Professional Documents
Culture Documents
Jaundice Heart Failure
Uploaded by
Ganda Edhi0 ratings0% found this document useful (0 votes)
42 views3 pagesOn rare occasions the first manifestation of heart disease is jaundice. Caused by passive congestion of the liver or acute ischaemic hepatitis. 8 patients (1.2%) had a primary cardiac cause for their jaundice. All had dyspnoea, an increased cardiothoracic ratio on chest x-ray and an abnormal electrocardiogram.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentOn rare occasions the first manifestation of heart disease is jaundice. Caused by passive congestion of the liver or acute ischaemic hepatitis. 8 patients (1.2%) had a primary cardiac cause for their jaundice. All had dyspnoea, an increased cardiothoracic ratio on chest x-ray and an abnormal electrocardiogram.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
42 views3 pagesJaundice Heart Failure
Uploaded by
Ganda EdhiOn rare occasions the first manifestation of heart disease is jaundice. Caused by passive congestion of the liver or acute ischaemic hepatitis. 8 patients (1.2%) had a primary cardiac cause for their jaundice. All had dyspnoea, an increased cardiothoracic ratio on chest x-ray and an abnormal electrocardiogram.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
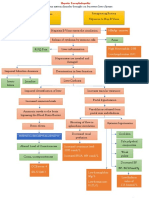
Jaundice as a presentation of heart failure
R van Lingen MRCP
2
U Warshow MRCP
1
H R Dalton DPhil FRCP
1
S H Hussaini MD FRCP
1
J R Soc Med 2005;98:357359
SUMMARY
On rare occasions the rst manifestation of heart disease is jaundice, caused by passive congestion of the liver or
acute ischaemic hepatitis. We looked for this presentation retrospectively in 661 patients referred over fty-six
months to a jaundice hotline (rapid access) service. The protocol included a full clinical history, examination and
abdominal ultrasound. Those with no evidence of biliary obstruction had a non-invasive liver screen for
parenchymal liver disease and those with suspected heart disease had an electrocardiogram, chest X-ray and
echocardiogram.
8 patients (1.2%), bilirubin 3179 m mmol/L, mean 46 m mmol/L, had a primary cardiac cause for their jaundice. All had
dyspnoea, an increased cardiothoracic ratio on chest X-ray and an abnormal electrocardiogram. The jugular venous
pressure was raised in the 3 in whom it was recorded. In 6 patients the jaundice was attributed to hepatic
congestion and in 2 to ischaemic hepatitis. All patients had severe cardiac dysfunction.
Jaundice due to heart disease tends to be mild, and a key feature is breathlessness. The most common
mechanism is hepatic venous congestion; ischaemic hepatitis is suggested by a high aminotransferase.
INTRODUCTION
Jaundice is an uncommon presentation of cardiac disease.
13
The two major causes are chronic congestion due to heart
failure and ischaemic hepatitis from acute circulatory
impairment. We conducted a retrospective review of
patients seen at a jaundice hotline service to determine the
proportion of such cases and their clinical characteristics.
METHODS
The Royal Cornwall Hospital is a district general hospital
serving a population of about 400 000. A hotline service
was started in November 1998 to facilitate rapid diagnosis
and treatment of patients with jaundice in the community,
and the initial results have been reported.
4
All patients had a
full history taken for alcohol use, medications and risk
factors for viral hepatitis. An abdominal ultrasound was
performed to identify biliary obstruction. In patients
without biliary obstruction, blood was tested for evidence
of virus infections (hepatitis A, B and C, EpsteinBarr,
cytomegalovirus), for autoantibodies and for alpha-1-
antitrypsin concentration, together with iron and copper
studies. In patients without evidence of biliary obstruction
or parenchymal liver disease, cardiac evaluation included an
electrocardiogram (ECG), an echocardiogram and a chest
X-ray.
RESULTS
Of 661 patients seen by the jaundice hotline service in fty-
six months 8 (1.2%) had a primary cardiac disorder. All
reported dyspnoea. Details are in Table 1. Their jaundice
was mild (bilirubin 3179 mmol/L, mean 46 mmol/L) and
only 2 had an alkaline phosphatase above normal. 2 patients
with severe cardiac failure and an alanine aminotransferase
exceeding 1000 iu/L were judged to have ischaemic
hepatitis. Both had a raised troponin, so the probable cause
of their cardiac decompensation was myocardial infarction
within the last 10 days; their liver function tests became
normal with treatment of their heart disease. All patients
had abnormal electrocardiograms, and echocardiograms
showed severe global or left ventricular impairment,
valvular abnormalities and in one case a left atrial myxoma.
The clinical assessment of jugular venous pressure was
recorded in only 3 of the 8 patients.
DISCUSSION
Among patients presenting via the hotline, heart disease was
a rare cause for jaundice. Moreover, the jaundice was always
mild. In all 8, the history of dyspnoea together with cardiac
enlargement on X-ray and ECG abnormalities pointed to the
underlying disorder. The jugular venous pressure, a bedside
assessment with diagnostic, therapeutic and prognostic
value,
4
was not well recorded in this series.
P
R
A
C
T
I
C
E
357
J O U R N A L O F T H E R O Y A L S O C I E T Y O F M E D I C I N E V o l u m e 9 8 A u g u s t 2 0 0 5
1
Cornwall Gastrointestinal Unit, Royal Cornwall Hospital Trust, Truro TR1 3LJ;
2
Department of Cardiology, Derriford Hospital, Plymouth PL6 8DH, UK
Correspondence to: Dr Hyder Hussaini
E-mail: hyder.hussaini@rcht.cornwall.nhs.uk
In 6 of the 8 patients the jaundice was probably due to
the passive liver congestion of low-output cardiac failure.
Other groups have described a raised alkaline phosphatase in
these circumstances
57
but this was seen in only 2 of the 6.
The phenomenon has been linked to the severity of
tricuspid regurgitation.
8,9
Suggested mechanisms for the
jaundice of low-output heart failure are decreased hepatic
blood ow, increased hepatic venous pressure and
decreased arterial oxygen saturation. In addition, work in
animals raises the possibility of endotoxin mediated
damage.
10
In the 2 patients with ischaemic hepatitis the probable
cause was myocardial infarction in the setting of severe
valvular disease. Such patients tend to have a massive rise in
aminotransferases with associated derangement in pro-
thrombin time.
11
Ischaemic hepatitis, which results from
hepatic circulatory failure, predominantly affects the
perivenular zone of the hepatic acinus.
2
Hepatic blood ow
declines by about 10% for every 10 mmHg drop in arterial
pressure.
12
Rapid resolution of the hypotension usually
leads to full recovery of the hepatitis.
12,13
It is noteworthy
that healthy individuals with acute hypotension from events
such as trauma do not seem to develop ischaemic hepatitis.
A retrospective analysis of patients with ischaemic hepatitis
indicated that all had underlying heart disease, predomi-
nantly right-sided.
14
Thus a baseline of hepatic congestion
may be required as a primer before the development of
ischaemic hepatitis.
We conclude that the combination of jaundice and
breathlessness should prompt a careful cardiological
examination, including assessment of the jugular venous
pressure, electrocardiogram, chest radiograph and echo-
cardiogram to exclude a cardiac cause. Ischaemic hepatitis is
suggested by a high alanine aminotransferase.
358
J O U R N A L O F T H E R O Y A L S O C I E T Y O F M E D I C I N E V o l u m e 9 8 A u g u s t 2 0 0 5
Table 1 Clinical details
Patient
(age)
Dyspnoea
duration JVP
Bilirubin
mmol/L
(ref. range
823)
ALT IU/L
(1044)
Alk phos
IU/L
(45122) Liver U/S ECG CXR Echo
M (54) 5 months : 33 41 99 Enlarged;
engorged
hepatic
veins
AF; partial
RBBB
Bilateral
pleural
effusions.
:C-th ratio
Left atrial
myxoma;
dilated RV
M (69) 1 month NR 51 50 82 Normal AF; LBBB Bilateral
pleural
effusions.
:C-th ratio
Dilated LV,
EF 15%
M (79) 1 month : 56 38 57 Dilated IVC
and hepatic
veins
LBBB :C-th ratio Dilated LV,
EF 18%
M (61) 3 months NR 33 25 111 Mild
parenchymal
irregularity
AF; LBBB :C-th ratio;
bibasal
shadowing
Dilated LV,
EF520%
M (72) 42 years
(known
cardiomyopathy)
NR 31 11 272 Normal AF; LBBB :C-th ratio Dilated LV,
EF 23%
F (69) 2 weeks NR 79 1213 887 Normal LBBB :C-th ratio Severe LV
i mpairment;
severe AS
M (80) 34 weeks NR 32 1085 141 Dilated hepatic
veins
AF;
partial
LBBB
:C-th ratio Severe MR;
normal LV
M (75) 1 month : 55 41 68 Incidental
single
gallstone
1st degree
heart
block;
LBBB
:C-th ratio Severe MR;
moderate
AS; mild LV
i mpairment
JVP=jugular venous pressure; ALT=alanine aminotransferase; alk phos=alkaline phosphatase; U/S=ultrasound; ECG=electrocardiogram; CXR=chest X-ray; IVC=inferior vena
cava; R/L BBB=right/left bundle branch block; AF=atrial brillation; c-th ratio=cardiothoracic ratio; RV, LV=right, left ventricle; EF=ejection fraction; AS=aortic stenosis;
MR=mitral regurgitation; NR=not recorded
REFERENCES
1 Giallourakis CC, Rosenberg PM, Friedman LS. The liver in heart
failure. Clin Liver Dis 2002;6:94767, viiiix
2 Neuberger J. The liver in systemic disease. In: Warrell DA, Cox TM,
Firth JD, Benz E, eds. Oxford Textbook of Medicine, 4th edn. Oxford:
Oxford University Press, 1993
3 Lowe MD, Harcombe AA, Grace AA, Petch MC. Restrictive
constrictive heart failure masquerading as liver disease. BMJ
1999;318:5856
4 Mitchell J, Hussaini H, McGovern D, Farrow R, Maskell G, Dalton H.
The jaundice hotline for the rapid assessment of patients with jaundice.
BMJ 2002;325:21315
5 Morrissey M, Durkin M, Gunnar R. The cardiovascular system. In:
Haubrich W, Schaffner F, Berk JE, eds. Bockus Gastroenterology, 5th edn.
Philadelphia: WB Saunders, 1995:3392403
6 Braunwald E. Heart failure. In: Braunwald E, Fauci A, Kasper D,
Hauser S, Longo DL, Jameson JL, eds. Harrisons Principles of Internal
Medicine, 15th edn. New York: McGraw-Hill, 2001:131829
7 Kumar P, Clarke M. Clinical Medicine, 3rd edn. London: Baillie`re
Tindall, 1994
8 Finlayson ND, Bouchier IA. Diseases of the liver and biliary system. In:
Edwards CR, Bouchier IA, Haslett C, Chilvers ER, eds. Davidsons
Principles and Practice of Medicine, 17th edn. Edinburgh: Churchill
Livingstone, 1995:5523
9 Lau GT, Tan HC, Kritharides L. Type of liver dysfunction in heart
failure in relation to the severity of tricuspid regurgitation. Am J Cardiol
2002;123:136784
10 Cogger VC, Fraser R, Le Couteur DG. Liver dysfunction and heart
failure. Am J Cardiol 2003;91:1399
11 Givertz MM, Colucci WS, Braunwald E. Clinical aspects of heart
failure: high-output failure, pulmonary edema. In: Braunwald E, Zipes
P, Libby P, eds. Heart Disease: a Textbook of Cardiovascular Medicine, 6th
edn. Philadelphia: WB Saunders, 2001
12 Dillon JF, Finlayson NDC. The liver in systemic disease. In: Shearman
DJC, Finlayson NDC, Camilleri M, Carter D, eds. Diseases of the
Gastrointestinal Tract and Liver. Edinburgh: Churchill Livingstone, 1997
13 Ellenberg M, Osserman KE. The role of shock in the production of
central liver cell necrosis. Am J Med 1951;11:1708
14 Seeto RK, Fenn B, Rockey DC. Ischemic hepatitis: clinical
presentation and pathogenesis. Am J Med 2000;109:10913
359
J O U R N A L O F T H E R O Y A L S O C I E T Y O F M E D I C I N E V o l u m e 9 8 A u g u s t 2 0 0 5
You might also like
- Research Kolengioma SarkiomastosisDocument7 pagesResearch Kolengioma SarkiomastosisGanda EdhiNo ratings yet
- Research Myoma Uteri New EraDocument12 pagesResearch Myoma Uteri New EraGanda EdhiNo ratings yet
- Measuring Carboxyhemoglobin (HbCO) LevelsDocument21 pagesMeasuring Carboxyhemoglobin (HbCO) LevelsGanda EdhiNo ratings yet
- Gender Differences in Cardiovascular Response To Isometric Exercise in The Seated and Supine PositionsDocument7 pagesGender Differences in Cardiovascular Response To Isometric Exercise in The Seated and Supine PositionsGanda EdhiNo ratings yet
- KPBI 02 Lab - Man.ug (Reviisi01)Document14 pagesKPBI 02 Lab - Man.ug (Reviisi01)Ganda EdhiNo ratings yet
- HTTP SofaDocument1 pageHTTP SofaGanda EdhiNo ratings yet
- Senin, 10 Maret 2008 CDK PengelolaanpenderitadengankeluhanDocument1 pageSenin, 10 Maret 2008 CDK PengelolaanpenderitadengankeluhanGanda EdhiNo ratings yet
- ATS Statement on Dyspnea Mechanisms, Assessment and ManagementDocument20 pagesATS Statement on Dyspnea Mechanisms, Assessment and ManagementTrismegisteNo ratings yet
- Referensi Sabtu080308Document1 pageReferensi Sabtu080308Ganda EdhiNo ratings yet
- ReferensiDocument1 pageReferensiGanda EdhiNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaGanda EdhiNo ratings yet
- Lab Activity PharmacoDocument3 pagesLab Activity PharmacoGanda EdhiNo ratings yet
- Daftar Kelompok 2007 Sem 5Document15 pagesDaftar Kelompok 2007 Sem 5Ganda EdhiNo ratings yet
- KLP Diskusi Blok BHL I Angk 2007Document7 pagesKLP Diskusi Blok BHL I Angk 2007Ganda EdhiNo ratings yet
- Absens IDocument4 pagesAbsens IGanda EdhiNo ratings yet
- Anafilaksisi Masa DepanDocument15 pagesAnafilaksisi Masa DepanGanda EdhiNo ratings yet
- Kelompok PraktikumDocument2 pagesKelompok PraktikumGanda EdhiNo ratings yet
- Jadwal BHL 1 - 2008Document1 pageJadwal BHL 1 - 2008Ganda EdhiNo ratings yet
- Note Taking & Power Reading 2010Document25 pagesNote Taking & Power Reading 2010Ganda EdhiNo ratings yet
- Promotion Best Star Cardiology FixDocument2 pagesPromotion Best Star Cardiology FixGanda EdhiNo ratings yet
- SGD 3 - 21 GramsDocument3 pagesSGD 3 - 21 GramsGanda EdhiNo ratings yet
- Bagaimana BerefleksiDocument6 pagesBagaimana BerefleksiGanda EdhiNo ratings yet
- Health, Stress, and CopingDocument17 pagesHealth, Stress, and CopingGanda EdhiNo ratings yet
- Pharmaco ToxicologyDocument49 pagesPharmaco ToxicologyGanda EdhiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Biochemistry of Liver: Alice SkoumalováDocument37 pagesBiochemistry of Liver: Alice Skoumalováandreas kevinNo ratings yet
- Pediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsDocument2 pagesPediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsBobet Reña100% (2)
- Treatment: Wilson DiseaseDocument4 pagesTreatment: Wilson Diseaseali tidaNo ratings yet
- SANDRA, Apollo OBG Minor Disorders in Neonates PPT - SECTION BDocument15 pagesSANDRA, Apollo OBG Minor Disorders in Neonates PPT - SECTION Bsandra0% (1)
- Cholestasis: DR I Gede Palgunadi Sppd-Finasim Fk-Unram/Rsup NTBDocument17 pagesCholestasis: DR I Gede Palgunadi Sppd-Finasim Fk-Unram/Rsup NTBMuzayyanatulhayat ARNo ratings yet
- Infectious Diseases EmqDocument24 pagesInfectious Diseases Emqfrabzi100% (1)
- Assessment of The Integumentary SystemDocument21 pagesAssessment of The Integumentary SystemSheila Mae Panis100% (1)
- Rosh ReviewDocument125 pagesRosh ReviewPrince Du100% (2)
- Newborn Assessment 2.16Document16 pagesNewborn Assessment 2.16rrbischofbergerNo ratings yet
- A Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaDocument34 pagesA Case On Periampullary Carcinoma.: Presented by DR Sumaiya Tasnim TanimaJobaer MahmudNo ratings yet
- Krok BukDocument242 pagesKrok BukLucja0% (1)
- A Case Report On Biliary AtresiaDocument2 pagesA Case Report On Biliary AtresiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Diagnostic Report: FinalDocument10 pagesDiagnostic Report: FinalKushagra SahniNo ratings yet
- Kamara - Factors Associated With Neonatal Hyperbilirubinemia in The First 2weeks of Life in OlaDocument56 pagesKamara - Factors Associated With Neonatal Hyperbilirubinemia in The First 2weeks of Life in OlaJulia StantonNo ratings yet
- Anesthesia and The Hepatobiliary SystemDocument35 pagesAnesthesia and The Hepatobiliary SystemscribdNo ratings yet
- Icterus Neonatorum: (Neonatal Hyperbilirubinemia)Document30 pagesIcterus Neonatorum: (Neonatal Hyperbilirubinemia)Dian Vera WNo ratings yet
- Pedia ReviewerDocument27 pagesPedia ReviewerEvangeline GoNo ratings yet
- Case Study: Obstructive JaundiceDocument11 pagesCase Study: Obstructive JaundiceZhy CaluzaNo ratings yet
- Group B and A streptococcus differentiationDocument75 pagesGroup B and A streptococcus differentiationDjdjjd SiisusNo ratings yet
- Sella Modul TropisDocument34 pagesSella Modul TropissellasellaNo ratings yet
- IJRPR5933Document8 pagesIJRPR5933rifa iNo ratings yet
- Digestive System: Yousef Ali Sazan Falah Snor Dilan KawtharDocument21 pagesDigestive System: Yousef Ali Sazan Falah Snor Dilan Kawtharkauther hassanNo ratings yet
- PEDIA 20Idiot20Notes 1Document76 pagesPEDIA 20Idiot20Notes 1Aljon S. TemploNo ratings yet
- PD 17 To 21Document148 pagesPD 17 To 21Loai Mohammed IssaNo ratings yet
- Hepatic Enceph PathophysioDocument1 pageHepatic Enceph PathophysioJessica FabroaNo ratings yet
- Biochemistry 1Document32 pagesBiochemistry 1zaydeeeeNo ratings yet
- AST Practical Handout For 2nd Year MBBSDocument4 pagesAST Practical Handout For 2nd Year MBBSIMDCBiochemNo ratings yet
- Dis LiverDocument40 pagesDis LiverPrem MorhanNo ratings yet
- Neonatal Jaundice Bilirubin Physiology and ClinicaDocument13 pagesNeonatal Jaundice Bilirubin Physiology and ClinicaNURUL NADIA BINTI MOHD NAZIR / UPMNo ratings yet
- Study of Haematological Parameters in Malaria: Original Research ArticleDocument6 pagesStudy of Haematological Parameters in Malaria: Original Research ArticleV RakeshreddyNo ratings yet