Professional Documents
Culture Documents
Febuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go To
Uploaded by
Anadi GuptaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Febuxostat (Uloric), A New Treatment Option For Gout: Carmela Avena-Woods Olga Hilas Author Information Go To
Uploaded by
Anadi GuptaCopyright:
Available Formats
Febuxostat (Uloric), A New Treatment Option
for Gout
Carmela Avena-Woods, PharmD and Olga Hilas, PharmD, MPH, BCPS, CGP
Author information Copyright and License information
Go to:
INTRODUCTION
Gout is a rheumatic condition resulting from the deposition of monosodium urate crystals (tophi)
in the joints or soft tissues. It is usually associated with elevated serum uric acid levels (greater
than 7 mg/dL). The diagnosis is based on uric acid crystals found in the joints, tissues, or body
fluids, as well as on gouty attacks or flares characterized by intense pain, swelling, redness, and
heat.
14
The peak incidence of gout occurs between 30 and 50 years of age. Approximately 1% to
2% of Americans are affected, with an equal prevalence in men and women; however, men are
more likely to have elevated serum uric acid levels (hyperuricemia).
2,4,5
Hyperuricemia results from the accumulation of uric acid, the end product of purine metabolism,
which possesses no physiological role.
2,6
It has been associated with a high-purine diet (i.e.,
meats, seafood), alcohol use, diuretic therapy, reduced renal clearance, hypertriglyceridemia, and
diabetes mellitus.
2,6,7
Non-steroidal anti-inflammatory medications (NSAIDs), colchicine,
corticosteroids, and analgesics are commonly used in the acute treatment of gout. Goals of
therapy include controlling acute attacks, preventing recurrent attacks, and preventing or
reversing complications.
6,8
Chronic management of gout may include the long-term use of urate-lowering agents after an
attack is treated and prophylactic therapy has been considered. Antihyperuricemic therapy is
indicated in patients who have had two or more gouty attacks per year, tophaceous gout, erosive
arthritis on radiographs, or uric acid kidney disease.
9,10
In most patients, a serum uric acid level
of below 6 mg/dL is the initial target for therapy. Urate-lowering agents should be started after
the complete resolution of a gouty attack because a rapid decrease in serum urate levels
sometimes exacerbates a subsequent attack.
2,8
Underexcretion of uric acid is responsible for gout in approximately 90% of patients; therefore,
uricosuric agents should be used in most patients after ongoing urate deposition has been
confirmed and attempts to correct or reverse other causes of hyperuricemia have been made.
6,7,11
Inhibitors of uric acid synthesis are also used, particularly for patients who produce excessive
amounts of urate (more than 800 mg in 24 hours).
8
Allopurinol (Zyloprim, Prometheus), a potent purine xanthine oxidase (XO) inhibitor, is the most
commonly used drug in the treatment of hyperuricemia. Until recently, it was the only available
inhibitor of uric acid synthesis. In February 2009, the FDA approved febuxostat (Uloric, Takeda
Pharmaceutics America), a structurally unrelated non-purine XO inhibitor, for the chronic
management of hyperuricemia in patients with gout.
12,13
Go to:
PHARMACOLOGY AND MECHANISM OF
ACTION
4,12,1417
Patients with gout can be categorized into two groups: (1) overproducers of uric acid or (2)
underexcreters of uric acid. Hyperuricemia can thus result from the endogenous production of
uric acid, a high rate of renal urate reabsorption, or a diet high in purines. XO inhibitors are
effective in treating patients with both categories of gout as a result of their inhibition of uric
acid synthesis by impairing the conversion of hypoxanthine to xanthine, which results in uric
acid formation.
As a non-purine selective XO inhibitor, febuxostat inhibits both oxidized and reduced types of
XO. It does not inhibit enzymes involved in purine or pyrimidine metabolism, as does
allopurinol. Febuxostat is also structurally unrelated to allopurinol; its structure does not
resemble a pyrimidine or a purine. The drugs active ingredient is 2-(3-cyano-4[2-
methylpropoxy] phenyl)-4-methylthiazole-5-carboxylic acid. The empirical formula is
C
16
H
16
N
2
O
3
S, with a molecular weight of 316.38. As a result of its selectivity and structural
differences, febuxostat tends to cause fewer adverse events when compared with allopurinol.
Go to:
PHARMACOKINETICS AND
PHARMACODYNAMICS
12,14,18,19
Febuxostat is administered orally and is quickly absorbed; it reaches its maximum plasma
concentration in 1 to 1.5 hours after the dose is taken. Following oral absorption, approximately
85% of the drug is absorbed. Although the rate and extent of absorption may decrease with food
intake and antacid use, no clinically significant change in the effect of febuxostat has been
reported; therefore, it may be taken without regard to food or antacid consumption. There is no
accumulation when it is given in therapeutic doses in daily intervals (once every 24 hours). It is
approximately 99.2% protein-bound, primarily to albumin.
Febuxostat is metabolized primarily by uridine diphosphate glucuronosyl-transferase (UGT)
enzymes by means of conjugation. A small portion also undergoes oxidation via cytochrome P
(CYP) 450 isoenzymes. However, oxidation via CYP 450 is clinically insignificant in terms of
the drugs pharmacokinetics. Febuxostat does not inhibit any major CYP isoenzymes, other than
CYP 2D6, to which it exerts a mild inhibitory effect for which no dose adjustments are required.
Febuxostat is eliminated by both renal and hepatic pathways. However, renal clearance is not
significant. Only a small amount of unchanged drug or metabolites is excreted in the urine. The
half-life is approximately five to eight hours. Over a 24-hour period, febuxostat results in a dose-
dependent decrease in serum uric acid concentrations. As a result, total daily urinary uric acid
excretions are reduced with an increase in total daily urinary xanthine excretion.
Go to:
CLINICAL EFFICACY
The FDAs approval of febuxostat was based on three randomized, double-blind, controlled
clinical trials involving patients with hyperuricemia (i.e., 8 mg/dL or higher) and gout.
FACT
20
The Febuxostat versus Allopurinol Controlled Trial (FACT) was conducted to compare the
safety and efficacy of febuxostat with that of allopurinol. In this phase 3, 52-week, multicenter
trial, 762 patients were randomly assigned to receive either febuxostat 80 mg, febuxostat 120
mg, or allopurinol 300 mg once daily for the study period. All participants receiving any urate-
lowering therapy were required to undergo a two-week washout period prior to randomization.
During this two-week period, as well as during the first eight weeks of the trial, patients were
also given 250 mg of naproxen (Naprosyn, Roche) twice daily or 0.6 mg of colchicine once daily
as a preventative measure against any associated acute gouty attacks. Any subsequent attacks
were treated according to the discretion of the investigators. Patients underwent physical
examination, laboratory testing, monitoring of vital signs, measurement of serum urate
concentration, assessment of renal function, and evaluation of compliance at two weeks, four
weeks, and monthly thereafter.
The primary endpoint was a serum urate concentration below 6 mg/dL at each of the last three
monthly measurements.
Secondary endpoints included the proportion of patients with serum urate concentrations of less
than 6 mg/dL at each visit and the percentage reduction of serum urate concentrations from
baseline to each visit. The researchers also evaluated clinical endpoints such as the percentage
reduction in tophus area, the number of tophi, and the proportion of subjects requiring treatment
for acute gouty attacks.
Of the 756 patients who were included in the final analysis, 53% of patients receiving 80 mg of
febuxostat, 62% of those receiving 120 mg of febuxostat, and 21% of those receiving allopurinol
reached the primary efficacy endpoint. Higher proportions of patients treated with febuxostat (as
opposed to allopurinol at all ranges of initial urate levels tested) also reached this endpoint.
All results were determined to be statistically significant. The secondary endpoints were also
achieved more frequently with febuxostat than with allopurinol. However, no statistically
significant differences among the groups were seen in the percentage reduction in tophus area or
in the reduction in number of tophi or gouty flares.
Adverse event rates were similar in all treatment groups. The most frequently reported adverse
events among all patients included liver function abnormalities, diarrhea, headaches, joint-related
signs and symptoms, and musculoskeletal and connective tissue signs and symptoms. Four
deaths were reported in the two febuxostat groups, but they were determined to be unrelated to
the drug.
APEX
21
The Allopurinol and Placebo-Controlled, Efficacy Study of Febuxostat (APEX) was a phase 3,
28-week, multicenter trial designed to compare the efficacy and safety of febuxostat, allopurinol,
and placebo in patients with normal and impaired renal function. Impairment was defined as a
serum creatinine level of 1.5 to 2 mg/dL.
A total of 1,072 patients received once-daily febuxostat (80, 120, or 240 mg), allopurinol (100 or
300 mg, based on renal function), or placebo. Participants receiving any urate-lowering therapy
underwent a two-week washout period prior to randomization. During this two-week period, as
well as during the first eight weeks of the trial, patients were also given either naproxen or
colchicine as prophylaxis for gout flares. Any subsequent flares were treated at the discretion of
the investigators. Serum urate levels, laboratory testing, gout flares, adverse events, concomitant
medication use, and the number and size of palpable tophi were evaluated at the every-four-week
visit.
The primary endpoint was the proportion of patients with the last three monthly serum urate
levels of below 6 mg/dL. Secondary endpoints included the proportion of patients with a serum
urate level of below 6 mg/dL at each visit, the percentage of reduction of serum urate from the
baseline value at each visit, the proportion of patients requiring treatment for gout flares between
weeks 8 and 28, the reduction in the number of tophi at each visit for patients with palpable tophi
at baseline, and the percentage of reduction in primary tophus size at each visit in patients with a
primary palpable tophus at the baseline evaluation.
Of the 1,067 patients who were included in the final analysis, higher and statistically significant
percentages of patients attained the primary endpoint. Forty-eight percent of the febuxostat 80-
mg group, 65% of the 120-mg group, and 69% of the 240-mg group achieved serum urate levels
below 6 mg/dL at the last three monthly visits, compared with the 22% of patients in both
allopurinol groups and none (0%) of the patients in the placebo group.
A significantly higher percentage of patients with impaired renal function who received
febuxostat 80 mg (44%), 120 mg (45%), and 240 mg (60%) also achieved the primary endpoint,
compared with patients receiving allopurinol 100 mg (0%). The febuxostat-treated patients also
attained the secondary endpoints more often compared with the allopurinol or placebo patients.
Higher and significant proportions of patients with serum urate levels of below 6 mg/dL at week
28 (or at the final visit) were observed with febuxostat therapy than with allopurinol or placebo.
None of the patients with renal impairment who received allopurinol 100 mg reached this
endpoint.
All febuxostat groups also experienced significantly greater decreases in serum urate levels from
baseline at week 28 (or at the final visit) compared with patients receiving allopurinol or placebo.
However, no significant differences among the groups were seen in the proportion of patients
requiring treatment for gout flares between weeks 8 and 28, in the number of tophi, or in the
percentage of reduction in tophus area.
The occurrence of adverse events was similar for all study groups. As in FACT, liver function
abnormalities, diarrhea, headaches, joint-related signs and symptoms, and musculoskeletal and
connective tissue signs and symptoms, as well as upper respiratory infections, were the most
frequently experienced events. Cardiovascular events were also similar in all groups. No deaths
were reported during the study period.
CONFIRMS
22
A study called The Efficacy and Safety of Oral Febuxostat in Subjects with Gout (CONFIRMS)
was the largest phase 3, 28-week, multicenter trial to compare daily febuxostat with allopurinol.
A total of 2,269 patients received febuxostat 40 mg, febuxostat 80 mg, or allopurinol 300 mg.
Patients with an estimated creatinine clearance [CrCl] of 30 to 59 mL/minute received 200 mg.
Prophylaxis of gout flares was provided at the investigators discretion throughout the study.
The primary endpoint was the proportion of patients who achieved final serum urate levels below
6 mg/dL. The secondary endpoint was the proportion of patients with mild chronic kidney
disease (CrCl, 6089 mL/minute) or moderate chronic kidney disease (CrCl, 3059 mL/minute)
who achieved final serum urate levels of less than 6 mg/dL.
Forty-five percent of patients who received febuxostat 40 mg, 67% of those receiving febuxostat
80 mg, and 42% of those receiving allopurinol achieved the primary endpoint. Urate-lowering
efficacy was similar for the febuxostat 40-mg and allopurinol groups, although the 80-mg dose
was superior to both the 40-mg dose and allopurinol.
In patients with chronic kidney disease (n =1,483), febuxostat 80 mg had greater urate-lowering
efficacy compared with the 40-mg dose and allopurinol; however, febuxostat 40 mg provided
greater urate-lowering efficacy than allopurinol in these patients. Overall, patients with baseline
tophi or serum urate levels higher than 10 mg/dL had a greater response to the 80-mg dose than
the 40-mg dose and allopurinol. All data were determined to be statistically significant.
The rates of adverse events (including cardiovascular events) were comparable for all groups and
levels of renal function. During the study, one patient in each febuxostat group died and three
allopurinol patients died.
Go to:
ADVERSE DRUG REACTIONS
12
Compared with allopurinol and placebo in clinical trials, febuxostat at doses of 40 mg and 80 mg
daily was associated with a higher percentage of liver function abnormalities, the most common
adverse reaction that resulted in discontinuation of therapy. Of those subjects taking febuxostat
40 mg, 1.2% experienced liver abnormalities, compared with 1.8% of patients who were
receiving 80 mg. In the allopurinol group, 0.9% discontinued therapy because of hepatic
abnormalities, compared with 0.7% of patients in the placebo group. Other common adverse
reactions that were experienced in 1% or more of subjects taking febuxostat and that occurred at
least 0.5% more often than in those receiving placebo were nausea, arthralgia, and rash.
Go to:
DRUG INTERACTIONS
12,14
Inhibition of XO by febuxostat may cause increased plasma concentrations of drugs that are
metabolized by this enzyme, although studies have not been conducted to confirm this effect.
Azathioprine (e.g., Imuran, GlaxoSmith-Kline), theophylline (Theo-Dur, Key), and
mercaptopurine (e.g., Purinethol, Gate) undergo some metabolism, mediated by XO, which has
the potential to result in toxic levels of these drugs. Therefore, the manufacturer identifies this
possibility as a contraindication for use.
There are no interactions between febuxostat and CYP 450 enzymes or CYP 1A2, 2C9, 2C19,
2D6, or 3A4. There appear to be no clinically significant effects of febuxostat on colchicine,
indomethacin, or naproxen, medications that are commonly used to treat gout. Because
hydrochlorothiazide (HCT) can cause an increase in uric acid levels, it was studied with
febuxostat. When the two agents are used together, the increase in uric acid levels has been
determined to be insignificant. No dose adjustment is necessary when febuxostat is used with
HCT, warfarin (Coumadin, Bristol-Myers Squibb), or desipramine (Norpramin, Sanofi-Aventis).
It is speculated that febuxostat is a weak inhibitor of CYP 2D6, although this property does not
seem to be clinically significant.
1
Even though febuxostat is highly protein-bound, the available
evidence is insufficient to verify the degree of displacement.
Go to:
CONTRAINDICATIONS
12
Because of the possible increases in plasma concentrations with febuxostat, this agent is
contraindicated in patients using azathioprine, mercaptopurine, or theophylline. As with other
medications, febuxostat should not be administered to patients with any hypersensitivity to any
component of the product.
Go to:
PRECAUTIONS AND WARNINGS
12
Patients should be informed that an increase in gout flares is common after the commencement
of febuxostat therapy. This is the result of the shift in urate from tissue deposits caused by the
reduction in serum uric acid levels. To help avoid such flares, prophylactic treatment with an
NSAID or colchicine is recommended when febuxostat is initiated. It may be beneficial to
continue prophylactic therapy for up to six months. Febuxostat does not need to be discontinued
if a flare occurs.
Although a causal relationship has not been established, patients should be monitored and
counseled for signs and symptoms of myocardial infarction and stroke. In randomized controlled
studies, there was a higher rate of cardiovascular thromboembolic events with febuxostat than
with allopurinol.
It is recommended that baseline liver function be assessed at two and four months and
periodically after febuxostat is initiated. Increases in liver transaminase levels are not affected by
the dose.
No adequate or well-controlled studies have been conducted on the use of febuxostat in pregnant
women. Febuxostat is a Pregnancy Category C drug. Caution should be used when this agent is
prescribed to nursing mothers because the drug has been noted to be excreted in the milk of rats.
Safety and effectiveness have not been established in patients 18 years of age or under.
Febuxostat is not recommended for patients who may have conditions that increase urate
formation. No studies have been conducted in patients with secondary hyperuricemia; however,
in rare instances, xanthine concentrations in the urine may increase and accumulate in the urinary
tract.
Go to:
DOSAGE AND ADMINISTRATION
12,14,18,19
Febuxostat is available in 40-mg and 80-mg tablets. For the treatment of gout, it is recommended
that the drug be started at 40 mg by mouth once daily. Two weeks after initiation, if serum uric
acid levels are not below 6 mg/dL, the dose can be increased to 80 mg daily.
Febuxostat can be taken with or without food. Although not clinically significant in relation to its
effects, there is a slight delay in absorption, of approximately one hour, if febuxostat is taken
with antacids that contain magnesium and aluminum hydroxide.
No dose adjustment is necessary in elderly patients or in patients with mild or moderate renal or
hepatic impairment. However, caution should be used when febuxostat is prescribed for patients
with severe renal impairment or hepatic impairment, because the data available in this regard are
inadequate.
Go to:
COST
12,23
Febuxostat (Uloric) is sold as 40-mg and 80-mg light green to green tablets. The product should
be protected from light and stored at room temperature (25C, or 77F). According to the 2009
edition of Red Book, the average wholesale price of a bottle of 30 tablets was $162, regardless of
strength.
Go to:
CONCLUSION
Febuxostat is the first drug approved and marketed for the treatment of gout in more than 40
years. It represents a new option for the management of hyperuricemia and gout, particularly in
patients who are unable to use or to tolerate the less expensive and more extensively studied
allopurinol.
Go to:
Footnotes
Disclosure: The authors report no financial or commercial relationships in regard to this article.
Go to:
REFERENCES
1. Wortmann RL. Disorders of purine and pyrimidine metabolism (chapter 353) Fauci AS,
Braunwald E, Kasper DL, et al. Harrisons Principles of Internal Medicine 17th edNew York:
McGraw-Hill; 2008. 2444. Available at:
www.accessmedicine.com/content.aspx?aid=2882696Accessed January 11, 2010.
2. Pittman JR, Bross MH. Diagnosis and management of gout. Am Fam Physician.
1999;599(7):17991806. [PubMed]
3. Loeb JN. The influence of temperature on the solubility of monosodium urate. Arthritis
Rheum. 1972;15:189192. [PubMed]
4. Becker MA, Schumacher HR, Wortmann RL, et al. Febuxostat, a novel nonpurine inhibitor of
xanthine oxidase. Arthritis Rheum. 2005;52(3):916923. [PubMed]
5. Hall AP, Barry PE, Dawber PR, et al. Epidemiology of gout and hyperuricemia: A long-term
population study. Am J Med. 1967;42:2737. [PubMed]
6. Eggebeen AT. Gout: An update. Am Fam Physician. 2007;76(6):801808. [PubMed]
7. Rott KT, Agudelo CA. Gout. JAMA. 2003;289(21):28572860. [PubMed]
8. Harris MD, Siegel LB, Alloway JA. Gout and hyperuricemia. Am Fam Physician.
1999;59(4):925934. [PubMed]
9. Keith MP, Gilliland WR. Updates in the management of gout. Am J Med. 2007;120(3):221
224. [PubMed]
10. Zhang W, Doherty M, Bardin T, et al. EULAR evidence based recommendations for gout:
Report of a task force of the EULAR Standing Committee for International Clinical Studies
Including Therapeutics (ESCISIT) Ann Rheum Dis. 2006;65:13121324. [PMC free article]
[PubMed]
11. Kelley WN, Schumacher HR., Jr . Crystal-associated synovitis. In: Kelley WN, editor.
Textbook of Rheumatology. 4th ed. Philadelphia: WB Saunders; 1993. pp. 12911336.
12. Uloric (febuxostat), prescribing information. Deerfield, IL: Takeda, Inc.; Feb, 2009.
13. FDA FDA approves drug for gout managementFebruary 13, 2009. Available at:
www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm149534.htmAccessed January
11, 2010.
14. Bruce SP. Febuxostat: A selective xanthine oxidase inhibitor for the treatment of
hyperuricemia and gout. Ann Pharmacother. 2006;40:21872194. [PubMed]
15. Febuxostat (Uloric) for chronic treatment of gout. Med Lett Drugs Ther. 2009;51(1312):37
38. [PubMed]
16. Okamoto K, Eger BT, Nishino T, et al. An extremely potent inhibitor of xanthine
oxidoreductase: Crystal structure of the enzyme-inhibitor complex and mechanism of inhibition.
J Biol Chem. 2003;278:18481855. [PubMed]
17. Takano Y, Hase-Aoki K, Horiuchi H, et al. Selectivity of febuxostat, a novel non-purine
inhibitor of xanthine oxidase/xanthine dehydrogenase. Life Sci. 2005;76:18351847. [PubMed]
18. Khosravan R, Grabowski B, Wu JT, et al. Effect of food or antacid on pharmacokinetics and
pharmacodynamics of febuxostat in healthy subjects. Br J Clin Pharmacol. 2007;65(3):355363.
[PMC free article] [PubMed]
19. Khosravan R, Grabowski BA, Wu J, et al. Pharmacokinetics, pharmacodynamics and safety
of febuxostat, a non-purine selective inhibitor of xanthine oxidase, in a dose escalation study in
healthy subjects. 2006;45(8):821841. [PubMed]
20. Becker MA, Schumacher HR, Wortmann RL, et al. Febuxostat compared with allopurinol in
patients with hyperuricemia and gout. N Engl J Med. 2005;353(23):24502461. [PubMed]
21. Schumacher HR, Becker MA, Wortmann RL, et al. Effects of febuxostat versus allopurinol
and placebo in reducing serum urate in subjects with hyperuricemia and gout: A 28-week, phase
III, randomized, double-blind, parallel group trial. Arthritis Rheum. 2008;59(11):15401548.
[PubMed]
22. Becker MA, Schumacher HR, Espinoza L, et al. A phase 3 randomized, controlled,
multicenter, double-blind trial (RCT) comparing efficacy and safety of daily febuxostat (FEB)
and allopurinol (ALLO) in subjects with goutPresented at the 2008 Annual Scientific Meeting of
the American College of Rheumatology, San Francisco, October 2429, 2008Available at:
http://acr.confex.com/acr/2008/webprogram/Paper3414.htmlAccessed January 11, 2010.
23. Uloric (febuxostat) Red Book 113th edThomson Healthcare; August2009. Supplement, p65.
You might also like
- DRUG CALCULATIONS GUIDEDocument42 pagesDRUG CALCULATIONS GUIDECarl Josef C. GarciaNo ratings yet
- Oxygen Therapy: Housemanship Training Programme Department of Anaesthesiology and Intensive CareDocument55 pagesOxygen Therapy: Housemanship Training Programme Department of Anaesthesiology and Intensive CaretorreslysNo ratings yet
- Pharmacodynamics 4Document28 pagesPharmacodynamics 4علي المحترفNo ratings yet
- Aluminum HydroxideIIDocument21 pagesAluminum HydroxideIIbayadmomoNo ratings yet
- Renal Failure PresentationDocument65 pagesRenal Failure PresentationBhawna JoshiNo ratings yet
- Care of Clients With Problems in OxygenationDocument185 pagesCare of Clients With Problems in OxygenationAnna Michelle Delos ReyesNo ratings yet
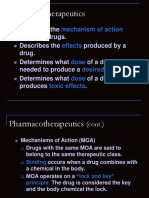
- Pharmaco TherapeuticsDocument19 pagesPharmaco TherapeuticsJareena BegumNo ratings yet
- Pharmacy Training - Gastro Intestinal TractDocument56 pagesPharmacy Training - Gastro Intestinal TractDylanSalam100% (1)
- Post Operative CareDocument25 pagesPost Operative CareS .BNo ratings yet
- Administering OxygenDocument26 pagesAdministering Oxygenjhuzt4_facebook_343onlyNo ratings yet
- PGC Reflection PaperDocument10 pagesPGC Reflection Paperapi-448502475No ratings yet
- Anatomy of The Urinary SystemDocument24 pagesAnatomy of The Urinary Systemgaylmm100% (2)
- Enteral Feeding: Gastric Versus Post-Pyloric: Table 1Document22 pagesEnteral Feeding: Gastric Versus Post-Pyloric: Table 1tasmeow23No ratings yet
- Non Steroidal Anti-Inflammatory Drugs (NSAIDs)Document16 pagesNon Steroidal Anti-Inflammatory Drugs (NSAIDs)Dilan GalaryNo ratings yet
- Plymouth Hospitals Guide to Nasogastric and Gastrostomy FeedingDocument45 pagesPlymouth Hospitals Guide to Nasogastric and Gastrostomy FeedingbandarascbNo ratings yet
- Care Provision For Older AdultsDocument7 pagesCare Provision For Older AdultsiamELHIZANo ratings yet
- Cirrhosis Case StudyDocument20 pagesCirrhosis Case StudyJodi Schaefer100% (1)
- Respiratory meds guide for new nursesDocument2 pagesRespiratory meds guide for new nursesmlbrown8No ratings yet
- Optimized Clinical Case StudiesDocument4 pagesOptimized Clinical Case StudiesAassh DcmbrNo ratings yet
- DrugsDocument20 pagesDrugsLee Won100% (1)
- VSim Pharm (Mary Richards)Document3 pagesVSim Pharm (Mary Richards)Jay Blastic's arts and FunNo ratings yet
- IV Anesthetic Agents Effects and UsesDocument72 pagesIV Anesthetic Agents Effects and UsesRaghavendra PrasadNo ratings yet
- Yorkshire Pharmacy Calculations TrainingDocument35 pagesYorkshire Pharmacy Calculations TrainingChrissieNo ratings yet
- Anti Neoplastic and Immunosupressant DrugsDocument29 pagesAnti Neoplastic and Immunosupressant DrugsAshraf Moby100% (1)
- Calculation of DosesDocument27 pagesCalculation of DosesAhmad Radhya Dionanda100% (1)
- Aluminum Hydroxide Antacids and Phosphate BindersDocument3 pagesAluminum Hydroxide Antacids and Phosphate BindersAP TOROBXNo ratings yet
- Fluid Balance in Clinical PracticeDocument8 pagesFluid Balance in Clinical Practicefernando_vaz2010100% (1)
- Depression in The ElderlyDocument23 pagesDepression in The Elderlylovelots1234No ratings yet
- Chapter 13. Heartburn and DyspepsiaDocument22 pagesChapter 13. Heartburn and DyspepsiaMonica CiorneiNo ratings yet
- Demonstration and Mechanism of Brudzinski and KernDocument3 pagesDemonstration and Mechanism of Brudzinski and KernYamamoto YuichiNo ratings yet
- Catheterization DemoDocument48 pagesCatheterization Demojonna casumpangNo ratings yet
- Group 5 - Hemodialysis - Chronic Kidney FailureDocument31 pagesGroup 5 - Hemodialysis - Chronic Kidney FailureKimberly Abella CabreraNo ratings yet
- NocturiaDocument10 pagesNocturiaKousik AmancharlaNo ratings yet
- Trauma and Emergency NursingDocument9 pagesTrauma and Emergency Nursingchinthaka18389021No ratings yet
- High Alert MedicationsDocument17 pagesHigh Alert MedicationsJoanna Marie Datahan EstomoNo ratings yet
- NURS 321/527 Unit 4 Review Digestion: GERD, Malabsorption, Pancreatitis, HepatitisDocument19 pagesNURS 321/527 Unit 4 Review Digestion: GERD, Malabsorption, Pancreatitis, HepatitisSamip PatelNo ratings yet
- Adults With Suspected Epiglottitis - Supraglottitis Guidelines For The Management ofDocument2 pagesAdults With Suspected Epiglottitis - Supraglottitis Guidelines For The Management ofAlexandros MegasNo ratings yet
- CS ShockDocument5 pagesCS ShockJuliusSerdeñaTrapal0% (5)
- Emergency Management of DKADocument12 pagesEmergency Management of DKAtinzioNo ratings yet
- The Format: Case Study FormDocument17 pagesThe Format: Case Study FormJane DyNo ratings yet
- Life and DeathDocument23 pagesLife and DeathJea Joel MendozaNo ratings yet
- Pleural EffusionDocument2 pagesPleural EffusionGellie Santos100% (1)
- Ventilation Servo-I With Nava Neurally Controlled VentilationDocument14 pagesVentilation Servo-I With Nava Neurally Controlled Ventilationraju_pnNo ratings yet
- IVTDocument71 pagesIVTIrene Soriano BayubayNo ratings yet
- (Osborn) Chapter 47: Osborn, Et Al., Test Item File For Medical-Surgical Nursing: Preparation For PracticeDocument19 pages(Osborn) Chapter 47: Osborn, Et Al., Test Item File For Medical-Surgical Nursing: Preparation For PracticeKittiesNo ratings yet
- Impaired Gas ExchangeDocument4 pagesImpaired Gas ExchangeNuraini Hamzah100% (1)
- IV Infusion SolutionDocument8 pagesIV Infusion SolutionmohammedNo ratings yet
- Post Op Worksheet FinalDocument5 pagesPost Op Worksheet FinalRiza Angela BarazanNo ratings yet
- MercaptopurineDocument2 pagesMercaptopurineBigBoostingNo ratings yet
- C 13Document11 pagesC 13Jo100% (1)
- Procedure-Nasogastric Tube InsertionDocument22 pagesProcedure-Nasogastric Tube Insertionmohamad dildarNo ratings yet
- Pain in Older PatientsDocument66 pagesPain in Older PatientsmehranerezvaniNo ratings yet
- Study Guide PNS and CNSDocument7 pagesStudy Guide PNS and CNSsquicciariniNo ratings yet
- Fundamentals Quizzing TIPSDocument41 pagesFundamentals Quizzing TIPSmelissamichellleNo ratings yet
- AnsimarDocument2 pagesAnsimarcop_perNo ratings yet
- Portfolio NFDN 2003 2Document3 pagesPortfolio NFDN 2003 2api-306095474No ratings yet
- Peg & TPNDocument23 pagesPeg & TPNapi-3722454100% (1)
- Walking Pneumonia, (Mycoplasma Pneumonia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandWalking Pneumonia, (Mycoplasma Pneumonia) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide To Different Pneumonias, Diagnosis, Treatment In Medical PracticeFrom EverandA Simple Guide To Different Pneumonias, Diagnosis, Treatment In Medical PracticeNo ratings yet
- 668236817Document4 pages668236817Anadi GuptaNo ratings yet
- Bussiness Case Five Steps To A Winning Business CaseDocument4 pagesBussiness Case Five Steps To A Winning Business CaseAnadi GuptaNo ratings yet
- Ola Ride Invoice 22 Feb 2017Document3 pagesOla Ride Invoice 22 Feb 2017Anadi GuptaNo ratings yet
- Mission of Swami SivanandaDocument3 pagesMission of Swami SivanandaSumit Kumar DashNo ratings yet
- Apex Floor-Plans PDFDocument5 pagesApex Floor-Plans PDFAnadi GuptaNo ratings yet
- 668236817Document4 pages668236817Anadi GuptaNo ratings yet
- The Essentials of Project Management, 4 EditionDocument6 pagesThe Essentials of Project Management, 4 EditionAnadi GuptaNo ratings yet
- FTTX PremisesDocument1 pageFTTX PremisesAnadi GuptaNo ratings yet
- Dishtv Dish+ Set Top Box With Recorder (South Only)Document2 pagesDishtv Dish+ Set Top Box With Recorder (South Only)Anadi GuptaNo ratings yet
- Amrapali Heartbeat CityDocument2 pagesAmrapali Heartbeat CityAnadi GuptaNo ratings yet
- Allergy Disease and Homeopathy TreatmentDocument15 pagesAllergy Disease and Homeopathy TreatmentAnadi GuptaNo ratings yet
- Ajnara Daffodil SIKKA KAMNADocument1 pageAjnara Daffodil SIKKA KAMNAAnadi GuptaNo ratings yet
- Mehboob Alam Abbasi: Curriculum VitaeDocument4 pagesMehboob Alam Abbasi: Curriculum VitaeAnadi GuptaNo ratings yet
- Lotus Green ReviewDocument1 pageLotus Green ReviewAnadi GuptaNo ratings yet
- Metro Among Slew of Projects Announced by Three AuthoritiesDocument2 pagesMetro Among Slew of Projects Announced by Three AuthoritiesAnadi GuptaNo ratings yet
- Reliance Jio plans to offer 4G wireless broadband at up to 49 MbpsDocument6 pagesReliance Jio plans to offer 4G wireless broadband at up to 49 MbpsAnadi GuptaNo ratings yet
- Kashish Developers Limited: Housing Residential Complex at Sector-111, Gurgaon, HaryanaDocument22 pagesKashish Developers Limited: Housing Residential Complex at Sector-111, Gurgaon, HaryanaAnadi GuptaNo ratings yet
- VVVVDocument3 pagesVVVVAnadi GuptaNo ratings yet
- 585453Document4 pages585453Anadi GuptaNo ratings yet
- Concient OneDocument3 pagesConcient OneAnadi GuptaNo ratings yet
- 16 National e Goverance Jaipur PDFDocument7 pages16 National e Goverance Jaipur PDFAnadi GuptaNo ratings yet
- Center ParkDocument14 pagesCenter ParkAnadi GuptaNo ratings yet
- Price ListDocument2 pagesPrice ListAnadi GuptaNo ratings yet
- CV for Amit Kumar YadavDocument2 pagesCV for Amit Kumar YadavAnadi GuptaNo ratings yet
- 38905918Document8 pages38905918Anadi GuptaNo ratings yet
- FiberOptics WhitePaperDocument19 pagesFiberOptics WhitePaperAnadi GuptaNo ratings yet
- Honey and Cinnamon Health Benefits PDFDocument4 pagesHoney and Cinnamon Health Benefits PDFAnadi GuptaNo ratings yet
- VVVDocument4 pagesVVVAnadi GuptaNo ratings yet
- Tramms D4.2Document0 pagesTramms D4.2Anadi GuptaNo ratings yet
- 1 - Censorship Lesson Plan F451Document4 pages1 - Censorship Lesson Plan F451Julia MaturoNo ratings yet
- Midterm PrinciplesDocument8 pagesMidterm Principlesarshad_pmadNo ratings yet
- Colorization of Silicon ProthesaDocument7 pagesColorization of Silicon ProthesanadyaNo ratings yet
- ALACC Method VerificationDocument10 pagesALACC Method VerificationVasu RajaNo ratings yet
- Socio-Cultural Impacts of Tourism in EthiopiaDocument10 pagesSocio-Cultural Impacts of Tourism in Ethiopiaarcherselevators100% (2)
- What Is Sociology - AutosavedDocument99 pagesWhat Is Sociology - Autosavedgragii100% (1)
- Texes 7-12 Social Studies Score 2016Document2 pagesTexes 7-12 Social Studies Score 2016api-323640755100% (1)
- Humanities 1 SyllabusDocument6 pagesHumanities 1 SyllabusEder Aguirre CapangpanganNo ratings yet
- Chattopadhyaya, B. D., Early Historical in Indian Archaeology Some Definitional ProblemsDocument12 pagesChattopadhyaya, B. D., Early Historical in Indian Archaeology Some Definitional ProblemsShyanjali DattaNo ratings yet
- ADR Form PDFDocument2 pagesADR Form PDFCha Tuban DianaNo ratings yet
- Quest For HarmonyDocument433 pagesQuest For HarmonyTanja David Arsov100% (3)
- Mary Fahey Music Lesson PlanDocument2 pagesMary Fahey Music Lesson Planapi-316572939No ratings yet
- Data Analysis Insights for Social ScientistsDocument9 pagesData Analysis Insights for Social Scientistsjuliamanaya14% (7)
- A Study On Consumer Perception Towards Online Shopping:Evidences From Consumers of Darazz OnlineDocument10 pagesA Study On Consumer Perception Towards Online Shopping:Evidences From Consumers of Darazz OnlineRoshanNo ratings yet
- Recommendation LettersDocument5 pagesRecommendation LettersChristian Irvin Harvey DavidNo ratings yet
- WorldDocument28 pagesWorldapi-3698598100% (1)
- HBLDocument21 pagesHBLNisar Akbar KhanNo ratings yet
- Unit 8 ErmDocument37 pagesUnit 8 ErmmitubaruahNo ratings yet
- The Effects of Student-Centered Approach in ImprovDocument9 pagesThe Effects of Student-Centered Approach in Improvsafira permata dewiNo ratings yet
- Approaches To Teaching ESPDocument8 pagesApproaches To Teaching ESProukia aidNo ratings yet
- Gravitation, Gauge Theories and Differential GeometryDocument178 pagesGravitation, Gauge Theories and Differential GeometryPaul Ramirez100% (1)
- ProposalDocument5 pagesProposalapi-273262763No ratings yet
- Midterm: Attendance Quiz 1 Quiz 2Document6 pagesMidterm: Attendance Quiz 1 Quiz 2Sohaib ArifNo ratings yet
- Training AND DevelopmentDocument62 pagesTraining AND DevelopmentUmbraSeriiNo ratings yet
- Assesment Checklist - RevisedDocument1 pageAssesment Checklist - Revisedapi-371585935No ratings yet
- Leadership Communication Purpose, Strategy, and Structure: Lectures Based On by Deborah J. Barrett, PH.DDocument11 pagesLeadership Communication Purpose, Strategy, and Structure: Lectures Based On by Deborah J. Barrett, PH.Dbudi100% (3)
- SASIP Launched to Evaluate School Performance in PakistanDocument2 pagesSASIP Launched to Evaluate School Performance in PakistanArooj Talat KhanNo ratings yet
- CARS Checklist - NHCC - EduDocument4 pagesCARS Checklist - NHCC - EduAngelica Faye LitonjuaNo ratings yet
- Brand ImageDocument2 pagesBrand Imagedollys59No ratings yet