Professional Documents
Culture Documents
Diabetic Retinopathy Facts
Uploaded by
Wisniardhy Suarnata Pradana0 ratings0% found this document useful (0 votes)
16 views8 pagesdiabetik retinopati
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdiabetik retinopati
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
16 views8 pagesDiabetic Retinopathy Facts
Uploaded by
Wisniardhy Suarnata Pradanadiabetik retinopati
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 8
Diabetic retinopathy - the facts
More information and support
If you have any questions about diabetic retinopathy:
ask your doctor or nurse;
contact your local screening office;
visit www.nscretinopathy.org.uk;
visit www.diabetes.org.uk;
visit www.nhsdirect.nhs.uk; or
visit www.rnib.org.uk.
Other leaflets available in this series
Eye screening for people with diabetes - the facts
Preparing for laser treatment for diabetic retinopathy
and maculopathy
This leaflet sets out
to answer some of
your questions about
the changes that
may occur, or have
occurred, in your eyes
if you have diabetes.
You might want
to discuss this
information with a
relative or carer
and with a health
professional.
Summary
Diabetic retinopathy affects your sight by damaging the small
blood vessels at the back of the eye.
Diabetic retinopathy progresses with time but may not cause
symptoms until it is quite far gone.
Laser treatment for sight-threatening diabetic retinopathy can
reduce the risk of you losing your sight.
Looking after your diabetes can reduce the risk of you
developing diabetic retinopathy and slow the rate at which it
happens.
What is diabetic retinopathy?
When diabetes affects the small blood vessels in the part of your
eye called the retina, this is known as diabetic retinopathy.
The retina lines the inside of the eye and acts rather like the film
in a camera (see diagram 1). The macula is the small central part
of the retina that you use to see things clearly and is the part
you are using now to read this leaflet. You use the rest of your
retina to see things around you and to see in the dark.
Blood vessels bring oxygen and nourishment to your retina.
These blood vessels may be damaged in a number of ways if you
have diabetes. Severe changes to the retinal blood vessels will
affect the health of your retina and this can damage your sight.
Why is diabetic retinopathy important?
Diabetic retinopathy can affect your sight and is still a
significant cause of blindness in the working population.
Laser treatment for sight-threatening retinopathy reduces
the risk of you losing your sight but needs to be given at the
appropriate stage and ideally before your vision has been
affected.
Summary
Diabetic retinopathy affects your sight by damaging the small
blood vessels at the back of the eye.
Diabetic retinopathy progresses with time but may not cause
symptoms until it is quite far gone.
Laser treatment for sight-threatening diabetic retinopathy can
reduce the risk of you losing your sight.
Looking after your diabetes can reduce the risk of you
developing diabetic retinopathy and slow the rate at which it
happens.
What is diabetic retinopathy?
When diabetes affects the small blood vessels in the part of your
eye called the retina, this is known as diabetic retinopathy.
The retina lines the inside of the eye and acts rather like the film
in a camera (see diagram 1). The macula is the small central part
of the retina that you use to see things clearly and is the part
you are using now to read this leaflet. You use the rest of your
retina to see things around you and to see in the dark.
Blood vessels bring oxygen and nourishment to your retina.
These blood vessels may be damaged in a number of ways if you
have diabetes. Severe changes to the retinal blood vessels will
affect the health of your retina and this can damage your sight.
Why is diabetic retinopathy important?
Diabetic retinopathy can affect your sight and is still a
significant cause of blindness in the working population.
Laser treatment for sight-threatening retinopathy reduces
the risk of you losing your sight but needs to be given at the
appropriate stage and ideally before your vision has been
affected.
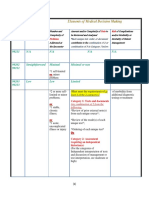
sclera
retina
macula
vitreous body
optic disc
cornea
pupil
iris
conjunctiva
lens
Who gets diabetic retinopathy?
All people with diabetes are at some risk of getting diabetic
retinopathy. This is true whether your diabetes is controlled by
diet, tablets or insulin. You are at greater risk if:
you have had diabetes for a long time;
your diabetes is poorly controlled;
you have high blood pressure; or
you are on insulin treatment.
What does diabetic retinopathy look like?
The earliest changes are called background retinopathy. Small
changes develop on the blood vessels and look like tiny red
dots. These are called microaneurysms. Larger red dots are called
retinal haemorrhages. They lie within the retina and are very
like a bruise on your skin. Background retinopathy does not
affect your sight and does not need treatment. However, you
should make sure that you go for screening every year.
As time goes by, your blood vessels may become constricted
and the retina may become starved of oxygen and nutrition.
Different signs can be seen in the retina at different stages
during this progression. These are called pre-proliferative
retinopathy. You will be referred to the hospital for more
examinations if we find signs of pre-proliferative retinopathy.
Eventually you may develop new blood vessels on the retina.
This is called proliferative diabetic retinopathy. At this stage
your sight is at risk as the vessels may bleed or may develop
scar tissue. This can pull the retina away from the underlying
layers of the eye, causing a traction retinal detachment. If the
new vessels bleed, you may see a sudden shower of floaters or
cobwebs in your sight, or your sight may be completely blurred.
This is called a vitreous haemorrhage and you should contact
your GP or an eye department immediately for advice. If you
develop proliferative retinopathy or if the eye specialist you
are seeing thinks you are very close to developing proliferative
retinopathy, you will be advised to have laser treatment.
You may also suffer from two different types of change to the
blood vessels in the macula. This is called diabetic maculopathy.
The commonest change is that the blood vessels become
leaky. Fats and fluid that are normally carried along in the
bloodstream may then leak into the macula. Fats that have
leaked into the retina are called exudates. Fluid leaking causes
waterlogging in the retina and is called oedema. Oedema at the
centre of the macula will cause you to lose some sight and you
may need gentle laser treatment.
Occasionally, the blood vessels in the macula become so
constricted that the macula is starved of oxygen and nutrition
causing your sight to get worse. This is called ischaemic
maculopathy and it does not usually respond to any type of
treatment.
How will I know if I have diabetic retinopathy?
Diabetic retinopathy does not usually cause a loss of sight
until it has reached an advanced stage. Even sight-threatening
retinopathy that is close to affecting your sight may not cause
symptoms.
Diabetic retinopathy is detected by examining the back of your
eyes to look at your retina. The healthcare professional who
looks after your diabetes should have made arrangements for
you to go for screening for diabetic retinopathy at least every
year. This will be done by taking photographs of the back of
your eye. You may also want to read Eye screening for people
with diabetes - the facts.
Doctors or optometrists (opticians) can also check your retina
using other special equipment.
You must get professional advice if you have any new problem
with your sight such as:
if your sight suddenly gets worse, distorted or you lose all or
part of your vision; or
you get a sudden increase in floaters in your vision.
Dos and donts
Diabetic retinopathy can get worse over time, but the following
measures can help you to reduce your risks of developing
diabetic retinopathy and to slow the progress of sight-
threatening retinopathy.
Control your blood glucose as effectively as possible.
See your doctor regularly to check that your blood pressure is
not raised.
Keep your regular screening appointment.
Get advice if you have a problem with your sight.
For your eyes and general health, you should also have your
cholesterol levels checked regularly and not smoke.
Diabetic retinopathy - the facts
More information and support
If you have any questions about diabetic retinopathy:
ask your doctor or nurse;
contact your local screening office;
visit www.nscretinopathy.org.uk;
visit www.diabetes.org.uk;
visit www.nhsdirect.nhs.uk; or
visit www.rnib.org.uk.
Other leaflets available in this series
Eye screening for people with diabetes - the facts
Preparing for laser treatment for diabetic retinopathy
and maculopathy
You might also like
- Clostridium Difficile Worksheet WPB: INFECTION SITE: Gastroenteritis CODE: GI-GEDEFINITION: Gastroenteritis MustDocument2 pagesClostridium Difficile Worksheet WPB: INFECTION SITE: Gastroenteritis CODE: GI-GEDEFINITION: Gastroenteritis MustWisniardhy Suarnata PradanaNo ratings yet
- Audit Checklist For Central Lines (Upload)Document2 pagesAudit Checklist For Central Lines (Upload)Joe Thesecondmonth100% (1)
- Infection Control Construction PermitDocument2 pagesInfection Control Construction PermitWisniardhy Suarnata PradanaNo ratings yet
- Brain, Mind, BehaviourDocument10 pagesBrain, Mind, BehaviourWisniardhy Suarnata PradanaNo ratings yet
- Corneal Ulcer Diagnosis and ManagementDocument215 pagesCorneal Ulcer Diagnosis and ManagementWisniardhy Suarnata Pradana100% (1)
- Trigger FingerDocument1 pageTrigger FingerWisniardhy Suarnata PradanaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Maddi (2006) PDFDocument10 pagesMaddi (2006) PDFJanine NogueraNo ratings yet
- Apraxia 2Document25 pagesApraxia 2Vellardo AlbayNo ratings yet
- Kolelitiasis in EnglishDocument18 pagesKolelitiasis in EnglishReza AkbarNo ratings yet
- Treatment of Emergency Cases Guidline Dr. Emal ShirzaiDocument104 pagesTreatment of Emergency Cases Guidline Dr. Emal Shirzaihamidazizih230No ratings yet
- 3C Diet ExcerciseDocument3 pages3C Diet ExcercisecarolinangelicaNo ratings yet
- Nutrition For HoneyDocument13 pagesNutrition For Honeydrsnair78No ratings yet
- CVS Case ProformaDocument2 pagesCVS Case ProformaRiyaSingh100% (1)
- Bacterial Food Intoxication Lecture # 6Document17 pagesBacterial Food Intoxication Lecture # 6muqaddasNo ratings yet
- HypotrophyDocument3 pagesHypotrophyopeyemi daramolaNo ratings yet
- Revewer by Bambang Daru Irwanto 1613010006 Inggil Indes RahmantoDocument10 pagesRevewer by Bambang Daru Irwanto 1613010006 Inggil Indes RahmantoadiiiiiiiiiiiiiiNo ratings yet
- Heart DiseaseDocument26 pagesHeart DiseaseJulia MarieNo ratings yet
- Backup of Homeostatic ImbalancesDocument5 pagesBackup of Homeostatic ImbalancesDwi N.No ratings yet
- Jurnal MalabsorbsiDocument6 pagesJurnal MalabsorbsiIda Putri IhsaniNo ratings yet
- ShejayLomongo BSN2Document15 pagesShejayLomongo BSN2Shejay LomongoNo ratings yet
- Mers-Cov: Frequently Asked Questions and AnswersDocument2 pagesMers-Cov: Frequently Asked Questions and AnswersKath ViteNo ratings yet
- Eye Care Tips For Computer ProfessionalsDocument22 pagesEye Care Tips For Computer ProfessionalsVel Murugan100% (1)
- Diarrhea in ChildrenDocument23 pagesDiarrhea in ChildrenSudeshna YadavNo ratings yet
- Rumana Shaikh 333 Pharmacology - Individual Task Topic 23-24 (VI Semester)Document10 pagesRumana Shaikh 333 Pharmacology - Individual Task Topic 23-24 (VI Semester)Rumana ShaikhNo ratings yet
- Perceptions, Attitudes, and Behaviors of Primary Care Providers Toward Obesity Management: A Qualitative StudyDocument18 pagesPerceptions, Attitudes, and Behaviors of Primary Care Providers Toward Obesity Management: A Qualitative StudyFitriani WidyastantiNo ratings yet
- Chapter 33: Atopic, Rheumatic, and Immunodeficiency Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionDocument8 pagesChapter 33: Atopic, Rheumatic, and Immunodeficiency Disorders Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuNo ratings yet
- Complications of Intravenous TherapyDocument29 pagesComplications of Intravenous TherapyKrizia BonillaNo ratings yet
- MeningoencephaloceleDocument13 pagesMeningoencephaloceleIda Bagus Yudha Prasista100% (1)
- Compile Nclex - RN Questions and AnswersDocument17 pagesCompile Nclex - RN Questions and Answerseric0% (1)
- 3-Level of MDMDocument3 pages3-Level of MDMmedical codingNo ratings yet
- tmpBC74 TMPDocument7 pagestmpBC74 TMPFrontiersNo ratings yet
- Onychauxis or HypertrophyDocument3 pagesOnychauxis or HypertrophyKathleen BazarNo ratings yet
- Denham Fatigue Facilitator's ManualDocument27 pagesDenham Fatigue Facilitator's Manualsergentul -No ratings yet
- Notes From Beynon LectureDocument6 pagesNotes From Beynon LecturearianNo ratings yet
- General Dermatology NotesDocument6 pagesGeneral Dermatology NotesPenny_Teoh_3451No ratings yet
- Differential Diagnosis of WeaknessDocument6 pagesDifferential Diagnosis of WeaknessAna LydiaNo ratings yet