Professional Documents
Culture Documents
Anemia
Uploaded by
Vishnu Reddy Vardhan PulimiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anemia
Uploaded by
Vishnu Reddy Vardhan PulimiCopyright:
Available Formats
Anemia in dogs
This condition is caused by the loss or destruction of a large amount of red blood cells, which can happen in the case of internal or external bleeding caused by injury or a drug reaction, or a disease such as an immune-mediated disorder or cancer. Signs of anemia include tiredness, exercise intolerance (difficulty exercising), decreased appetite, and pale gums, though dogs with mild cases may not have any signs at all. A severe anemic may need a transfusion, and in all cases the underlying cause of the problem must be treated.
Summary
If your dog has anemia dont panic. Though severe anemia is life threatening and requires immediate veterinary attention, mild cases can be easier to reverse or manage.
Anemia develops when the number of red blood cells in the bloodstream is reduced. Since theyre responsible for the transport and delivery of oxygen throughout the body, a deficiency in red blood cells can be potentially catastrophic to the entire system.
There are many causes and types of anemia, ranging from simple blood loss or the destruction of red blood cells within the body as part of a specific disease process to the inability of the body to produce enough red blood cells. Treatment varies based on the underlying cause.
Signs and Identification
Because red blood cells carry oxygen, which is essential for all basic bodily functions, the most common signs of anemia are lethargy and exercise intolerance. Decreased appetite and pale mucous membranes (the gums, for example) are typical as well. Mild anemia may not be evident except through blood testing.
Identifying anemia definitively is done in the laboratory. Most veterinarians can perform a quick blood test called a packed cell volume (PCV) in the hospital. The PCV indicates the percentage of red blood cells in the bloodstream. If a dogs PCV is lower than the normal range, anemia is diagnosed.
Other blood tests can offer more detailed information regarding the anemia, such as whether the body is losing vs. destroying red blood cells and if its producing new red blood cells to replace them. Among these, the CBC (complete blood cell count) is the most common and critical. It evaluates the individual components of the blood, a fundamental first step in the evaluation of any anemia.
In dogs, the most common anemia-inciting processes include: Blood loss stemming from a severe injury that causes bleeding externally or internally Immune-mediated disease (a condition in which the bodys immune system attacks its own red blood cells) Bleeding into the gastrointestinal tract as a result of disease or severe inflammation Gastrointestinal bleeding as a reaction to certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) Infectious diseases, including certain diseases that are spread by ticks Blood loss from severe flea infestations (especially in very small dogs and puppies) Exposure to toxins such as lead or rat poison Cancer (may lead to bleeding into the gastrointestinal tract or bleeding from a tumor) Sometimes, anemia is caused by a lack of red blood cell production as a result of chronic diseases (such as certain types of cancer or kidney disease) or exposure to certain medications that may interfere with red blood cell production.
Diagnosis of these can be achieved with a battery of tests, including blood testing (such as a biochemistry panel), urinalysis, specific testing for tick-borne diseases, bacterial or viral infections and parasites, and imaging techniques like X-rays, ultrasound, and sometimes more sophisticated testing (such as CT scanning and the surgical biopsy of specific tissues).
Affected Breeds
All breeds of dogs can develop anemia, though some may suffer rare forms related to specific genetic diseases, such as hemophilia and other clotting disorders.
Treatment
In cases of anemia resulting from either acute or chronic loss or destruction of a large amount of red blood cells, a blood transfusion may be recommended (or required) for survival.
As previously mentioned, severe anemia results in a significantly reduced ability of the blood to deliver oxygen throughout the body and, most importantly, to vital organs such as the brain. Therefore, a blood transfusion is necessary to help deliver oxygen and nutrients to major organs and other parts of the body. Occasionally, multiple transfusions are required before the dogs body can produce enough red blood cells on its own.
Other treatments for anemia will ultimately need to be tailored to the underlying cause.
Prevention
Certain causes of anemia may be preventable. For example, to reduce the risk of infectious diseases and vehicular trauma, proper containment or supervision of dogs when outside is considered essential. Vaccination and parasite prevention are also recommended.
Anemia is a defined as a deficiency of red blood cells (erythrocytes) in the circulatory system. Adult dogs are anemic when the concentration of red cells in whole blood is less than 37 percent by volume. The
normal range is 39 to 60 percent. Red cells are produced by the bone marrow and have an average life span of 110 to 120 days. Old red cells are trapped by the spleen and removed from the circulation. The iron they contain is recycled to make new erythrocytes.
The purpose of red blood cells is to carry oxygen. Thus, the symptoms of anemia are caused by insufficient oxygen in the organs and muscles. Signs include lack of appetite, lethargy, and weakness. The mucous membranes of the gums and tongue become pale pink to white. In dogs with severe anemia, the pulse and respiratory rate are rapid, and the dog may collapse with exertion. A heart murmur may be heard. Recommended Related to Dogs
Caring for a Newborn Puppy
During the first few weeks of life, a puppys primary activities are feeding, keeping warm and developing social skills. In most cases, humans will simply watch the mother dog provide all necessary care for her puppies. However, if the puppy in your care has been separated from his mother, or if the mother dog has rejected her young or cannot produce enough milk, caring for the pup is up to you.
Read the Caring for a Newborn Puppy article > >
Anemia can be caused by blood loss, hemolysis, or inadequate red blood cell production. Blood-Loss Anemia
In adult dogs the most common causes of blood loss are trauma, slow gastrointestinal bleeding associated with stomach and duodenal ulcers, parasites, and tumors in the gastrointestinal tract. Chronic blood loss also occurs through the urinary system. Hookworms and fleas are common causes of chronic blood loss in puppies.
Treatment: Treatment must be directed toward the cause of the anemia. Gastrointestinal bleeding can be detected by checking the stools for microscopic traces of blood. Urinalysis will pick up traces of blood
in the urine that may not be visible to the naked eye. Other tests can also be used to determine the cause of the occult (microscopic) bleeding. Hemolytic Anemias
Hemolysis is an acceleration in the normal process of red blood cell breakdown. Red blood cells break down to form bile and hemoglobin. With severe hemolysis, these breakdown products accumulate in the body. Accordingly, in a dog experiencing an acute hemolytic crisis you would expect to see jaundice and hemoglobinuria (passing dark-brown urine that contains hemoglobin). In addition, the dog appears weak and pale and has a rapid pulse. The spleen, liver, and lymph nodes may be enlarged.
Causes of hemolysis include immune-mediated hemolytic anemia, congenital hemolytic anemia, infectious diseases (such as canine babesiosis and leptospirosis), drug reactions to medications such as acetaminophen, and poisonous snake bites. A number of bacteria produce toxins that destroy red blood cells, so hemolysis can also occur with severe infections. Immune-Mediated Hemolytic Anemia
This is the most common cause of hemolysis in adult dogs. Red blood cell destruction is caused by autoantibodies that attack antigens present on the surface of the cells, or by antigens from medications or organisms attached to the red blood cell walls. The weakened cells are trapped in the spleen and destroyed mmune-Mediated Hemolytic Anemia continued...
Poodles, Old English Sheepdogs, Irish Setters, and Cocker Spaniels are predisposed to immune-mediated hemolytic anemia, but all breeds are susceptible. Affected dogs are usually between 2 and 8 years of age; females outnumber males four to one.
Most cases of immune-mediated hemolytic anemia are idiopathic. That is, the reason why the autoantibodies developed in that particular dog is unknown. In some cases there is a history of recent drug therapy. An immune-mediated hemolytic anemia also occurs with systemic lupus erythematosus.
The diagnosis is made by microscopic examination of blood smears, looking for specific changes in the appearance of the erythrocytes and other blood elements; and by serologic blood tests.
Treatment: Treatment of idiopathic immune-mediated hemolytic anemia is directed toward preventing further red cell destruction by blocking the antigen-antibody reaction using corticosteroids and immunosuppressants. Severe anemia is corrected with blood transfusions. Splenectomy (removal of the spleen) may be beneficial, but only when tests prove that the spleen is contributing to the hemolytic process.
The response to treatment depends on the rate of hemolysis and whether an underlying cause can be found and corrected. The outlook is guarded; even with appropriate medical treatment, the mortality rate is close to 40 percent. Congenital Hemolytic Anemia
Several inherited abnormalities in the structure of red blood cells can result in their premature destruction. Phosphofructokinase deficiency is an autosomal recessive trait that occurs in English Springer Spaniels and Cocker Spaniels. A deficiency of this enzyme results in changes in the pH of red blood cells, causing the cells to periodically fragment and produce bouts of hemoglobinuria. There is no effective treatment.
Pyruvate kinase deficiency is another red blood cell enzyme deficiency caused by an autosomal recessive gene. This disease is recognized in several breeds, including Basenjis, Beagles, and West Highland White Terriers. Puppies usually develop the hemolytic anemia at 2 to 12 months of age. Death by age 3 is the usual outcome. Methemoglobinemia in Dogs
The purpose of hemoglobin in the blood is to carry oxygen from the lungs to other parts of the body. Methemoglobin is the result of iron oxygenation, and while it is a form of hemoglobin, it does not carry oxygen. Under normal conditions, methemoglobin is converted back to hemoglobin, and a balance is maintained. But when there is too much methemoglobin in the blood, inadequate oxygenation of bodily tissues ensues. A visible sign of methemoglobinemia is when the blood becomes brownish in color, instead of the normal oxygen rich red color. Methemoglobinemia can be the result of a genetic disorder, or it can be caused by later exposure to certain chemical agents.
Symptoms
Depression Weakness Rapid breathing Discoloration of skin and mucous membranes Jaundice Vomiting Hypothermia Swelling of face or jaw
Causes
Genetic disorder Acetaminophen ingestion Ibuprofen ingestion Topical anesthetics such as benzocaine Skunk musk
Diagnosis
Your veterinarian will want to know whether your dog has ingested acetaminophen or ibuprofen, or whether you have applied a topical medication. Blood tests may also be done at a laboratory to examine the levels of methemoglobins. If the methemoglobinemia is chronic, it is likely that the blood test will reveal a high volume of red blood cells. On the other hand, if the anemia is severe, or the cause is exposure to drugs such as acetaminophen, ibuprofen, or a topical medication, the veterinarian will look for evidence of organ injury.
A spot test may be performed where a drop of the dogs blood will be placed on an absorbent white paper and a drop of normal blood will be placed next to it. If the animal is suffering from methemoglobinemia, its blood will be noticeably browner than the bright red of the normal blood spot. Treatment
Mild to moderate no treatment necessary If drug-induced, discontinuation of the drug Acetaminophen or ibuprofen overdose vomiting induced immediately Inherited animals have normal life expectancy and do not require treatment Severely anemic blood transfusions Electrolyte imbalances resulting from vomiting, diarrhea, kidney injury, or impending shock may be treated with IVs In cases of severe anemia, methylene blue may be administered intravenously to reduce the methemoglobin count
Living and Management
Exercise extreme care when using acetaminophen and ibuprofen medications. If your pet has ingested them by accident, induce vomiting and take it to the veterinarian immediately. If you are giving your pet ibuprofen for pain, be alert for symptoms of anemia. Color should return to the skin and mucous membranes once the amount of methemoglobin in the blood has returned to a level that is not critical, and blood on the spot test appears bright red. If methylene blue treatment has been given, the proportion of red cells in the blood should be monitored closely.
You might also like
- Project Report For 10 Buffaloes VIjayawadaDocument13 pagesProject Report For 10 Buffaloes VIjayawadaVishnu Reddy Vardhan PulimiNo ratings yet
- Energy and Nutrient Requirements of Buffaloes (#127263) - 108819Document10 pagesEnergy and Nutrient Requirements of Buffaloes (#127263) - 108819Vishnu Reddy Vardhan PulimiNo ratings yet
- Starting Dairy Farm with 200 Desi CattleDocument20 pagesStarting Dairy Farm with 200 Desi CattleVishnu Reddy Vardhan PulimiNo ratings yet
- Sheep Project ReportDocument11 pagesSheep Project ReportVishnu Reddy Vardhan PulimiNo ratings yet
- Nutriprime Product ListDocument2 pagesNutriprime Product ListVishnu Reddy Vardhan PulimiNo ratings yet
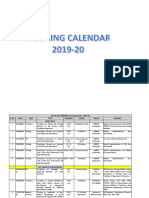
- tc19 20Document77 pagestc19 20Vishnu Reddy Vardhan PulimiNo ratings yet
- Feeding Maize Silage Effects on Nellore Lamb CarcassesDocument5 pagesFeeding Maize Silage Effects on Nellore Lamb CarcassesVishnu Reddy Vardhan PulimiNo ratings yet
- Breed Multiplication Farm OngoleDocument26 pagesBreed Multiplication Farm OngoleVishnu Reddy Vardhan Pulimi100% (8)
- Farmulas VDocument1 pageFarmulas VVishnu Reddy Vardhan PulimiNo ratings yet
- Pelleting HistoryDocument7 pagesPelleting HistoryKarim Salum VillavicencioNo ratings yet
- 4.1 Determination of Ash and Acid-Insoluble Ash: The International Pharmacopoeia - Ninth Edition, 2019Document1 page4.1 Determination of Ash and Acid-Insoluble Ash: The International Pharmacopoeia - Ninth Edition, 2019manushaNo ratings yet
- Instructions For Importing Kemin Rumen Protected Amino Acids Digital Feedbank Files Into Amts Formulation SoftwareDocument1 pageInstructions For Importing Kemin Rumen Protected Amino Acids Digital Feedbank Files Into Amts Formulation SoftwareVishnu Reddy Vardhan PulimiNo ratings yet
- Use of Sweeteners in Animal NutritionDocument5 pagesUse of Sweeteners in Animal NutritionVishnu Reddy Vardhan PulimiNo ratings yet
- A Guide To Feed MixingDocument5 pagesA Guide To Feed MixingJohn HonestNo ratings yet
- Apgli Application FormDocument3 pagesApgli Application Formmass1984No ratings yet
- DDO's PrakasamDocument46 pagesDDO's PrakasamVishnu Reddy Vardhan PulimiNo ratings yet
- Feed toxin binders reduce poultry exposureDocument5 pagesFeed toxin binders reduce poultry exposureVishnu Reddy Vardhan PulimiNo ratings yet
- Sheep NutritionDocument8 pagesSheep NutritionMarNo ratings yet
- TECHNO-ECONOMIC ASSUMPTIONS FOR CROSSBRED AND BUFFALOESDocument4 pagesTECHNO-ECONOMIC ASSUMPTIONS FOR CROSSBRED AND BUFFALOESVishnu Reddy Vardhan PulimiNo ratings yet
- Feed toxin binders reduce poultry exposureDocument5 pagesFeed toxin binders reduce poultry exposureVishnu Reddy Vardhan PulimiNo ratings yet
- SheepDocument3 pagesSheepVishnu Reddy Vardhan PulimiNo ratings yet
- MVSC Merit ListDocument10 pagesMVSC Merit ListVishnu Reddy Vardhan PulimiNo ratings yet
- Vitamin ReqDocument1 pageVitamin ReqVishnu Reddy Vardhan PulimiNo ratings yet
- New Microsoft Excel WorksheetDocument10 pagesNew Microsoft Excel WorksheetVishnu Reddy Vardhan PulimiNo ratings yet
- Anti-Inflammatory Drugs in Dogs: Mechanism of InflammationDocument1 pageAnti-Inflammatory Drugs in Dogs: Mechanism of InflammationVishnu Reddy Vardhan PulimiNo ratings yet
- Poultry Vaccination and Deworming ScheduleDocument3 pagesPoultry Vaccination and Deworming SchedulekumarNo ratings yet
- Anti-Inflammatory Drugs in Dogs: Mechanism of InflammationDocument1 pageAnti-Inflammatory Drugs in Dogs: Mechanism of InflammationVishnu Reddy Vardhan PulimiNo ratings yet
- Tuberculosis DiagnosisDocument18 pagesTuberculosis DiagnosisVishnu Reddy Vardhan PulimiNo ratings yet
- Estrus SynchronizationDocument7 pagesEstrus SynchronizationVishnu Reddy Vardhan PulimiNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Final Final PosterDocument1 pageFinal Final Posterapi-486056653No ratings yet
- High Voltage - WikipediaDocument7 pagesHigh Voltage - WikipediaMasudRanaNo ratings yet
- Non-Directive Counselling RogersDocument5 pagesNon-Directive Counselling RogersSanjeev ChaudharyNo ratings yet
- Mini-Pitch Session Exceptionalities and InclusionDocument18 pagesMini-Pitch Session Exceptionalities and Inclusionapi-486583325No ratings yet
- Abas 3 Chapter 5Document62 pagesAbas 3 Chapter 5GF David SalasNo ratings yet
- Shell Alexia 40 cylinder oil designed for IMO 2020 complianceDocument2 pagesShell Alexia 40 cylinder oil designed for IMO 2020 complianceStefas DimitriosNo ratings yet
- Maternal and Child Health Nursing, 8 Edition.: LESSON PREVIEW/REVIEW (5 Minutes)Document7 pagesMaternal and Child Health Nursing, 8 Edition.: LESSON PREVIEW/REVIEW (5 Minutes)raker boiNo ratings yet
- Liu030 Nepal Bans Solo Mountain ClimbersDocument2 pagesLiu030 Nepal Bans Solo Mountain Climberssanti.miranda.parrillaNo ratings yet
- Chem For Engineering Material by Pup BuddiesDocument46 pagesChem For Engineering Material by Pup BuddiesJedidiah MondaresNo ratings yet
- Buttermilk and Ghee ResidueDocument15 pagesButtermilk and Ghee ResidueRonak RawatNo ratings yet
- A Presentation On Kit KatDocument9 pagesA Presentation On Kit KatRaju DoleyNo ratings yet
- PTSD Checklist (PCL)Document1 pagePTSD Checklist (PCL)Manikanta Sai KumarNo ratings yet
- OECD Guideline Toxicokinetics StudyDocument20 pagesOECD Guideline Toxicokinetics StudyChirag PatelNo ratings yet
- Calculation of shell and dish thicknessDocument2 pagesCalculation of shell and dish thicknessThiru AnanthNo ratings yet
- Spez KR QUANTEC Prime enDocument155 pagesSpez KR QUANTEC Prime enDave FansolatoNo ratings yet
- Amazon To Unionize or NotDocument4 pagesAmazon To Unionize or NotPatrick MutetiNo ratings yet
- ASTM D1123 Contenido Agua en Glicol PDFDocument5 pagesASTM D1123 Contenido Agua en Glicol PDFdianacalixtogNo ratings yet
- BOM Eligibility CriterionDocument5 pagesBOM Eligibility CriterionDisara WulandariNo ratings yet
- Eye, E.N.T. & Dental AnaesthesiaDocument22 pagesEye, E.N.T. & Dental AnaesthesiawellawalalasithNo ratings yet
- NPD High Level Status: Concept Development FeasibilityDocument22 pagesNPD High Level Status: Concept Development FeasibilityRaviNo ratings yet
- Lembar Latihan - P1 - PD MitraDocument123 pagesLembar Latihan - P1 - PD MitratiengcityNo ratings yet
- Dermato Venerology ScienceDocument11 pagesDermato Venerology ScienceAQis AQishNo ratings yet
- Chloe Kho - Assignment 5 - MTT PracticeDocument5 pagesChloe Kho - Assignment 5 - MTT PracticeanthonyNo ratings yet
- English Dept Guidebook: Grammar & Exercises for Level 4Document57 pagesEnglish Dept Guidebook: Grammar & Exercises for Level 4KIngLyonLuis100% (1)
- Series NRX With PXR - Type NF Low Voltage Power (Air) Circuit Breaker Instruction ManualDocument70 pagesSeries NRX With PXR - Type NF Low Voltage Power (Air) Circuit Breaker Instruction ManualHamilton GutierrezNo ratings yet
- FLSPfister IB05000 I GBTRWSD0216 MailDocument26 pagesFLSPfister IB05000 I GBTRWSD0216 MailLuis Angel BusturiaNo ratings yet
- Face SerumDocument10 pagesFace SerumLiliana CojocaruNo ratings yet
- Success On The Wards 2007Document32 pagesSuccess On The Wards 2007mnNo ratings yet
- GS I: Factors Driving Development of Global Textile IndustriesDocument54 pagesGS I: Factors Driving Development of Global Textile IndustriesAMIT RAJNo ratings yet
- Observations of Children's Interactions With Teachers, PeersDocument25 pagesObservations of Children's Interactions With Teachers, PeersMazlinaNo ratings yet