Professional Documents
Culture Documents
2013 - BestPractices For HLD
Uploaded by
Daniela CirnatuOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2013 - BestPractices For HLD
Uploaded by
Daniela CirnatuCopyright:
Available Formats
Best Practices for
High-Level Disinfection
(HLD)
Objectives
At the end of this program, participants will be able to:
explain the Spaulding classification system for the
reprocessing of reusable medical devices,
understand the importance of effective cleaning and
decontamination prior to HLD,
identify commonly used agents for HLD,
discuss SGNA recommended steps for the HLD of
flexible endoscopes.
Spaulding Classification System
In 1968, Dr. Earle Spaulding devised a rational
approach to disinfection and sterilization that is
still in use today. He believed that instruments
and equipment should be reprocessed according
to the nature of the item and the level of risk
associated with their intended use.
This is referred to as Spaulding's classification system
and it has been refined and retained over the years,
because it is so clear and logical. The three (3) categories
he described were critical, semi-critical and non-critical.
Spaulding Classification System
Critical items are medical devices that enter sterile tissue
or the vascular system. These items should be sterile
when used. Examples include, but are not limited to:
surgical instruments, cutting endoscopic accessories that
break the mucosal barrier, endoscopes used in sterile body
cavities, cardiac, vascular or urinary catheters, implants,
needles and ultrasound probes used in the sterile body
cavities.
Spaulding Classification System
Semi-critical items are medical devices that come into
contact with non-intact skin or mucous membranes.
These items should be high level disinfected when used.
Examples include, but are not limited to: vaginal and
rectal probes, anesthesia equipment, laryngoscopes,
bronchoscopes and gastrointestinal endoscopes (and
accessories).
Spaulding Classification System
Non-critical items are medical devices that come into
contact with only intact skin. These items should receive
intermediate level disinfection, low-level disinfection or
cleaning. Intact skin acts is considered an effective
barrier to most organisms. Examples of non-critical item
include, but are not limited to: tourniquets and blood
pressure cuffs, linens, bed pans and stethoscopes.
The terminology adopted by the CDC and widely used,
describes disinfectants in terms of their activity as set out
below. This program will focus on high-level disinfection
(HLD).
High-level disinfectants are chemical sterilants, which when
used for a shorter exposure period than would be required
for sterilization, kill all microorganisms with the exception
of high numbers of bacterial spores.
Intermediate-level disinfectants may kill mycobacteria,
vegetative bacteria, most viruses, and most fungi but do not
necessarily kill bacterial spores
Low-level disinfectants may kill most vegetative bacteria,
some fungi, and some viruses.
Three Levels of Disinfection
Pre-cleaning must occur at point of use in order to keep
blood and other organic material from drying. Blood and
body fluids, as well as saline, are highly corrosive and can
damage instruments. Dried blood and debris is difficult, if
not impossible to clean during decontamination, which can
cause disinfection or sterilization not to be achieved.
Surgical instruments should be wiped as needed with
sterile surgical sponges moistened with sterile water during
the procedure to remove gross soil. Instruments with
lumens should be irrigated with sterile water.
Cleaning and Decontamination
Flexible endoscopes used on the sterile field should be
pre-cleaned to the following recommended steps:
1. Wipe external surfaces with a lint-free cloth saturated
with sterile water.
2. Alternate suctioning the channels with sterile water
and air.
3. Hand the endoscope and accessories to the circulator
as soon as possible, so he/she may pre-clean (follow
the steps on the next slide).
Cleaning and Decontamination
Flexible endoscopes used in GI/Endoscopy Centers
should be pre-cleaned in the Procedure Room wearing
appropriate PPE and using the following recommended
steps:
1. External surface of insertion tube should be cleaned
with a soft cloth or sponge and an enzymatic detergent.
2. Internal suction/biopsy channels cleaned by suctioning
copious amounts of enzymatic detergent and air.
3. Air/water channels flushed with enzymatic solution,
then flushed using low-pressure compressed air or a
syringe if air is not available.
Cleaning and Decontamination
4. Complex design components or channels should be
flushed or purged with water and/or enzymatic
detergent solution per the MFGs IFU.
5. The tip of the endoscope should be inspected for
damage to any surface and any working part, and for
cleanliness.
6. The video protective cap (if applicable) should be
attached after removing the endoscope from the light
source and suction.
7. Remove all detachable parts and immerse in enzymatic
detergent solution until transport.
Cleaning and Decontamination
Cleaning and Decontamination
Flexible endoscopes are some
of the most complex devices
for health care workers to
reprocess, due to their unique
design and multiple reprocessing
steps.
Strict adherence to the scope
MFGs validated instructions
for use (IFU) is required.
After pre-cleaning at point of use, contaminated items
should be immediately transported to the decontamination
area before any remaining organic material dries on the
surface, box lock, crevices or channels of the instruments.
Surgical instruments should be covered with a wet towel
or treated with an instrument cleaner prior to transport.
Contaminated items can expose health care workers and
can contaminate the environment during transport. A
sealed container should be used to avoid contaminating
the environment or exposure to health care workers. Per
OSHA, the transport container must be labeled to indicate
biohazardous contents.
Transport
Meticulous cleaning and decontamination must proceed
HLD or sterilization. Medical device manufacturers are
required to provide healthcare facilities with validated
reprocessing instructions for use (IFU).
It is important to have and follow each device MFGs IFU
to ensure worker and patient safety. This is especially true
for complex devices with multiple pieces that have joints,
crevices, lumens, ports and channels. Proper PPE is
required for all cleaning and decontamination steps.
Cleaning and Decontamination
Pasteurization is a heat-automated HLD process that uses
time and heat (i.e. 160-170F/21.7-25C) for 30 minutes
for HLD of heat-sensitive semi-critical devices. Medical
washer/pasteurizers have wash, rinse and pasteurization
cycles. Some pasteurizers offer quality assurance data
recorders that document the temperature and cycle time.
Heat HLD
For chemical HLD, health care facilities must purchase
FDA cleared HLD products as listed on the FDA website.
Products selected should be compatible and efficacious
with the materials or items to be disinfected.
The use of incompatible chemicals can damage the
surfaces of the instrument, causing corrosion, scratches
and other surface irregularities. Such damage can be a
challenge for cleaning, HLD, interfere with proper
function, and reduce the life and cosmetic appearance
of the device.
Chemical HLD
FDA-cleared Chemical sterilants and HLDs
Device Type # of Registered
Products
Chemical
Sterilization
High Level
Disinfection
Glutaraldehyde 17 X X
Hydrogen Peroxide 4 X X
Ortho-phthaldehyde
(OPA)
3 X
Peracetic Acid 2 X X
Sodium Hypochlorite 1 X
Chemical Vapor
w/Formaldehyde
2 X
Hydrogen Peroxide Gas
Plasma
1 X
Hydrogen Peroxide
without Plasma
1 X
Ozone Gas 1 X
Source: www.fda.gov/MedicalDevices/DeviceRegulationandGuidance/ReprocessingofSingle-UseDevices/ucm133514.htm
HLD requires appropriate temperature, contact time, and
length of use following solution activation. MFGs IFU
should be followed when preparing disinfectant solutions,
calculating expirations dates, and labeling solution soaking
containers.
Chemical HLD
Glutaraldehyde has been widely used for a long time in
health care facilities as a HLD for reusable medical devices.
Most solutions are acidic and must be activated to become
sporicidal. There are a variety of brand names available in
a variety of concentrations, with and without surfactants.
Chemical HLD
HLD and Steriliant
requires no mixing or
activation
Ortho-phthaladehyde (OPA) has demonstrated superior
mycobactericidal activity compared to glutaraldehyde and
requires no mixing or activation. OPA has been shown to
last longer before reaching its MEC and the concentration
of the active ingredient does not decrease with age alone.
Chemical HLD
Other solutions FDA-cleared for HLD include hydrogen
peroxide, peracetic acid and sodium hypochlorite in a
variety of concentrations and combinations. The FDA
website has a listing of manufacturers, active ingredients
and contact conditions for each cleared solution.
Chemical HLD
Because most HLDs are reused, they must be tested and
recorded prior to each use to assure that they remain
above their MEC. If the test strip fails, the HLD solution
should not be used, even if its within the reuse life.
Chemical HLD
Reprocessing of Flexible Endoscopes
Chemical HLD is recognized as the standard for the
reprocessing of flexible gastrointestinal endoscopes by
SGNA, ASGE, ACG, AGA, APIC and AST. Also, the
CDC and The Joint Commission recognize HLD as
appropriate for gastrointestinal endoscopes.
Standards of Infection Control in
Reprocessing of Flexible
Gastrointestinal Endoscopes
Are you following the updated 2012 SGNA Standards?
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5. Manual HLD:
1. Completely immerse the endoscope and all
removable parts in a basin of HLD.
a. The basin must be of a size to accommodate the
endoscope without undue coiling, and must have a
tight-fitting lid to contain the chemical vapors.
b. To prevent damage, the endoscope should be not
be soaked with other sharp instruments.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5. Manual HLD
2. Flush disinfectant into all channels of the
endoscope until it can be seen exiting the opposite
end of each channel. Take care that all channels are
filled with the chemical, and that no air pockets
remain within the channels.
SGNA Standards of Infection Control in
Reprocessing of Flexible Endoscopes
5A. Manual HLD:
a. Complete microbial destruction cannot occur
unless all surfaces are in complete contact with the
chemical.
b. Since internal contact cannot be visually confirmed
because of scope design, purging until a steady flow
of solution observed is necessary.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5A. Manual HLD:
3. Cover the soaking basin with a tight-fitting lid
to minimize chemical vapor exposure.
Note that:
a. Exposure to chemical vapors may present a
health hazard.
b. The reprocessing area should have engineering
controls to ensure good air quality.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5A. Manual HLD:
4. Soak the endoscope in the HLD solution for
the time/temperature required to achieve HLD.
Use a timer to verify soaking time.
5. Purge all channels completely with air before
removing the endoscope from the HLD solution.
Note that purging the channels preserves the
concentration and volume of the chemical, and
prevents exposure from dripping and spilling.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5A. Manual HLD:
6. RINSE (same as after Manual Cleaning)
a. Thoroughly rinse the endoscope and all removable
parts with clean water to remove residual debris and
detergent.
b. Purge water from all channels using forced air.
Dry the exterior of the endoscope with a soft, lint-
free cloth to prevent dilution of the liquid chemical
germicide used in subsequent steps.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
6. Drying:
a. Purge all channels with air until dry.
Note that:
1) Bacteria such as Pseudomonas aeruginosa have been
identified in both tap and filtered water, and may multiply
in a moist environment.
2) Avoid the use of excessively high air pressure which
can damage the internal channels of flexible endoscopes.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
6. Drying:
b. Flush all channels, including accessory channels,
with alcohol until the alcohol can be seen exiting the
opposite end of each channel.
1) 70% isopropyl alcohol is used to assist in drying the
interior channel surfaces.
2) It must be properly stored in a closed container
between uses, because when exposed to air, it rapidly
evaporates, and if less than recommended % level,
cannot be relied upon to assist in the drying process.
3) Alcohol flushes should be used even when sterile
water is used for rinsing.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
6. Drying:
c. Purge all channels with air. Note that alcohol
mixes with the remaining water on the channel
surfaces and acts to encourage evaporation of the
residual water as air flows through the channel.
d. Remove all channel adapters.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
6. Drying:
e. Dry the exterior of the endoscope with a soft,
clean lint-free towel.
f. Thoroughly rinse and dry all removable parts.
Do not attach removable parts (e.g. valves, etc.)
to the endoscope during storage as this can trap
liquid inside.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
7. Storage:
Hang the endoscope in a vertical position to facilitate
drying (with caps, valves, and other detachable components
removed, per MFGs IFU).
a. The storage area should be clean, well
ventilated and dust free.
b. Correct storage will prevent damage.
c. The interval of storage before use has
limited investigations and warrants further
data.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5B. Automated HLD:
Automated Endoscope Reprocessors (AERs)
standardize the disinfection process and decrease
personnel exposure to HLDs.
NOTE:
It is necessary to follow
all steps for the manual
cleaning prior to using
an AER.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
5B. Automated HLD:
An AER should have the following features:
a. Circulate fluids through all endoscope channels at an equal
pressure without trapping air. Channel flow sensors provide
an added measure of compliance.
b. Detergent and disinfectant cycles should be followed by
thorough rinse cycles and forced air to remove all used
solutions.
c. Disinfectant should not be diluted with any fluids.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
An AER should have the following features:
d. Machine should be self-disinfecting.
e. No residual water should remain in hoses and reservoirs.
f. Cycles for alcohol flushing and forced air drying are desirable.
g. Should also feature a self-contained or external water
filtration system.
In addition, a method to automatically store or print data
verification of cycle completion, is desirable.
SGNA Standards of Infection Control
in Reprocessing of Flexible Endoscopes
To use an AER:
1. Follow steps for manual cleaning of endoscope.
2. Prepare the AER according to the MFGs guidelines.
3. Place the endoscope in the AER and attach all channel
adapters according to the MFGs IFU.
a. The elevator channel of a duodenoscope has a very small
lumen. Since most AERs cannot generate pressure required to
force fluid through the lumen, a 2-5 ml syringe must be used
to manually reprocess (all steps) the elevator channel unless
the AER is validated to perfuse this channel.
To use an AER:
4. Place valves and other removable parts into the
soaking basin of the AER. Unless the AER has a
dedicated space for accessories, reprocess these
items separately.
5. If the AER has a cycle that uses enzymatic
detergent, it should be a product that is compatible
with the AER and the endoscope.
6. Set the AER for the appropriate time and
temperature depending on the chemical used.
7. Start the AER and allow it to complete all
cycles or phases. Note that if cycles or phases
are interrupted, HLD cannot be ensured and
the full cycle must be repeated.
To use an AER:
8. If AER does not include a final alcohol rinse,
this step should be done manually followed by
purging all the channels with air until dry.
The ERCP elevator and elevator channel must
be manually perfused and dried per MFGs
instructions.
9. Drying and storage procedures are the same as
described in the manual disinfection section.
To get a free copy of the complete SGNA
document, go to: www.sgna.org
Healthcare facilities are responsible for providing a safe
work and patient care environment. Patients, visitors, and
health care workers should be protected from injuries or
illnesses caused by hazardous chemicals.
When handling HLDs, personnel should wear protective
apparel that may include, but is not limited to:
100% nitrile rubber or 100% butyl rubber gloves when
handling glutaraldehyde. PVC gloves should not be
worn because they absorb glutaraldehyde.
Protective eye wear, face mask, and impervious gown.
Chemical HLD Safety
Glutaraldehyde should only be used in well ventilated
areas or in freestanding or vented chemical fume hoods.
Vapor generated from glutaraldehyde can may aggravate
preexisting respiratory conditions.
AAMI describes adequate ventilation as:
1. Room large enough to ensure adequate dilution of vapors.
2. 10 air exchanges per hour.
3. Exhaust located at the source of the discharge of vapors.
4. Fresh air return at ceiling level across room from exhaust vents.
5. Routine maintenance and surveillance of system.
6. Elimination of cross draft effects.
7. Air must not be recirculated.
Chemical HLD Safety
Glutaraldehyde can be absorbed by inhalation, ingestion
and through the skin. It has a detectable odor at 0.04 parts
per million volume (ppmv) and is irritating to skin and
mucous membranes at 0.3 ppmv.
Vapors are released whenever solutions are disturbed and
the surface tension is broken, such as mixing, adding and
removing equipment, or disposing of a glutaraldehyde
solution can cause a break in the surface tension.
Whenever the glutaraldehyde solution is not being
accessed, it should be covered with a tight-fitting lid.
Chemical HLD Safety
Glutaraldehyde vapor monitoring is important per
The American Conference of Governmental Industrial
Hygienists (ACGIH) which recommends a ceiling limit
of 0.05 ppm for occupational exposure.
OSHA has not established exposure limits; however,
OSHA can regulate exposure and has recommended
following the ACGIH limit.
Chemical HLD Safety
To avoid these glutaraldehyde issues, many health care
facilities have switched to using an OPA for HLD. The
Rapicide OPA/28 features the fastest disinfection time,
twice the reuse period of other OPA brands and guaranteed
materials compatibility.
Chemical HLD
Exposure monitoring is not required; however, OPA is
still a potential irritant of eyes, skin, nose and other tissues
resulting in symptoms such as stinging, excessive tearing,
coughing, and sneezing. Like glutaraldehyde, OPA fixes
proteins, allows for biofilm formation and exposure causes
staining on linen, skin, instruments and AERs.
Chemical HLD Safety
Personnel should receive initial training and competency
validation on procedures, chemicals used, and PPE and
should receive additional training when new equipment,
instruments, supplies, or procedures are introduced.
Employers must provide a written hazard communication
program, hazard evaluation, hazardous materials inventory,
Safety Data Sheets, labels on all containers of hazardous
chemicals, and employee training.
Training and Education
A quality control program should be established in all
areas where HLD is used. Quality control programs
should be documented and should include, but not be
limited to:
Orientation programs
Competency assurance
Continuing education
Quality control checks
Investigation of adverse events
Monitoring of solution replacement intervals
Quality Control Program
Surfaces of complex instruments require meticulous
cleaning in order to minimize infection control risks
to patients and staff. Inadequate cleaning can potentially
leave residual protein on a surface.
Quality control checks, such as
ATP systems and VERiFIND
Protein Detection Kit, provide
rapid and easy to read
cleaning verification.
Quality Control Program
Health care workers responsible for HLD must maintain
the technical skills needed to establish and maintain a safe
practice environment for patients, visitors and peers.
Administrative personnel must ensure competency
validation of personnel participating in decontamination
and HLD of reusable medical devices. The validation of
competencies should include all types of devices the
individual is authorized to reprocess.
CONCLUSION
THANK YOU!
SPSmedical Supply Corp.
Sterilization Products & Services
6789 W. Henrietta Road
Rush, NY 14543 USA
Fax: (585) 359-0167
Ph: (800) 722-1529
website: www.SPSmedical.com
2013, SPSmedical Supply Corp.
Free CE programs are available in our
Sterilization Classroom on the
SPSmedical website.
References & Resources
Association for the Advancement of Medical Instrumentation. (2010). Chemical sterilization and
high level disinfection in health care facilities (ANSI/AAMI ST58:2005/(R) 2010). Arlington, VA.
Association of periOperative Registered Nurses. (2013 Edition). Recommended Practices for
High-Level Disinfection.
Society of Gastroenterology Nurses and Association, Inc. (2007) Guideline for High-Level
Disinfectants & Sterilants for Reprocessing Flexible Gastrointestinal Endoscopes.
Society of Gastroenterology Nurses and Association, Inc. (2012) Standards of Infection Control
in Reprocessing of Flexible Gastrointestinal Endoscopes.
Occupational Health and Safety Administration (OSHA). (2012). Hazardous waste and emergency
response. www.osha.gov
Rutala, W. A., Weber, D. J., & the Healthcare Infection Control Practices Advisory Committee
(HICPAC). (2008). Guideline for Disinfection and Sterilization in Healthcare Facilities.
You might also like
- Statistical Methods for Evaluating Safety in Medical Product DevelopmentFrom EverandStatistical Methods for Evaluating Safety in Medical Product DevelopmentA. Lawrence GouldNo ratings yet
- Eli Lilly Biotech Pilot Plant, Indianapolis, United States of AmericaDocument5 pagesEli Lilly Biotech Pilot Plant, Indianapolis, United States of AmericaShyam Sunder BudhwarNo ratings yet
- Biological Evaluation of Medical Devices / Biosafety: Applicable ProductsDocument5 pagesBiological Evaluation of Medical Devices / Biosafety: Applicable ProductsAnonymous iqoU1mtNo ratings yet
- Iec62304 3Document5 pagesIec62304 3Abdul RahmanNo ratings yet
- ISO 18113-1 2022 Ed.2 - Id.79866 Publication PDF (En)Document60 pagesISO 18113-1 2022 Ed.2 - Id.79866 Publication PDF (En)Qualidade FrilaboNo ratings yet
- Cleaning and Sterilization GuideDocument48 pagesCleaning and Sterilization GuideFrankArenasNo ratings yet
- Rockwell Software Product CatalogDocument36 pagesRockwell Software Product CatalogAdhemar RodoNo ratings yet
- Lecture7 Introduction To Medical Devices ManagementDocument7 pagesLecture7 Introduction To Medical Devices ManagementRula BastoniNo ratings yet
- ZFP Op Man - EN PDFDocument142 pagesZFP Op Man - EN PDFMohamed Abd El-Fattah GalalNo ratings yet
- Regulatory Samvad Feb 2020Document19 pagesRegulatory Samvad Feb 2020vibhu yadavNo ratings yet
- Bioinformatics CompaniesDocument18 pagesBioinformatics Companiesmy.dear.sirNo ratings yet
- Principles of Software EngineeringDocument2 pagesPrinciples of Software EngineeringKr UthayanNo ratings yet
- Lecture4 Introduction To Medical Devices ManagementDocument9 pagesLecture4 Introduction To Medical Devices ManagementRula BastoniNo ratings yet
- Pacs (Picture Archiving and Communication Systems) & Vna (Vendor Neutral Archives)Document18 pagesPacs (Picture Archiving and Communication Systems) & Vna (Vendor Neutral Archives)LawrenceNo ratings yet
- Auditing Operating Systems Networks: Security Part 1: andDocument24 pagesAuditing Operating Systems Networks: Security Part 1: andAmy RillorazaNo ratings yet
- Defect Tracking SystemDocument21 pagesDefect Tracking Systemmughees1050% (2)
- High Performance Medical Grade Resins PDFDocument11 pagesHigh Performance Medical Grade Resins PDFGeorge CobraNo ratings yet
- ART - 0608 - Improving Ops With EBRDocument4 pagesART - 0608 - Improving Ops With EBRkumar_chemicalNo ratings yet
- Recent Trends in Sterile InspectionsDocument40 pagesRecent Trends in Sterile InspectionsSilke IgemannNo ratings yet
- Data Integrity & SecurityDocument3 pagesData Integrity & SecurityReshma WawhalNo ratings yet
- McKesson Letter of FDA's Proposed Medical Device Data Systems RuleDocument5 pagesMcKesson Letter of FDA's Proposed Medical Device Data Systems RulehuffpostfundNo ratings yet
- Detailed Design Specification TemplateDocument8 pagesDetailed Design Specification Templatemaddy_cooldude6763No ratings yet
- IntegrityDocument25 pagesIntegrityChhatrashal Singh RathoreNo ratings yet
- Glucometer SRSDocument15 pagesGlucometer SRSYisha XiaNo ratings yet
- Competitive Analysis of Market Leaders in Data ModelingDocument24 pagesCompetitive Analysis of Market Leaders in Data ModelingXavier Martinez Ruiz100% (2)
- SBSI CoagulationDocument3 pagesSBSI Coagulationjay primaNo ratings yet
- Global Medical Device Nomenclature: Mark Wasmuth Secretary General GMDN AgencyDocument23 pagesGlobal Medical Device Nomenclature: Mark Wasmuth Secretary General GMDN AgencyluNo ratings yet
- Seven Principles of Software TestingDocument3 pagesSeven Principles of Software TestingpedromoritzNo ratings yet
- Dell EMC Validates Your Virtualized Genetec Video Management System Before It Reaches Your HandsDocument11 pagesDell EMC Validates Your Virtualized Genetec Video Management System Before It Reaches Your HandsPrincipled TechnologiesNo ratings yet
- GMP 2023 - Sessions PresentationsDocument289 pagesGMP 2023 - Sessions PresentationsKamanashish Chowdhury100% (1)
- Automated Packaging Systems Autolabel Pi-4000 In-Line, Programmable, Thermal Transfer PrinterDocument2 pagesAutomated Packaging Systems Autolabel Pi-4000 In-Line, Programmable, Thermal Transfer PrinterEdgar HoowerNo ratings yet
- SharePoint 2013 Qualif. Pack List-1Document2 pagesSharePoint 2013 Qualif. Pack List-1akbarmulangathNo ratings yet
- Software Quality EnginneringDocument26 pagesSoftware Quality EnginneringVinay PrakashNo ratings yet
- Research Paper Artificial Intelligence in Medical JEEV AI-IJRASETDocument8 pagesResearch Paper Artificial Intelligence in Medical JEEV AI-IJRASETIJRASETPublicationsNo ratings yet
- 03 System TestingDocument17 pages03 System TestingramNo ratings yet
- Data Validation, Processing, and Reporting Data ValidationDocument8 pagesData Validation, Processing, and Reporting Data ValidationNaga Ajay Kumar DintakurthiNo ratings yet
- Aplicabilidad 21CFR11Document6 pagesAplicabilidad 21CFR11Aydee RojasNo ratings yet
- Symbient PRD TemplateDocument5 pagesSymbient PRD TemplateBikash Chandra SahooNo ratings yet
- Test Design Specification TemplateDocument4 pagesTest Design Specification TemplateRifQi TaqiyuddinNo ratings yet
- SDLCDocument22 pagesSDLCRishabh AroraNo ratings yet
- What Is JIRA?: Issue: Every Task, Bug, Enhancement Request BasicallyDocument1 pageWhat Is JIRA?: Issue: Every Task, Bug, Enhancement Request Basicallylilithknowsitall6393No ratings yet
- Oven ManualDocument28 pagesOven ManualromwellNo ratings yet
- Backup and Recovery Best Practices For Leadership and PlanningDocument5 pagesBackup and Recovery Best Practices For Leadership and PlanningVijay Jangetti SanjeeviNo ratings yet
- FDA Design Considerations For Devices Intended For Home UseDocument27 pagesFDA Design Considerations For Devices Intended For Home Use0SpYkeNo ratings yet
- Manufacturing Execution System (MES) : ServiceDocument48 pagesManufacturing Execution System (MES) : ServiceNhat Tan MaiNo ratings yet
- Smart Lab E BookDocument24 pagesSmart Lab E BookNaveed MubarikNo ratings yet
- Strategic Management and Project Management: PurposeDocument10 pagesStrategic Management and Project Management: PurposesurapolNo ratings yet
- Road Map To Design Successful Software - Ictms (Integrated Clinical Trial Management System)Document8 pagesRoad Map To Design Successful Software - Ictms (Integrated Clinical Trial Management System)SanjayPravinbhaiVarmaNo ratings yet
- Requirement Engineering SummaryDocument14 pagesRequirement Engineering SummaryBob ChanNo ratings yet
- Seilevel Agile Requirements Document TemplateDocument10 pagesSeilevel Agile Requirements Document TemplateSanoufar ANo ratings yet
- GMP Simatic Pcs7-V90 en En-UsDocument184 pagesGMP Simatic Pcs7-V90 en En-UshuykhiemNo ratings yet
- Broch Biostat-STR-Flexsafe SBI1509-e NeuDocument24 pagesBroch Biostat-STR-Flexsafe SBI1509-e NeuBrian VasquezNo ratings yet
- FDA Pre Submission Cover LetterDocument5 pagesFDA Pre Submission Cover Letteregdxrzadf100% (2)
- Medical Product DevelopmentDocument64 pagesMedical Product DevelopmentIhsanNo ratings yet
- CDRH201461 HomeUseDesign FinalGuidanceDocument27 pagesCDRH201461 HomeUseDesign FinalGuidancerehmanabbasiNo ratings yet
- Unique Device IdentificationDocument15 pagesUnique Device IdentificationSureshNo ratings yet
- AG3110 - Vue PACS and Vue Archive 12.2 Administration GuideDocument177 pagesAG3110 - Vue PACS and Vue Archive 12.2 Administration GuideAndreia Yamamoto MorassutiNo ratings yet
- Sferd Handbook Flexible Endoscopes Cleaning Disinfection - en PDFDocument106 pagesSferd Handbook Flexible Endoscopes Cleaning Disinfection - en PDFmochkurniawanNo ratings yet
- Software ArchitectureDocument30 pagesSoftware ArchitectureMukesh RegmiNo ratings yet
- Labelling Nutrition-Vitamins Minerals-Guidance Tolerances Summary Table 012013 enDocument1 pageLabelling Nutrition-Vitamins Minerals-Guidance Tolerances Summary Table 012013 enDaniela CirnatuNo ratings yet
- 202103011101-Ghid de Prevenire Iaam 2021Document52 pages202103011101-Ghid de Prevenire Iaam 2021Daniela CirnatuNo ratings yet
- Notification File Food Supplement / Fortified Food: OmpanyDocument4 pagesNotification File Food Supplement / Fortified Food: OmpanyDaniela CirnatuNo ratings yet
- Disinfection and SterilizationDocument23 pagesDisinfection and SterilizationDaniela Cirnatu100% (1)
- Mayo Clinic Proceedings: Vitamin D Supplementation During The COVID-19 PandemicDocument2 pagesMayo Clinic Proceedings: Vitamin D Supplementation During The COVID-19 PandemicDaniela CirnatuNo ratings yet
- Patient Identity NicknameDocument2 pagesPatient Identity NicknameDaniela CirnatuNo ratings yet
- 11.5 ArsenicDocument18 pages11.5 ArsenicDaniela CirnatuNo ratings yet
- Hepatorenal and Genotoxic Effects of Genetically Modified Quail Meat in A 90-Day Dietary Toxicity Study in MiceDocument7 pagesHepatorenal and Genotoxic Effects of Genetically Modified Quail Meat in A 90-Day Dietary Toxicity Study in MiceDaniela CirnatuNo ratings yet
- CXS - 197e Norma Codex AVOCADO Draft EnglishDocument6 pagesCXS - 197e Norma Codex AVOCADO Draft EnglishDaniela CirnatuNo ratings yet
- Chemistry Investigatory ProjectDocument19 pagesChemistry Investigatory ProjectDivya Vatsa50% (4)
- Study On Detergent PowderDocument12 pagesStudy On Detergent PowderRamesh Choudhary100% (2)
- Spectracron 110 FD Alkyd Enamel PDFDocument2 pagesSpectracron 110 FD Alkyd Enamel PDFSatish Vishnubhotla0% (1)
- Analysis of Cement by Banana FiberDocument48 pagesAnalysis of Cement by Banana FiberKyaw KhineNo ratings yet
- Chapter 9 The Endocrine SystemDocument1 pageChapter 9 The Endocrine SystemacNo ratings yet
- Chemistry Investigatory Project 2017-18Document29 pagesChemistry Investigatory Project 2017-18Ashok KumarNo ratings yet
- Realistic Well Planning With Dynamic Well Control ModellingDocument7 pagesRealistic Well Planning With Dynamic Well Control ModellingAoun MuhammadNo ratings yet
- 30 Sewage Treatment PlanDocument63 pages30 Sewage Treatment PlanYuri Duri100% (1)
- Final Examination: Your Answer On The Space Provided For. (40 Points)Document5 pagesFinal Examination: Your Answer On The Space Provided For. (40 Points)Wichel AnnNo ratings yet
- Carbon NanotubesDocument15 pagesCarbon NanotubesLaraib HabibNo ratings yet
- Universitas Ahmad Dahlan - JellyDocument15 pagesUniversitas Ahmad Dahlan - JellyMaqfirotul LailyNo ratings yet
- Trepanning Positioning Welding ManualDocument14 pagesTrepanning Positioning Welding ManualGovindan PerumalNo ratings yet
- S Start of Lesson E End of Lesson Grading 1-5: Learning Outcomes Progress ArrowDocument30 pagesS Start of Lesson E End of Lesson Grading 1-5: Learning Outcomes Progress ArrowYu Seung KimNo ratings yet
- Mil PRF 9954DDocument8 pagesMil PRF 9954DjhscribdaccNo ratings yet
- Single Phase Heat Transfer and Pressure Drop Characteristics of Micro-Fin TubesDocument2 pagesSingle Phase Heat Transfer and Pressure Drop Characteristics of Micro-Fin TubesGerehNo ratings yet
- 11 - Isomerism in TMCDocument18 pages11 - Isomerism in TMCMohit KambojNo ratings yet
- Eucomex - Eucomex - EnglishDocument2 pagesEucomex - Eucomex - EnglishNelson IbarraNo ratings yet
- Simulation of Reactive Distillation ColumnDocument6 pagesSimulation of Reactive Distillation ColumnthanhndbNo ratings yet
- Special Issue Honoring Don Mackay: Oil Spill Impact Modeling: Development and ValidationDocument16 pagesSpecial Issue Honoring Don Mackay: Oil Spill Impact Modeling: Development and Validationbrice mouadjeNo ratings yet
- 4 Elements, Mixtures and Compounds: WorksheetDocument3 pages4 Elements, Mixtures and Compounds: WorksheetMfanafuthiNo ratings yet
- Toxicity of Common Laboratory Chemicals To Human Red Blood Cells Laboratory ActivityDocument4 pagesToxicity of Common Laboratory Chemicals To Human Red Blood Cells Laboratory ActivityKuven Malig-onNo ratings yet
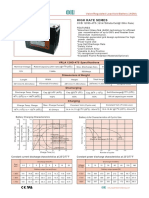
- High Rate Series: CCB 12HD-475Document1 pageHigh Rate Series: CCB 12HD-475orunmila123No ratings yet
- Rusting WorksheetDocument2 pagesRusting WorksheetSelwah Hj AkipNo ratings yet
- Magnetic Terms and UnitsDocument3 pagesMagnetic Terms and UnitsDeepak Choudhary DCNo ratings yet
- Advanced Inorganic Chemistry (CHM4301) : Alkenes and AlkynesDocument19 pagesAdvanced Inorganic Chemistry (CHM4301) : Alkenes and AlkynesAnonymous lClX1bNo ratings yet
- Jotun Penguard Express CF TDSDocument5 pagesJotun Penguard Express CF TDSnihad_mNo ratings yet
- Name: Grade & Section: Teacher: Score: General Direction: This Is A 50-Item Test, Read Each Direction Written in Every Type of Test, Answer ThisDocument4 pagesName: Grade & Section: Teacher: Score: General Direction: This Is A 50-Item Test, Read Each Direction Written in Every Type of Test, Answer ThisMara LabanderoNo ratings yet
- Hot Tap ProcedureDocument6 pagesHot Tap ProcedureNatarajan MurugesanNo ratings yet
- 2002Document38 pages2002B GirishNo ratings yet
- Pulp Mill Odor ControlDocument6 pagesPulp Mill Odor Controlalakazum28No ratings yet