Professional Documents
Culture Documents
Open Fractures and Timing To Closure
Uploaded by
Jati Nugroho0 ratings0% found this document useful (0 votes)
53 views4 pagesoke
Original Title
Open Fractures and Timing to Closure
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentoke
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
53 views4 pagesOpen Fractures and Timing To Closure
Uploaded by
Jati Nugrohooke
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
VOLUME 20, MAY 2010 19
Open Fractures and Timing to Closure:
A Review
T. Ty Fowler, MD
1
Benjamin C. Taylor, MD
1
Brian R. Williams
2
1
Department of Orthopaedic Surgery,
Mount Carmel Medical Center,
Columbus, OH
2
University of Toledo,
College of Medicine, Toledo, OH
Controversy exists between primary and delayed closure of open fracture wounds and complication rates. Traditional
teaching has been to close open fractures in a delayed fashion. However, many investigators have shown low
infection rates with primary closure of open fractures. Much of the literature available indicates primary closure can
be performed on Gustilo and Anderson type I and II open fractures and even type IIIA with specic inclusion and
exclusion criteria. Primary closure is contraindicated when wound debridement is inadequate, wound edges cannot be
approximated without tension, or the wound remains contaminated. Timing of the closure of an open fracture wound
can have implications on patient care, ranging from morbidity and mortality to economic considerations. We present a
review of the published literature concerning the timing of closure of open fracture wounds.
Infection is a common sequela of open
fracture injuries. In 1976, Gustilo and Anderson
1
(GA) classied open fracture injuries into three
categories: type I, II, or III. A type I fracture is
categorized as a wound that is less than one
cm long and clean. Type II injuries are classied
as a fracture with a laceration more than one
cm, without extensive soft-tissue damage, aps,
or avulsions. Type III injuries were originally
categorized as either an open segmental fracture,
an open fracture with extensive soft-tissue
damage, or a traumatic amputation. Special
categories in type III were gunshot injuries,
any open fracture caused by a farm injury, and
any open fracture with accompanying vascular
injury requiring repair. Type III injuries were
further modied in 1984 by Gustilo et al
2
to
include three subtypes. Type IIIA is described
as adequate soft-tissue coverage of a fractured
bone despite extensive soft-tissue laceration or
aps, or high-energy trauma irrespective of the
size of the wound. Type IIIB refers to inadequate
soft-tissue coverage with periosteal stripping
requiring ap reconstruction, often associated
with massive contamination. Type IIIC describes
any open fracture associated with arterial injury
that requires vascular repair for limb salvage.
Delayed closure of open fractures, dened as
wound closure occurring at any time after the
initial debridement, was established as standard
of care prior to the advent of current antibiotics,
modern debridement methods, and improved
fracture stabilization procedures
3
. In 1939,
Trueta discussed the advantages and necessity of
thorough debridement of war injuries to reduce
infection
3
. However, in 1943, the use of penicillin
resulted in further reduction of infection;
therefore, the importance of performing a
thorough debridement was no longer emphasized.
The resulting recommendations were delayed
closure, noting a lower infection rate when
compared with primary closure complicated
by inadequate debridements
3
. As stated by
Hohmann et al
4
, the standard of treating open
wound fractures has become a combination of
urgent aggressive debridement with excision of
all dead and devitalized tissue, early stabilization
of the fracture, and initiation of broad-spectrum
antibiotics. Subsequently, the wound is debrided
every 48 to 72 hours, with closure of the wound
after nal adequate debridement
3-5
. It has been
shown that the optimal timing of wound closure
or coverage is within seven days of injury, as
delays greater than seven days are associated with
higher infection rates
3-5
.
According to the literature, the most important
aspect of surgical open fracture treatment
is thorough debridement and irrigation
1-20
.
Multiple reports have shown that infections
of open wounds likely are not caused by the
initial contamination, but instead by organisms
acquired secondarily through nosocomial
routes
1-4
. In accordance, Patzakis et al
17
reported
only 18% of infections related to open fractures
are due to the initial organism. This has led to
many authors suggesting that primary wound
closure is safe and may actually reduce the rate
of infection
3,4,7,9,17,19
. The present article reviews
the controversy concerning the standard of
care for open fracture closure and addresses the
following two questions: Is there evidence in the
literature to support primary closure at the time
of initial debridement of open fractures? What
are the contraindications to performing primary
closure of open fractures?
Review and Discussion of the Pertinent
Literature
Many authors consider a tension free closure
in an open fracture wound a pre-requisite for
primary closure
4,7,8,18-20
. As a result of signicant
edema and damage to the soft-tissue envelope
after high-energy trauma, increased tension in the
skin aps is a concern when attempting primary
closure. This increased tension theoretically
has a negative effect on the cutaneous blood
ow leading to necrosis of the skin edges and
Corresponding Author:
T. Ty Fowler, MD
793 West State Street
Columbus,Ohio 43222
ty_fowler@hotmail.com
20 FOWLER ET AL
UNIVERSITY OF PENNSYLVANIA ORTHOPAEDIC JOURNAL
eventual wound breakdown. In a pig model, Sagi et al
21
found
that the Allgower-Donati suture-pattern had a signicantly
smaller effect on cutaneous blood ow with increasing
tension when compared to a simple, vertical mattress, and
horizontal mattress suture pattern.
In 1976, Gustilo and Anderson
1
completed a retrospective
and prospective study of 1025 open long bone fractures
before the current sub-classication of type III injuries. Their
study demonstrated a decrease from a 20% infection rate to
6% in type I and II injuries with primary closure at initial
debridement. In a subanalysis of type III injuries, sixteen of
the injuries were closed primarily leading to a 44% infection
rate, whereas ve underwent delayed closure with a resulting
infection rate of 20%. The authors concluded that type I and II
injuries should be closed primarily, whereas type III fracture
closure should be delayed
1
. It is necessary to reiterate the
importance of debridement when treating open fractures, as
quoted in their landmark article: If there is the slightest doubt
in the surgeons mind as to whether there has been adequate
debridement of the wound after open fracturethe safe rule
is not to close the wound
1
.
A comprehensive literature review article prepared by
Crowley et al
19
reviewed studies addressing primary and delayed
closures of open fractures. The investigators recommended
primary closure of open GA type I, II, and IIIA fractures, with
the exception of wounds that are grossly contaminated with
feces or stagnant water, or fractures resulting from farmyard-
related injuries. However, type IIIB and IIIC injuries were
recommended to be managed by specialized teams and the
wounds should be closed at the earliest possible time
19
.
A randomized, prospective study of eighty-two open
fractures of the lower and upper extremities was completed
by Benson and colleagues
18
that yielded no signicant
differences in infection rates between primary and delayed
closure. The groups were comparable statistically with respect
to time from injury to debridement, immediate internal
xation, subjective classication of gross contamination, and
associated injuries. Forty-four injuries were closed primarily,
three (6.8%) of which resulted in supercial infection. The
other thirty-eight cases were left open for an average of four to
six days before closure of the wound, resulting in two (5.2%)
deep infections. Hohmann et al
4
had similar results in their
retrospective study of the timing of open tibia fracture closure
with deep infection being the end point. They included GA
type I, II, and IIIA open fractures, and therefore excluded
type IIIB and IIIC injuries, polytraumas, associated injuries,
unrelated signicant comorbidities, presentation greater than
twenty-four hours post-injury, or surgeries within the previous
six months. The authors reported no statistically signicant
difference in infection rates between forty-nine patients who
were treated with primary closure at initial debridement with
a 2 % infection rate, and forty-six patients treated with delayed
closure who had an infection rate of 4.3%. However, the
authors found almost twice the length of stay for patients who
underwent delayed closure, and they concluded that primary
closure is potentially more cost-effective in appropriately
selected patients
4
.
Furthermore, DeLong and colleagues
7
retrospectively
studied 119 open fracture injuries and closures. These
consisted of fractures involving the tibia (52), femur (27),
radius and ulna (12), ankle (11), patella (9), and humerus
(4). Seventy-six of the injuries were closed primarily and
seventeen of the closures were delayed. Three of the primary
closure cases resulted in infection and two of the delayed
closures resulted in infection. The investigators concluded that
there were no statistically signicant differences in infection,
delayed union, or nonunion between procedures. Inherent in
retrospective studies, this study was not without limitations.
These authors noted that the wounds in the delayed closure
group were unable to be closed without tension on the skin
edges, which is an accepted indication for delayed closure.
Arguably these two groups are not equivalent and, therefore,
should not be compared with respect to infection rate. To
decrease variation between groups, the authors performed
a subanalysis within the three types of open fracture grades
and found no signicant differences between the two closure
methods. Similar to Hohmann et als conclusion
4
, DeLong et
al
7
stated that primary closures provide a lower number of
operations, and decreased health care costs and hospital stays
with no increase in infection.
Gleuck et al
20
retrospectively examined forty-two open
fractures of the distal radius and closure methods. Three of the
twenty-seven cases that underwent primary closure resulted
in infections. Investigators analyzed the correlations between
infection and the following: Gustilo and Anderson type I-III
open fracture, time from injury to irrigation and debridement,
primary versus delayed closures, method of stabilization,
and degrees of contamination. The degree of contamination
was the only variable found to be statistically signicant
in its correlation to infection. The investigators suggested
that primary closure is safe in relatively clean wounds.
However, there is no evidence to support primary closure of
contaminated wounds regardless of classication type
20
.
Rajasekaran and colleagues
9
prospectively studied upper and
lower extremity open fractures to determine safe criteria for
primary closure of GA type III injuries. They excluded type I, II,
and IIIC fractures immediately, as well as patients suffering from
shock, peripheral vascular disease, drug-dependent diabetes
mellitus, peripheral vasculitis, connective-tissue disorders, or
wound contamination by sewage or farm substances. Specic
inclusion criteria were reported as wound debridement within
twelve hours of injury, no skin loss, stable skeletal xation, and
bleeding skin margins closed by direct apposition under no
tension. The authors ndings showed that only ve of the 173
(2.9%) wounds had deep infections. Therefore, they concluded
that primary closure in open fractures is appropriate in properly
selected patients
9
. It is worthy to note that strict criteria for
primary closure, as stated above, led to only 185 fractures of
557 (33%) type III open fractures that were able to be primarily
closed at the initial debridement.
A prospective study was completed by Shtarker et al
6
of
thirty-two open tibia fractures, including eleven type I, ten type
II and eleven type IIIA open fractures, with primary closure.
Two of the closures resulted in skin necrosis leading to skin
TIMING OF CLOSURE FOR OPEN FRACTURES 21
VOLUME 20, MAY 2010
grafts; however, there were no infections. Similar to Gustilo and
Anderson
1
, Shtarker et al
6
recommended primary closure if the
surgeon is condent that the wounds are free of contamination.
Weitz-Marshall and Bosse
3
performed a literature review
of the timing of wound closures. They concluded that it was
the surgeons judgment gained by experience that is required
for primary closure protocol along with an adequate amount
of debridement. Furthermore, contraindications for primary
closure included grossly contaminated wounds with feces,
stagnant water, dirt, or injuries occurring in the farm setting.
Moreover, primary closure was not suggested if the antibiotic
treatment was delayed for more than twelve hours, if a
questionable amount of viable tissue at initial surgery remains,
or if there was a concern regarding adequacy of debridement
3
.
Reuss and Cole
8
retrospectively reviewed eighty-one open
tibial shaft fractures. Thirty-two patients underwent delayed
closure and the remaining forty-nine wounds were closed
primarily at the time of initial debridement. Delayed closures
resulted in 19% infection rate, whereas only 2% of the primary
closures became infected. All the infections were GA type III
injuries, one type IIIA (primary closure group), and six type
IIIB (delayed closure group). However, the groups in their
study are not equivalent, as the more severe injuries required
more debridements and were closed on a delayed basis. There
was a statistically signicant association between multiple
debridements and infection, and a higher fracture grade. The
authors stated that primary closure is acceptable based on the
surgeons discretion regarding the adequacy of debridement
and low contamination of the wound.
Lavelle et al
14
performed a web-based survey to determine
the methods of treatment for open fractures by ACGME
accredited residency programs. They found that the vast
majority of programs were primarily closing GA type I (88%)
and type II (86%) open fractures. Type IIIA open fractures
however, were only primarily closed by 57% of programs.
Other investigators who have studied the current topic
disagree with the recommendation of primary closures of
appropriately selected wounds. In an instructional course
lecture article Zalavras and colleagues
12
reviewed the
treatment of open fractures and concluded that the duration
of antibiotic therapy, the time between injury and surgery,
or the type of wound closure are not signicant variables
in outcomes. The authors stated that, in their review of the
literature, infection rates are equal between primary and
delayed closure; however, they warn that there is an increased
risk of Clostridia perfringens contamination causing gas
gangrene with primary closure despite providing no evidence
to support this claim
12
. In stark contrast to their own literature
review and the previously mentioned studies, they recommend
that open wounds should not be closed primarily due to the
risk of gas gangrene and that no rationale exists for primary
closure, since delayed closure is a time-tested standard of
care
12
. However, there may be some bias due to the selective
reporting of the sources the investigators reviewed, as well as
their personal preference for treating open fractures.
Russell et al
5
retrospectively reviewed ninety cases of extra-
articular open tibia fractures from 1981 through 1986. Despite
the difference in groups (primary closure group had twice as
many GA type III open fractures), results showed that primary
closures resulted in a 50% infection rate versus a 33% infection
rate for delayed closure. If type III fractures were removed
and only type I and II fractures were analyzed, there was no
statistically signicant difference in the infection rate between
primary and delayed procedures. Despite their results with
respect to type I and II fractures, they concluded that there is
no place for primary closure of any open tibia fracture
5
.
Conclusion
This article reviews the controversy concerning the
standard of care for timing of closure of open fractures and
addresses the following two questions: Is there evidence in
the literature to support primary closure at the time of initial
debridement of open fractures? What are the contraindications
to performing primary closure of open fractures?
It is the authors opinion and that of our institution that
primary closure is an acceptable procedure for treatment of
appropriately selected open fractures. It is strongly agreed in
the literature that adequate debridement is the most important
factor in minimizing infection while treating open fractures
1-20
.
Given the available evidence in the literature, which lacks an
abundance of Level I studies, very low infection rates with
primary closure of type I and II open fractures can be obtained
when ensuring adequate debridement
1-4,6-9, 13, 16,18-20
. Moreover,
Rajasekaran and colleagues
9
, as well as Shtarker et al
6
have
shown acceptable low infection rates of type IIIA fractures
treated with primary closure. Crowley et als systemic review
19
also advocated primary closure in type IIIA open fractures when
gross contamination is absent. Rajasekaran et al
9
controlled for
very specic parameters whereby primary closure of open
fracture wounds was acceptable: debridement within twelve
hours of injury, appropriate stabilization of the fracture, and
closure of skin margins by direct apposition with no tension
on wound edges. The authors advocate the use of Rajasekarans
criteria and further emphasize thorough wound debridement
and the use of the Allgower-Donati suture for closure.
Based on the literature reviewed and the authors opinion,
contraindications for primary closure include inadequate
debridement. If a surgeon is unable to approximate wound
edges without tension to the wound, then closure should be
delayed. Furthermore, if the wound is heavily contaminated
with drug-resistant anaerobic or gram negative bacteria
including those found in feces, stagnant water, or farm setting,
primary closure should be avoided.
It should be emphasized that the studies reviewed, many of
which were retrospective, also are plagued by low numbers
and inadequate power. There is a strong need for well-designed
prospective Level I studies to further support, potentially
modify, or refute the above recommendations.
Acknowledgement
The authors acknowledge the editorial assistance of Janet
L. Tremaine, ELS, Tremaine Medical Communications, Dublin,
Ohio.
22 FOWLER ET AL
UNIVERSITY OF PENNSYLVANIA ORTHOPAEDIC JOURNAL
11. Olson SA, Schemitsch EH. Open fractures of the tibial shaft: an update. Instr Course Lect
2003;52:623-631.
12. Zalavras CG, Marcus RE, Levin LS, Patzakis MJ. Management of open fractures and
subsequent complications. Instr Course Lect. 2008;57:51-63.
13. Gardner MJ, Mehta S, Barei DP, Nork SE. Treatment protocol for open AO/OTA type C3
pilon fractures with segmental bone loss. J Orthop Trauma 2008;22(7):451-457.
14. Lavelle WF, Uhl R, Krieves M, Drvaric DM. Management of open fractures in adult
patients: current teaching in ACGME accredited residency programs. J Surg Orthop Adv
2007;16(3):111-117.
15. Al-Arabi YB, Nader M, Hamidian-Jahromi AR, Woods DA. The effect of the timing
of antibiotics and surgical treatment on infection rates in open long-bone fractures: a 9-year
prospective study from a district general hospital. Injury 2007;38(8):900-905
16. Levin LS. Early versus delayed closure of open fractures. Injury 2007;38:896-899.
17. Patzakis MJ, Bains Rs, Lee J, Shepherd L, Singer G, Ressler R, Harvey F, Holtom
P. Prospective, randomized, double-blind study comparing single-agent antibiotic therapy,
ciprooxacin, to combination antibiotic therapy in open fracture wounds. J Orthop Trauma 2000;
14:529-533.
18. Benson DR, Riggins RS, Lawrence RM, Hoeprich PD, Huston AC, Harrison JA.
Treatment of open fractures: a prospective study. J Trauma 1983;23:25-30.
19. Crowley DJ, Kanakaris NK, Giannoudis PV. Debridement and wound closure of open
fractures: the impact of the time factor on infection rates. Injury 2007;38:879-889.
20. Glueck DA, Charoglu CP, Lawton JN. Factors associated with infection following open
distal radius fractures. Hand 2009;4:330-334.
21. Sagi HC, Papp S, Dipasquale T. The effect of suture pattern and tension on cutaneous blood
ow as assessed by laser Doppler owmetry in a pig model. J Orthop Trauma 2008 Mar;22(3):171-175.
References
1. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-
ve open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am
1976;58-A:453-458.
2. Gustilo RB, Mendoza RM, Williams DN. Problems in the management of Type III (severe)
open fractures. J Trauma 1984;24:742-746.
3. Weitz-Marshall AD, Bosse MJ. Timing of closure of open fractures. J Am Assoc Orthop Surg
2002;10:379-384.
4. Hohmann E, Tetsworth K, Radziejowski MJ, Wiesniewski TF. Comparison of delayed and
primary wound closure in the treatment of open tibial fractures. Arch Orthop Trauma Surg 2007;
127:131-136.
5. Russell GG, Henderson R, Arnett G. Primary or delayed closure for open tibial fractures. J
Bone Joint Surg Br 1990;72-B:125-128.
6. Shtarker H, David R, Stolero J, Grimberg B, Soudry M. Treatment of open tibial fractures
with primary suture and Ilizarov xation. Clin Orthop Relat Res 1997;335:268-274.
7. DeLong WG Jr, Born CT, Wei SY, Petrik ME, Ponzio R, Schwab CW. Aggressive treatment
of 119 open fracture wounds. J Trauma 1999;46:1049-1054.
8. Reuss BL, Cole JD. Effect of delayed treatment on open tibial shaft fractures. Am J Orthop
2007;36:215-220.
9. Rajasekaran S, Dheenadhayalan J, Babu JN, Sundararajan SR, Venkatramani H,
Sabapathy SR. Immediate primary skin closure in type-iii A and B open fractures: results after a
minimum of ve years. J Bone Joint Surg Br 2009;91-B:217-224.
10. Charalambous CP, Siddique I, Zenios M, Roberts S, Samarji R, Paul A, Hirst P. Early
versus delayed surgical treatment of open tibial fractures: effect on the rates of infection and need
of secondary surgical procedures to promote bone union. Injury 2005;36:656-661.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
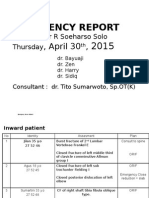
- ER Report: 4 Patients with Orthopedic InjuriesDocument49 pagesER Report: 4 Patients with Orthopedic InjuriesJati NugrohoNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- CorelDRAW X4 Key SerialasdasdDocument1 pageCorelDRAW X4 Key SerialasdasdJati NugrohoNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Git PDFDocument8 pagesGit PDFJati NugrohoNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Maping Onko 25 Juni 2013 FixDocument2 pagesMaping Onko 25 Juni 2013 FixJati NugrohoNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- CorelDRAW X4 Key SerialasdasdDocument1 pageCorelDRAW X4 Key SerialasdasdJati NugrohoNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 20 JuniDocument2 pages20 JuniJati NugrohoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- What Is OsteosarcomaDocument3 pagesWhat Is OsteosarcomadhinahafizNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Clavicle FracturesDocument35 pagesClavicle FracturesJati Nugroho0% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- VCA 341 Lecture 6 FracturesDocument7 pagesVCA 341 Lecture 6 FracturesJati NugrohoNo ratings yet
- Covering Letter-CMM PDFDocument3 pagesCovering Letter-CMM PDFJati NugrohoNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Clinical Mental Health Counseling in Community and Agency Settings 5Th Edition Full ChapterDocument41 pagesClinical Mental Health Counseling in Community and Agency Settings 5Th Edition Full Chapterwilliam.kellar832100% (24)
- What Is Link AdaptationDocument4 pagesWhat Is Link AdaptationAshutosh SinghNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- SSC 146G Summer 2016 Human Sexuality SyllabusDocument1 pageSSC 146G Summer 2016 Human Sexuality SyllabusJames SmithNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- أبعاد التنمية الإجتماعية العربية في ضوء التجربة الأردنيةDocument36 pagesأبعاد التنمية الإجتماعية العربية في ضوء التجربة الأردنيةkadhim4981No ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Semaphore Twinsoft Manual PDFDocument101 pagesSemaphore Twinsoft Manual PDFReza AnantoNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Thank You LetterDocument2 pagesThank You LetterFathina57% (7)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- scn625 Summativeeval SarahltDocument6 pagesscn625 Summativeeval Sarahltapi-644817377No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Fundamentals of Human Neuropsychology 7th Edition Kolb Test BankDocument26 pagesFundamentals of Human Neuropsychology 7th Edition Kolb Test BankDanielYoungabrn100% (60)
- Sugar Cane White FlyDocument13 pagesSugar Cane White Flyvishnu0751No ratings yet
- Chronology of TLM Event in The PhilippinesDocument3 pagesChronology of TLM Event in The PhilippinesTheus LineusNo ratings yet
- Aprils Detox GuideDocument20 pagesAprils Detox GuideKwasi BempongNo ratings yet
- BSD Magazine MaioDocument101 pagesBSD Magazine MaioBruno AlvimNo ratings yet
- King Rama VDocument3 pagesKing Rama Vsamuel.soo.en.how2324No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- KNAW Proceedings from 1919-1920Document481 pagesKNAW Proceedings from 1919-1920Eduardo Salgado EnríquezNo ratings yet
- Urology Case Reports: Shakhawan Hama Amin Said, Rezhin Yaseen Abdalla, Ismaeel Aghaways, Ari Mohammed AbdullahDocument3 pagesUrology Case Reports: Shakhawan Hama Amin Said, Rezhin Yaseen Abdalla, Ismaeel Aghaways, Ari Mohammed AbdullahHardiTariqHammaNo ratings yet
- Ebook Torrance (Dalam Stanberg) - 1-200 PDFDocument200 pagesEbook Torrance (Dalam Stanberg) - 1-200 PDFNisrina NurfajriantiNo ratings yet
- CSEC English B June 2013 P2Document7 pagesCSEC English B June 2013 P2Jhanett RobinsonNo ratings yet
- Chapter04 PDFDocument36 pagesChapter04 PDFBabuM ACC FIN ECONo ratings yet
- Application for Test Engineer PositionDocument3 pagesApplication for Test Engineer PositionAsz WaNieNo ratings yet
- Chapter 8 SQL Complex QueriesDocument51 pagesChapter 8 SQL Complex QueriesJiawei TanNo ratings yet
- Case - 1 Marketing and Distribution of MushroomDocument2 pagesCase - 1 Marketing and Distribution of MushroomKetan BohraNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Phonology BibliogrDocument6 pagesPhonology BibliogrSnapeSnapeNo ratings yet
- Demand Letter Jan 16Document8 pagesDemand Letter Jan 16jhean0215No ratings yet
- CSE Qualifications and PointersDocument9 pagesCSE Qualifications and PointersChristopher de LeonNo ratings yet
- Biology-A Complete Solution For - V. Educational ServicesDocument2,088 pagesBiology-A Complete Solution For - V. Educational Servicesteamindian gamersNo ratings yet
- Chisholm - Referring To Things That No Longer ExistDocument13 pagesChisholm - Referring To Things That No Longer ExistMichele Paolini PaolettiNo ratings yet
- Perceptiual - Cognitive SkillDocument17 pagesPerceptiual - Cognitive SkillGeovani AkbarNo ratings yet
- Treasures Book 1 Unit 1Document33 pagesTreasures Book 1 Unit 1Janinne AbuegNo ratings yet
- Project 4: Creative Illustration: Theme: Nouns and AdjectivesDocument2 pagesProject 4: Creative Illustration: Theme: Nouns and Adjectivesapi-278922030No ratings yet
- Highly Effective College StudentsDocument8 pagesHighly Effective College StudentsPhoenix Kylix0% (1)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)