Professional Documents
Culture Documents
Emergency Orthopaedics
Uploaded by
Akhmad Dikhyak FerdiyansahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Emergency Orthopaedics
Uploaded by
Akhmad Dikhyak FerdiyansahCopyright:
Available Formats
Orthopedic Emergencies
Ted Parks, MD
Compartment Syndrome
Neurovascular Injuries
Open Fractures
Dislocations
Septic Arthritis
Extremity Amputation
Compartment Syndrome
Anatomy of a Compartment
Compartment Syndrome
Compartment Syndrome
Signs and Symptoms:
Pain out of proportion to injury
Hx of blunt, closed trauma
Firm, swollen, tense extremity
Pain with passive motion of distal parts
The 4 Ps
Pain
Pallor
Paresthesias
Pulselessness
Measuring compartment pressures
Measuring compartment pressures
Pressure Measurements
<15mmHg = normal, resting
<30mmHg = normal, injured
>45mmHg = compartment syndrome
30 45mmHg: borderline
Watch and re-measure frequently
Consider other clues
Compartment Syndrome
Treatment
Treatment = Fasciotomy
Neurovascular Injuries
Colles Fracture
Neurovascular Injuries
Nerve Injuries
Neurological (sensory) deficits
Document grade and extent
For example:
subjective sensory deficit to light touch, median
nerve distribution
or
complete loss of sensation, dorsum all 5 fingers
If you dont document nerve injuries, you
may be held responsible for them
Neurological (sensory) deficits
Reduce the fracture, OR
Start immediately to find someone who can
Once the fracture is reduced, repeat the sensory
exam and document any improvement (or lack
thereof)
If the sensory exam does not improve
Neurological (sensory) deficits
Do nothing! Over 90% of fracture
associated nerve injuries are either
neuropraxias or axonotmeses and they will
resolve with time once the fracture is
reduced.
Neuropraxisa
Neuropraxisa
No structural damage
Nerve function returns in minutes once
local microcirculation is reestablished
Axonotmesis
Axonotmesis
Axons are damaged and deteriorate
(Wallerian degeneration), but all other
structural elements remain intact
Axon begins to regenerate after a few
weeks, growing at about 1mm/day
Motor endplates disappear without
stimulation
Neurotmesis
Neurotmesis
Essentially no chance for return of function
without repair
Once repaired, expect slow return of
function (as with axonotmesis)
Neurological injuries that dont
resolve after fracture reduction
Observe
Get EMG/NCS studies at 6 weeks
Repeat EMG/NCS studies at 12 weeks,
if no sign of improvement, explore and repair the
nerve. Nerve repair results not significantly
worse 3 months out.
Why are these emergencies?
Vascular Injuries
Vascular Injuries
Poor pulses (doppler?)
Cold, pale skin
Poor capillary refill
Vascular Injuries
1. Document exam
2. Reduce fracture (or call somebody who
will)
3. Repeat exam
4. If no change on exam, order STAT
arteriogram
5. Repair/thrombectomy
Open Fractures
Open Fractures
Problem = Infection
Open Fractures
Start broad spectrum IV anitbiotics
(example=Zosin 3.375gm)
Debride wound of obvious foreign material
Apply an occlusive dressing
Splint extremity
Formal I&D in the OR ASAP
Open Fractures
Start broad spectrum IV anitbiotics
(example=Zosin 3.375gm)
Debride wound of obvious foreign material
Apply an occlusive dressing
Splint extremity
Formal I&D in the OR ASAP
Open Fractures
Risk of osteomyelitis decreases
dramatically if I&D is done before
4-6 hours*
*R.M. Gustilo The Journal of Bone and Joint Surg.
2002, 84:682
Dislocations
Dislocations
Compromise blood
flow to tissues
Injure cartilage
surfaces
Cause ischemia of
cartilage
Dislocations
Compromise blood
flow to tissues
Injure cartilage
surfaces
Cause ischemia of
cartilage
Dislocations
Compromise blood
flow to tissues
Injure cartilage
surfaces
Cause ischemia of
cartilage
Dislocations
Document neurovascular exam
Reduce the joint, or call somebody who
can
Immobilize the extremity
Document the reduction with an xray
Septic Arthritis
Septic Arthritis
Any joint that is red, hot, swollen with no
history of trauma is infected until proven
otherwise
Fever, WBC, ESR, CRP all helpful, but not
diagnostic
Definitive test = aspiration
Knee Joint Aspiration Technique
Pt supine on table
Knee extended
Muscles relaxed
Lateral approach
Sub-patellar
Septic Arthritis
Aspiration:
1. Cultures
Septic Arthritis
Aspiration:
1. Cultures
2. Gram stain
Septic Arthritis
Aspiration:
1. Cultures
2. Grams stain
3. Crystals
Septic Arthritis
Aspiration:
1. Cultures
2. Grams stain
3. Crystals
4. Cell count:
Presume infection if >50,000 WBC per
high powered field
Septic Joint
Start broad spectrum antibiotics as soon
as you have finished the aspiration
(ie: Zosin IV, Augmentin PO)
If gram stain and cell count are negative,
D/C abx and await cultures
If Gram stain or cell count are positive,
proceed with surgical I&D ASAP
Exceptions
Traumatic Amputations
Start abx ASAP
Give one aspirin PR
Place amputated part
in a small bag of
sterile saline, place that
bag in a bag of ice
Xray stump and part
Clean stump by irregating with sterile
saline
Thank You!
Ted Parks, MD
(303) 321-1333
You might also like
- Neurological Aspect in Musculoskeletal Diseases Entrapment and CompressionDocument38 pagesNeurological Aspect in Musculoskeletal Diseases Entrapment and CompressionBakingpancakesNo ratings yet
- NeckDocument67 pagesNeckdr_asaleh100% (1)
- Pinched Nerve, A Simple Guide to the Condition, Treatment and Related DiseasesFrom EverandPinched Nerve, A Simple Guide to the Condition, Treatment and Related DiseasesNo ratings yet
- Spinal Stenosis And Pinched Nerve A Simple Guide to These conditionsFrom EverandSpinal Stenosis And Pinched Nerve A Simple Guide to These conditionsRating: 5 out of 5 stars5/5 (1)
- A Simple Guide to Neuralgia and Related Nerve DisordersFrom EverandA Simple Guide to Neuralgia and Related Nerve DisordersRating: 5 out of 5 stars5/5 (5)
- Chapter 29Document93 pagesChapter 29api-3743202No ratings yet
- Back PainDocument110 pagesBack PainRushdaNo ratings yet
- Scrotal Swelling Causes and TreatmentsDocument63 pagesScrotal Swelling Causes and TreatmentsTommysNo ratings yet
- Neurovascular Assessment.... MMMMMDocument7 pagesNeurovascular Assessment.... MMMMMArian May MarcosNo ratings yet
- Principles Fracture ManagementDocument88 pagesPrinciples Fracture ManagementYauffa Hanna Elt MisykahNo ratings yet
- Orthopedic Study GuideDocument17 pagesOrthopedic Study GuideD'Arby Janelle SmithNo ratings yet
- Complications of FracturesDocument104 pagesComplications of FracturesAmit Kochhar100% (3)
- Fracture RehabilitationDocument43 pagesFracture Rehabilitationnanahossam12345No ratings yet
- Herniated Nucleus PulposusDocument41 pagesHerniated Nucleus PulposusMichael John F. Natividad100% (1)
- Compressive Neuropathy of Upper LimbDocument49 pagesCompressive Neuropathy of Upper LimbYamunaVaaneeSivalingamNo ratings yet
- Compartment SyndromeDocument29 pagesCompartment SyndromeFazmial UjirNo ratings yet
- Open FractureDocument106 pagesOpen FractureNizwan ShamNo ratings yet
- Carpal Tunnel SyndromeDocument39 pagesCarpal Tunnel SyndromeNindyNo ratings yet
- Orthopaedic Emergencies AndreDocument49 pagesOrthopaedic Emergencies AndreLusi MunawarohNo ratings yet
- Pengayaan Koass Ortho - Update 5 VersionDocument122 pagesPengayaan Koass Ortho - Update 5 Versionanon_967171484No ratings yet
- Compartment SyndromeDocument25 pagesCompartment SyndromeestyjayantiNo ratings yet
- 3 Complications of FracturesDocument101 pages3 Complications of Fracturesq77gkyhzs4No ratings yet
- Principles of Musculoskeletal AssessmentDocument36 pagesPrinciples of Musculoskeletal AssessmentroshinisureshNo ratings yet
- Care of Patients with Musculoskeletal TraumaDocument7 pagesCare of Patients with Musculoskeletal TraumaJosephine Navarro100% (1)
- Compartment Syndromes: T. Toan Le, MD and Sameh Arebi, MDDocument74 pagesCompartment Syndromes: T. Toan Le, MD and Sameh Arebi, MDJefriKusumaNo ratings yet
- G04 Compartment SyndromeDocument31 pagesG04 Compartment Syndromesebastian1207No ratings yet
- Compartment Syndromes: T. Toan Le, MD and Sameh Arebi, MDDocument74 pagesCompartment Syndromes: T. Toan Le, MD and Sameh Arebi, MDHendry JohannesNo ratings yet
- Thoracic Outlet SyndromeDocument16 pagesThoracic Outlet SyndromeDeepak RajNo ratings yet
- Compartment SynDocument51 pagesCompartment SynFIYINFOLUWA ESTHER AYODELENo ratings yet
- AmputationDocument32 pagesAmputationjubaershimulNo ratings yet
- Carpal Tunnel SyndromeDocument23 pagesCarpal Tunnel Syndromeanon_312039754No ratings yet
- BOOK3 CamilleDocument8 pagesBOOK3 CamilleSteve tarucNo ratings yet
- Hand Examination MSDocument138 pagesHand Examination MSMadhuSudhan KNo ratings yet
- Surgery - Dychioco - Musculo Skeletal InjuriesDocument79 pagesSurgery - Dychioco - Musculo Skeletal Injuries3rd yrsNo ratings yet
- Askep Pada Pasien Dengan Kerusakan Multi SistemDocument76 pagesAskep Pada Pasien Dengan Kerusakan Multi SistemmeldaiskaNo ratings yet
- Compartment SyndromeDocument24 pagesCompartment SyndromeDexter BluesNo ratings yet
- Compartment - Syndrome Rev 2017Document19 pagesCompartment - Syndrome Rev 2017Sanaz NikiNo ratings yet
- G02-Assessment, Management and Decision Making in The Treatment of Polytrauma Patients With Head InjuriesDocument42 pagesG02-Assessment, Management and Decision Making in The Treatment of Polytrauma Patients With Head InjuriesAbdirizak SheikdonNo ratings yet
- Lecture 6 Spinal Cord InjuriesDocument26 pagesLecture 6 Spinal Cord InjuriesMahroosh KhanNo ratings yet
- Departement of Orthopaedic and TraumatologyDocument89 pagesDepartement of Orthopaedic and TraumatologyMukhizalNo ratings yet
- Spinal Surgery in The DogDocument38 pagesSpinal Surgery in The Doglovefriends_845661No ratings yet
- Fracture PP Ahmad Aqel 2013Document32 pagesFracture PP Ahmad Aqel 2013aqel605859No ratings yet
- Common Musculoskeletal Problems: DefinedDocument17 pagesCommon Musculoskeletal Problems: DefinedAllean Sarmiento ApolinarioNo ratings yet
- Seminar W2 Management of Orthopaedic EmergenciesDocument45 pagesSeminar W2 Management of Orthopaedic EmergenciesUN EPNo ratings yet
- Musculoskeletal Trauma FracturesDocument47 pagesMusculoskeletal Trauma FracturesLydia Lopz MsnrncdNo ratings yet
- Lumbar Puncture BY BHERU LALDocument6 pagesLumbar Puncture BY BHERU LALBheru LalNo ratings yet
- Colles FractureDocument89 pagesColles Fracturenur syafiqah kamaruzaman100% (1)
- Carpal Tunnel Syndrome AntyDocument22 pagesCarpal Tunnel Syndrome Antyamel015No ratings yet
- Complications of Multiple FracturesDocument35 pagesComplications of Multiple Fractureshello from the other sideNo ratings yet
- Neuorlogical AssessmentDocument38 pagesNeuorlogical AssessmentSalman KhanNo ratings yet
- Fracture Dan Penanganan EmergencyDocument52 pagesFracture Dan Penanganan Emergencyshindie lethulurNo ratings yet
- Cns Examination: BY Chris VictorDocument35 pagesCns Examination: BY Chris VictorRwabugili ChrisNo ratings yet
- Ortho EssentialDocument39 pagesOrtho EssentialaninuninNo ratings yet
- S T O P: Ports Rauma and Veruse ReventionDocument37 pagesS T O P: Ports Rauma and Veruse ReventionNabiha AjmalNo ratings yet
- Bursitis-Tendonitis-Dr - Amit PatelDocument52 pagesBursitis-Tendonitis-Dr - Amit PatelAmitNo ratings yet
- Safari 2Document35 pagesSafari 2HengYiZhiNo ratings yet
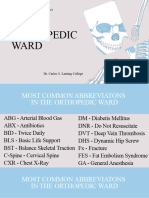
- Orthopedic-Ward-Abbrev CC FX NI-Lecture 20230830Document30 pagesOrthopedic-Ward-Abbrev CC FX NI-Lecture 20230830Yong VillafriaNo ratings yet
- Joint and Back Pain: Myriam I. Garcia Gonzalez, MD Internal Medicine Board CertifiedDocument39 pagesJoint and Back Pain: Myriam I. Garcia Gonzalez, MD Internal Medicine Board CertifiedStephanie RiveraNo ratings yet
- Compartment Syndrome AndreDocument40 pagesCompartment Syndrome AndreOlivia Christy KaihatuNo ratings yet
- FractureDocument30 pagesFractureFarida LaksitariniNo ratings yet