Professional Documents
Culture Documents
Niveles de Vanco
Uploaded by
giseladelarosa2006Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Niveles de Vanco
Uploaded by
giseladelarosa2006Copyright:
Available Formats
RESEARCH ARTI CLE Open Access
Effect of vancomycin serum trough levels on
outcomes in patients with nosocomial
pneumonia due to Staphylococcus aureus: a
retrospective, post hoc, subgroup analysis of the
Phase 3 ATTAIN studies
Steven L Barriere
1*
, Martin E Stryjewski
2
, G Ralph Corey
3
, Fredric C Genter
1
and Ethan Rubinstein
4
Abstract
Background: Existing data are not consistently supportive of improved clinical outcome when vancomycin dosing
regimens aimed at achieving target trough levels are used. A retrospective, post hoc, subgroup analysis of
prospectively collected data from the Phase 3 ATTAIN trials of telavancin versus vancomycin for treatment of
nosocomial pneumonia was conducted to further investigate the relationship between vancomycin serum trough
levels and patient outcome.
Methods: Study patients were enrolled in 274 study sites across 38 countries. A total of 98 patients had
Staphylococcus aureus nosocomial pneumonia and vancomycin serum trough levels available. These patients were
grouped according to their median vancomycin trough level; < 10 g/mL, 10 g/mL to < 15 g/mL, and 15 g/mL.
Results: Clinical cure rates in the < 10 g/mL, 10 g/mL to < 15 g/mL, and 15 g/mL vancomycin trough level
groups were 70% (21/30), 55% (18/33), and 49% (17/35), respectively (p = 0.09), and the frequencies of patient death
were 10% (3/30), 15% (5/33), and 20% (7/35), respectively (p = 0.31). Renal adverse events were more frequent in
the 15 g/mL (17% [6/35]) than the < 10 g/mL (0%) and 10 g/mL to < 15 g/mL (3% [1/33]) trough level groups
(p < 0.01). When patients with acute renal failure or vancomycin exposure within 7 days prior to study medication were
excluded, clinical cure rates in the < 10 g/mL, 10 g/mL to < 15 g/mL, and 15 g/mL vancomycin trough level
groups (71% [12/17], 60% [9/15], and 27% [3/11], respectively; p = 0.04) and the number of deaths (12% [2/17], 20%
[3/15], and 45% [5/11], respectively; p = 0.07) demonstrated a trend towards worse outcomes in the higher vancomycin
trough level groups.
Conclusions: The findings of our study suggest that higher vancomycin trough levels do not result in improved
clinical response but likely increase the incidence of nephrotoxicity.
Trial registration: NCT00107952 and NCT00124020
Keywords: Vancomycin, Trough levels, Nosocomial pneumonia, Staphylococcus aureus
* Correspondence: sbarriere@theravance.com
1
Theravance, Inc., South San Francisco, CA 94080, USA
Full list of author information is available at the end of the article
2014 Barriere et al.; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative
Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and
reproduction in any medium, provided the original work is properly credited.
Barriere et al. BMC Infectious Diseases 2014, 14:183
http://www.biomedcentral.com/1471-2334/14/183
Background
Staphylococcus aureus has emerged as a major cause of
nosocomial pneumonia (NP), with rates of methicillin-
resistant strains (MRSA) as high as 70% reported in some
US studies [1]. Vancomycin, linezolid, and telavancin are
currently approved for treatment of NP due to MRSA in
the United States [2].
Vancomycin serum trough levels of 515 g/mL have
previously been targeted to optimize clinical outcome in
patients with NP, although more recent literature suggests
a vancomycin trough level of 1520 g/mL [3]. This range
of trough concentrations is required to achieve the pre-
sumed optimal vancomycin AUC/MIC (area under the
curve/minimum inhibitory concentration) target of > 400
for S. aureus with MIC values 1 g/mL [3].
Existing data are not consistently supportive of im-
proved clinical outcome when vancomycin dosing regi-
mens aimed at achieving this AUC/MIC target are used
[4,5]. Most recently, the results of the Phase 4 ZEPHyR
trial comparing vancomycin with linezolid for MRSA
NP found that higher trough levels of vancomycin were
associated with lower cure rates [6].
In terms of safety, several investigations indicate
that vancomycin serum levels > 15 g/mL [5,7], and
particularly > 20 g/mL [8], can result in significant
nephrotoxicity. Using Monte Carlo simulation and a
pharmacokinetic/pharmacodynamic model derived from
patient data, Patel et al. [9] suggested that for infections
due to S. aureus with MIC values 1 g/mL, vanco-
mycin doses with an acceptable probability of AUC/
MIC target attainment would result in unacceptable
levels of nephrotoxicity.
Using prospectively collected data from the Assess-
ment of Telavancin for Treatment of Hospital-Acquired
Pneumonia (ATTAIN) Phase 3 clinical trials, we sought
to further elucidate the relationship between measured
vancomycin trough concentrations and clinical response,
overall safety, incidence of nephrotoxicity, and mortality
in patients with S. aureus NP.
Methods
The ATTAIN trials were two identical, randomized,
double-blind, comparator-controlled, parallel-group, Phase
3 studies (NCT00107952 and NCT00124020) investigating
the efficacy and safety of telavancin versus vancomycin for
treatment of Gram-positive NP in adult patients [10]. The
institutional review board at each site approved the
protocol (see Additional files 1 and 2), and all patients
or their authorized representatives provided written in-
formed consent.
Vancomycin was administered at 1 g every 12 hours
for 721 days. Investigators were not provided with spe-
cific vancomycin trough recommendations as there were
no authoritative guidelines available when the studies
were conducted. Vancomycin dosing could be monitored
and adjusted for weight and/or renal function according
to site-specific standard procedures (while maintaining
study blind).
The analysis population for the current investigation
consisted of patients in the ATTAIN all-treated (AT)
population (all randomized patients who received 1 dose
of study medication) who had S. aureus NP and vanco-
mycin serum trough levels available. These patients were
grouped according to their median vancomycin trough level
over the study period; < 10 g/mL, 10 g/mL to < 15 g/
mL, and 15 g/mL.
Clinical cure was defined as improvement or lack of
progression of baseline radiographic findings at end of
study therapy (EOT) and resolution of signs and symp-
toms of pneumonia at the test of cure (TOC) visit. Failure
was defined as persistence or progression of signs and
symptoms or progression of radiological signs of pneumo-
nia at EOT; termination of study medications due to lack
of efficacy and initiation within two calendar days of a
different potentially effective anti-staphylococcal medica-
tion; death on or after Day 3 attributable to primary infec-
tion; or relapsed infection at TOC. Renal adverse events
(AEs) were defined by the investigators as acute renal fail-
ure, chronic renal failure, renal impairment, renal insuffi-
ciency, and/or by laboratory values as increased creatinine
(at least 1.5 baseline to a value 1.5 mg/dL). In patients
with preexisting renal dysfunction, renal adverse events
were defined if they had a worsening of their baseline
renal function during the study. Increased creatinine was
defined programmatically using laboratory data. Kruskall-
Wallis for continuous variables (e.g., age and Acute Physi-
ology and Chronic Health Evaluation II (APACHE II)
score) and Cochran-Mantel-Haenszel general association
statistics for categorical variables (e.g., acute renal failure
and bacteremia) were used to compare the baseline
characteristics across the three vancomycin trough groups
(< 10 g/mL, 10 g/mL to < 15 g/mL, and 15 g/mL).
Cochran-Armitage trend test was used to evaluate clinical
outcomes. No adjustment for multiple comparisons was
made and a nominal two-sided p-value of < 0.05 was con-
sidered statistically significant.
Results
Vancomycin serum trough levels were available from 98
patients with S. aureus NP in the ATTAIN AT population;
30, 33, and 35 patients had median vancomycin trough
levels of < 10 g/mL, 10 g/mL to < 15 g/mL, and 15 g/
mL, respectively. Baseline patient characteristics were gen-
erally similar between the three vancomycin trough level
groups, although there was a greater proportion of patients
who had failed prior antibiotic treatment in the higher
vancomycin trough groups (p = 0.002; Table 1). While not
statistically significantly different, more patients in the
Barriere et al. BMC Infectious Diseases 2014, 14:183 Page 2 of 5
http://www.biomedcentral.com/1471-2334/14/183
higher vancomycin trough groups had preexisting acute
renal failure or multilobar pneumonia, and there were more
bacteremic patients in the lower vancomycin trough groups
(Table 1). Despite these differences, APACHE II scores
were similar between the vancomycin trough groups
(Table 1). Median trough levels were similar in patients
who received 7 days or > 7 days of therapy with vanco-
mycin (data not shown).
No statistically significant relationship was observed be-
tween clinical cure or the number of deaths and vanco-
mycin trough level (Table 2). In addition, median length
of therapy did not differ between the groups (Table 2).
However, when patients with acute renal failure or vanco-
mycin exposure within the 7 days prior to the first dose
of study medication were excluded, there was a trend to-
wards lower clinical cure rates (p = 0.04) and a greater
number of deaths (p = 0.07) in the higher vancomycin
trough groups (Table 2). There was a greater incidence of
serious AEs and renal AEs as the vancomycin trough level
increased (p = 0.03 and p < 0.01, respectively) (Table 2).
This relationship was maintained when patients with acute
renal failure or vancomycin exposure within the 7 days
prior to the first dose of study medication were excluded
(p = 0.02 and p = 0.01, respectively) (Table 2).
Discussion
This analysis of patients treated with vancomycin for NP
suggests that clinical outcomes were not improved when
recommended vancomycin trough levels ( 15 g/mL)
were achieved [3]. Importantly, all but one patient was
infected with S. aureus isolates with MIC values 1 g/
mL, indicating that nearly all patients with a vancomycin
trough level 15 g/mL should have achieved the rec-
ommended AUC/MIC target [3]. The worse outcomes
observed in the higher vancomycin trough groups may
reflect differences in patient baseline characteristics be-
tween the groups. Specifically, acute renal failure was
more common in the higher vancomycin trough groups,
which may have influenced vancomycin distribution, and
is also associated with poor clinical outcomes. Further-
more, investigators may have employed more aggressive
dosing in patients with infections that were perceived to
be more severe due to prior antimicrobial treatment fail-
ure or multilobar involvement, both of which were more
common in the higher vancomycin trough groups.
There was more nephrotoxicity associated with the
higher vancomycin troughs, consistent with previous re-
ports [5,7,8,11] and a recent prospective study [12]. Al-
though this may also be attributable to a greater number
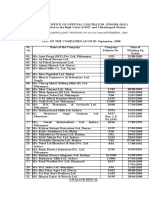
Table 1 Baseline characteristics and clinical outcomes of ATTAIN study patients with Staphylococcus aureus nosocomial
pneumonia according to vancomycin trough levels
Vancomycin trough level (g/mL), n (%)
*
p
< 10 (n = 30) 10 to < 15 (n = 33) 15 (n = 35)
Age (mean SD, year) 60 20 69 13 69 14 0.14
APACHE II score (mean SD) 16 5 17 7 18 6 0.45
Creatinine clearance 50 mL/min 10 (33) 18 (55) 14 (40) 0.22
Acute renal failure 2 (7) 5 (15) 10 (29) 0.06
Multilobar pneumonia 17 (57) 19 (58) 28 (80) 0.08
Bacteremia
6 (20) 2 (6) 2 (6) 0.10
Resident in ICU 20 (67) 24 (73) 28 (80) 0.48
Use of vasopressor/inotropic 5 (17) 5 (15) 7 (20) 0.87
Shock 2 (7) 2 (6) 4 (11) 0.68
Potentially nephrotoxic prior antibiotic therapy
Vancomycin 11 (37) 14 (42) 17 (49) 0.63
Amikacin 1 (3) 1 (3) 2 (6)
Gentamicin 0 2 (6) 1 (3)
Prior antibiotic failure 11 (37) 18 (55) 28 (80) 0.002
MRSA 20 (67) 26 (79) 30 (86) 0.18
Staphylococcus aureus MIC > 1 g/mL 0 0 1 (3) 0.41
APACHE II, Acute Physiology and Chronic Health Evaluation II; ATTAIN, Assessment of Telavancin for Treatment of Hospital-Acquired Pneumonia; ICU, intensive
care unit; MIC, minimum inhibitory concentration; MRSA, methicillin-resistant Staphylococcus aureus; SD, standard deviation.
*
Unless otherwise stated.
Kruskall-Wallis or Cochran-Mantel-Haenszel general association.
S. aureus recovered from baseline blood cultures.
Barriere et al. BMC Infectious Diseases 2014, 14:183 Page 3 of 5
http://www.biomedcentral.com/1471-2334/14/183
of patients with severe infections in the higher trough
population, exclusion of the patients with major risk fac-
tors for nephrotoxicity did not change the observed trend.
Concomitant medications also may contribute to the renal
toxicity observed. In the study by Hidayat et al. [13],
nephrotoxicity was reported in 11 of 95 subjects. Ten of
these 11 subjects received concomitant nephrotoxic agents;
in contrast, only 17 of the 84 subjects (20%) with no renal
toxicity received nephrotoxic agents (interestingly, all 11
cases of renal toxicity occurred in the 63 subjects who had
vancomycin trough levels of 1520 g/mL). A post hoc
examination of our own data revealed prior and/or
concomitant use of one or more known nephrotoxic agents
in 40%, 42%, and 54% of patients in the < 10 g/mL,
10 g/mL to < 15 g/mL, and 15 g/mL vancomycin
trough groups, respectively (data not shown).
The main limitation of this study is that it was a post hoc,
exploratory analysis; the ATTAIN studies were not de-
signed to evaluate the impact of vancomycin trough levels,
and as such, patients were not randomized to achieve a spe-
cific trough target. In addition, the sample size may be too
small to draw a definitive conclusion. However, the data
were obtained from rigorously monitored, registrational,
Phase 3 trials that likely capture critical information in a
more systematic fashion than retrospective studies.
Conclusion
In summary, the findings of our study suggest that
higher vancomycin trough levels do not result in im-
proved clinical response but likely increase the incidence
of nephrotoxicity. Prospective controlled studies are re-
quired to further assess the validity of the current vanco-
mycin dosing recommendations.
Additional files
Additional file 1: Institutional Review Boards/Ethics Committees by
Country-Study 0015.
Additional file 2: Institutional Review Boards/Ethics Committees by
Country-Study 0019.
Competing interests
SLB is an employee of, and holds stock/stock options for Theravance. FCG was
an employee of Theravance at the time of the study. MES has received
consulting fees/honoraria from Astellas, Cempra, Cerexa, Furiex, The Medicines
Company, Nabriva, PRA International, Theravance, and Trius; has received other
financial support (e.g., travel expenses, review activities, and manuscript
preparation reimbursement) from Astellas (travel only), Cempra, and Theravance;
Table 2 Clinical outcomes of ATTAIN study patients with Staphylococcus aureus nosocomial pneumonia according to
vancomycin trough levels
Vancomycin trough level (g/mL), n/N (%) p
*
< 10 10 to < 15 15
All patients
Clinical cure 21/30 (70) 18/33 (55) 17/35 (49) 0.09
MRSA 13/20 (65) 15/26 (58) 16/30 (53) 0.42
MRSA based on median trough levels collected up to study Day 4 14/26 (54) 11/20 (55) 8/16 (50) 0.83
Any serious adverse event 4/30 (13) 8/33 (24) 13/35 (37) 0.03
Renal adverse events
0/30 (0) 1/33 (3) 6/35 (17) <0.01
Significant increases in serum creatinine
0/30 (0) 0/33 (0) 4/35 (11) 0.02
Increase 2 to < 3 times from baseline 0/30 (0) 0/33 (0) 1/35 (3)
Increase 3 times from baseline 0/30 (0) 0/33 (0) 3/35 (9)
Deaths 3/30 (10) 5/33 (15) 7/35 (20) 0.31
Median length of therapy in days (interquartile range) 10 (6, 12) 11 (8, 14) 11 (8, 15) 0.14
Excluding patients with ARF or vancomycin exposure within 7 days
Clinical cure 12/17 (71) 9/15 (60) 3/11 (27) 0.04
Any serious adverse event 2/17 (12) 3/15 (20) 6/11 (55) 0.02
Renal adverse events
0/17 (0) 0/15 (0) 3/11 (27) 0.01
Significant increases in serum creatinine
0/17 (0) 0/15 (0) 2/11 (18) 0.06
Deaths 2/17 (12) 3/15 (20) 5/11 (45) 0.07
ATTAIN, Assessment of Telavancin for Treatment of Hospital-Acquired Pneumonia; ARF, acute renal failure; MRSA, methicillin-resistant Staphylococcus aureus.
*
Two-sided p-value for Cochran-Armitage test for trend; p-value based on exact test reported for sparse data (any cell < 5).
Renal failure, renal insufficiency, renal impairment, creatinine increased.
1.5 mg/dL and increase to at least 1.5 baseline.
Excluding patients with acute renal failure and/or vancomycin exposure within 7 days prior to the first dose of study medication.
Kruskall-Wallis.
Barriere et al. BMC Infectious Diseases 2014, 14:183 Page 4 of 5
http://www.biomedcentral.com/1471-2334/14/183
and has received grants/grants pending from Duke University (NIH) and
Theravance. GRC has served on advisory boards for Cempra, Cerexa, Inimex,
Pfizer, and Trius; is a consultant for Astellas, Cempra, Cerexa, Dr Reddys Lab,
Inimex, Merck, Pfizer, Polymedix, PRA International, Theravance, and Trius; has
received grants/grants pending from Cubist, Innocoll, The Medicines Company,
and Theravance; and has received other financial support (e.g., travel expenses,
manuscript preparation reimbursement) from Theravance. ER has served as a
consultant/on advisory boards for Astellas, Atox, Bayer, BiondVax, Merck, Ortho-
McNeil, Pfizer, Theravance, and Wyeth; has provided expert testimony for
Johnson & Johnson; has received grants/other research support from Astellas,
Bayer-Schering, Cubist, Daiichi, Merck, Pfizer, Theravance, and Wyeth; and has
received payment for lectures/speakers bureaus from Astellas, Bayer, Cubist, and
Pfizer.
Authors contributions
SLB was the ATTAIN study monitor, was involved in the study design and
data interpretation, and was the lead author of this manuscript. FCG was
involved in the statistical analysis, data interpretation, and development of
the manuscript. MES was an ATTAIN study investigator, and was involved in
data interpretation and development of the manuscript. GRC was an ATTAIN
study co-principal investigator, and was involved in the study design, data
interpretation, and development of the manuscript. ER was an ATTAIN study
co-principal investigator, and was involved in the study design, data interpret-
ation, and development of the manuscript. All authors reviewed and approved
the final version of the manuscript.
Author information
Fredric C. Genter was an employee of Theravance, Inc. at the time of the study.
Acknowledgments
The ATTAIN studies and publication development were supported by
Theravance, Inc. The authors would like to acknowledge Whedy Wang
(Theravance, Inc.) for statistical support and advice. Editorial and writing
support was provided by Emily Howard, a medical writer at Envision
Scientific Solutions, funded by Theravance.
Author details
1
Theravance, Inc., South San Francisco, CA 94080, USA.
2
Centro de Educacin
Mdica e Investigaciones Clinicas (CEMIC) Norberto Quirno, Buenos Aires,
Argentina.
3
Duke Clinical Research Institute and Department of Medicine,
Division of Infectious Diseases, Duke University Medical Center, Durham, NC
27710, USA.
4
Section of Infectious Diseases, Department of Internal Medicine
and Medical Microbiology, University of Manitoba, Winnipeg, Manitoba, Canada.
Received: 24 June 2013 Accepted: 31 March 2014
Published: 4 April 2014
References
1. DeRyke CA, Lodise TP Jr, Rybak MJ, McKinnon PS: Epidemiology, treatment,
and outcomes of nosocomial bacteremic Staphylococcus aureus
pneumonia. Chest 2005, 128(3):14141422.
2. American Thoracic Society; Infectious Diseases Society of America:
Guidelines for the management of adults with hospital-acquired,
ventilator-associated, and healthcare-associated pneumonia. Am J Respir
Crit Care Med 2005, 171(4):388416.
3. Rybak MJ, Lomaestro BM, Rotschafer JC, Moellering RC, Craig WA, Billeter M,
Dalovisio JR, Levine DP: Vancomycin therapeutic guidelines: a summary
of consensus recommendations from the Infectious Diseases Society of
America, the American Society of Health-System Pharmacists, and the
Society of Infectious Diseases Pharmacists. Clin Infect Dis 2009,
49(3):325327.
4. Jeffres MN, Isakow W, Doherty JA, McKinnon PS, Ritchie DJ, Micek ST,
Kollef MH: Predictors of mortality for methicillin-resistant Staphylococcus
aureus health-care-associated pneumonia: specific evaluation of
vancomycin pharmacokinetic indices. Chest 2006, 130(4):947955.
5. Hermsen ED, Hanson M, Sankaranarayanan J, Stoner JA, Florescu MC, Rupp ME:
Clinical outcomes and nephrotoxicity associated with vancomycin trough
concentrations during treatment of deep-seated infections. Expert Opin
Drug Saf 2010, 9(1):914.
6. Kunkel M, Chastre JE, Kollef MH, Niederman MS, Shorr AF, Wunderink RG,
McGee W, Olvey S, Reisman A, Baruch A: Linezolid vs vancomycin in the
treatment of nosocomial pneumonia proven due to methicillin-resistant
Staphylococcus aureus (abstract LB-49), Infectious Diseases Society of
America (IDSA) 48th Annual Meeting. Canada: Vancouver, BC; 2010.
7. Jeffres MN, Isakow W, Doherty JA, Micek ST, Kollef MH: A retrospective
analysis of possible renal toxicity associated with vancomycin in patients
with health care-associated methicillin-resistant Staphylococcus aureus
pneumonia. Clin Ther 2007, 29(6):11071115.
8. Lodise TP, Patel N, Lomaestro BM, Rodvold KA, Drusano GL: Relationship
between initial vancomycin concentration-time profile and nephrotoxicity
among hospitalized patients. Clin Infect Dis 2009, 49(4):507514.
9. Patel N, Pai MP, Rodvold KA, Lomaestro B, Drusano GL, Lodise TP:
Vancomycin: we can't get there from here. Clin Infect Dis 2011,
52(8):969974.
10. Rubinstein E, Lalani T, Corey GR, Kanafani ZA, Nannini EC, Rocha MG, Rahav G,
Niederman MS, Kollef MH, Shorr AF, Lee PC, Lentnek AL, Luna CM, Fagon JY,
Torres A, Kitt MM, Genter FC, Barriere SL, Friedland HD, Stryjewski ME; for the
ATTAIN Study Group: Telavancin versus vancomycin for hospital-acquired
pneumonia due to gram-positive pathogens. Clin Infect Dis 2011,
52(1):3140.
11. Wong-Beringer A, Joo J, Tse E, Beringer P: Vancomycin-associated
nephrotoxicity: a critical appraisal of risk with high-dose therapy. Int J
Antimicrob Agents 2011, 37(2):95101.
12. Bosso JA, Nappi J, Rudisill C, Wellein M, Bookstaver PB, Swindler J, Mauldin PD:
Relationship between vancomycin trough concentrations and nephrotoxicity:
a prospective multicenter trial. Antimicrob Agents Chemother 2011,
55(12):54755479.
13. Hidayat LK, Hsu DI, Quist R, Shriner KA, Wong-Beringer A: High-dose vanco-
mycin therapy for methicillin-resistant Staphylococcus aureus infections:
efficacy and toxicity. Arch Intern Med 2006, 166(19):21382144.
doi:10.1186/1471-2334-14-183
Cite this article as: Barriere et al.: Effect of vancomycin serum trough
levels on outcomes in patients with nosocomial pneumonia due to
Staphylococcus aureus: a retrospective, post hoc, subgroup analysis of
the Phase 3 ATTAIN studies. BMC Infectious Diseases 2014 14:183.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Barriere et al. BMC Infectious Diseases 2014, 14:183 Page 5 of 5
http://www.biomedcentral.com/1471-2334/14/183
You might also like
- Organizational Approaches To Improving Resuscitation EffectivenessDocument12 pagesOrganizational Approaches To Improving Resuscitation Effectivenessgiseladelarosa2006No ratings yet
- Uslam Bacterimeia Edad SexoDocument6 pagesUslam Bacterimeia Edad Sexogiseladelarosa2006No ratings yet
- Insulina SC UciDocument18 pagesInsulina SC Ucigiseladelarosa2006No ratings yet
- Jama Intern Med 2014 Aug 174 (8) 10 BenfitsDocument8 pagesJama Intern Med 2014 Aug 174 (8) 10 Benfitsgiseladelarosa2006No ratings yet
- Vasopresina Efectos AdversosDocument9 pagesVasopresina Efectos Adversosgiseladelarosa2006No ratings yet
- Cambios Resp Vena CavaDocument7 pagesCambios Resp Vena Cavagiseladelarosa2006No ratings yet
- HDFVVC EfectoDocument11 pagesHDFVVC Efectogiseladelarosa2006No ratings yet
- Visitas Policivas UciDocument4 pagesVisitas Policivas Ucigiseladelarosa2006No ratings yet
- Antioxidant EsDocument2 pagesAntioxidant Esgiseladelarosa2006No ratings yet
- Chest: Latent Class Analysis Identifi Es Distinct Phenotypes of Primary Graft Dysfunction After Lung TransplantationDocument7 pagesChest: Latent Class Analysis Identifi Es Distinct Phenotypes of Primary Graft Dysfunction After Lung Transplantationgiseladelarosa2006No ratings yet
- Clin Infect Dis. 2014 Lodise 666 75Document10 pagesClin Infect Dis. 2014 Lodise 666 75giseladelarosa2006No ratings yet
- Jama Intern Med 2014 Aug 174 (8) 2 MeaningDocument2 pagesJama Intern Med 2014 Aug 174 (8) 2 Meaninggiseladelarosa2006No ratings yet
- Jama Intern Med 2014 Aug 174 (8) 4 AntibioticDocument2 pagesJama Intern Med 2014 Aug 174 (8) 4 Antibioticgiseladelarosa2006No ratings yet
- JMN 140070Document2 pagesJMN 140070giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1106Document9 pagesIntensive Care Medicine 2014 40 (8) 1106giseladelarosa2006No ratings yet
- Jama Intern Med 2014 Aug 174 (8) 6 EvidenceDocument2 pagesJama Intern Med 2014 Aug 174 (8) 6 Evidencegiseladelarosa2006No ratings yet
- The Role of Copy-and-Paste in The Hospital Electronic Health RecordDocument2 pagesThe Role of Copy-and-Paste in The Hospital Electronic Health RecordHLMeditNo ratings yet
- Intensive Care Medicine 2014 40 (8) 1124Document8 pagesIntensive Care Medicine 2014 40 (8) 1124giseladelarosa2006No ratings yet
- Jama Intern Med 2014 Aug 174 (8) 2 MeaningDocument2 pagesJama Intern Med 2014 Aug 174 (8) 2 Meaninggiseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1151Document4 pagesIntensive Care Medicine 2014 40 (8) 1151giseladelarosa2006No ratings yet
- The Role of Copy-and-Paste in The Hospital Electronic Health RecordDocument2 pagesThe Role of Copy-and-Paste in The Hospital Electronic Health RecordHLMeditNo ratings yet
- Intensive Care Medicine 2014 40 (8) 1147Document4 pagesIntensive Care Medicine 2014 40 (8) 1147giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1115Document9 pagesIntensive Care Medicine 2014 40 (8) 1115giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1147Document4 pagesIntensive Care Medicine 2014 40 (8) 1147giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1106Document9 pagesIntensive Care Medicine 2014 40 (8) 1106giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1140Document4 pagesIntensive Care Medicine 2014 40 (8) 1140giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1097Document9 pagesIntensive Care Medicine 2014 40 (8) 1097giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1115Document9 pagesIntensive Care Medicine 2014 40 (8) 1115giseladelarosa2006No ratings yet
- Intensive Care Medicine 2014 40 (8) 1089Document8 pagesIntensive Care Medicine 2014 40 (8) 1089giseladelarosa2006No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Learning Stations Lesson PlanDocument3 pagesLearning Stations Lesson Planapi-310100553No ratings yet
- Individual Assignment ScribdDocument4 pagesIndividual Assignment ScribdDharna KachrooNo ratings yet
- SEO Design ExamplesDocument10 pagesSEO Design ExamplesAnonymous YDwBCtsNo ratings yet
- Numerical Methods: Jeffrey R. ChasnovDocument60 pagesNumerical Methods: Jeffrey R. Chasnov2120 sanika GaikwadNo ratings yet
- National Advisory Committee For AeronauticsDocument36 pagesNational Advisory Committee For AeronauticsSamuel ChristioNo ratings yet
- Unit 1 - Introduction To BankingDocument17 pagesUnit 1 - Introduction To Bankingc08No ratings yet
- sl2018 667 PDFDocument8 pagessl2018 667 PDFGaurav MaithilNo ratings yet
- ExpDocument425 pagesExpVinay KamatNo ratings yet
- Statement of Compulsory Winding Up As On 30 SEPTEMBER, 2008Document4 pagesStatement of Compulsory Winding Up As On 30 SEPTEMBER, 2008abchavhan20No ratings yet
- C Exam13Document4 pagesC Exam13gauravsoni1991No ratings yet
- Ijimekko To Nakimushi-Kun (The Bully and The Crybaby) MangaDocument1 pageIjimekko To Nakimushi-Kun (The Bully and The Crybaby) MangaNguyễn Thị Mai Khanh - MĐC - 11A22No ratings yet
- Singer NM37 57manualDocument266 pagesSinger NM37 57manualpaulkoby100% (2)
- 2016 Mustang WiringDocument9 pages2016 Mustang WiringRuben TeixeiraNo ratings yet
- DSE61xx Configuration Suite Software Manual PDFDocument60 pagesDSE61xx Configuration Suite Software Manual PDFluisNo ratings yet
- Conceptual FrameworkDocument24 pagesConceptual Frameworkmarons inigoNo ratings yet
- Report Daftar Penerima Kuota Telkomsel Dan Indosat 2021 FSEIDocument26 pagesReport Daftar Penerima Kuota Telkomsel Dan Indosat 2021 FSEIHafizh ZuhdaNo ratings yet
- NGPDU For BS SelectDocument14 pagesNGPDU For BS SelectMario RamosNo ratings yet
- Ground Water Resources of Chennai DistrictDocument29 pagesGround Water Resources of Chennai Districtgireesh NivethanNo ratings yet
- CL 5313 17021-1 Requirements Matrix-1458-5Document6 pagesCL 5313 17021-1 Requirements Matrix-1458-5Ana AnaNo ratings yet
- Inventarisasi Data Kondisi Jalan Ke Dalam Aplikasi Sistem Informasi Geografis (Sig)Document10 pagesInventarisasi Data Kondisi Jalan Ke Dalam Aplikasi Sistem Informasi Geografis (Sig)Wiro SablengNo ratings yet
- School Quality Improvement System PowerpointDocument95 pagesSchool Quality Improvement System PowerpointLong Beach PostNo ratings yet
- 5 Dec2021-AWS Command Line Interface - User GuideDocument215 pages5 Dec2021-AWS Command Line Interface - User GuideshikhaxohebkhanNo ratings yet
- 2019 May Chronicle AICFDocument27 pages2019 May Chronicle AICFRam KrishnaNo ratings yet
- Master of Commerce: 1 YearDocument8 pagesMaster of Commerce: 1 YearAston Rahul PintoNo ratings yet
- Planview Innovation Management Maturity Model PDFDocument1 pagePlanview Innovation Management Maturity Model PDFMiguel Alfonso Mercado GarcíaNo ratings yet
- Abinisio GDE HelpDocument221 pagesAbinisio GDE HelpvenkatesanmuraliNo ratings yet
- MSDS FluorouracilDocument3 pagesMSDS FluorouracilRita NascimentoNo ratings yet
- Active and Passive Voice of Future Continuous Tense - Passive Voice Tips-1Document5 pagesActive and Passive Voice of Future Continuous Tense - Passive Voice Tips-1Kamal deep singh SinghNo ratings yet
- CGV 18cs67 Lab ManualDocument45 pagesCGV 18cs67 Lab ManualNagamani DNo ratings yet
- WassiDocument12 pagesWassiwaseem0808No ratings yet