Professional Documents
Culture Documents
Hypertension
Uploaded by
WanAzrenCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertension
Uploaded by
WanAzrenCopyright:
Available Formats
Introduction
If an individuals resting blood pressure is persistently high, it not only
puts a strain on the heart but also damages the walls of the arteries,
making them stiffer and more prone to clogging and haemorrhage. This
causes problems in the organs they supply and leads to potentially fatal
conditions and debilitating disorders, such as coronary heart disease
and stroke.
Hypertension, defined as a persistent raised blood pressure of
140/90mmHg,
1,2,3
is one of the most common disorders in the UK.
*
Although it rarely causes symptoms on its own, the damage it does to
the arteries and organs can lead to considerable suffering and
burdensome healthcare costs. Hypertension is arguably the most
important modifiable risk factor for coronary heart disease (the leading
cause of premature death in the UK) and stroke (the third leading
cause). It is also an important cause of congestive heart failure (heart
strain) and chronic kidney disease. This has earned hypertension a
reputation as the silent killer, making it a key priority for prevention,
detection and control, and one of the most important challenges facing
public health today.
Despite isolated examples of good practice, a truly joined-up approach
to tackling hypertension is lacking, particularly around prevention,
early detection and clinical protocols for control. It is therefore critical
that primary care staff and local multi-agency teams work together to
establish programmes which not only identify and treat people with
hypertension but actively promote healthy lifestyles and implement
preventive strategies in order to meet the challenge of tackling
hypertension
Footnote: Blood pressure is expressed as two numbers eg. 140/90mmHg 140 is the
systolic pressure (highest pressure during each pulse) and 90 is the diastolic pressure
(lowest pressure). It is measured in millimetres of mercury (mmHg).
*Thresholds for hypertension in people with Type 1 and Type 2 diabetes are slightly lower.
Hypertension the Silent Killer
Bri ef i ng St at ement
H
y
p
e
r
t
e
n
s
i
o
n
t
h
e
S
i
l
e
n
t
K
i
l
l
e
r
H
y
p
e
r
t
e
n
s
i
o
n
t
h
e
S
i
l
e
n
t
K
i
l
l
e
r
2
Hypert ensi on t he Si l ent Ki l l er
Faculty of Public Health Briefing Statement
Evidence
The associated risks of hypertension increase
gradually in parallel with rising blood pressure. A
large-scale international study has shown that
significantly increased risks of cardiovascular
disease begin to appear at a level as low as
115/75mmHg
5
far lower than the current average
adult blood pressure (eg. England average:
131/74mmHg for men and 126/73mmHg for
women).
6
The threshold of 140/90mmHg (as a diagnosis of
hypertension) has been designated to indicate when
a particular course of action should be instituted,
such as intervening medically.
1,2,3
Effects of hypertension on health
Hypertension is usually symptomless and often not
regarded as a disease in its own right. However, it is
a major risk factor in a number of potentially fatal
conditions and debilitating disorders:
Coronary heart disease
Stroke
Heart failure
Chronic kidney disease
Aortic aneurysm
Retinal disease
Peripheral vascular disease
Prevalence of hypertension
In England, 32% of men and 30% of women, aged
16 years or over, have hypertension.
6
The equivalent
figures for Scotland are 33% of men and 28% of
women.
20
There are no exactly comparable figures
for Wales or Northern Ireland. However, 15% of
adults in Wales reported being treated for high blood
pressure.
7
In Northern Ireland, 19% of men and
27% of women reported having been diagnosed with
high blood pressure.
8
Risk factors for hypertension
Although hypertension is itself a risk factor for a
number of conditions, (see above) there are also
risk factors both unmodifiable and modifiable
which predispose certain people to developing
hypertension.
Unmodifiable risk factors
Age and gender
The association between increasing age and
increasing systolic blood pressure is thought to
reflect the length of time people are exposed to
modifiable risk factors. For any given age up to 65
years women tend to have a lower blood pressure
than men. After 65 years, this trend is reversed.
6
The cause is unknown. Prevalence also increases
with age.
Ethnicity
Hypertension is more prevalent in different ethnic
groups, such as black Caribbean men and women,
and less prevalent in Bangladeshi men and women,
for example.
9
Some of the differences in prevalence
are thought to be related to inherited differences in
the way the body reacts to salt
10
and in blood
pressure controlling hormones.
Main risk factors for
developing hypertension*
Unmodifiable Modifiable
Age and gender Excess salt
Ethnicity Overweight and obesity
Physical inactivity
Excess alcohol
Diabetes
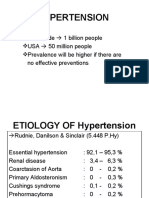
Five main types of hypertension
4
Essential (or primary): accounts for 95% of cases of hypertension in the UK. No specific underlying cause
but thought to result from a genetic predisposition in addition to the cumulative
effects of various lifestyle factors eg. salt intake, physical inactivity.
Secondary: accounts for up to 5% of cases. Caused by an underlying disease, most commonly
chronic kidney disease, or as a side-effect of medication.
Malignant (or accelerated): a very high or rapidly rising blood pressure which threatens end-organ damage and
requires urgent or emergency treatment. About 1% of those with essential
hypertension develop malignant hypertension.
Gestational: occurs during pregnancy and usually returns to normal following childbirth.
White-coat: occurs when a persons blood pressure is high when they see a doctor or nurse, but
is normal at other times.
* This is not an exhaustive list of risk factors. For a full list see
Easing the Pressure: Tackling Hypertension
4
3
Hypert ensi on t he Si l ent Ki l l er
Faculty of Public Health Briefing Statement
Modifiable risk factors
Excess salt
Evidence has shown a strong association between
salt intake and elevated blood pressure.
11
In the UK,
65-70% of the salt we eat comes from processed
foods such as bread, cereals, ready meals etc.
11
Average adult daily intake is 9g of salt per day
three times the amount actually needed.
12
The daily
recommended level is 6g for adults representing
what is actually achievable across the population, not
what is optimal. For children, different thresholds
have been set according to age.
11
Overweight and obesity
Obesity multiplies the risk of developing
hypertension about fourfold in men and threefold in
women.
13
It is well documented that levels of
overweight and obesity have increased over the last
decade. In the UK, about two-thirds of men and over
half of women are either overweight (BMI of 25-
29.9kg/m
2
) or obese (BMI of 30kg/m
2
).
4
Physical inactivity
People who do not take enough aerobic exercise (eg.
running, walking and cycling) are more likely to
have or to develop hypertension. Large cross-
sectional and longitudinal studies have shown a
direct positive correlation between habitual aerobic
physical inactivity and hypertension.
14
59% of men
and 72% of women in Scotland,
15
and 70% of men
and 74% of women in Northern Ireland do not meet
physical activity guidelines.
8
In Wales, 14% of adults
do not exercise,
16
and in England, only 37% of men
and 24% of women meet recommended levels.
6
Excess alcohol
Blood pressure rises when large amounts of alcohol
are consumed, particularly when binge-drinking.
Heavy alcohol use is a well-established risk factor for
hypertension and stroke. A large study of almost
6,000 men, aged 35-64 years, followed-up for 21
years, found that there was a strong correlation
between alcohol consumption and mortality from
stroke.
17
Diabetes
Hypertension is more prevalent in people with Type
1 and Type 2 diabetes than in the non-diabetic
population (whether they are overweight or not), as
a consequence of kidney damage and insulin
resistance respectively. In England, as many as 70%
of adults with Type 2 diabetes have hypertension,
doubling the risk of a cardiovascular event.
4
Costs
In addition to the suffering caused to patients,
carers and their families, as a consequence of
hypertension, there is also a considerable cost
burden to the NHS, social care and the wider
economy. It is extremely difficult to calculate the
proportion attributable to hypertension. However,
with regard to the main consequences coronary
heart disease and stroke it has been calculated
that total costs are equivalent to about 7.06bn for
coronary heart disease, and 5.77bn for stroke.
16
Prevention
There is an increasing body of evidence to support
various lifestyle changes to prevent hypertension.
There are two approaches to preventing
hypertension:
Whole population
The aim is to prevent hypertension by lowering
average blood pressure by relatively small amounts
across a whole population. It has been estimated
that a reduction as small as 2mmHg in average adult
systolic blood pressure could save more than 14,000
UK lives per year.
18
This can be achieved by
encouraging enough people to change their lifestyles
sufficiently to reduce their blood pressure.
Main lifestyle changes include:
Reduce salt intake (to an average of 6g/day for
adults)
11
Increase fruit and vegetable intake
Increase habitual physical activity to
recommended levels
Keep alcohol intake within recommended
benchmark limits
Control weight
At-risk individuals or groups
This approach focuses on those known to be at
higher risk of developing hypertension. The risk
factors described above, and further explained in
Easing the Pressure: Tackling Hypertension,
4
can be
used to identify target individuals and groups. For
example, focus could be on those who are
overweight or obese, or those from particular ethnic
communities who have an increased risk of
hypertension (see Ethnicity p.2).
4
Hypert ensi on t he Si l ent Ki l l er
Faculty of Public Health Briefing Statement
Detection and control
Detection
The task of identifying those adults with existing
hypertension is a daunting one and in a general
practice setting it makes sense to priorities those
patients at high overall risk of cardiovascular
disease, or who show signs or symptoms of target-
organ damage that may be due to, or exacerbated
by, hypertension. There are three main ways of
identifying patients with hypertension known as
case-finding:
Opportunistic case-finding in various settings
often undertaken during a consultation on
another health matter, or in settings such as
health fairs, workplaces etc.
Systematic screening programmes usually
based on a proactive call-recall programme.
Targeted case-finding in general practice
focuses on patients most likely to have
hypertension or complications from it.
Well-maintained disease registers are necessary
for successful implementation.
Control
Evidence shows that lowering blood pressure in
people with hypertension is associated with a
reduction in cardiovascular disease risk. A
large-scale meta-analysis of observation prospective
studies among hypertensive patients aged 40-69
years showed that a 20mmHg lower systolic blood
pressure is associated with:
5
less than half the risk of dying from a stroke, and
half the risk of dying from coronary heart
disease.
It is important that clinical decisions about
whether and how to treat hypertensive patients
are based on both their blood pressure level and
overall cardiovascular risk not on blood
pressure alone. Please refer to appropriate clinical
guidelines. The key guidelines that provide clinical
protocols for instituting therapies, including drug
therapy, to control hypertension are produced by the
British Hypertension Society, NICE and Scottish
Intercollegiate Guideline Network.
1,2,3
As a consequence of poor detection and diagnosis,
many people with hypertension go untreated or
receive inadequate treatment the proportion of
those untreated tends to be higher in older people
and manual socioeconomic groups.
4
The National
Service Frameworks (NSFs) and GMS contract
provide incentives to address this.
Adherence and concordance
Of those who are diagnosed, only 10% are
controlled to the target of 140/90mmHg.
19
This is
due to poor practitioner understanding of treatment
regimens, and to patients not taking medication as
prescribed known as poor adherence. Poor
adherence to prescribed medications is the most
important cause of uncontrolled blood pressure.
Reasons for this include forgetfulness, difficulty in
reading written instructions or in opening medicine
bottles.
Concordance means shared decision-making and
agreeing a plan of treatment that best represents
the intentions of both the patient and clinician. It is
an important step in motivating patients to take
their medicines as prescribed. Agreements should
be supported with written information, a care plan
and patient-held record. This issue is explored by
the Medicines Partnership Organisation (see Useful
Organisations p.6).
Policy Context
There are numerous policy drivers at both national
and local level which are relevant to hypertension.
Easing the Pressure: Tackling Hypertension gives
details of relevant policies and strategies.
4
However,
key drivers include:
England: The NSFs for Coronary Heart Disease,
Older People, Diabetes and Renal Services all have
standards relevant to the prevention, detection and
control of hypertension.
The public health white paper, Choosing Health,
builds on the NSFs. It introduces a number of new
initiatives including tough targets for salt reduction
in processed foods, nutrient-based standards for
public sector catering and specialist anti-obesity
services in primary care trusts.
The Department of Health Public Service Agreement
sets objectives to substantially reduce mortality
rates from the major killer diseases as well as
improve health outcomes for people with long-term
conditions. It also aims to halt the year-on-year rise
in obesity among children. The Priorities and
Planning Framework 2003-2006 also requires
practice-based registers to be updated to ensure
patients with CHD and diabetes receive appropriate
advice. National Standards, Local Action: Health and
Social Care Standards and Planning Framework
2005/06-2007/08 sets national targets and
standards for NHS and social services authorities.
Scotland: Improving Health in Scotland: the
Challenge Framework for Action sets targets for
improving the life expectancy and health-life
expectancy of all adults.
The Coronary Heart Disease and Stroke Strategy
for Scotland recommends that all NHS boards
should develop explicit CHD and stroke prevention
strategies to target groups classed as high risk
including those with hypertension.
The white paper, Towards a Healthier Scotland, sets
targets for CHD, stroke, physical activity, diet and
alcohol, to improve those life circumstances that
impact on health.
Wales: The white paper, Improving Health in
Wales: A Plan for the NHS with its Partners sets the
direction for health services in Wales, including
increasing the power of local health groups to
deliver strong community-based health and social
care services.
To reduce deaths from CHD, Tackling Coronary
Heart Disease in Wales: Implementing through
Evidence requires everyone at high risk of
developing, or who have been diagnosed with, CHD
to have access to a multifactorial risk assessment
and appropriate treatment.
Northern Ireland: The Investing for Health strategy
aims to improve the health and well-being of people
in Northern Ireland including reducing the mortality
rate from circulatory diseases, in particular heart
disease and stroke.
The Northern Ireland Evidence-based Stroke Strategy
provides a challenging agenda for the development of
stroke services over the next 5-10 years.
International: The World Health Report 2002:
Reducing Risks, Promoting Healthy Life describes
the burden of disease, disability and death that can
be attributed to a small number of health risks,
including blood pressure.
Recommendations
The prevention, detection and control of
hypertension are essential to national strategies
concerned with CHD, stroke, diabetes, chronic
kidney disease and the health of older people. The
following recommendations can help local multi-
agency teams implement strategies to tackle
hypertension at local level:
Establish a local hypertension action team, with
key partners including health services, local
authorities and voluntary organisations for
example, to develop a local hypertension
strategy. Easing the Pressure: Tackling
Hypertension gives comprehensive guidance on
how to go about this.
4
Undertake a service review or audit of local
services to identify current activity, gaps,
priorities and possible opportunities for service
development.
Review and agree local clinical guidelines and
protocols on the detection, treatment and
management of hypertension. The review
should consider national guidance as well as
reflect local circumstance. Ensure guidelines
have local ownership, including primary and
secondary care.
Develop comprehensive local programmes to
promote healthy eating and physical activity.
Support local primary care practitioners
through regular practice visits to advise on
developing at-risk registers, call-recall rotas,
prescribing, IT systems, staffing issues, and
additional resources.
Produce patient information to explain the risks
of hypertension and give advice on the various
interventions and treatments to prevent and
reduce blood pressure.
Hold local events and meetings to raise
awareness of hypertension, such as local health
fairs, awareness days. Encourage people to
know their number (ie. their blood pressure
level). These events could be targeted at
specific groups and give relevant lifestyle
advice.
Set local standards for public sector catering
services such as schools, NHS, to include
recommendations on salt levels.
5
Hypert ensi on t he Si l ent Ki l l er
Faculty of Public Health Briefing Statement
The Faculty of Public Health has produced, in association
with the National Heart Forum, Easing the Pressure:
Tackling Hypertension a toolkit for developing a local
strategy to tackle high blood pressure.
4
Supported by the
key organisations involved in tackling hypertension, the
toolkit provides local health improvement teams with the
essential building blocks to develop an effective
programme for the prevention and control of hypertension.
An online resource has also been developed and includes
a ready-reckoner to help calculate local prevalence, and
checklists to help identify gaps and monitor progress (see:
www.fph.org.uk/Publications). Easing the Pressure
forms part of a wider campaign of work aimed at promoting
healthier lifestyles to reduce disease burden through the
production of toolkits on the wider determinants of health
including physical activity, obesity, food poverty and fuel
poverty. The Faculty also advocates on salt reduction as
part of its salt strategy.
References
1 Williams B, Poulter NR, Brown MJ et al.
2004. Guidelines for management of
hypertension: report of the fourth
working party of the British
Hypertension Society, 2004-BHS IV.
Journal of Human Hypertension; 18:139-
85
2 National Institute for Clinical Excellence
(NICE). 2004. Hypertension:
Management of Hypertension in Adults
in Primary Care. Clinical Guideline
No.18. London: NICE
3 Scottish Intercollegiate Guidelines
Network (SIGN). 2001. Hypertension in
Older People. A National Clinical
Guideline. SIGN Publication No.49.
Edinburgh: SIGN
4 Maryon-Davis A, Press V on behalf of the
Faculty of Public Health and National
Heart Forum. 2005. Easing the Pressure:
Tackling Hypertension. A toolkit for
developing a local strategy to tackle
high blood pressure. London: Faculty of
Public Health
5 Prospective Studies Collaboration. 2002.
Age-specific relevance of usual blood
pressure to vascular mortality: a meta-
analysis of individual data for one
million adults in 61 prospective studies.
Lancet; 360: 1903-12
6 Joint Health Surveys Unit. 2004. Health
Survey for England 2003. Volume 2. Risk
factors for cardiovascular disease.
London: The Stationery Office
7 National Assembly for Wales. Welsh health
Survey 1998. Results of the Second
Welsh Health Survey. 1999. Newport:
Government Statistical Service
8 Northern Ireland Statistics and Research
Agency (NISRA). 2002. Northern Ireland
Health and Social Wellbeing Survey
2001. Belfast: NISRA
9 Joint Health Surveys Unit. 2000. Health
Survey for England. The Health of
Ethnic Minority Groups 99. London: The
Stationery Office
10Stewart JA, Dundas R, Howard RS et al.
1999. Ethnic differences in incidence of
stroke: prospective study with stroke
register. British Medical Journal; 300:
967-72
11Scientific Advisory Committee on
Nutrition. 2003. Salt and Health. London:
Department of Health
12Henderson L, Gregory J, Swan G. 2002.
National Diet and Nutrition Survey:
Adults Aged 19-64. Volume 1. London:
The Stationery Office
13National Audit Office. 2001. Tackling
Obesity in England. London: The
Stationery office
14Paffenbarger RS Jr, Jung DL, Leung RW,
Hyde RT. 1991. Physical activity and
hypertension: an epidemiological view.
Annals of Medicine; 23: 319-27
15Physical Activity Task Fore. 2003. Lets
Make Scotland More Active. A Strategy
for Physical Activity. Edinburgh: Scottish
Executive
16Liu JLY, Maniadakis N, Gray A, Rayner M.
2002. The economic burden of coronary
heart disease in the UK. Heart; 88: 597-
603
17Hart CL, Smith D, Hole DJ, Hawthorne M.
1999. Alcohol consumption and
mortality from all causes, CHD and
stroke: results from a prospective
cohort study of Scottish men with 21
years of follow up. BMJ; 318: 1725-29
18Critchley J, Capewell S. 2003. Substantial
potential for reductions in CHD
mortality in the UK through changes in
risk factor levels. Journal of
Epidemiology and Community Health; 57:
243-47
19Brown MJ, Cruickshank JK, Dominiczak AF.
2003. Better blood pressure control:
how to combine drugs. Journal of Human
Hypertension; 3: 53-9
20Joint Health Surveys Unit on behalf of the
Scottish Executive. 2000. The Scottish
Health Survey 1998. London: The
Stationery Office.
Publications
Easing the Pressure: Tackling
Hypertension (2005)
Online resource
www.fph.org.uk
Choosing Health: Making Healthy Choices
Easier (2004)
National Service Frameworks for Coronary
Heart Disease (2000), Diabetes (2001),
Older People (2001), Renal Services (2005)
National Standards, Local Action: Health
and Social Care Standards and Planning
Framework 2005/06-2007-08 (2004)
Public Service Agreement (2002)
Priorities and Planning Framework
2003-06 (2002)
Department of Health
www.dh.gov.uk
Coronary Heart Disease and Stroke
Strategy for Scotland (2002)
Improving Health in Scotland: the
Challenge Framework for Action (2003)
Towards a Healthier Scotland (1999)
Scottish Executive
www.scotland.gov.uk
Improving Health in Wales: A Plan for the
NHS with its Partners (2001)
National Assembly for Wales
www.wales.gov.uk
Tackling Coronary Heart Disease in Wales:
Implementing through Evidence (2001)
National Health Service for Wales
www.wales.nhs.uk
Investing for Health (2002)
Department of Health, Social Services and
Public Safety
www.dhsspsni.gov.uk
Northern Ireland Evidence-based Stroke
Strategy (2001)
Northern Ireland Chest, Heart and Stroke
Association
www.nichsa.com
6
Hypert ensi on t he Si l ent Ki l l er
Faculty of Public Health Briefing Statement
World Health Report 2002: Reducing
Risks, Promoting Healthy Life
World Health Organization
www.who.int/en
Useful Organisations
Blood Pressure Association
www.bpassoc.org.uk
British Heart Foundation
Heart Information Line: 08450 70 80 70
www.bhf.org.uk
British Hypertension Society
www.hyp.ac.uk
Consensus Action on Salt and Health
www.actiononsalt.org.uk
Diabetes UK
Helpline: 020 7424 1030
www.diabetes.org.uk
Food Standards Agency
www.food.gov.uk
Medicines Partnership Taskforce
www.medicine-partnership.org
National Heart Forum
www.heartforum.org.uk
National Institute of Health and Clinical
Excellence
www.nice.org.uk
National Kidney Federation
Helpline: 0845 601 0209
www.kidney.org.uk
Stroke Association
Helpline: 0845 30 33 100
www.stroke.org.uk
Acknowledgments
Authors:
Dr Alan Maryon-Davis FFPH FRCP
Convener, Cardiovascular Health Working
Group, Faculty of Public Health
Lindsey Stewart (and Series Editor)
Faculty of Public Health
Produced by:
Faculty of Public Health
4 St Andrews Place
London NW1 4LB
t: 020 7935 3115
e: healthpolicy@fph.org.uk
w: www.fph.org.uk
Registered charity no: 263894
ISBN: 1-900273-19-5
Published May 2005. The information provided in
this statement is correct at time of going to press.
Design and print: www.fosterandlisle.co.uk
Summary
This briefing gives an overview of the burden of
hypertension including the implications for
health and the cost to individuals, society and
the NHS. It also makes important
recommendations for action that can be
implemented at local level. It is not intended as
an exhaustive resource but as a signpost to the
key evidence, publications and organisations as
a next step to understanding and tackling this
important public health issue.
You might also like
- TransplantationDocument11 pagesTransplantationmardsz100% (1)
- Colorectal CancerDocument23 pagesColorectal Cancerralph_gail100% (1)
- Ischaemic Heart Disease Mku 2020Document38 pagesIschaemic Heart Disease Mku 2020ElvisNo ratings yet
- Acute Kidney InjuryDocument37 pagesAcute Kidney InjuryLani BuenaventuraNo ratings yet
- Left-Sided Congestive Heart Failure Case PresentationDocument64 pagesLeft-Sided Congestive Heart Failure Case PresentationNicole Villanueva, BSN - Level 3ANo ratings yet
- Addisonian Crisis: Manish K Medical Officer IgmhDocument47 pagesAddisonian Crisis: Manish K Medical Officer IgmhNaaz Delhiwale100% (1)
- PancreatitisDocument59 pagesPancreatitisAarif RanaNo ratings yet
- Implementing NICE guidance for hypertension case scenariosDocument51 pagesImplementing NICE guidance for hypertension case scenariosrwev3No ratings yet
- What Are Electrolytes? What Causes Electrolyte Imbalance?: Fast Facts On ElectrolytesDocument11 pagesWhat Are Electrolytes? What Causes Electrolyte Imbalance?: Fast Facts On ElectrolytesL InfiniteNo ratings yet
- Anal FistulaDocument26 pagesAnal FistulaBeverly PagcaliwaganNo ratings yet
- Seminar: Pere Ginès, Aleksander Krag, Juan G Abraldes, Elsa Solà, Núria Fabrellas, Patrick S KamathDocument18 pagesSeminar: Pere Ginès, Aleksander Krag, Juan G Abraldes, Elsa Solà, Núria Fabrellas, Patrick S KamathcastillojessNo ratings yet
- Effects of a Sedentary LifestyleDocument9 pagesEffects of a Sedentary LifestylethomasNo ratings yet
- Disorders of The EyeDocument16 pagesDisorders of The Eyelisette_sakuraNo ratings yet
- Hyperosmolar Hyperglycemic State (HHS)Document21 pagesHyperosmolar Hyperglycemic State (HHS)Malueth AnguiNo ratings yet
- PANCREATITISDocument38 pagesPANCREATITISVEDHIKAVIJAYANNo ratings yet
- HypertensionDocument20 pagesHypertensiondocbayNo ratings yet
- Congestive Heart FailureDocument74 pagesCongestive Heart FailureNiharikaNo ratings yet
- NCP Incarcerated Inguinal HerniaDocument3 pagesNCP Incarcerated Inguinal HerniaAHm'd MetwallyNo ratings yet
- Diabetes NotesDocument10 pagesDiabetes Notestripj33No ratings yet
- Myasthenia Gravis: An Autoimmune Neurologic DisorderDocument16 pagesMyasthenia Gravis: An Autoimmune Neurologic DisorderHibba NasserNo ratings yet
- Pulmonary EmbolismDocument80 pagesPulmonary EmbolismVarun B Renukappa100% (1)
- Identify CVD Risk in the Office with Framingham & Non-Fasting TestsDocument28 pagesIdentify CVD Risk in the Office with Framingham & Non-Fasting TestsJuwanto Wakimin100% (1)
- SCI (Spinal Cord Injury)Document51 pagesSCI (Spinal Cord Injury)Awal AlfitriNo ratings yet
- Cardiac Enzyme StudiesDocument4 pagesCardiac Enzyme StudiesDara VinsonNo ratings yet
- Myocardial Infarction. BPTDocument62 pagesMyocardial Infarction. BPTAanchal GuptaNo ratings yet
- Acute Pancreatitis: J Koh & D ChengDocument7 pagesAcute Pancreatitis: J Koh & D ChengGloriaaaNo ratings yet
- SepsisDocument33 pagesSepsisv_vijayakanth7656No ratings yet
- Heart Failure Case Study 1 Fall 2014 JeremyDocument5 pagesHeart Failure Case Study 1 Fall 2014 Jeremyapi-264487290No ratings yet
- Abdominal Aortic Aneurysmn FINAL WORDDocument16 pagesAbdominal Aortic Aneurysmn FINAL WORDErica P. ManlunasNo ratings yet
- Cardiac Arrest CPR GuideDocument54 pagesCardiac Arrest CPR GuideIdha FitriyaniNo ratings yet
- LeukemiaDocument23 pagesLeukemiaSrm GeneticsNo ratings yet
- Hypertension - Clinical: DR Teh Jo Hun AzizahDocument32 pagesHypertension - Clinical: DR Teh Jo Hun AzizahAzizah AzharNo ratings yet
- Managing Hypertension in PregnancyDocument20 pagesManaging Hypertension in PregnancyRelly Arevalo-AramNo ratings yet
- Cancer NursingDocument53 pagesCancer Nursingfairwoods100% (1)
- Biliary DisoderDocument50 pagesBiliary DisoderZanida ZainonNo ratings yet
- Diabetes Mellitus Complications GuideDocument48 pagesDiabetes Mellitus Complications GuideAnditha Namira RS100% (1)
- Acute Abdominal Pain Case: AppendicitisDocument70 pagesAcute Abdominal Pain Case: AppendicitisVenny VeronicaNo ratings yet
- Cerebrovascular Accident: "A Case Study Presentation"Document35 pagesCerebrovascular Accident: "A Case Study Presentation"Kristine YoungNo ratings yet
- By: Calaour, Carrey Dasco, Danica Amor Dimatulac, Kevin Lim, Shiela Marie Pagulayan, Sheena May Pua, Mar KristineDocument41 pagesBy: Calaour, Carrey Dasco, Danica Amor Dimatulac, Kevin Lim, Shiela Marie Pagulayan, Sheena May Pua, Mar Kristineceudmd3d100% (2)
- Myocardial Infarction: Practice Essentials, Background, Definitions PDFDocument12 pagesMyocardial Infarction: Practice Essentials, Background, Definitions PDFMukhtar UllahNo ratings yet
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDocument2 pagesPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenNo ratings yet
- Aneurysm PDFDocument20 pagesAneurysm PDFKV100% (1)
- What Is Rheumatoid ArthritisDocument16 pagesWhat Is Rheumatoid ArthritisDurge Raj GhalanNo ratings yet
- Benign Prostatic HyperplasiaDocument5 pagesBenign Prostatic HyperplasiajustmiitmiideeNo ratings yet
- Management of CholeraDocument69 pagesManagement of CholeraNatalia LawrenceNo ratings yet
- Pulmonary Embolism Guide: Causes, Symptoms & DiagnosisDocument60 pagesPulmonary Embolism Guide: Causes, Symptoms & DiagnosisRafika RaraNo ratings yet
- Care PlanDocument26 pagesCare PlanChevelle Valenciano-GaanNo ratings yet
- Lipid Profile Disease DiagnosisDocument31 pagesLipid Profile Disease DiagnosisGeetanjali Jha100% (1)
- Lung Cancer ScreeningDocument17 pagesLung Cancer ScreeningNguyen Minh DucNo ratings yet
- Emergency Management of DKADocument12 pagesEmergency Management of DKAtinzioNo ratings yet
- COLORECTAL CANCER: SIGNS, STAGES, RISK FACTORS & TREATMENTDocument31 pagesCOLORECTAL CANCER: SIGNS, STAGES, RISK FACTORS & TREATMENTIrene RealinoNo ratings yet
- Understand Diabetes Mellitus Types, Causes, Symptoms and TreatmentDocument22 pagesUnderstand Diabetes Mellitus Types, Causes, Symptoms and TreatmentEman KhammasNo ratings yet
- Diabetic KetoacidosisDocument4 pagesDiabetic KetoacidosisAbigael Patricia Gutierrez100% (1)
- Different Diagnostic Procedure of Typhoid Fever ADocument8 pagesDifferent Diagnostic Procedure of Typhoid Fever AdjebrutNo ratings yet
- Burn Injury PathophysiologyDocument1 pageBurn Injury PathophysiologyMonique Ann DanoyNo ratings yet
- CaseDocument15 pagesCaseNuzma AnbiaNo ratings yet
- Understanding Systolic Hypertension in The Elderly: R Gupta, RR KasliwalDocument7 pagesUnderstanding Systolic Hypertension in The Elderly: R Gupta, RR KasliwallolitlolatNo ratings yet
- 8731 ch03Document37 pages8731 ch03Mohammed Salim AmmorNo ratings yet
- How Alcohol Raises Blood PressureDocument4 pagesHow Alcohol Raises Blood PressureAlessandraNo ratings yet
- AnalysisDocument8 pagesAnalysisJovita Gámez de la RosaNo ratings yet
- Terapi CairanDocument12 pagesTerapi CairanWanAzrenNo ratings yet
- UntitledDocument4 pagesUntitledapi-61200414No ratings yet
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolNo ratings yet
- Basic Chest Radiology ArticleDocument16 pagesBasic Chest Radiology ArticleUsman ShahidNo ratings yet
- DeathbyStrangulation DR - DeanhawleyDocument9 pagesDeathbyStrangulation DR - DeanhawleybaetyNo ratings yet
- WHO Dengue Guidelines 2013Document160 pagesWHO Dengue Guidelines 2013Jason MirasolNo ratings yet
- Diagnosis and Management of Splenic TraumaDocument6 pagesDiagnosis and Management of Splenic TraumaArdel RomeroNo ratings yet
- Myocardial Infarction: Signs and SymptomsDocument5 pagesMyocardial Infarction: Signs and SymptomsKelly OstolNo ratings yet
- Global Citizens AssignmentDocument9 pagesGlobal Citizens Assignmentapi-658645362No ratings yet
- Medical Tribune May 2013Document39 pagesMedical Tribune May 2013Marissa WreksoatmodjoNo ratings yet
- Dual Antiplatelet Therapy Benefits for Prior MI PatientsDocument40 pagesDual Antiplatelet Therapy Benefits for Prior MI PatientsKarren Taquiqui PleteNo ratings yet
- VeslimDocument26 pagesVeslimAbhishekNo ratings yet
- Diabetes The NumbersDocument24 pagesDiabetes The NumbersSasikala RajendranNo ratings yet
- Joseph A. Ladapo, M.D., Ph.D. Curriculum Vitae Business InformationDocument33 pagesJoseph A. Ladapo, M.D., Ph.D. Curriculum Vitae Business InformationWCTV Digital TeamNo ratings yet
- Heart Failure Care Plan LippincottDocument62 pagesHeart Failure Care Plan LippincottDyllano100% (1)
- Research Essay Vongsy 1Document10 pagesResearch Essay Vongsy 1api-509641593No ratings yet
- University For Development Studies: WWW - Udsspace.uds - Edu.ghDocument149 pagesUniversity For Development Studies: WWW - Udsspace.uds - Edu.ghAmeliaNo ratings yet
- The Mediterranean Diet and Cardiovascular HealthDocument20 pagesThe Mediterranean Diet and Cardiovascular HealthResti Eka SaputriNo ratings yet
- Hawthorn (Crataegus SPP.) in The Treatment of Cardiovascular DiseaseDocument10 pagesHawthorn (Crataegus SPP.) in The Treatment of Cardiovascular DiseaseAnonymous EAPbx6No ratings yet
- Physical Activity Readiness Questionnaire 2020Document3 pagesPhysical Activity Readiness Questionnaire 2020freyang esperanzaNo ratings yet
- Iups Programa 25072017 BXDocument76 pagesIups Programa 25072017 BXSonja BuvinicNo ratings yet
- Introduction To Non Communicable DiseasesDocument35 pagesIntroduction To Non Communicable DiseasesNayyar Raza Kazmi100% (1)
- Substance Abuse Treatment and Care For WomenDocument107 pagesSubstance Abuse Treatment and Care For WomenLjilja Taneva100% (1)
- QR Management of Type 2 Diabetes Mellitus (5th Edition) PDFDocument8 pagesQR Management of Type 2 Diabetes Mellitus (5th Edition) PDFKai Xin100% (1)
- Eating Activity Guidelines For New Zealand AdultsDocument87 pagesEating Activity Guidelines For New Zealand AdultsCharli HarrisonNo ratings yet
- NPCDCS Final Operational GuidelinesDocument78 pagesNPCDCS Final Operational GuidelinesTitiksha KannureNo ratings yet
- Sodium Glucose Cotransporter 2 Inhibitors in The Treatment of Diabetes MellitusDocument21 pagesSodium Glucose Cotransporter 2 Inhibitors in The Treatment of Diabetes MellitusManuel PérezNo ratings yet
- Ayusante CatalogueDocument12 pagesAyusante CatalogueAnkit Modi0% (1)
- NCP Nutrition Assesment MatrixDocument22 pagesNCP Nutrition Assesment MatrixPoschita100% (1)
- Why Women Live Longer Than MenDocument21 pagesWhy Women Live Longer Than MenKavitha Bahu ReddyNo ratings yet
- Improve Health and Fitness Goals Through Regular Exercise (EED119Document6 pagesImprove Health and Fitness Goals Through Regular Exercise (EED119Skarzy Abajar100% (1)
- Reading ComprehensionDocument6 pagesReading ComprehensionShanti SubramaniamNo ratings yet
- A Healthy Cholesterol 2011 Final PDFDocument20 pagesA Healthy Cholesterol 2011 Final PDFAli K SheqlawaNo ratings yet
- Hypertension SlidesDocument166 pagesHypertension SlidesStella CooKeyNo ratings yet
- New Approach For CV Risk Management (Prof. DR - Dr. Djanggan Sargowo, SPPD, SPJP (K) )Document56 pagesNew Approach For CV Risk Management (Prof. DR - Dr. Djanggan Sargowo, SPPD, SPJP (K) )Yulia SumarnaNo ratings yet
- Unit 1 New Syllabus NotesDocument69 pagesUnit 1 New Syllabus Notesmalak sherif100% (1)
- Physical Education Chapter - 3Document15 pagesPhysical Education Chapter - 3pragatiNo ratings yet