 pagesORL Interns NotesSandy Chiong MaganitoNo ratings yet
- INTERNS NOTES - OtorhinolaryngologyDocument15 pagesINTERNS NOTES - OtorhinolaryngologyKarl Jimenez SeparaNo ratings yet
- ENT MCQforstudents AnswersDocument30 pagesENT MCQforstudents AnswersOlaNo ratings yet
- Common ENT Conditions PwPT2008Document75 pagesCommon ENT Conditions PwPT2008Garlic BreadNo ratings yet
- diagnosis-of-ent-disorders-you-make-the-callDocument137 pagesdiagnosis-of-ent-disorders-you-make-the-callsaifsaffa2No ratings yet
- ENT Previous Year QuestionsDocument13 pagesENT Previous Year QuestionsKoki AlagarNo ratings yet
- مراجعة الأوسكىDocument238 pagesمراجعة الأوسكىHala BahaaNo ratings yet
- EntDocument32 pagesEntaini natasha100% (3)
- ENT Lectures 1Document123 pagesENT Lectures 1lxnalexander100% (1)
- Otits MediaDocument68 pagesOtits MediaSaidi EdwardNo ratings yet
- Ears&MouthDocument76 pagesEars&Mouthrichelley08No ratings yet
- Common Ent Emergencies 24126Document64 pagesCommon Ent Emergencies 24126Krittin NaravejsakulNo ratings yet
- Drugs and Substance AbuseDocument75 pagesDrugs and Substance Abuseseline sherylNo ratings yet
- Common Ent EmergenciesDocument65 pagesCommon Ent EmergenciesferaNo ratings yet
- Ear Procedure Guideline: Treatment ModalitiesDocument12 pagesEar Procedure Guideline: Treatment ModalitiesissaiahnicolleNo ratings yet
- Eardrum Repair Surgery DefinitionDocument4 pagesEardrum Repair Surgery DefinitionMelly Selvia ANo ratings yet
- Acute Diffuse Otitis ExternaDocument36 pagesAcute Diffuse Otitis ExternaIlham Isnin Dolyanov HasibuanNo ratings yet
- 11 - Otitis - PrecDocument6 pages11 - Otitis - PrecRhaina KhairaniNo ratings yet
- Ear Infection Assessment and ManagementDocument8 pagesEar Infection Assessment and ManagementArt Christian Ramos100% (1)
- Concept Book Ent Working FileDocument801 pagesConcept Book Ent Working FileDrAssadullah HamzaNo ratings yet
- Nur 218 Peds Exam 1 Study Guide Role of The Pediatric NurseDocument9 pagesNur 218 Peds Exam 1 Study Guide Role of The Pediatric NurseNurseme13No ratings yet
- Ear ExaminationDocument47 pagesEar ExaminationHarshit Bhardwaj100% (4)
- Acute Otitis MediaDocument16 pagesAcute Otitis Mediaadrianne18sNo ratings yet
- OtosclerosisDocument9 pagesOtosclerosisSuprit SnNo ratings yet
- Case DR - Oscar OMADocument8 pagesCase DR - Oscar OMApasukan5jari100% (1)
- CSOM Retroauricular FistulaDocument154 pagesCSOM Retroauricular FistulaM.rizki DestiantoroNo ratings yet
- CSOM Retroauricular FistulaDocument151 pagesCSOM Retroauricular FistulaM.rizki DestiantoroNo ratings yet
- CASE ANALYSIS - Chronic TympanomastoiditisDocument5 pagesCASE ANALYSIS - Chronic TympanomastoiditisTerry Mae Atilazal SarciaNo ratings yet
- ENT Urgencies / Emergencies in Primary CareDocument55 pagesENT Urgencies / Emergencies in Primary CareDr_Aan_ArdiansyahNo ratings yet
- Maxillary Sinus Anatomy and Oroantral FistulaDocument26 pagesMaxillary Sinus Anatomy and Oroantral FistulaRobins DhakalNo ratings yet
- Respiratory SystemDocument24 pagesRespiratory SystemHani El-asferNo ratings yet
- ENTDocument40 pagesENTwhoosh2008No ratings yet
- Otitis MediaDocument26 pagesOtitis MediaRiteka SinghNo ratings yet
- Presentation Otitis ExternaDocument24 pagesPresentation Otitis ExternaRichard GunawanNo ratings yet
- Choanal Atresia sDocument4 pagesChoanal Atresia sCosbyNo ratings yet
- Earache and DischargeDocument24 pagesEarache and Dischargearianne javierNo ratings yet
- ENT Ear I Scenarios (Compiled)Document35 pagesENT Ear I Scenarios (Compiled)rumman tariqNo ratings yet
- Respiratory Disorders ExplainedDocument89 pagesRespiratory Disorders ExplainedSyed MaazNo ratings yet
- Otitis MediaDocument67 pagesOtitis MediaFurqan MirzaNo ratings yet
- Clinical Manual of OtolaryngologyDocument49 pagesClinical Manual of Otolaryngologygamecockusc1992100% (3)
- Understanding Otitis Media: Causes, Symptoms and Treatment of Ear InfectionsDocument98 pagesUnderstanding Otitis Media: Causes, Symptoms and Treatment of Ear InfectionsLody Lean CruzNo ratings yet
- Deviated Nasal SeptumDocument15 pagesDeviated Nasal SeptumSrinivas Sukhavasi50% (2)
- ENT Emergency PresentationDocument135 pagesENT Emergency PresentationshahiruddinNo ratings yet
- EntDocument105 pagesEntNikhil KumarNo ratings yet
- ENT - Clinical NotesDocument114 pagesENT - Clinical NotesTANINo ratings yet
- The Ear, Nose, and Throat Exam: Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, Usa LT, MC, UsnDocument37 pagesThe Ear, Nose, and Throat Exam: Jeffrey Texiera, MD and Joshua Jabaut, MD CPT, MC, Usa LT, MC, Usnsaraswati SabatNo ratings yet
- Choanal Atresia Diagnosis and TreatmentDocument12 pagesChoanal Atresia Diagnosis and Treatmentsubinj_350% (2)
- Assessing Ear Pain in ChildrenDocument20 pagesAssessing Ear Pain in ChildrenPrince K. TaileyNo ratings yet
- Ear: Anatomy, Common Conditions, and Clinical EvaluationDocument19 pagesEar: Anatomy, Common Conditions, and Clinical EvaluationleeNo ratings yet
- Presenters: Eko Nugroho Fariz Afristya Raymond Win Ruli Aulia Stacy GabriellaDocument48 pagesPresenters: Eko Nugroho Fariz Afristya Raymond Win Ruli Aulia Stacy GabriellaYosephine ninaNo ratings yet
- Ear ExaminationDocument13 pagesEar Examinationsejal3vijNo ratings yet
- Expose On EntDocument20 pagesExpose On EntDUCHELNo ratings yet
- Hearing Loss in Children - Etiology - UpToDateDocument39 pagesHearing Loss in Children - Etiology - UpToDateAlexander AdrielNo ratings yet
- Tympanoplasty Indications, Types, ProcedureDocument55 pagesTympanoplasty Indications, Types, ProcedurePrasanna DattaNo ratings yet
- CSOMDocument50 pagesCSOMFurqan MirzaNo ratings yet
- OHNS--Otolaryngology; Head and Neck surgery: pocket field guideFrom EverandOHNS--Otolaryngology; Head and Neck surgery: pocket field guideNo ratings yet
- Anaphylaxis: A Practical GuideFrom EverandAnaphylaxis: A Practical GuideAnne K. EllisNo ratings yet
- 3rd Paragraph PDFDocument36 pages3rd Paragraph PDFDaphne Ongbit JaritoNo ratings yet
- Maternal Mortality Among Women Seeking Health Care Services in Kisii Level 5 HospitalDocument6 pagesMaternal Mortality Among Women Seeking Health Care Services in Kisii Level 5 HospitalDaphne Ongbit JaritoNo ratings yet
- Risk factors for carcinogenesis in choledochal cyst patientsF/491Gender/AgeTodanitypeTable 1. Clinical characteristics of 15 patients with malignant tumors arising from choledochal cystsDocument8 pagesRisk factors for carcinogenesis in choledochal cyst patientsF/491Gender/AgeTodanitypeTable 1. Clinical characteristics of 15 patients with malignant tumors arising from choledochal cystsDaphne Ongbit JaritoNo ratings yet
- 2014 Evidence-Based Guideline For The Management HypertensionDocument14 pages2014 Evidence-Based Guideline For The Management HypertensionEganata NugrahaNo ratings yet
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolNo ratings yet
- 30a2131 Complete Blood Count Normal Pediatric Values PDFDocument1 page30a2131 Complete Blood Count Normal Pediatric Values PDFReziel Basilan Manalo100% (2)
- Banco de Oro (BDO) - Online Bills Payment: Credit ScheduleDocument1 pageBanco de Oro (BDO) - Online Bills Payment: Credit ScheduleDaphne Ongbit JaritoNo ratings yet
- ProposalDocument14 pagesProposalDaphne Ongbit JaritoNo ratings yet
- Gold in IRA - May6Document5 pagesGold in IRA - May6Daphne Ongbit JaritoNo ratings yet
- Acute Diare WHO 2005Document50 pagesAcute Diare WHO 2005Boby Abdul RahmanNo ratings yet
- CholeDocument4 pagesCholeDaphne Ongbit JaritoNo ratings yet
- CholeDocument4 pagesCholeDaphne Ongbit JaritoNo ratings yet
- Southwestern University Matias H. Aznar Memorial College of Medicine Urgello ST., Cebu City, PhilippinesDocument1 pageSouthwestern University Matias H. Aznar Memorial College of Medicine Urgello ST., Cebu City, PhilippinesDaphne Ongbit JaritoNo ratings yet
- Tetanus: Introduced in 1930s (DT) and 1952/3 (DTP) NotifiableDocument8 pagesTetanus: Introduced in 1930s (DT) and 1952/3 (DTP) NotifiableDaphne Ongbit JaritoNo ratings yet
- SSC Bundle PDFDocument1 pageSSC Bundle PDFBramantyo NugrahaNo ratings yet
- Clinician Rated Severity of Oppositional Defiant DisorderDocument2 pagesClinician Rated Severity of Oppositional Defiant DisorderDaphne Ongbit JaritoNo ratings yet
- Nervous System Functions and Neuron CommunicationDocument8 pagesNervous System Functions and Neuron CommunicationDaphne Ongbit JaritoNo ratings yet
- CHED ) Region 7 Forum 5514Document7 pagesCHED ) Region 7 Forum 5514Daphne Ongbit JaritoNo ratings yet
- Board Exam PrimerDocument9 pagesBoard Exam PrimerEngr Jibril Naval Labiao67% (3)
- A Lectin With Antifungal and Mitogenic Activities From Capsicum FrutescensDocument7 pagesA Lectin With Antifungal and Mitogenic Activities From Capsicum FrutescensDaphne Ongbit JaritoNo ratings yet
- 4 Computer System LecDocument9 pages4 Computer System LecDaphne Ongbit JaritoNo ratings yet
- A Brief History of Organic ChemistryDocument5 pagesA Brief History of Organic ChemistryDaphne Ongbit JaritoNo ratings yet
- Picot Presntation 2Document18 pagesPicot Presntation 2api-650274498No ratings yet
- Cancer IntroDocument29 pagesCancer Intromara5140No ratings yet
- Brain Tumor Detection Using CNNDocument10 pagesBrain Tumor Detection Using CNNIJRASETPublicationsNo ratings yet
- World Teachers' Day Celebration: 15 R C Y Chapter Wide Youth CampDocument16 pagesWorld Teachers' Day Celebration: 15 R C Y Chapter Wide Youth CampLevy LigaoNo ratings yet
- Cure For PolioDocument51 pagesCure For PoliohgutierrezcableNo ratings yet
- St. Paul University's 4th Quarter Health Education 7 DIPDocument8 pagesSt. Paul University's 4th Quarter Health Education 7 DIPClarisse-joan Bumanglag GarmaNo ratings yet
- GL Medic Surv 2001 PDFDocument139 pagesGL Medic Surv 2001 PDFAlief AzizNo ratings yet
- Analysis of Anticancer Drugs: A Review: TalantaDocument25 pagesAnalysis of Anticancer Drugs: A Review: Talantasrayu2603No ratings yet
- (Biomedical Engineering) : BM: Biosciences and BioengineeringDocument22 pages(Biomedical Engineering) : BM: Biosciences and BioengineeringDevasyaNo ratings yet
- Cancer Pain: Who Guidelines ForDocument2 pagesCancer Pain: Who Guidelines ForBean GemboelzNo ratings yet
- Hospital Expenditure Report by DoctorDocument32 pagesHospital Expenditure Report by Doctorgalih wicaksonoNo ratings yet
- 2012 Levasseur Activate PDFDocument109 pages2012 Levasseur Activate PDFMaybelline DipasupilNo ratings yet
- Dhikr Therapy For Reducing Anxiety in Cancer PatientDocument6 pagesDhikr Therapy For Reducing Anxiety in Cancer PatientRisfialdo Lily WidiatamaNo ratings yet
- Anti Aging Plan PDFDocument352 pagesAnti Aging Plan PDFVladimirDimchevNo ratings yet
- Oncology NursingDocument12 pagesOncology NursingDick Morgan Ferrer80% (5)
- J. Biol. Chem.-2020-Traughber-8252-61Document11 pagesJ. Biol. Chem.-2020-Traughber-8252-61exoNo ratings yet
- B The Can Be Given IntramuscularDocument14 pagesB The Can Be Given IntramuscularHussein Ismail ZannounNo ratings yet
- 2008-CE337 - The Intraoral and Extraoral ExamDocument33 pages2008-CE337 - The Intraoral and Extraoral Examyongky100% (1)
- SARMS Powders Prices - David FromDocument1 pageSARMS Powders Prices - David FromOld World OrderNo ratings yet
- 2016 WHO Classification of Tumours of The Central Nervous System (Digitalizado)Document411 pages2016 WHO Classification of Tumours of The Central Nervous System (Digitalizado)Juan Eduardo Rocha Aguirre50% (2)
- NUS Engineering Annual Report 2016Document23 pagesNUS Engineering Annual Report 2016Glenden KhewNo ratings yet
- Article 1Document21 pagesArticle 1Diana RiosNo ratings yet
- PE1 Module Week 1Document7 pagesPE1 Module Week 1마이No ratings yet
- 2013 in ScienceDocument73 pages2013 in SciencescribdreaderplusNo ratings yet
- CBEDocument17 pagesCBElovtetaNo ratings yet
- Johanna Budwig Diet ProtocolDocument43 pagesJohanna Budwig Diet Protocolchatkat66100% (1)
- Listado Libros SpringerDocument479 pagesListado Libros SpringerMichael Cano LombardoNo ratings yet
- Radiology PDFDocument81 pagesRadiology PDFrawaNo ratings yet
- Jurnal Tonsil Limfoma Non HodgkinDocument5 pagesJurnal Tonsil Limfoma Non HodgkinAhmad RamadhanuNo ratings yet
- The Femal Lower Genital Tract and CervixDocument70 pagesThe Femal Lower Genital Tract and CervixHussein MreydemNo ratings yet